Abstract
Purpose
To evaluate the impact of a community-based pharmacist-led face-to-face counseling program on medication adherence for patients who were new to therapy (NTT) for statin medications.
Patients and methods
This retrospective cohort study evaluated a program that was implemented in 76 national community pharmacies located in the midwest USA. It consisted of two face-to-face patient counseling sessions with a pharmacist that addressed patient barriers to adherence. A group of 2056 NTT statin patients was identified between September 1, 2010 and October 31, 2010, and was followed for 12 months. The intervention group consisted of 586 patients, and the comparison group comprised 516 patients. Outcomes were measured using the continuous medication possession ratio (MPR), categorical MPR, and medication persistency.
Results
After adjusting for covariates, the intervention group had statistically greater MPR than the comparison group at every month measured. For example, at 12 months the intervention group had a MPR of 61.8% (CI, 54.5%–69.2%) and the comparison group had a MPR of 56.9% (CI, 49.5%–64.3%); this 4.9% difference is significant (P < 0.01). The 12 month categorical MPR also showed significant differences between groups (χ 2 = 6.12, P < 0.05); 40.9% of the intervention group and 33.7% of comparison group had a MPR greater than or equal to 80%. Finally, the intervention group had significantly greater persistency with their medication therapy than the comparison group at 60, 90, 120, and 365 days.
Conclusion
Patients who participated in brief face-to-face counseling sessions with a community pharmacist at the beginning of statin therapy demonstrated greater medication adherence and persistency than a comparison group. This brief targeted intervention at the initiation of maintenance drug therapy moderates the high risk of nonadherence and discontinuation; it helps patients establish a routine of daily self-medication and potentially improves their long-term clinical outcomes.
Introduction
Nonadherence to medication therapy is a problem faced by many patients with chronic conditions.Citation1,Citation2 It is estimated that more than 25% of patients in the USA are nonadherent with their prescribed medications.Citation3 With over 133 million Americans, almost half of adults, living with at least one chronic condition, this problem is costly in terms of morbidity, mortality and health care budgets.Citation4–Citation7 In 2009, the annual cost of nonadherence in the USA was estimated at USD$290 billion.Citation8
Hypercholesterolemia is one of the most common chronic conditions, affecting over 33.5 million adults in the USA, and it is a significant risk factor for cardiovascular disease.Citation9,Citation10 For some patients, it can be managed with improvements to diet and exercise; but for many others, additional medication therapy such as statin drugs, is required to lower cholesterol levels.Citation11,Citation12 Unfortunately, many patients are nonadherent to statin medications.Citation9 It has been reported that medical costs and risk of hospitalization for patients with hypercholesterolemia whose medication adherence rates were less than 80%, were significantly higher than for those with adherence rates of 80% and greater.Citation7
Nonadherence may be driven by a myriad of factors that can be practical and behavioral. These factors include personal beliefs/environment, sociodemographic characteristics, disease state, comorbidities, health status, cost factors, patient perception of drug therapy value, issues related to drug regimen complexity and side effects, health literacy, and poor communication with health professionals.Citation13–Citation17 For example, a survey of patients with poor adherence to antihypertensive drug therapy in a managed care setting found that simple forgetfulness and being too busy were the most common reasons given for poor adherence.Citation18
Community pharmacists are well positioned to help patients overcome barriers to adherence. Several studies demonstrate that patient counseling by community pharmacists can improve persistence, adherence, self-care, and in some cases yield a net economic return.Citation7,Citation19–Citation22 For example, Project ImPACT showed that for patients with poorly controlled lipid disorders, counseling by pharmacists in community pharmacy settings can improve persistence and adherence with drug therapy, and improve lipid levels.Citation19 In the Asheville Program, a multi-year study involving consultation for diabetic patients with community-based pharmacists, glycosylated hemoglobin (A1C) values and lipid levels improved, medical costs decreased and worker productivity increased.Citation20 The Ten City Challenge demonstrated that community pharmacist-provided diabetes patient coaching results in greater patient engagement in self-care and improved process of care indicators including A1C, influenza vaccinations, systolic and diastolic blood pressure, lipid profiles and percentage of patients receiving foot and eye examinations.Citation21 Finally, a systematic review of the published literature found pharmacist face-to-face interventions performed in community pharmacy settings to be more effective than other types of interventions at improving patient adherence to medication therapy.Citation22
The objective of the present study was to assess the impact of a community-based pharmacist-led face-to-face counseling program on medication adherence for patients who were new to therapy with statin medications.
