Abstract
Background
Rheumatic heart disease (RHD) is a major cause of preventable premature cardiovascular-related death in developing countries. However, information regarding adherence rates and associated factors is limited and inconsistent in Ethiopia.
Methods
A cross-sectional study was conducted from August to November 2019 among selected RHD patients on follow-up at four hospitals in Jimma zone. Data were collected using a structured questionnaire. Adherence of RHD patients to secondary prophylaxis in the previous consecutive 12 months was assessed based on the annual frequency of received prophylaxis (monthly injection of benzathine penicillin). Good adherence was considered the patient receiving >80% of the annual dose. The collected data were entered into Epidata 3.1 and analysed using SPSS 23.
Results
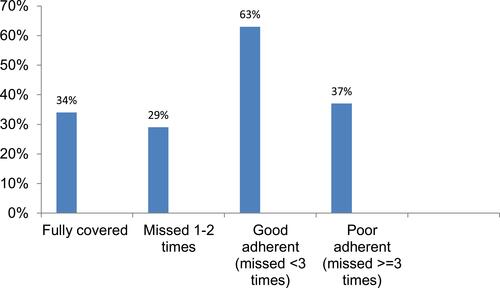
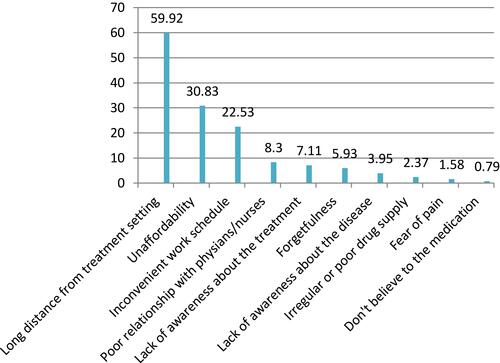
A total of 253 RHD patients taking prophylaxis were included in the analysis, and of those 178 (70.4%) were female, giving a male:female ratio of 1:2.4. The mean age was 24±11 (6–65) years. About 63% had good adherence to benzathine penicillin prophylaxis. New York Heart Association functional class I and II, rural residence, >30 km from health facility, and duration of prophylaxis >5 years were associated with poor adherence (respectively: AOR 12.6 [95% CI 2.5–63], P=0.016; AOR 6.8 [95% CI 1.9–24.4], P=0.003; AOR 5.5 [95% CI 1.2–26.7], P=0.046; AOR 1.2 [95% CI 1.1–3.2], P=0.021). Leading barriers to good adherence were long distance from the treatment setting (56.9%), followed by lack of money (38%).
Conclusion
Patients with class I and II heart failure and those living in rural areas, especially >30 km from a hospital, were identified to be poorly adherent to secondary prophylaxis.
Introduction
Acute rheumatic fever (ARF) and its sequela, rheumatic heart disease (RHD), remain important causes of morbidity and mortality in areas of socioeconomic deprivation.Citation1–Citation3 The Global Burden of Disease study estimated in 2013 that there were 33 million cases of RHD worldwide, causing 275,000 deaths annually.Citation4,Citation5 Many echocardiographic screening studies even put the prevalence of RHD at eight to 57 in 1,000 children, with true prevalence of 62–78 million individuals worldwideCitation6 and about 1.4 million deaths each year.Citation7,Citation8 The prevalence of RHD is estimated to be higher in developing countries than developed countries, ranging from 24 in 1,000 to 0.3 in 1,000, respectively.Citation9 It is estimated that 95% of cases of RHD and deaths related to this disease occur in developing countries.Citation10–Citation12 Moreover, significant costs are associated with the treatment of RHD, including heart-valve replacement.Citation13,Citation14 The severity and prognosis of RHD depends on the extent of cardiac involvement and the frequency of recurrent events.Citation15,Citation16
Systematic reviews of hospital-based death and cause-of-death studies in Africa have highlighted RHD as the main cause of cardiac morbidity and mortality in children and young adults.Citation17–Citation19 The clinical course of acute rheumatic carditis in Africa runs a fulminant course and seems more malignant.Citation20,Citation21 ARF and its complications, eg RHD, remain an enormous health problem in poor countries.Citation22–Citation24 Ethiopia is one of the African countries that share the burden of ARF and RHD, where it accounts for 50% of cardiac admission, with prevalence of 39.6% and 32.8% among Ethiopian cardiac patients in Addis Ababa and Jimma town, respectively.Citation25,Citation26 A retrospective study of deaths between 1995 to 2001 at the Tikur Anbassa Teaching Hospital, Addis Ababa, Ethiopia reported that 26.5% of cardiovascular deaths were due to RHD.Citation27
Rational use of secondary prophylaxis (regular intramuscular injections of benzathine penicillin G) is a critical cost-effective intervention for preventing morbidity and mortality related to RF.Citation28 A patient with RHD is expected to receive at least 80% of the annual prescribed injections. Otherwise, there is a higher risk of recurrent ARF and its complications.Citation29,Citation30 However, ensuring adequate adherence to secondary prophylaxis has been a challenge, and the adherence rate is poor among adolescents and chronic patients,Citation31–Citation36 due to different factorsCitation34,Citation37–Citation42 and barriers.Citation43–Citation48 There are no reliable and consistent data in Ethiopia, asstudies have been conducted only at a single institution. Therefore, the present study aimed to assess adherence of RHD patients to secondary prophylaxis and associated factors at multiple hospitals in Jimma zone, southwest Ethiopia.
