Abstract
Background
The Model of Health Care Empowerment (HCE) defines HCE as the process and state of being engaged, informed, collaborative, committed, and tolerant of uncertainty regarding health care. We examined the hypothesized antecedents and clinical outcomes of this model using data from ongoing human immunodeficiency virus (HIV)-related research. The purpose of this paper is to explore whether a new measure of HCE offers direction for understanding patient engagement in HIV medical care. Using data from two ongoing trials of social and behavioral aspects of HIV treatment, we examined preliminary support for hypothesized clinical outcomes and antecedents of HCE in the context of HIV treatment.
Methods
This was a cross-sectional analysis of 12-month data from study 1 (a longitudinal cohort study of male couples in which one or both partners are HIV-seropositive and taking HIV medications) and 6-month data from study 2, a randomized controlled trial of HIV-seropositive persons not on antiretroviral therapy at baseline despite meeting guidelines for treatment. From studies 1 and 2, 254 and 148 participants were included, respectively. Hypothesized antecedents included cultural/social/environmental factors (demographics, HIV-related stigma), personal resources (social problem-solving, treatment knowledge and beliefs, treatment decision-making, shared decision-making, decisional balance, assertive communication, trust in providers, personal knowledge by provider, social support), and intrapersonal factors (depressive symptoms, positive/negative affect, and perceived stress). Hypothesized clinical outcomes of HCE included primary care appointment attendance, antiretroviral therapy use, adherence self-efficacy, medication adherence, CD4+ cell count, and HIV viral load.
Results
Although there was no association observed between HCE and HIV viral load and CD4+ cell count, there were significant positive associations of HCE scores with likelihood of reporting a recent primary care visit, greater treatment adherence self-efficacy, and higher adherence to antiretroviral therapy. Hypothesized antecedents of HCE included higher beliefs in the necessity of treatment and positive provider relationships.
Background
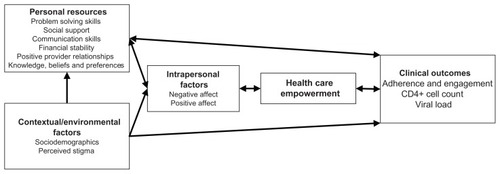
The model of health care empowerment (HCE) was recently proposed as a structure for understanding and intervening in how people perceive their participation in health care.Citation1 The construct of HCE, defined as the state and process of being engaged, informed, committed, tolerant of uncertainty, and collaborative in one’s interactions with health care, offers direction for addressing differences in health care service utilization and outcomes across a wide range of populations and illnesses. The model hypothesizes that HCE is influenced through a dynamic interplay of contextual/environmental factors (such as age, race, and stigma), personal resources (such as finances, adaptive beliefs about treatment, problem-solving skills, and trust in providers), and intrapersonal processes and states (such as depressive symptoms and positive affect).
The treatment of human immunodeficiency virus (HIV) and acquired immune deficiency syndrome (AIDS) is one example of a medical context that offers a rich opportunity to illustrate the potential applicability of HCE. HIV disease in the US and other developed countries is a heavily stigmatized condition that disproportionately affects populations who are economically and socially marginalized, including members of racial and ethnic minority groups, gay and transgender persons, and people with substance abuse histories.Citation2–Citation4 Treatment guidelines and antiretroviral therapy options are rapidly changing, and treatments have been historically difficult to tolerate, yet require vigilant adherence to prevent development of viral resistance, hastening of disease progression, and increased likelihood of the transmission of drug-resistant HIV to others.Citation5–Citation7
The purpose of this paper is to present preliminary support for the construct of HCE in the context of HIV treatment, with a particular emphasis on evaluating whether scores on a new measure of HCE are associated with hypothesized antecedents and clinical outcomes. Data from two ongoing studies of social and behavioral aspects of HIV treatment offer empirical evidence and direction for future indepth studies of HCE in HIV and other illnesses in which patient involvement in ongoing treatment is critical yet variable.
Materials and methods
A new measure of HCE was included in assessment batteries for two ongoing studies of social and behavioral factors of HIV treatment. Study 1 is a longitudinal cohort study of male couples in which one or both partners are HIV-seropositive and taking antiretroviral therapy. Couples are interviewed every 6 months for 2 years. HCE was assessed at the 12-month assessment wave as part of a comprehensive survey and blood was drawn for CD4+ cell count and HIV viral load. Study 2 is a randomized controlled trial of HIV-seropositive persons who were not on antiretroviral therapy at baseline despite meeting HIV treatment guidelines on CD4+ cell count cutoff for initiation of antiretroviral therapy (ie, ≤500 cells/mm3).Citation8 HCE was assessed at the 6-month assessment wave as part of a comprehensive survey and blood drawn for CD4+ cell count and HIV viral load.
