Abstract
Purpose
Medication non-adherence is a major public health issue. Recent evidence suggests that depression, inadequate social support, and lower levels of self-efficacy are associated with poor medication adherence. However, the mechanism underlying the association among depression, social support, self-efficacy and medication adherence is unclear. This study aims to examine the mediating role of social support and self-efficacy between depression and medication adherence in older patients with coronary heart disease.
Patients and Methods
Data were collected from 238 hospitalized older patients with coronary heart disease. Depression, social support, self-efficacy, and medication adherence were assessed using structured questionnaires. A serial multiple mediation model was tested using the PROCESS macro for SPSS.
Results
A total of 238 older patients with CHD with a mean age of 70.5 years were involved in this cross-sectional study. Depression was negatively correlated with medication adherence in older patients with coronary heart disease. Social support and self-efficacy were positively associated with medication adherence, and fully mediated the relationship between depression and medication adherence. Three mediation paths were included in the model: (a) social support, (b) chain combination of social support and self-efficacy, and (c) self-efficacy.
Conclusion
Social support and self-efficacy explain the association of depression and medication adherence in older CHD patients and may be the keys target for enhanced intervention to improve medication adherence in older CHD patients with depression.
Introduction
Coronary heart disease (CHD) is the main cause of death worldwide, accounting for more than eight million deaths globally each year.Citation1 It is reported that approximately 85% of people aged 65 or older die as a consequence of CHD.Citation2 As a common chronic disease, CHD can lead to poor health-related quality of lifeCitation3,Citation4 and increase healthcare costs.Citation5 As a result of lifestyle changing and an aging population, it is estimated that the number of people with CHD will increase from 8.1 to 22.6 million a year by 2030 in China.Citation6 Evidence-based medication therapy is used as the primary treatment strategy for patients with CHDCitation4 and the treatment is recommended to continue for the rest of their life. Medication adherence, defined as taking medication as prescribed over time, is essential for patients with CHD to generate optimal clinical outcomes, eg, low all-cause mortality, low risk of cardiovascular rehospitalization, and high quality of life.Citation4,Citation7 Nevertheless, medication non-adherence is common and has become a serious public health issue owing to the fact that more than half of older patients with CHD do not take their medication as prescribed.Citation8,Citation9 Evidence has revealed that medication non-adherence is associated with adverse clinical outcomes and increased healthcare costs.Citation10,Citation11
CHD patients with depression are less likely to adhere, at least in some aspects, to treatment regimens such as medication, exercise, and cardiac rehabilitation.Citation12,Citation13 Evidence suggests that depressive symptoms may contribute to poor medication adherence in CHD patients.Citation14,Citation15 Depression is prevalent in patients with CHD, with up to 51% of patients affectedCitation16 and over one-third of whom severely affected;Citation17 thus it is imperative to explore effective measures to improve medication adherence among CHD patients with depression.
Medication adherence can be enhanced through support from family members, community, and friends, as well as other social services.Citation18 Cohen et alCitation19 define social support as “the social resources that individuals perceive to be available or that are actually provided to them by nonprofessionals in the context of both formal support groups and informal helping relationships”. Xiao et alCitation20 propose that individuals’ support utilization should be included in social support. Individuals’ attitude toward support utilization varies, for example, some people might be offered the support, but refuse to take it. With the increase of age, the need of CHD patients for social support increases over time.Citation21 Findings from recent studies illustrate that social support can promote adherence to health behaviors, which is significantly associated with improved medication adherence.Citation22–Citation24
On the other side, evidence shows that self-efficacy may play an important role in adherence to medication.Citation14,Citation25,Citation26 Medication self-efficacy is generally defined as the belief or confidence in one’s ability to persist with taking medication for desired outcomes, and it has been demonstrated to be a strong predictor of health-promoting behaviors and health-related outcomes in patients with chronic disease.Citation27 Previous studies found that CHD patients with lower self-efficacy might show a poor medication adherence.Citation14,Citation28 Polsook et alCitation29 developed a self-efficacy enhancement program (SEP) based on Bandura’s self-efficacy components and implemented the SEP in patients with acute myocardial infarction, and found that SEP was significantly effective in improving medication adherence.