Methods
We conducted a retrospective cohort study to evaluate a program designed to improve medication adherence and persistency among patients who were new to therapy (NTT) for statin medications. Patients were defined as NTT if the patient had no evidence of a filled prescription in the statin therapeutic class during the previous 15 months. The program was implemented in 76 national community pharmacies located in a major metropolitan area in the Midwest. The program consisted of two face-to-face patient counseling sessions with a clinical pharmacist.
All 214 licensed pharmacists providing interventions received 2 hours of additional training via an interactive webinar. The training focused on brief motivational interviewing techniques for addressing patient barriers to adherence. It also included practical techniques on how to fit the counseling sessions into their existing pharmacy workflow.
Patient selection
When a patient submitted a prescription for a statin medication and was identified by the pharmacy data system as NTT, the system notified the pharmacist to offer the patient a first fill face-to-face counseling session. The first session consisted of motivational interviewing to determine the patient’s confidence and commitment to following the prescribed treatment regimen as well as discussion about f itting medications into their daily routine. Patients who completed the initial counseling session and who were not excluded due to self-report of prior use of statins were automatically eligible for a follow-up counseling session to be completed at their second fill. The pharmacy data system notified the pharmacist to offer a second counseling session that reinforced messages from the first session; the pharmacist inquired about the patient’s experience during the first month of treatment and focused on removing any barriers to adherence. On average, the new to therapy conversation lasted 3 to 5 minutes, and follow-up conversations were 1 to 2 minutes in length.
Patients who filled their initial statin prescription and received both face-to-face first fill and second fill counseling sessions that were less than 6 months apart were included in the intervention group. Targeted NTT patients who filled their initial statin prescription during the study period but did not receive any face-to-face counseling were included in the comparison group. Comparison group patients did not receive consultations due to various reasons such as caregivers picking up the prescription, use of drive through prescription pick-up, or did not have time to wait for consultation during busy hours. In addition, to align with the criteria applied to the intervention group, patients in the comparison group were required to have at least two filled prescriptions and the first and second fill had to occur less than 6 months apart.
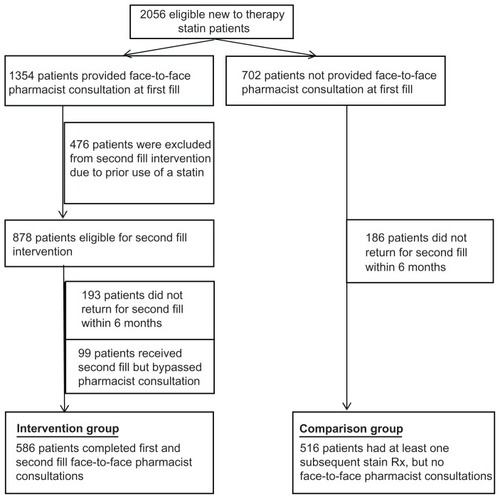
A group of 2056 patients who were NTT for statin medication between September 1, 2010 and October 31, 2010 were followed for 12 months after their initial identification date. Eligibility criteria included NTT patients who filled an initial 30-day quantity of statin medication. There was no quantity restriction for refills; so some patients may have refilled with 90-day quantities. As detailed in , out of 2056 NTT patients, 702 patients did not receive any intervention, while 476 patients received a first fill intervention but were not eligible for a second fill intervention due to prior use of statin medication. After applying inclusion and exclusion criteria, the intervention group consisted of 586 patients and the comparison group included 516 patients. There were no statistically significant differences between the intervention and comparison groups in mean age, age bands, gender distribution, pharmaceutical benefit plan type, or co-pay amounts (). The average income level of patients, as determined by pharmacy trade area estimates, was not significantly different between groups (data not shown). Finally, there was no significant difference between the groups in comorbidities as measured by the number of unique therapeutic classes.