Methods
Study Setting and Design
The study was conducted at four public hospitals in Jimma zone (Jimma Medical Center, Shenen Gibe Hospital, Agaro Hospital, and Seka Chekorsa Hospital), which are located in Oromia region, southwest Ethiopia. Jimma Medical Center and Shenen Gibe Hospital are located in Jimma town, 354 km from the capital — Addis Ababa. Jimma Medical Center is one of the country’s teaching hospitals, and serves as a referral hospital for southwest Ethiopia. Agaro Hospital is a district hospital located in Agaro town, about 45 km from Jimma to the west direction, where Seka Chekorsa Hospital is a district hospital located in Seka Chekorsa town, 20 km from Jimma to the south.
A cross-sectional study design was employed at cardiac clinics of Jimma medical center, outpatient clinics of Agaro, Seka Chekorsa and Shenen Gine hospitals from August to November 2019 among RHD patients on follow-up who fulfilled inclusion criteria (all age-groups, on benzathine penicillin prophylaxis for at least 1 year before the date of interview). Sample size was calculated using the single-population formula by taking P’=50% with margin error of 0.05. Finally, a total sample of 278 RHD patients were considered to represent RHD patients after computing the finite population–correction formula and 10% contingency for nonresponse. Patients who met the inclusion criteria were consecutively recruited until the estimated sample was reached.
Data Collection
Data were collected with a structured questionnaire administered by face-to-face interviews. Necessary medical data were reviewed from patient records. Information on demographic and socioeconomic characteristics, health care team–related factors, system-related factors, condition-related factors, therapy-related factors, and patient-related factors were collected according to WHO recommendations.Citation32 Adherence of RHD patients was determined based on frequency of annual prophylaxis received, and possible barriers were assessed if they had missed more than three shots by providing multiple-choice questions. Data were collected by trained medical interns and nurses working at cardiac clinics, supervised by internal medicine residents.
Data Processing and Analysis
Data were entered into EpiData version 3.1 and then exported to SPSS version 23 for further analysis. Cross-tabulation and logistic regression were applied to examine associations between predictors and the outcome variable (adherence status). Descriptive statistics, ie, means ± SD, frequency, and percentages aere used to express variables. ORs and 95% CI were used to quantify the strength of associations. All statistical tests were two-tailed, and P<0.05 was considered statistically significant.
Operational Definitions
Adherence
RHD patients were regarded as having good adherence when the rate of adherence to secondary prophylaxis was ≥80% of the expected injections (if injected more than ten times per year) while good adherence was egarded as the patient missing prophylaxis at least three times per year.Citation29,Citation36,Citation49 In Ethiopia, adherence to secondary prophylaxis is focused to eradicate/prevent the disease by promoting injections for patients every 4 weeks.Citation50 Benzathin penicillin G injection is given, in accordance with the WHO 2003 guideline recommendation.Citation51
Results
Sociodemographic Characteristics of Participants
From 278 expected RHD patients, 253 participated in the study, giving a response rate of 91%. These patients, all of whom were on benzathine penicillin, were included in the analysis, of which 178 (70.4%) were female, giving a male:female ratio of 1:2.4. The mean age of patients was 24±11 (6-65) years, and the majority (109, 43.1%) were aged >24 years. The majority of the patients (73.1%) were Oromo in ethnicity and Muslim in religion (75.5%), rural residents (66%), and attending Jimma Medical Center (77.9%). The mean annual income was US$50, as detailed in .