Participants and procedures
Recruitment for both studies included outreach to clinics and agencies, and posting of advertisements and flyers in the San Francisco Bay area community. HIV-positive serostatus was verified by HIV antibody testing or provision of documentation by potential participants, and antiretroviral therapy regimens were verified by examination of prescribed medication vials or official medication lists from the dispensing pharmacy. Participants provided written informed consent and all procedures were approved by the local institutional review board at the University of California, San Francisco. Combinations of audio computer-assisted self-interviewing and computer-assisted personal interviewing were used to optimize self-report, to minimize data collection errors, and to facilitate efficient data management.Citation9 Screening, data collection, and phlebotomy procedures occurred in private areas of research facilities and all participants were compensated for their involvement.
Measures
Participants in both studies were asked about general demographic information and HIV treatment history, including time since HIV diagnosis and past medical treatment details. The following variables were assessed in at least one of the two studies and are organized according to their hypothesized role as informed by the HCE model ().
Health care empowerment
The 27-item measure of HCE was developed specifically by the investigators to assess the five hypothesized domains of health care empowerment: informed (five items, sample item “I am knowledgeable about my health condition(s)”); committed (six items, sample item “I am determined to work hard to get the most out of my health care”); collaborative (six items, sample item “I think of my health care providers as my partners in dealing with my health condition[s]”); engaged (five items, sample item “Others would probably say that I am a very engaged and active patient”); and tolerant of uncertainty (five items, sample item “I have learned to live with the uncertainty of my health condition”). Responses include five choices ranging from “strongly disagree” to “strongly agree” and a global score is created by summing responses to all individual items. Cronbach’s alphas of 0.94 and 0.96 were calculated for study 1 and study 2, respectively, demonstrating acceptable internal reliability, and 6-month test-reliability estimates of 0.73 were available for study 1. This is the first publication to use this new measure.
Hypothesized clinical outcomes of HCE
To examine hypothesized proximal and downstream clinical consequences of HCE, the following data were analyzed (study 1 and/or study 2 indicate in which study the measure was administered), and reported alphas are for the current samples.
Primary care appointment attendance (study 1 and study 2): failure to consistently attend clinic appointments has been linked to poor virological control.Citation10,Citation11 We documented the time since most recent primary care visit and, for consistency between the two studies, classified all participants as having a primary care visit within the prior 3 months or not.
Antiretroviral therapy use (study 2): whether participants had initiated antiretroviral therapy during the follow-up period was documented for study 2 participants, all of whom met criteria for antiretroviral therapy initiation per HIV treatment guidelinesCitation8 at study enrollment.
Adherence self-efficacy (study 1 and study 2): adherence self-efficacy, or confidence in one’s ability to comply with a treatment plan, has been consistently linked to medication adherence over time.Citation12,Citation13 The HIV- Adherence Self Efficacy Scale (HIV-ASES) assesses patient confidence in carrying out health-related behaviors (eg, asking physician questions, keeping appointments, adhering to medication).Citation14 This measure includes two subscales, ie, integration and perseverance; α = 0.91 and 0.78, respectively, for study 1, and α = 0.91 and 0.65, respectively, for study 2.
Medication adherence (study 1 and study 2): adherence to antiretroviral medications was assessed using two well validated measures of self-report. The adherence measure developed to assess adherence in the AIDS Clinical Trials GroupCitation15 solicits detailed information about self-reported adherence over the previous 3 days. Adherence scores on this scale have been correlated with viral load.Citation15,Citation16 Second, a visual analog scale was administered,Citation17 which assesses 30-day adherence reporting separately for each drug along a continuum anchored by “0%” to “100%.” This measure has been shown to be correlated with other adherence measures, such as electronic medication monitors.Citation18,Citation19 The 3-day adherence measure was dichotomized as 100% versus <100% adherence and the 30-day visual analog scale adherence is reported as a continuous variable.