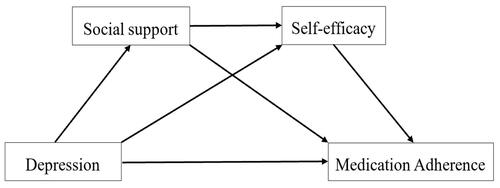
In summary, existing literature demonstrates that depression, social support, and self-efficacy are significantly associated with medication adherence among patients with CHD.Citation14,Citation23,Citation28 Self-efficacy partially mediates the relationship between depression and medication adherence,Citation30,Citation31 and social support also mediates the association between the two.Citation23 In addition, self-efficacy totally mediates the association of social support with treatment adherence, after adjusted for demographic and medical covariates.Citation32 However, limited information is available concerning the mechanism underlying the relationships among the three variables and medication adherence in CHD patients. Clarifying this mechanism will contribute to healthcare professionals to develop targeted interventions to improve medication adherence in older patients with CHD. Therefore, this study is aimed to examine the multiple mediating role of social support and self-efficacy between depression and medication adherence in older patients with CHD. The hypothesized mediator model is shown in .
Patients and Methods
Participants
This is a cross-sectional study. Participants was recruited from 8 cardiovascular units in four tertiary hospitals (each with >500 inpatient beds) in Baoding, a city in northern China. The inclusion criteria were as follows: (1) diagnosis as CHD by a physician, (2) age ≥ 60 years old, and (3) having history of cardiovascular medication use. Participants were excluded if they had (1) a cognitive disorder, or (2) cancer, or (3) were classified as having New York Heart Association class IV heart failure. The minimum number of patients was 178 based on a medium effect size of 0.15, α of 0.05 and a power of 0.90 (using G*power 3.1 version).Citation33 Considering 20% missing rate, a sample size of 214 was required in this study. A convenient sample of 238 participants met the sample size requirement for the study.
Instruments
Socio-Demographic and Clinical Characteristics
The socio-demographic and clinical data include age, gender, marital status, education attained, monthly income, family history of CHD, co-morbidity and duration of CHD. Data were reviewed from hospital medical records by three trained research assistants.
Depression
The 9-item Patient Health Questionnaire (PHQ-9) was used to assess depression. This scale consists of one dimension and nine items.Citation34 Each item is scored from 0 (not at all) to 3 (nearly every day). The total scores range from 0 to 27. Higher total scores correlate with more severe depression. Scores are categorized as follows: none (0–4), mild (5–9), moderate (10–14) and severe depression (≥15).Citation35 The scale has good validity and reliability (with Cronbach’s alpha coefficient of 0.86), and is widely used in China.Citation36 The Cronbach’s alpha coefficient was 0.836 in our study.
Social Support
Social support was measured using the Social Support Rating Scale (SSRS) developed by Xiao.Citation20 It consists of ten items that form three subscales: objective support (three items), perceived support (four items), and support utilization (three items). The total scores for SSRS range from 12 to 66. A higher score reflects better social support. Scores are categorized as follows: low social support (12–22), medium social support (23–44), and high social support (45–66). The SSRS has been widely used in China and has demonstrated good reliability and validity.Citation37 The internal consistency coefficient for this scale was 0.829 in this study.
Self-Efficacy
Self-efficacy for medication adherence was measured using the Self-Efficacy for Appropriate Medication Use Scale (SEAMS), developed by Risser et al.Citation38 This scale contains two dimensions (thirteen items): self-efficacy for taking medications under difficult circumstances (eight items), and self-efficacy for continuing to take medications when circumstances surrounding medication-taking are uncertain (five items). Each question is assigned points from 1 to 3 (1=not confident, 2=somewhat confident, and 3=very confident). The sum of the 13 items ranges from 13–39. Higher total scores indicate better self-efficacy for medication adherence. The Chinese version of SEAMS was translated by Dong et al (Cronbach’s alpha coefficient of 0.915)Citation39 and has demonstrated good internal consistency, reliability, and validity in CHD patients.Citation40 In this study, the Cronbach’s alpha coefficient was 0.913.