Table 1 Sociodemographic characteristics of patients with rheumatic heart disease on monthly benzathine penicillin at four hospitals in Jimma zone from August to November 2019
Clinical Characteristics of Participants
Almost three quarters (74.3%) of patients had a history of hospitalization for RHD. More than half (56.5%) were in NYHA class II. There were no other cases of RHD in the family among 94.5% of respondents, and only 14 (5.5%) reported family member/s suffering from a similar illness ().
Table 2 Clinical characteristics of participants with RHD on monthly benzathine penicillin at four hospitals in Jimma zone from August to November, 2019
Adherence of RHD Patients to Secondary Prophylaxis
Of the 253 RHD patients receiving secondary prophylaxis, 86 (34%) had received all annual injections and 167 (65.2%) had missed their regular injection at least once in the past year. The proportion of patients who had missed injections once/twice and three or more times was 29% and 37%, respectively. In sum, 160 (63%) were identified as having good adherence, while 93 (37%) were considered poorly adherent to monthly benzathine penicillin injections (ie, missing fewer than and three or more injections in the past year, respectively), as detailed in .
Factors Associated with Adherence of RHD Patients to Secondary Prophylaxis
To determine factors associated with adherence of RHD patients to secondary prophylaxis, cross-tabulation and logistic regression were applied. For binary logistic regression, eleven independent variables (age, sex, urban/rural residence, distance from health facility, family size, monthly household income, duration of prophylaxis, duration of disease, NYHA class, hospitalization history, and family history of RHD) were selected (P<0.25) as potential predictors of adherence status. Finally, four variables (NYHA stage I and II, rural residence, distance from health facility >30 km, and duration of prophylaxis (>5 years)) were determined as the factors associated with poor adherence ().
Table 3 Factors associated with adherence status of RHD patients to secondary prophylaxis by cross-tabulation and logistic regression
(respectively: AOR 12.6 [95% CI 2.5–63], P=0.016; AOR 6.8 [95% CI 1.9–24.4], P=0.003; AOR 5.5 [95% CI 1.2–26.7], P=0.046; AOR 1.2 [95% CI 1.1–3.2], P=0.021)
Barriers to Good Adherence to Secondary Prophylaxis
The main reasons for missing prophylaxis were were long distance from treatment settings (56.9%), lack of money (38%), unaffordability (30.8%), and inconvenient work schedule (22.5%; ).
Discussion
A patient with RHD is expected to receive at least 80% of annual prescribed injections. Receiving <80% places them at higher risk of recurrent ARF and its complications.Citation36,Citation49 The present study revealed an adherence rate of 63%, which is within the range of 29.5%Citation44 to 93.6%Citation52 reported so far. This finding was almost comparable with Pelajo et al, who reported an adherence rate of 65% among RHD patients in Brazil.Citation31 However, our figure was considerably higher than that found by Sayed (29.5%),Citation44 Thompson et al (48.7%),Citation48 Prasad et al (50%),Citation46 Musoke et al (54%),Citation53 Gasse et al (54%),Citation38 Mohammed et al (55.2%),Citation29 Huck et al (58%),Citation43 and Harrington et al (59%).Citation34 On the other hand, it was considerably less than of Saxena et al (93.6%),Citation52 Culliford-Semmens et al (92%),Citation54 Kumar et al (90%),Citation45 Mekonnen et al (80.6%),Citation37 and Sial et al (73.5%).Citation55
The variability in levels of adherence may reflect the different systems in which these studies were done, duration of followup, different factors that may influence adherence, individual study designs, and population variations.