CD4+ cell count and viral load (study 1 and study 2): HIV viral load was determined using the COBAS® AmpliPrep/COBAS® TaqMan® HIV test kit (Roche Molecular Systems Inc, Pleasanton, CA), which has a threshold for undetectability ≤20 copies/mL. A detectable viral load indicates incomplete viral suppression, or inadequately controlled HIV infection. CD4+ cell count provides a gauge of immune functioning, with lower counts typically indicating longer infection and/or greater immune system deterioration. In healthy persons, the normal range of CD4+ cell count is 500–1500 cells/mm3 of blood, and current HIV treatment guidelines recommend offering antiretroviral therapy to all HIV-seropositive persons with a CD4+ cell count below 500.Citation8
Hypothesized antecedents of HCE
HCE is hypothesized to be related to three categories of variables, ie, cultural/social/environmental factors, personal resources (both material and psychological), and intrapersonal factors.
Cultural/social/environmental factors
Demographics (study 1 and study 2): including age, gender, race, and ethnicity were assessed via interview. HIV-related stigma (study 2) is believed to be a strong driver of HIV risk and treatment outcomes, and is often cited when discussing the sources of HIV-related disparities.Citation20–Citation27 HIV stigma (study 2) was assessed using the four-item distancing subscale of a stigma scale developed by Sowell, which assesses perceived distancing from others due to HIV-positive status (α = 0.90).Citation26,Citation28
Personal resources
Social problem-solving (study 1): investigated using the Social Problem-Solving Inventory-Revised questionnaire, Citation29,Citation30 a 25-item, self-administered questionnaire that assesses problem orientation (negative and positive), problem-solving styles (avoidant and impulsive/careless), and rational problem-solving skills. The measure has been widely used, has been predictive of health and risk behaviors,Citation31 and has shown meaningful relationships with antiretroviral therapy adherence in our prior work.Citation32 As before, we combined the positive problem-solving scores into a constructive problem-solving scale (α = 0.82) and the negative problem-solving scales into a dysfunctional problem-solving scale (α = 0.85).
Treatment knowledge (study 2): a 16-item HIV treatment knowledge assessment was administered, with higher scores reflecting more accurate knowledge of aspects of treatment such as adherence, side effects, and drug resistance (α = 0.83).Citation33
Treatment beliefs (study 1 and study 2): assessed using the HIV version of the Beliefs About Medications Questionnaire,Citation34 which includes subscales of treatment necessity (α = 0.84 and 0.82) and treatment concerns (α = 0.66 and 0.72).
Preference for treatment decision-making (study 1): The 6-item Autonomy Preference Index specifically assesses patient preferences for shared medical decision-making (α = 0.67), with good evidence of concurrent and criterion validity.Citation35 Higher scores reflect stronger preferences for patient involvement in treatment decision-making.
Opportunity for shared decision-making (study 1): The 3-item Decision-Making Opportunity ScaleCitation36 assesses how often a provider discusses the pros and cons of each medical care choice, elicits statements of patient preference, and takes patient preference into account when making treatment decisions (α = 0.85). Higher scores indicate a patient’s perception of greater opportunity for involvement, as enabled by the provider.
Decisional balance (study 1 and study 2): A single item by Beach et alCitation37 assessing decisional balance preference was administered, ie, “Which best describes how decisions about your HIV treatment are made during your visits with your HIV care provider?” Response choices are 0 (“Provider makes most or all of the decisions”) 1 (“Provider and I make the decisions together”), and 2 (“I make most or all of the decisions”). Higher scores indicate a patient’s perception of greater involvement in treatment decisions.
Assertive communication (study 2): assessed with the 5-item Patient Communication Index scale of the Patient Reactions Questionnaire, with higher scores indicating greater difficulty with assertive communication with providers (α = 0.92).Citation38
Positive provider interactions (study 2): The Positive Patient-Provider Interaction scaleCitation39 assesses the degree to which recent patient-provider interactions were seen as constructive by patients (α = 0.95).
Trust in providers (study 2): The 11-item Trust in Physician ScaleCitation40 assesses patients’ interpersonal trust in their provider and has been used in the context of HIV treatment (α = 0.74).Citation41
Personal knowledge by provider (study 1 and study 2): A single item, ie, “My provider really knows me as a person.” In previous work, higher agreement with this statement was linked with greater antiretroviral therapy uptake and adherence.Citation37
Social support (study 2): The Social Provisions ScaleCitation42 assesses level, type, and perceived satisfaction with social support from one’s social network. For the current analysis, we used the overall score, with higher values representing greater perceived social support (α = 0.91).