Table 1 Baseline characteristics of study groups
Outcome measures
Adherence was measured using the medication possession ratio (MPR), which was calculated by taking patients’ total days’ supply of statin medications during the observation period and dividing by total days during the observation period.Citation23 Monthly MPR was calculated for an observation period starting with the initial fill and ending at the specified month; measurement continued until month 12. For overlapping prescriptions such as early refills, the start date of the refill was adjusted to the day after the prior prescription was exhausted. Similarly, if the due date of the last prescription was beyond the observational period, the due date of the last prescription was truncated to the end of the observational period. Additionally, a categorical MPR was used to compare the study groups at 365 days. We considered patients with an MPR of 80% or higher as adherent, and patients with an MPR less than 80% were nonadherent. The 80% threshold is commonly used to imply “adherent” in medication adherence research.Citation23
Persistency is the duration in days from the initiation to discontinuation of statin therapy during the follow-up period.Citation23 We measured persistency as the percentage of patients who had any available statin medication at 60, 90, and 120 days using a 15-day permissive gap. We also measured persistency at 365 days using a 60-day permissive gap. Patients were considered discontinued if they did not have a refill within the permissive gap. In a review of the persistency literature, Sikka et al reported that permissive refill gaps range from 15 to 120 days, and there is little direction in the literature to determine the appropriate length of the gap.Citation24 We used the shortest permissive gap in order to measure the early impact of the intervention; it essentially measures how quickly patients return to refill their medications. A larger permissive gap was also used to assess the long-term persistency to medications.
Statistical analysis
The association between patient adherence and pharmacist face-to-face counseling was evaluated with a multivariate linear regression model including covariates of age, gender, number of therapeutic classes, insurance plan type (cash, commercial, government), and prescription co-pay amount measured in USD$10 bands between USD$0 and USD$30, and over USD$30. The regression model was repeated using monthly MPR results from 2 to 12 cumulative months to determine the relationship between the study groups and medication adherence. Student’s t-tests were calculated to determine the statistical significance of differences between unadjusted MPR group means. Chi-square tests were used to determine differences in proportions for categorical MPR and persistency. The P-value for statistical significance was set at α ≤ 0.05. All analyses were conducted using SAS® Software (v 9.2; SAS Institute Inc, Cary, NC).
Results
The unadjusted MPR for the intervention group was significantly greater than the comparison group at every month measured ().
Table 2 Unadjusted medication possession ratio by study group and month
After adjusting for covariates, the regression model also showed that the intervention group had significantly greater MPR than the comparison group at every monthly period measured ( and ). Over time, both groups had decreasing MPR, however, the intervention group declined at a slower rate during most months. At the end of 12 months, the intervention group had an MPR of 61.8% and the comparison group had an MPR of 56.9%; this was an absolute difference of 4.9% and a relative difference of 8.6% (intervention group MPR/comparison group MPR) (P < 0.01).
Figure 2 Adjusted† medication possession ratio (MPR) by study group and month.
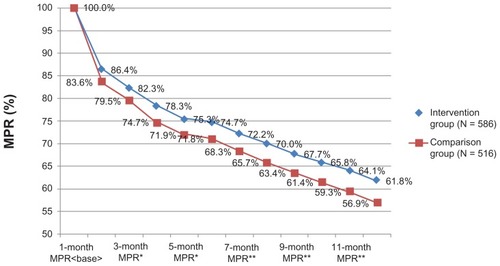
Table 3 Adjusted medication possession ratio (MPR) by study group and monthTable Footnote†
The categorical MPR showed that the intervention group had a significantly higher proportion of adherent patients (MPR ≥ 80%) than the comparison group. At 12 months, 40.9% of the intervention group and 33.7% of the comparison group were adherent. The 7.2% difference between the groups was significant (χ2 = 6.12, P < 0.05).
The intervention group had greater initial persistency to their medication therapy than the comparison group (). Using a 15-day permissive gap, 79.5% of patients in the intervention group and 74.0% of patients in the comparison group were persistent at 60 days (χ2 = 4.66, P < 0.05). Using a 60-day permissive gap, 43.9% of patients in the intervention group and 38.2% of patients in the comparison group were persistent at 365 days (χ2 = 3.65, P = 0.05).