Factors associated with adherence in the present study were: 1) heart condition of the patients (also supported by Sial et alCitation55); 2) residence (also in harmony with Gasse et al,Citation38 who reported that living rurally where there is no health-system coverage predisposes RHD patients to poor adherence to secondary prophylaxis); and 3) long distance from the health institution (also supported by a number of studiesCitation34,Citation39,Citation41,Citation48).
The present finding was also consistent with other studies conducted in Africa: Uganda,Citation56,Citation57 MalawiCitation58, Tanzania,Citation59 and South Africa.Citation60
In this study, the commonest reasons reported for missing monthly benzathine prophylaxis injections was long distance from hospitals (56.9%), lack of money (38%), unaffordability (30.8%), and inconvenient work schedule (22.5%). This finding is also supported by different studies.Citation40,Citation43–Citation45,Citation47,Citation61
Conclusion
After adjusting for confounding effects of other variables, place of residence, duration of prophylaxis, NYHA class, and distance from institution were found to be independently associated with adherence to secondary prophylaxis.
RHD patients dwelling in rural areas, especially >30 km from a hospital, were identified to be poorly adherent to secondary prophylaxis. As such, authors the recommend that prophylaxis be delivered at nearby primary health–care units, continuous health education about secondary prophylaxis adherence be strengthened, primary-health facilities be assessed for the delivery of secondary prophylaxis, and further research and solutions directly targeting these barriers to improve patient adherence and decrease overall risk, including recurrence of ARF. Finally, the authors kindly request that all responsible organizations/bodies (Federal Ministry of Health, health institutions, health-care providers) focus on providing health awareness about the disease and prophylaxis to the entire community via different media.
Data-Sharing Statement
Materials needed can be provided upon request from the corresponding author.
Ethics Approval and Consent to Participate
Ethics approval for this study was obtained from the Jimma University Ethics Committee. All participants provided informed consent or informed consent was obtained from a parent or legal guardian of any patient aged <18 years, and this study was conducted in accordance with the Declaration of Helsinki.
Acknowledgment
The authors would like to thank Jimma University for providing funding, all data collectors, and the RHD patients who participated in the study.
Disclosure
The authors declared that they have no conflicts of interest.
Additional information
Funding
References
- Carapetis JR, Beaton A, Cunningham MW, et al. Acute rheumatic fever and rheumatic heart disease. Nat Rev Dis Primers. 2016;2(1):1–24.
- Zühlke LJ, Engel ME, Watkins D, Mayosi BM. Incidence, prevalence and outcome of rheumatic heart disease in South Africa: a systematic review of contemporary studies. Int J Cardiol. 2015;199:375–383.
- Coffey PM, Ralph AP, Krause VL. The role of social determinants of health in the risk and prevention of group A streptococcal infection, acute rheumatic fever and rheumatic heart disease: a systematic review. PLoS Negl Trop Dis. 2018;12(6):e0006577. doi:10.1371/journal.pntd.0006577
- Nulu S, Bukhman G, Kwan GF. Rheumatic heart disease: the unfinished global agenda. Cardiol Clin. 2017;35(1):165–180. doi:10.1016/j.ccl.2016.08.006
- Palafox B, Mocumbi AO, Kumar RK, et al. The WHF roadmap for reducing CV morbidity and mortality through prevention and control of RHD. Glob Heart. 2017;12(1):47–62. doi:10.1016/j.gheart.2016.12.001
- Gemechu T, Mahmoud H, Parry EH, Phillips DI, Yacoub MH. Community-based prevalence study of rheumatic heart disease in rural Ethiopia. Eur J Prev Cardiol. 2017;24(7):717–723. doi:10.1177/2047487316687104
- Dougherty S, Khorsandi M, Herbst P. Rheumatic heart disease screening: current concepts and challenges. Ann Pediatr Cardiol. 2017;10(1):39. doi:10.4103/0974-2069.197051
- Steer AC, Kado J, Wilson N, et al. High prevalence of rheumatic heart disease by clinical and echocardiographic screening among children in Fiji. J Heart Valve Dis. 2009;18(3):327–335.