Medication Adherence
The medication adherence of CHD patients was measured by the medication adherence questionnaire for coronary heart disease developed by the researchers’ team based on Chinese cardiovascular disease rehabilitation/Secondary prevention guidelines (2015 Edition).Citation41,Citation42 The questionnaire includes major elements related to medication adherence, such as “schedule”, “dosage”, “frequency”, “type”, “regular review” and “medication adjustment”, and contains six items, each measuring a specific medication-related behavior (eg, “How often do you comply with the medication frequency as prescribed?” “How often do you comply with the medication dosage as prescribed?” “How often do you comply with the medication schedule as prescribed?” “How often do you never interruption of taking medication as prescribed?” “How often do you take medication as prescribed without adding or removing medication?” “How often do you review on time and adjust or continue to take medication as prescribed?”). The items are scored on a rating scale from 0 (Never) to 3 (Always). The total scores range from 0 to 18, with higher scores correlating to better medication adherence. The Cronbach alpha coefficient in this study was 0.831, and the test-retest reliability was 0.866. The criterion-related validity of the medication adherence questionnaire was 0.738, with MMAS-8Citation43 as a comparator criterion.
Data Collection
The data were collected from September to December 2017. Three research assistants received uniform training before the survey. The training includes the purpose, process, and methods of data collection of the study. To recruit participants from the cardiology ward in hospitals, the research assistants screened for participants who meet the eligibility and criteria and asked eligible patients if they were willing to participate in the survey. Upon expression of interest, the research assistants introduced themselves, explained the study, and obtained informed consent. The survey and the brief interview took about 30 minutes to complete and the research assistants explained content of the items if the participants expressed any questions or confusion. If the patients had no ability to complete the survey by themselves, the face-to-face interview was conducted to collect data.
Ethical Considerations
This study conformed with the principles outlined in the Declaration of Helsinki and was approved by the Ethics Committee of Hebei University. The researchers explained the aim and procedure of the study to eligible patients, and obtained their informed written consent. The participants were guaranteed that their participation was voluntary, and that all data would be held securely and confidentially, and that it would only be accessed by the research team.
Statistical Analysis
Data were analyzed using IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics were used to present the socio-demographic and clinical characteristics, depression, social support, self-efficacy, and medication adherence of the sample. A Pearson correlation coefficient was computed to examine the relationship between the four variables (depression, social support, self-efficacy, and medication adherence). Multivariable linear regression was used to examine the multivariate relationships among depression(X1), social support(X2), self-efficacy(X3) and medication adherence(Y). To control the effects of covariates, all the demographic and clinical variables (such as age, gender, marital status, education, income, family history of CHD, co-morbidity and duration of CHD) were entered into the regression model.
The overall model () was tested using the approach proposed by Preacher and HayesCitation44 which allows multiple mediators to be included in the mediation analysis. It is hypothesized that depression (X) would be associated with social support (M1), which, in turn, affects self-efficacy (M2) and influences medication adherence (Y) (). A serial mediator model with two mediators of social support and self-efficacy provided three indirect effects that sum to a total indirect effect. The indirect effects in the model were through (a) social support, (b) self-efficacy, and (c) both social support and self-efficacy. We then run the SPSS PROCESS macro for a testing serial mediation model with model 6 and 5000 bootstrap samples. In addition, covariates (age, gender, marital status, education, income, family history of CHD, co-morbidity and duration of CHD) were controlled in the model. 95% confidence interval (CI) was estimated for the mediation effects, with CI not containing zero, indicating the mediation effects being significant. Harman’s single-factor test was used to examine the common method bias (CMB). The variance explained by the first factor was lower than 40%, indicating that no CMB exists in the research data.
Results
Sample Characteristics
The sample consisted of 238 older patients with CHD, 134 males and 104 females, aged between 60 and 87 years old (mean=70.50, SD=6.40). Socio-demographic and clinical characteristics are shown in .
Table 1 Sample Socio-Demographic and Clinical Characteristics (N=238)
Descriptive Statistics and Correlation Among Depression, Social Support, Self-Efficacy, and Medication Adherence
As shown in , the mean score for medication adherence and depression were 14.77 ± 3.08 and 3.26 ± 3.60, respectively, and the total prevalence rates of depression was 21.01%, with mild (13.03%), moderate (6.30%) and severe (1.68%), respectively. The mean SSRS score was 39.47 (SD=5.24) and the average self-efficacy score was 35.71 (SD=4.25). The depression was negatively related to social support (r=−0.146, P=0.025), self-efficacy (r=−0.212, P=0.001), and medication adherence (r=−0.214, P=0.001), whereas social support and self-efficacy were positively related to medication adherence (r=0.366, P<0.001 and r=0.573, P<0.001, respectively). Social support was positively associated with self-efficacy (r=0.344, P<0.001) (). Multivariate linear regression analysis showed that depression was not associated with medication adherence when social support and self-efficacy were entered into regression model after adjusting the covariates ().