Table 4 Medication persistency between study groups
Discussion
Patients who participated in community pharmacist face-to- face counseling sessions at the beginning of statin therapy demonstrate greater adherence and persistence to their medication therapy than a usual care comparison group. The pharmacists used motivational interviewing techniques in their counseling to help patients get a good start on their new medication. This method allowed patients to articulate their confidence and commitment to their new therapy and to address any perceived barriers to good adherence. In addition, the counseling helped patients learn to fit the medication into their daily routine. The initial gains in adherence, seen immediately after the counseling sessions, continued for 12 months. Over time, both groups had decreasing MPR, however the intervention group declined at a slower rate. The measure of persistency using a relatively short permissive gap of 15 days showed that patients in the intervention group refilled their prescriptions more quickly than the comparison group. However, the short permissive gap was too restrictive to measure the true persistency over time because it removes data for patients who are still on therapy but late to refill their medications. When we used a 60-day permissive gap, the groups were marginally, but significantly different at the end of 12 months. Together these results show that the intervention had positive impact, however additional interventions may be needed, beyond the initial consultations, to reinforce the positive behavior change seen in the intervention group. While not measured in this study, improved adherence to statin therapy should lead to reductions in lipid levels and ultimately reductions in morbidity, mortality, and health care costs.Citation7
These findings are similar to other studies demonstrating the impact of pharmacist interventions to improve medication adherence.Citation19,Citation25,Citation26 Cutrona et al conducted a systematic review of randomized studies of various methods to improve medication adherence to a range of cardiovascular medications.Citation22 They report that 5 out of 6 studies that measured comprehensive pharmacist interventions that included multiple session, blister packaging, and other tools, significantly improved medication adherence between 7%–27%.
The present study measured the impact of two brief counseling sessions on patients new to therapy for statin medications. Additional research is needed to independently validate these findings and determine whether they generalize to other therapeutic classes and chronic conditions. Furthermore, a multi-armed, randomized study design is recommended to compare the effectiveness of various adherence interventions and control for potential biases.
Limitations
This analysis utilized data from a single pharmacy chain and did not include data from other pharmacies. Furthermore, as with all studies using pharmacy claims data and MPR to determine adherence; it is not possible to determine whether the medications were actually taken as prescribed. Patients in the intervention group were counseled by different pharmacists at different stores; therefore, there was some uncontrolled variation in the intervention. Patients essentially self-selected into either the intervention or comparison group, which may have introduced some uncontrolled bias. However, the fact that the demographics and utilization characteristics of both groups are similar provides some assurance that the baseline group differences are minimal. Furthermore, we used a multivariate linear regression model including covariates of age, gender, number of therapeutic classes, insurance plan type, and prescription co-pay amount to minimize potential bias.
Conclusion
Patients who participated in brief face-to-face counseling sessions with a community pharmacist at the beginning of statin therapy demonstrate greater medication adherence and persistency than a comparison group. This brief intervention at the initiation of maintenance drug therapy moderates the high risk of nonadherence and discontinuation; it helps patients establish a routine of daily self-medication and potentially improves their long-term clinical outcomes.
Acknowledgments
The authors wish to acknowledge Janeen DuChane, Nikhil Khandelwal, Elan Rubenstein and Rachel O’Koren for their help developing the manuscript. This study was sponsored by Walgreen Co. All contributors were employees of Walgreen Co and Elan Rubinstein is a consultant to Walgreen Co.
Disclosure
The authors report no financial relationship other than that outlined in the Acknowledgments or other potential conflicts of interest related to the subject of this manuscript. KR, JJ, and MT designed the study methodology; JJ and MT conducted the analysis; MT, JJ, ER, and RO wrote sections of the manuscript; and KR, SE, JD, and ID provided editorial review.