Intrapersonal factors
Depressive symptoms (study 1 and study 2): the Center for Epidemiologic Studies Depression Scale (CES-D)Citation43 was administered to measure depressed mood in the past week. The CES-D consists of 20 items rated on a 4-point scale according to how frequently they were experienced in the previous week (α = 0.92 and 0.92).
Positive and negative affect (study 1): We administered the Differential Emotions ScaleCitation44,Citation45 which assesses 60 emotions of varied valence rated on a 5-point scale according to how frequently they were experienced in the past week. The scale was scored for total positive (α = 0.90) and negative affect (α = 0.86).
Perceived stress (study 2): Cohen’s Perceived Stress ScaleCitation46 assesses the degree to which a person describes situations in the prior month as stressful. A total score is provided by summing ratings on a 5-point scale (α = 0.86), with higher scores indicating greater reports of distress.
Data analysis
The reported analyses were exploratory and guided by the model of HCE.Citation1 The first analytic goal was to explore unadjusted associations of HCE with hypothesized clinical outcomes of HCE, eg, HIV biomarker measures of adherence as well as self-reported subjective measures of adherence self-efficacy. These include proximal and distal or downstream indicators of active, empowered engagement in medical treatment. The second goal was to use existing data to explore bivariate and multivariate associations of hypothesized antecedents of HCE. For each study, initial analyses described frequencies for categorical variables and measures of central tendency (median) and variability (standard deviations) for continuous variables. Bivariate analyses correlated HCE scale scores with clinical biomarker and self-report data, contextual/environmental factors, personal resource factors, and intrapersonal factors. Contextual/environmental, personal, and intrapersonal factors for which bivariate associations with HCE were significant at P < 0.25 were included in multivariable regression models explaining HCE in each study.Citation47 Beginning with the least significant explanatory variable, the hypothesized contextual/environmental, personal, and intrapersonal antecedents were removed until all remaining correlates in adjusted analyses were significant at P < 0.05 (ie, backward elimination).Citation48 SAS version 9 (SAS Institute Inc, Cary, NC) was used to generate descriptive statistics; Mplus version 6 (Muthén and Muthén, Los Angeles, CA) was used to generate bivariate and adjusted analysis results via full information maximum likelihood, which makes use of all available information in the data to obtain optimal parameter estimates and standard errors when one or more cases have incomplete data.Citation49 This method prevents different sample sizes being used for the backward elimination procedure for multivariable regression analyses due to some participants missing information on one or more measures. Bivariate (ie, unadjusted) correlations were reported using the r statistic. Adjusted coefficients from multivariable regression models were reported using the standardized regression coefficient, β, to quantify the amount of change per standard deviation in HCE as a function of each explanatory variable in the context of other significant correlates of HCE.
Results
Sample characteristics for participants in both studies are provided in . Study 2 participants included a greater proportion of African Americans, reported lower income and education, and were more likely to report histories of homelessness and injection drug use. Due to differences in study eligibility criteria, study 2 included more women and heterosexuals, and study 1 participants were more likely to have higher CD4+ cell counts and an undetectable viral load.
Table 1 Participant characteristics
Hypothesized clinical outcomes of HCE
Examination of hypothesized clinical outcomes of HCE in study 1 resulted in significant positive associations of HCE scores with likelihood of reporting a primary care visit in the previous 3 months (r = 0.29, P = 0.001), greater adherence self-efficacy integration (r = 0.39, P < 0.001) and perseverance scores (r = 0.33, P < 0.001), higher 3-day antiretroviral therapy adherence (r = 0.21, P = 0.004), and higher 30-day antiretroviral therapy adherence (r = 0.23, P = 0.001). In study 2, there was a similar pattern, in which higher HCE scores were reported by those reporting primary care visits in the prior 3 months (r = 0.25, P = 0.003), those with higher adherence self-efficacy integration scores (r = 0.26, P < 0.001), and those with higher 30-day antiretroviral therapy adherence reports (r = 0.27, P = 0.002). Unlike study 1, there was no association between HCE scores and adherence self-efficacy perseverance and 3-day antiretroviral therapy adherence. HCE was not associated with CD4 or viral load in either sample (see ).