Table 2 Descriptive Statistics and Correlations Among the Depression, Social Support, Self-Efficacy and Medication Adherence (N=238)
Table 3 Associations of Demographic, Clinical and Other Variables and Medication Adherence Among Older CHD Patients (N=238)
Mediation Effects
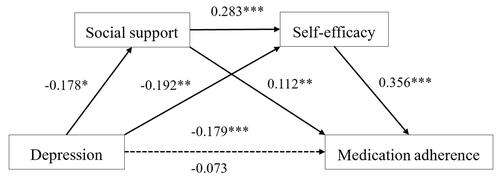
The mediated indirect effects of a specific path are shown in and . displays that the standardized coefficient of depression on medication adherence decreased from −0.179 (95% CI (−0.288, −0.070)) to −0.073 (95% CI (−0.165, 0.019)), which was not statistically significant, after introducing the mediators of social support and self-efficacy into the model. Thus, both multivariate linear regression () and mediation analysis results indicated full mediation, and the relationship between depression and medication adherence was totally mediated by social support and self-efficacy. The effect of the size of the mediational variable was derived from the ratio of the indirect effect over the total effect of the relationship between depression and medication adherence. The mediation effect of depression on medication adherence through social support was −0.020 (95% CI (−0.056, −0.002)), with an effect size of 11.17%. As a result, the serial mediation effect was −0.018 (95% CI (−0.050, −0.001)), accounting for 10. 06% of the total effect. The serial mediation effect of social support and self-efficacy was thus confirmed in the relationship between depression and medication adherence. The mediation effect of depression on medication adherence through self-efficacy was −0.068 (95% CI (−0.143, −0.002)), with an effect size of 37.99% ().
Table 4 Mediation Analysis of Depression and Medication Adherence (N=238)
Figure 2 Result of multiple mediator model. The numbers are standardized coefficients. −0.179=standardized coefficient before introducing social support and self-efficacy into the model; −0.073=standardized coefficients after introducing social support and self-efficacy into the model. The mediation model was adjusted for the following covariates: age, gender, marital status, education, income, family history of CHD, co-morbidity, duration of CHD. *P<0.05, **P<0.01, ***P<0.001.
Common Method Bias
The Herman single-factor analysis was used to examine Common Method Bias, and 38 items of the four variables, ie, depression, social support, self-efficacy, and medication adherence were examined by non-rotation principal component factor analysis. The first factor resulted in 21.65% of variance lower than 40%, indicating that there was no Common Method Bias in our study.
Discussion
The current investigation provides a new insight towards understanding of how depression influences medication adherence among older patients with CHD. The results found that depression was indirectly related to medication adherence through three pathways, (a) social support only, (b) self-efficacy only, and (c) combined social support and self-efficacy.
Depression and Medication Adherence
Depression was significantly correlated with medication adherence in older patients with CHD, which matches well with previous findings,Citation14,Citation30 suggesting that older CHD patients with depression tend to have poor medication adherence. Patients with chronic conditions often require lifelong medication therapy, and are recommended to adhere lifestyles which are synchronous with treatment goals.Citation45 Expectations of the benefits of treatment recommendations are an essential component of patient adherence.Citation46 Depressed patients usually have an outlook of hopelessness, and lack energy and motivation, which may contribute to their poor adherence to medication, especially in the long term.Citation47 The results reported by Son et al,Citation14 revealed that CHD patients who underwent primary percutaneous coronary intervention with depressive symptoms are more likely to be non-adherent to medication. In addition, our study confirmed that the relationship between depression and medication adherence was fully mediated by social support and self-efficacy. These findings comprise an essential knowledge base for developing interventions to improve medication adherence among older CHD patients with depressive symptoms.