- Carapetis JR, McDonald M, Wilson NJ. Acute rheumatic fever. Lancet. 2005;366(9480):155–168. doi:10.1016/S0140-6736(05)66874-2
- Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden of group A streptococcal diseases. Lancet Infect Dis. 2005;5(11):685–694. doi:10.1016/S1473-3099(05)70267-X
- Carapetis JR, Mayosi BM, Kaplan EL. Controlling rheumatic heart disease in developing countries. Cardiovasc J S Afr. 2006;17(4):164–165.
- Watkins DA, Johnson CO, Colquhoun SM, et al. Global, regional, and national burden of rheumatic heart disease, 1990–2015. N Engl J Med. 2017;377(8):713–722. doi:10.1056/NEJMoa1603693
- Milne RJ, Lennon D, Stewart JM, Vander Hoorn S, Scuffham PA. Mortality and hospitalisation costs of rheumatic fever and rheumatic heart disease in New Zealand. J Paediatr Child Health. 2012;48(8):692–697. doi:10.1111/j.1440-1754.2012.02446.x
- Cilliers AM. Rheumatic fever and its management. BMJ. 2006;333(7579):1153–1156. doi:10.1136/bmj.39031.420637.BE
- Meira ZMA, Goulart EMA, Colosimo EA, Mota CCC. Long term follow up of rheumatic fever and predictors of severe rheumatic valvar disease in Brazilian children and adolescents. Heart. 2005;91(8):1019–1022. doi:10.1136/hrt.2004.042762
- Feinstein AR, Stern EK, Spagnuolo M. The prognosis of acute rheumatic fever. Am Heart J. 1964;68(6):817–834. doi:10.1016/0002-8703(64)90132-2
- Mayosi BM, Gamra H, Dangou J-M, Kasonde J. Rheumatic heart disease in Africa: the Mosi-o-Tunya call to action. Lancet Glob Health. 2014;2(8):e438–e439. doi:10.1016/S2214-109X(14)70234-7
- Hewitson J, Zilla P. Children’s heart disease in sub-Saharan Africa: challenging the burden of disease: children’s heart disease. Sa Heart. 2010;7(1):18–29.
- Nkomo VT. Epidemiology and prevention of valvular heart diseases and infective endocarditis in Africa. Heart. 2007;93(12):1510–1519. doi:10.1136/hrt.2007.118810
- Zühlke L, Mirabel M, Marijon E. Congenital heart disease and rheumatic heart disease in Africa: recent advances and current priorities. Heart. 2013;99(21):1554–1561.
- Essop MR, Nkomo VT. Rheumatic and nonrheumatic valvular heart disease: epidemiology, management, and prevention in Africa. Circulation. 2005;112(23):3584–3591. doi:10.1161/CIRCULATIONAHA.105.539775
- McLaren MJ, Markowitz M, Gerber MA. Rheumatic heart disease in developing countries: the consequence of inadequate prevention. Ann Intern Med. 1994;120(3):243–245. doi:10.7326/0003-4819-120-3-199402010-00012
- Eisenberg MJ. Rheumatic heart disease in the developing world: prevalence, prevention, and control. Eur Heart J. 1993;14(1):122–128. doi:10.1093/eurheartj/14.1.122
- Carapetis JR. Rheumatic heart disease in developing countries. N Engl J Med. 2007;357(5):439–441. doi:10.1056/NEJMp078039
- Hodes RM. Pattern of heart disease in Ethiopia as seen in a cardiology referral clinic. Cardiology. 1988;75(6):458–464. doi:10.1159/000174417
- Habte B, Alemseged F, Tesfaye D. The pattern of cardiac diseases at the cardiac clinic of Jimma University specialised hospital, south West Ethiopia. Ethiop J Health Sci. 2010;20(2).
- Oli K, Asmera J. Rheumatic heart disease in Ethiopia: could it be more malignant? Ethiop Med J. 2004;42(1):1–8.
- WHO. WHO programme for the prevention of rheumatic fever/rheumatic heart disease in 16 developing countries: report from Phase I (1986–90). WHO Cardiovascular Diseases Unit and principal investigators. Bull World Health Organ. 1992;70(2):213–218.