References
- SabatéEAdherence to Long-term Therapies: Evidence for ActionGenevaWorld Health Organization2003 Available from: http://whqlibdoc.who.int/publications/2003/9241545992.pdfAccessed March 1, 2012
- YeawJBennerJSWaltJGSianSSmithDBComparing adherence and persistence across 6 chronic medication classesJ Manag Care Pharm2009159724736
- ThierSLYu-IsenbergKSLeasBFIn chronic disease, nationwide data show poor adherence by patients to medication and by physicians to guidelinesManag Care2008172485218361259
- National Center for Chronic Disease Prevention and Health PromotionChronic Diseases: The Power to Prevent, the Call to ControlNational Center for Chronic Disease Prevention and Health Promotion2009 Available from: http://www.cdc.gov/chronicdisease/resources/publications/AAG/chronic.htmAccessed March 1, 2012
- HoPMRumsfeldJSMasoudiFAEffect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitusArch Intern Med2006166171836184117000939
- HoPMMagidDJMasoudiFAMcClureDLRumsfeldJSAdherence to cardioprotective medications and mortality among patients with diabetes and ischemic heart diseaseBMC Cardiovasc Disord200664817173679
- SokolMCMcGuiganKAVerbruggeRREpsteinRSImpact of medication adherence on hospitalization risk and healthcare costMed Care200543652153015908846
- New England Healthcare InstituteThinking Outside the Pillbox: A System-wide Approach to Improving Patient Medication Adherence for Chronic DiseaseCambridge, MANew England Healthcare Institute2009 Available from: http://www.nehi.net/uploads/full_report/pa_issue_brief__final.pdfAccessed March 1, 2012
- RogerVLGoASLloyd-JonesDMHeart disease and stroke statistics – 2011 update: a report from the American Heart AssociationCirculation20111234e18e20921160056
- KeevilJGCullenMWGangnonRMcBridePESteinJHImplications of cardiac risk and low-density lipoprotein cholesterol distributions in the United States for the diagnosis and treatment of dyslipidemia: data from National Health and Nutrition Examination Survey 1999 to 2002Circulation2007115111363137017353444
- CholesterolTreatmentTrialistsCollaboratorsKearneyPMBlackwellLEfficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysisLancet2008371960711712518191683
- PreissDSattarNLipids, lipid modifying agents and cardiovascular risk: a review of the evidenceClin Endocrinol (Oxf)200970681582819067719
- Krousel-WoodMAMuntnerPIslamTMoriskyDEWebberLSBarriers to and determinants of medication adherence in hypertension management: perspective of the cohort study of medication adherence among older adultsMed Clin North Am200993375376919427503
- OsterbergLBlaschkeTAdherence to MedicationN Engl J Med2005353548749716079372
- ChernewMGibsonTBYu-IsenbergKSokolMCRosenABFendrickAMEffects of increased patient cost sharing on socioeconomic disparities in health careJ Gen Intern Med20082381131113618443882
- PedanAVarastehLSchneeweissSAnalysis of factors associated with statin adherence in a hierarchical model considering physician, pharmacy, patient, and prescription characteristicsJ Manag Care Pharm200713648749617672810
- GelladWFGrenardJMcGlynnEAA Review of Barriers to Medication Adherence: A Framework for Driving Policy OptionsSanta Monica, CARAND Health2009
- NairKVBellettiDADoyleJJUnderstanding barriers to medication adherence in the hypertensive population by evaluating responses to a telephone surveyPatient Prefer Adherence2011519520621573051
- BlumlBMMcKenneyJMCzirakyMJPharmaceutical care services and results in project ImPACT: hyperlipidemiaJ Am Pharm Assoc (Wash)200040215716510730019
- BuntingBASmithBHSutherlandSEThe Asheville Project: clinical and economic outcomes of a community-based long-term medication therapy management program for hypertension and dyslipidemiaJ Am Pharm Assoc20084812331
- FeraTBlumlBMEllisWMDiabetes Ten City Challenge: final economic and clinical resultsJ Am Pharm Assoc2009493383391
- CutronaSLChoudhryNKFischerMAModes of delivery for interventions to improve cardiovascular medication adherence: ReviewAm J Manag Care2010161292994221348564
- CramerJARoyABurrellAMedication compliance and persistence: terminology and definitionsValue Health2008111444718237359
- SikkaRXiaFAubertREEstimating medication persistency using administrative claims dataAm J Manag Care200511744945716044982
- KripalaniSYaoXHaynesRBInterventions to enhance medication adherence in chronic medical conditions: a systematic reviewArch Intern Med2007167654055017389285
- LeeJKGraceKATaylorAJEffect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trialJAMA2006296212563257117101639