The Mediation Role of Self-Efficacy Between Depression and Medication Adherence
Our results revealed that older CHD patients with higher self-efficacy had better medication adherence, which is in line with those of prior studies supporting a strong association between self-efficacy and medication adherence among CHD patients.Citation14,Citation28 Patients with higher self-efficacy may dedicate more effort and have a greater tendency to persist in their attempts to perform a target activity.Citation29 Also, our study confirmed self-efficacy as a mediator of the association between depression and medication adherence, revealing that older CHD patients with depressive symptoms have a lower confidence in their adherence to medication, ultimately leading to poor medication adherence. Son et al reported that CHD patients with depressive symptoms were more likely to develop low self-efficacy for medication, which was in accordance with our results.Citation30 Based on Bandura’s self-efficacy theory,Citation27 an individual’s self-efficacy for healthy behaviors may partially depend on his psychological or emotional state; positive emotion may enhance healthy behaviors, while negative emotion diminish them. Depressed patients, plagued by pessimism and hopelessness, tend to have reduced confidence in their ability to follow medication regimens persistently.
The Mediation Role of Social Support Between Depression and Medication Adherence
Social support was positively correlated to medication adherence, which is consistent with reports from previous studies.Citation18,Citation32 Patients with adequate social support may receive more external objective or subjective support from family members, relatives, or institutions, which promotes patients to likely obtain more health-related information to aid them to cope with diseases and adhere to medication.Citation18 And this study showed that social support mediated the relationship between depression and medication adherence. Kim et al’s studyCitation23 indicated that the social support played a significant mediation role in reducing the negative effect of depression symptoms on medication adherence, which is similar to our view. Depression is more likely to affect the extent to which one may seek social support. Depressed patients with negative interpersonal effect and emotion tend not to make good use of social support network and may obtain less support, subsequently, lower lever of social support may be related to poor medication adherence.
The Chain Mediating Effect of Social Support and Self-Efficacy Between Depression and Medication Adherence
Interestingly, our study also found that the relationship between depression and medication adherence was mediated by the chain combination of social support and self-efficacy. This indicates that older CHD patients with depression may have less social support, and inadequate social support may subsequently reduce their confidence in their ability to adhere to medication, eventually resulting in poor medication adherence. Tavor et alCitation47 showed that self-efficacy and social support mediated the relationship between depression and adherence and Maeda et alCitation32 indicated that self-efficacy fully mediated the association of social support with treatment adherence, which support our findings. However, our results are partially inconsistent with those of Kim et alCitation23 in their suggestion that social support totally mediated the association of depression with medication adherence in patients. The inconsistency may be due to that only one mediation variable (social support) was tested in Kim et al’s study. Older CHD patients with depressive symptoms may have fewer external resources or poor social network utilization, which reduces their level of social support essential for managing their health.Citation21 Patients with higher level of social support are possibly to have more diverse external resources for them to obtain verbal or behavioral encouragement, normative or informative influence, and take advantages therefrom to overcome their own problems, all of which may promote the level of self-efficacy for medication use.Citation32 When social support including economical or psychological support is not inadequate, patients may have lesser confidence in taking their medication, relating to poor medication adherence.Citation32,Citation48
Limitations
This study may have the following two limitations. One is that, due to the cross-sectional nature, this study suggested the association among social support, depression, self-efficacy and medication adherence. Therefore, the causal relationship could not be suggested in our analysis. The other is that, because the participants were recruited using a convenience sample process from only one region, it may not be sufficient to represent the population, thus generalizability of the findings is limited. And the number of participants enrolled in this study was small due to the limited time, our findings should be validated in a larger and more diverse CHD patients. Therefore, future studies with employing a larger and randomized sample and stronger statistical parametric analyses may be necessary to confirm the findings here. Additionally, longitudinal study designs with collecting multi-wave data are also recommended to identify the causal relationships among social support, self-efficacy, depression, and medication adherence in the future.
Clinical Practices
Despite these limitations, our study has some important implications for clinical practice. A considerable, existing body of evidence states that medication non-adherence in patients with CHD is a public health issue, necessitating the development and implementation of effective interventions.Citation49,Citation50 Based on our finding, healthcare professionals should recognize the effect of depression on older CHD patients, and the mediating role of social support and self-efficacy in the association of depression and medication adherence. Interventions focused on social support and self-efficacy may be beneficial to improve medication adherence in older CHD patients with depression. Thus, healthcare professionals should develop interventions focused on promoting social support and increasing self-efficacy to improve medication adherence in older CHD patients with depression in clinical practice.