- Mohammed K, Demissie WR, Gare MB. Adherence of rheumatic heart disease patients to secondary prophylaxis and main reasons for poor adherence at Jimma Medical Center. E J Cardiovasc Med. 2019;7(1):22. doi:10.32596/ejcm.galenos.2019.00004
- Reményi B, Wilson N, Steer A, et al. World Heart Federation criteria for echocardiographic diagnosis of rheumatic heart disease—an evidence-based guideline. Nat Rev Cardiol. 2012;9(5):297–309.
- Pelajo CF, Lopez-Benitez JM, Torres JM, de Oliveira SK. Adherence to secondary prophylaxis and disease recurrence in 536 Brazilian children with rheumatic fever. Pediatr Rheumatol. 2010;8(1):22. doi:10.1186/1546-0096-8-22
- WHO. Adherence to Long-Term Therapies: Evidence for Action. World Health Organization; 2003.
- Sabaté E, Sabaté E. Adherence to Long-Term Therapies: Evidence for Action. World Health Organization; 2003.
- Harrington Z, Thomas DP, Currie BJ, Bulkanhawuy J. Challenging perceptions of non-compliance with rheumatic fever prophylaxis in a remote Aboriginal community. Med J Aust. 2006;184(10):514–517. doi:10.5694/j.1326-5377.2006.tb00347.x
- Carapetis JR, Zühlke LJ. Global research priorities in rheumatic fever and rheumatic heart disease. Ann Pediatr Cardiol. 2011;4(1):4. doi:10.4103/0974-2069.79616
- Remenyi B, Carapetis J, Wyber R, Taubert K, Mayosi BM. Position statement of the World Heart Federation on the prevention and control of rheumatic heart disease. Nat Rev Cardiol. 2013;10(5):284. doi:10.1038/nrcardio.2013.34
- Mekonen KK, Yismaw MB, Abiye AA, Tadesse TA. Adherence to Benzathine Penicillin G secondary prophylaxis and its determinants in patients with rheumatic heart disease at a cardiac center of an Ethiopian Tertiary Care Teaching Hospital. Patient Prefer Adherence. 2020;14:343. doi:10.2147/PPA.S238423
- Gasse B, Baroux N, Rouchon B, Meunier J-M, De Frémicourt I, D’Ortenzio E. Determinants of poor adherence to secondary antibiotic prophylaxis for rheumatic fever recurrence on Lifou, New Caledonia: a retrospective cohort study. BMC Public Health. 2013;13(1):131. doi:10.1186/1471-2458-13-131
- Farzana K, Faruque MO, Zareen S, Choudhury KN, Hossain A. Factors affecting therapeutic compliance among the patients with rheumatic heart disease in Bangladesh. Cardiovasc J. 2018;10(2):180–185. doi:10.3329/cardio.v10i2.36289
- Janvier D Factors, beliefs and barriers associated with adherence to secondary prophylaxis amongst children and adolescents with rheumatic heart disease at Public Tertiary Hospitals in Rwanda–a cross-sectional study; 2019.
- Ralph AP, Read C, Johnston V, et al. Improving delivery of secondary prophylaxis for rheumatic heart disease in remote Indigenous communities: study protocol for a stepped-wedge randomised trial. Trials. 2016;17(1):51. doi:10.1186/s13063-016-1166-y
- Nemani L, Maddury J, Barik R, Arigondam AK. A Cross-sectional study to look at the determinants of poor adherence to secondary penicillin prophylaxis for rheumatic heart disease at a tertiary care center in South India. J Clin Prev Cardiol. 2018;7(1):5. doi:10.4103/JCPC.JCPC_25_17
- Huck DM, Nalubwama H, Longenecker CT, Frank SH, Okello E, Webel AR. A qualitative examination of secondary prophylaxis in rheumatic heart disease: factors influencing adherence to secondary prophylaxis in Uganda. Glob Heart. 2015;10(1):63–69. doi:10.1016/j.gheart.2014.10.001
- Sayed GA Compliance for secondary prophylaxis for controlling rheumatic fever and rheumatic heart disease in Egyptian children; 2011.
- Kumar R, Thakur JS, Aggarwal A, Ganguly NK. Compliance of secondary prophylaxis for controlling rheumatic fever and rheumatic heart disease in a rural area of northern India. Indian Heart J. 1997;49(3):282.