Table 2 Hypothesized clinical correlates of health care empowerment
Hypothesized antecedents of HCE
Although there was a positive bivariate relationship between age and higher HCE scores in study 1 (r = 0.15, P = 0.01), none of the contextual/social/background variables were significant in the adjusted models for either study 1 or study 2 (see and ). In the adjusted model for study 1, several personal resource factors were associated with higher HCE, including higher constructive problem solving (β = 0.17, P = 0.01) and lower dysfunctional problem solving (β = −0.28, P = 0.01), higher beliefs in the necessity of treatment (β = 0.14, P = 0.02), higher reports of involvement in treatment decision-making (β = 0.19, P < 0.001), higher scores on the Autonomy Preference Index (β = 0.22, P < 0.001), and perceptions that the provider knows the patient as a person (β = 0.27, P < 0.001). In study 2, adjusted analyses revealed a positive association with beliefs in treatment necessity (β = 0.27, P = 0.01) and perceptions of recent positive provider interactions (β = 0.25, P = 0.004), and an association of lower HCE with greater difficulty with assertive communication with providers (β = −0.31, P < 0.001).
Table 3 Hypothesized antecedents of health care empowerment (study 1, n = 254)
Table 4 Hypothesized antecedents of health care empowerment, study 2 (n = 148)
In study 1 adjusted analyses, higher HCE scores were associated with lower reported symptoms of depression (β = 0.25, P = 0.001) and higher reports of positive emotion (β = 0.28, P < 0.001). Depression and perceived stress were not associated with HCE scores in study 2.
Discussion
Findings from the two studies provide support for the model of health care empowerment in the context of HIV treatment. Consistent with the hypothesized role of HCE, greater patient empowerment was associated with reports of active participation in HIV care and perceived confidence in ability to adhere to treatment and self-reports of recent medication adherence. The association between HCE and laboratory markers of clinical status did not reach statistical significance, but this may be due to a restricted range on these variables, limited sample sizes, and the specific eligibility criteria regarding antiretroviral therapy use in the two studies.
The resulting correlates of HCE support a central role for knowledge, skills, provider relationships, and psychological well being in association with patient empowerment. From a research perspective, these findings offer direction for future in-depth studies of the role of empowerment. From a clinical perspective, findings suggest that providers who make efforts to get to know their patients beyond their clinical presentation, who strive to respect and foster patient autonomy, and who make concrete efforts to involve patients in decision-making may be effective in fostering health care empowerment in their patients. Interventions designed to improve patient skills in problem solving and assertive communication with providers edify treatment knowledge and reinforce a solid understanding for the need for prescribed treatments, and detect and treat depressive symptoms while fostering positive affect may promote greater patient empowerment and thus more productive engagement in care. Such improvements in empowerment may then facilitate better treatment utilization and adherence to antiretroviral therapy, resulting in more effective virological control and decreased HIV transmission to others.Citation50,Citation51
The pattern of hypothesized antecedents of HCE suggests no direct statistical association of contextual factors with empowerment scores, including stigma. Consistent with the model of HCE, it may be that these factors operate indirectly on empowerment by affecting other elements in the model, such as personal resources (eg, treatment knowledge) and intrapersonal factors (eg, depression). It is also likely that the samples recruited were not representative of the larger population on such measures as HIV stigma; those who are willing to enroll in ongoing research related to HIV might not be as sensitive or affected by HIV stigma as others who chose not to enroll. The limited sample sizes in this exploratory work precluded larger model testing through such procedures as structural equation modeling which could test simultaneous moderator and mediator effects.
Although generally consistent results were found between the two studies and the results were in the expected directions, the findings should be generalized with caution. The studies used convenience samples from one geographic area and relied primarily on self-reported measures, such as appointment attendance and medication adherence. Data are cross-sectional and thus cannot be used to determine causality. The 3-month time frame for the primary care visit variable may be too restrictive, because patients in stable clinical care may have less frequent but regular provider visits. The relatively modest sample sizes and limited variability of gender, age, race, and ethnicity preclude specific analysis of subgroups, and findings should thus be considered preliminary. Nonetheless, the pattern of findings across the two studies offers encouragement for further investigation of the model of health care empowerment.
In summary, our results reveal a rough map of the terrain of health care empowerment. Future investigations are needed to refine the measurement of the construct, to form and test new hypotheses, and to evaluate the fit of the construct and the model of health care empowerment in other illness settings and across cultures.
Acknowledgments
This publication was supported by National Institutes of Health/National Institute of Mental Health grant numbers R01MH0790700, K24MH087220, K08 MH085566, and F32MH086323, National Institutes of Health/National Institute of Nursing Research grant number R01NR011087, and NIH/NCRR UCSF-CTSI grant number UL1RR024131.