Conclusion
The present study addressed a gap in the literature by exploring the role of self-efficacy and social support in the relationship between depression and self-reported medication adherence among older CHD patients. Social support and self-efficacy help to fully mediate the relationship between depression and medication. Additionally, this study identified that depression could affect medication adherence through the chain mediation of social support and self-efficacy. Thus, social support and self-efficacy are suggested to be given more attention to identify even better strategies for health professionals to improve medication adherence among CHD patients with depression.
Acknowledgments
The authors thank the participants for their contribution to this study.
Disclosure
The authors declare that they have no conflicts of interest in this work.
Additional information
Funding
References
- World Health Organisation. The top 10 causes of death. Fact sheet N° 310; 2017. Available from: http://www.who.int/mediacentre/factsheets/fs310/en/. Accessed January 17, 2022.
- Stern S, Behar S, Gottlieb S. Aging and disease of the heart. Circulation. 2003;108:e99–e101. doi:10.1161/01.CIR.0000086898.96021.B9
- Muhammad I, He HG, Kowitlawakul Y, Wang WR. Narrative review of health‐related quality of life and its predictors among patients with coronary heart disease. Int J Nurs Pract. 2016;22(1):4–14. doi:10.1111/ijn.12356
- Fihn SD, Gardin JM, Abrams J, et al. ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2012;60(24):e44–e164. doi:10.1016/j.jacc.2012.07.013
- Liu S, Li Y, Zeng X, et al. Burden of cardiovascular diseases in China, 1990–2016: findings from the 2016 global burden of disease study. JAMA Cardiol. 2019;4(4):342–352. doi:10.1001/jamacardio.2019.0295
- Jiang L, Krumholz HM, Li X, Li J, Hu S. Achieving best outcomes for patients with cardiovascular disease in China by enhancing the quality of medical care and establishing a learning health-care system. Lancet. 2015;386(10002):1493–1505. doi:10.1016/S0140-6736(15)00343-8
- Sabate E. Adherence to Long-Term Therapies: Evidence for Action. Geneva: World Health Organization; 2003.
- Zheng F, Ding S, Lai L, et al. Relationship between medication literacy and medication adherence in patients with coronary heart disease in Changsha, China. Front Pharmacol. 2019;10:1537. doi:10.3389/fphar.2019.01537
- Martins NFF, Abreu DPG, Silva BT, Semedo DS, Pelzer MT, Ienczak FS. Functional health literacy and adherence to the medication in older adults: integrative review. Rev Bras Enferm. 2017;70(4):868–874. doi:10.1590/0034-7167-2016-0625
- Walsh CA, Cahir C, Tecklenborg S, Byrne C, Culbertson C, Bennett KE. The association between medication non-adherence and adverse health outcomes in ageing populations: a systematic review and meta-analysis. Brit J Clin Pharmacol. 2019;85(11):2464–2478. doi:10.1111/bcp.14075
- Du LP, Cheng ZW, Zhang YX, Li Y, Mei D. The impact of medication adherence on clinical outcomes of coronary artery disease: a meta-analysis. Eur J Prev Cardiol. 2017;24(9):962–970. doi:10.1177/2047487317695628
- Sin NL, Kumar AD, Gehi AK, Whooley MA. Direction of association between depressive symptoms and lifestyle behaviors in patients with coronary heart disease: the heart and soul study. Ann Behav Med. 2016;50(4):523–532. doi:10.1007/s12160-016-9777-9
- Ho SY. The Impact of Depression on Treatment Adherence and Cardiorespiratory Fitness in Cardiac Rehabilitation. Burlington: The University of Vermont; 2017.
- Son YJ, Kim SH, Park JH. Role of depressive symptoms and self-efficacy of medication adherence in Korean patients after successful percutaneous coronary intervention. Int J Nurs Pract. 2014;20(6):564–572. doi:10.1111/ijn.12203
- Goldstein CM, Gathright EC, Garcia S. Relationship between depression and medication adherence in cardiovascular disease: the perfect challenge for the integrated care team. Patient Prefer Adher. 2017;11:547–559. doi:10.2147/PPA.S127277
- Ghaemmohamadi MS, Behzadifar M, Ghashghaee A, et al. Prevalence of depression in cardiovascular patients in Iran: a systematic review and meta-analysis from 2000 to 2017. J Affect Disord. 2018;227:149–155. doi:10.1016/j.jad.2017.10.026
- Al-Zaru IM, Alhalaiqa F, Dalky HF, Arramadan KA, Batiha AM. Depression in nonhospitalized Jordanian patients with coronary artery disease. J Nurs Res. 2020;28(1):1–9.doi:10.1097/jnr.0000000000000341
- Turan GB, Aksoy M, Çiftçi B. Effect of social support on the treatment adherence of hypertension patients. J Vas Nurs. 2019;37(1):46–51. doi:10.1016/j.jvn.2018.10.005
- Cohen S, Gottlieb B, Underwood L. Social Relationships and Health: Challenges for Measurement and Intervention. New York: Oxford University Press; 2000.