- Prasad A, Prasad A, Singh BK, Kumar S. Compliance to the secondary prophylaxis and awareness of rheumatic heart disease: a cross-sectional study in low-income province of India. J Fam Med Primary Care. 2020;9(3):1431. doi:10.4103/jfmpc.jfmpc_1056_19
- Gordis L, Markowitz M, Lilienfeld AM. Why patients don’t follow medical advice: a study of children on long-term antistreptococcal prophylaxis. J Pediatr. 1969;75(6):957–968. doi:10.1016/S0022-3476(69)80332-X
- Thompson SB, Brown CH, Edwards AM, Lindo JLM. Low adherence to secondary prophylaxis among clients diagnosed with rheumatic fever, Jamaica. Pathog Glob Health. 2014;108(5):229–234. doi:10.1179/2047773214Y.0000000146
- De Dassel JL, Fittock MT, Wilks SC, Poole JE, Carapetis JR, Ralph AP. Adherence to secondary prophylaxis for rheumatic heart disease is underestimated by register data. PLoS One. 2017;12(5):e0178264. doi:10.1371/journal.pone.0178264
- Watkins D, Zuhlke L, Engel M, et al. Seven key actions to eradicate rheumatic heart disease in Africa: the Addis Ababa communiqué. Cardiovasc J Afr. 2016;27(3):184–187. doi:10.5830/CVJA-2015-090
- WHO. Rheumatic fever and rheumatic heart disease. Available from: https://www.who.int/cardiovascular_diseases/publications/trs923/en/. Accessed November 1, 2020.
- Saxena A, Mehta A, Ramakrishnan S. Adherence to benzathine penicillin in children with rheumatic fever/rheumatic heart disease: results from an Indian pediatric RHD registry. J Am Coll Cardiol. 2015;65(10 Supplement):A2019. doi:10.1016/S0735-1097(15)62019-8
- Musoke C, Mondo CK, Zhang W, et al. Benzathine penicillin adherence for secondary prophylaxis among patients affected with rheumatic heart disease attending Mulago Hospital. Cardiovasc J Afr. 2013;24(4):124. doi:10.5830/CVJA-2013-022
- Culliford-Semmens N, Tilton E, Webb R, et al. Adequate adherence to benzathine penicillin secondary prophylaxis following the diagnosis of rheumatic heart disease by echocardiographic screening. N Z Med J. 2017;130(1457):50.
- Sial JA, Farman MT, Batra MK, Karim M. Adherence to secondary prophylaxis of rheumatic fever in patients with rheumatic heart disease in rural areas. Pak Heart J. 2018;51(3).
- Huck DM, Nalubwama H, Longenecker CT, et al. Examination of secondary prophylaxis in rheumatic heart disease: factors influencing adherence to secondary prophylaxis in Uganda. Glob Heart. 2015;10(1):63–69.e1. doi:10.1016/j.gheart.2014.10.001
- Andrea B, Robert M, Craig S, Emmy O, Peter L, Charles M. Response to letters regarding article, “Echocardiography screening for rheumatic heart disease in Ugandan Schoolchildren”. Circulation. 2012;126(25):e478–e479. doi:10.1161/CIRCULATIONAHA.112.147538
- Sanyahumbi A, Beaton A, Guffey D, et al. Two-year evolution of latent rheumatic heart disease in Malawi. Congenit Heart Dis. 2019;14(4):614–618. doi:10.1111/chd.12756
- Pallangyo P, Millinga J, Bhalia S, et al. Medication adherence and survival among hospitalized heart failure patients in a tertiary hospital in Tanzania: a prospective cohort study. BMC Res Notes. 2020;13(1):89. doi:10.1186/s13104-020-04959-w
- Prendergast AJ Perkins S, Joachim A. Participation in research improves overall patient management: insights from the Global Rheumatic Heart Disease registry (REMEDY). Cardiovasc J Afr. 2018;29(2):98–105. doi:10.5830/CVJA-2017-054
- Petricca K, Mamo Y, Haileamlak A, Seid E, Parry E. Barriers to effective follow-up treatment for rheumatic heart disease in Jmma, Ethiopia: a grounded theory analysis of the patient experience. Ethiop J Health Sci. 2009;19(1).