Disclosure
Portions of the findings of this research were presented by the principal author at the 6th International Conference on HIV Treatment and Prevention Adherence on May 22–24, 2011, in Miami, FL, the Psychology Colloquium, University of Alabama at Birmingham, November 2, 2011, and the European Society of Patient Compliance, Adherence, and Persistence on November 18–19, 2011, Utrecht, The Netherlands. The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
References
- JohnsonMOThe shifting landscape of health care: Toward a model of health care empowermentAm J Public Health20111012264270
- OramasionwuCUBrownCMRyanLLawsonKAHunterJMFreiCRHIV/AIDS disparities: the mounting epidemic plaguing US blacksJ Natl Med Assoc2009101121196120420070007
- OramasionwuCUBrownCMLawsonKARyanLFreiCREvaluating HIV/AIDS disparities for blacks in the United States: a review of antiretroviral and mortality studiesJ Natl Med Assoc2009101121221122920070010
- GiamiALe BailJHIV infection and STI in the trans population: a critical reviewRev Epidemiol Sante Publique2011594259268 French21767925
- VolberdingPDeeksSGAntiretroviral therapy and management of HIV infectionLancet20103769734496220609987
- McNeilDGEarly HIV therapy sharply curbs transmissionNew York Times5122011
- GardnerEMMcLeesMPSteinerJFDel RioCBurmanWJThe spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infectionClin Infect Dis201152679380021367734
- Department of Health and Human ServicesGuidelines for the Use of Antiretroviral Agents in HIV-infected Adults and AdolescentsWashington, DCDepartment of Health and Human Services and the Henry J Kaiser Family Foundation2011
- TurnerCFKuLRogersSMLindbergLDPleckJHSonensteinFLAdolescent sexual behavior, drug use, and violence: Increased reporting with computer survey technologyScience199828053658678739572724
- GiordanoTPGiffordALWhiteACJrRetention in care: a challenge to survival with HIV infectionClin Infect Dis200744111493149917479948
- MugaveroMJAmicoKRWestfallAOEarly retention in HIV care and viral load suppression: implications for a test and treat approach to HIV preventionJ Acquir Immune Defic Syndr2012591869321937921
- JohnsonMOCatzSLRemienRHTheory guided, empirically supported avenues for intervention on HIV medication nonadherence: Findings from the Healthy Living ProjectAIDS Patient Care STDS2003171264565614746658
- SeveliusJMCarricoAJohnsonMOAntiretroviral therapy adherence among transgender women living with HIVJ Assoc Nurses AIDS Care201021325626420347342
- JohnsonMONeilandsTBDilworthSMorinSFRemienRHChesneyMAThe role of self-efficacy in HIV treatment adherence: validation of the HIV Treatment Adherence Self-Efficacy Scale (HIV-ASES)J Behav Med200730535937017588200
- ChesneyMAIckovicsJRChambersDBSelf-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee and Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG)AIDS Care200012325526610928201
- ChesneyMAIckovicsJAdherence to combination therapy in AIDS clinical trialsPaper presented at the Annual Meeting of the AIDS Clinical Trials GroupWashington DCJuly 19–22, 1997
- WalshJCPozniakALNelsonMRMandaliaSGazzardBGVirologic rebound on HAART in the context of low treatment adherence is associated with a low prevalence of antiretroviral drug resistanceJ Acquir Immune Defic Syndr200230327828712131564
- WalshJCMandaliaSGazzardBGResponses to a 1 month self-report on adherence to antiretroviral therapy are consistent with electronic data and virological treatment outcomeAIDS200216226927711807312
- OyugiJHByakika-TusiimeJCharleboisEDMultiple validated measures of adherence indicate high levels of adherence to generic HIV antiretroviral therapy in a resource-limited settingJ Acquir Immune Defic Syndr20043651100110215247564
- HerekGMGluntEKAn epidemic of stigma: public reactions to AIDSAm Psychol198843118868913063145
- BuntingSMSources of stigma associated with women with HIVANS Adv Nurs Sci199619264738939289
- ChesneyMASmithAWCritical delays in HIV testing and care: The potential role of stigmaAm Behav Sci199942711621174
- DemarcoFJCoping with the Stigma of AIDS: An Investigation of the Effects of Shame, Stress, Control and Coping on Depression in HIV-Positive and -Negative Gay Men (Immune Deficiency, Sexual Orientation)East Lansing, MIMichigan State University1999
- TimberlakeSSigurdsonJHIV, stigma, and rates of infection: a human rights and public health imperativePLoS Med200741e5217411320
- RaoDKekwaletsweTCHosekSMartinezJRodriguezFStigma and social barriers to medication adherence with urban youth living with HIVAIDS Care2007191283317129855
- EmletCAMeasuring stigma in older and younger adults with HIV/AIDS: an analysis of an HIV stigma scale and initial exploration of subscalesRes Soc Work Pract2005154291300
- ReisnerSLMimiagaMJSkeerMPerkovichBJohnsonCVSafrenSAA review of HIV antiretroviral adherence and intervention studies among HIV-infected youthTop HIV Med2009171142519270345
- SowellRLLowensteinAMoneyhamLDemiAMizunoYSealsBFResources, stigma, and patterns of disclosure in rural women with HIV infectionPublic Health Nurs19971453023129342922
- D’ZurillaTJNezuAMDevelopment and preliminary evaluation of the social problem-solving inventoryPsychol Assess199022156163
- Maydeu-OlivaresAD’ZurillaTJA factor-analytic study of the social problem-solving inventory: an integration of theory and dataCognit Ther Res1996202115133
- ElliottTRJohnsonMOJacksonRSocial problem solving and health behaviors of undergraduate studentsJ Coll Stud Dev19973812431
- JohnsonMOElliottTRNeilandsTBMorinSFChesneyMAA social problem solving model of adherence to HIV medicationsHealth Psychol200625335536316719607
- BalfourLKowalJTascaGADevelopment and psychometric validation of the HIV Treatment Knowledge ScaleAIDS Care20071991141114818058398
- HorneRWeinmanJHankinsMThe Beliefs about Medicines Questionnaire: The development and evaluation of a new method for assessing the cognitive representation of medicationPsychol Health1999141124
- EndeJKazisLAshAMoskowitzMAMeasuring patients’ desire for autonomy: decision making and information-seeking preferences among medical patientsJ Gen Intern Med19894123302644407
- HarveyRMKazisLLeeAFDecision-making preference and opportunity in VA ambulatory care patients: association with patient satisfactionRes Nurs Health199922139489928962
- BeachMCDugganPSMooreRDIs patients’ preferred involvement in health decisions related to outcomes for patients with HIV?J Gen Intern Med20072281119112417514382
- GalassiJPSchanbergRWareWBThe patient reactions assessment: A brief measure of the quality of the patient-provider medical relationshipPsychol Assess199243346351
- JohnsonMOChesneyMGoldsteinRBPositive provider interactions, adherence self-efficacy, and adherence to antiretroviral medications among HIV infected adults: A mediation modelAIDS Patient Care STDS200620425826816623624
- AndersonLADedrickRFDevelopment of the trust in physician scale: a measure to assess interpersonal trust in patient-physician relationshipsPsychol Rep1990673 Pt 2109111002084735
- AlticeFLMostashariFFriedlandGHTrust and the acceptance of and adherence to antiretroviral therapyJ Acquir Immune Defic Syndr2001281475811579277
- CutronaCERatings of social support by adolescents and adult informants: Degree of correspondence and prediction of depressive symptomsJ Pers Soc Psychol19895747237302795439
- RadloffLSThe CES-D scale: A self-report depression scale for research in the general populationAppl Psychol Meas19771385401
- IzardCEHuman EmotionsNew York, NYPlenum Press1977
- IzardCEDoughertyFBloxomBMKotschNEThe Differential Emotions Scale: A Method of Measuring the Subjective Experience of Discrete EmotionsNashville, TNVanderbilt University1974
- CohenSKamarckTMermelsteinRA global measure of perceived stressJ Health Soc Behav19832443853966668417
- HosmerDWLemeshowSApplied Logistic RegressionNew York, NYJohn Wiley and Sons2000
- VittinghoffEGliddenDVShiboskiSMcCullochCERegression Methods in BiostatisticsNew York, NYSpringer2005
- LittleRJARubinDBStatistical Analysis with Missing DataNew York, NYJohn Wiley and Sons2002
- CohenMSChenYQMcCauleyMPrevention of HIV-1 infection with early antiretroviral therapyN Engl J Med2011365649350521767103
- DonnellDBaetenJMKiarieJHeterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort analysisLancet201037597312092209820537376