- Xiao SY. The theoretical basis and research application of Social Support Rating Scale. J Clin Psychiat. 1994;4(2):98–100. Chinese.
- Su SF, Chang MY, He CP. Social support, unstable angina, and stroke as predictors of depression in patients with coronary heart disease. J Cardiovasc Nurs. 2018;33(2):179–186. doi:10.1097/JCN.0000000000000419
- Chiou AF, Hsu SP, Hung HF. Predictors of health-promoting behaviors in Taiwanese patients with coronary artery disease. Appl Nurs Res. 2016;30:1–6. doi:10.1016/j.apnr.2015.08.008
- Kim CJ, Schlenk EA, Kim DJ, Kim D, Erlen JA, Kim SE. The role of social support on the relationship of depressive symptoms to medication adherence and self-care activities in adults with type 2 diabetes. J Adv Nurs. 2015;71(9):2164–2175. doi:10.1111/jan.12682
- Spikes T, Higgins M, Quyyumi A, Reolly C, Pemu P, Dunbar S. The relationship among health beliefs, depressive symptoms, medication adherence, and social support in African Americans with hypertension. J Cardiovasc Nurs. 2019;34(1):44–51. doi:10.1097/JCN.0000000000000519
- Huang YM, Shiyanbola OO, Smith PD. Association of health literacy and medication self-efficacy with medication adherence and diabetes control. Patient Prefer Adher. 2018;12:793–802. doi:10.2147/PPA.S153312
- Lu M, Xia H, Ma J, et al. Relationship between adherence to secondary prevention and health literacy, self-efficacy and disease knowledge among patients with coronary artery disease in China. Eur J Cardiovasc Nurs. 2020;19(3):230–237. doi:10.1177/1474515119880059
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs: Prentice-Hall, Inc.; 1986.
- Al-Ganmi AHA, Alotaibi A, Gholizadeh L, Perry L. Medication adherence and predictive factors in patients with cardiovascular disease: a cross-sectional study. Nurs Health Sci. 2020;22(2):454–463. doi:10.1111/nhs.12681
- Polsook R, Aungsuroch Y, Thongvichean T. The effect of self-efficacy enhancement program on medication adherence among post-acute myocardial infarction. Appl Nurs Res. 2016;32:67–72. doi:10.1016/j.apnr.2016.05.002
- Son YJ, Won MH. Depression and medication adherence among older Korean patients with hypertension: mediating role of self-efficacy. Int J Nurs Pract. 2017;20:564–572. doi:10.1111/ijn.12525
- Schoenthaler A, Ogedegbe G, Allegrante JP. Self-efficacy mediates the relationship between depressive symptoms and medication adherence among hypertensive African Americans. Health Educ Behav. 2009;36(1):127–137. doi:10.1177/1090198107309459
- Maeda U, Shen BJ, Schwarz ER, Farrell KA, Mallon S. Self-efficacy mediates the associations of social support and depression with treatment adherence in heart failure patients. Int J Behav Med. 2013;20(1):88–96. doi:10.1007/s12529-011-9215-0
- Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. doi:10.3758/BRM.41.4.1149
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999;282(18):1737–1744. doi:10.1001/jama.282.18.1737
- Schutt PE, Kung S, Clark MM, et al. Comparing the Beck Depression Inventory-II (BDI-II) and Patient Health Questionnaire (PHQ-9) depression measures in an outpatient bariatric clinic. Obes Surg. 2016;26(6):1274–1278. doi:10.1007/s11695-015-1877-2
- Yuan J, Ding R, Wang L, Sheng L, Li J, Hu D. Screening for depression in acute coronary syndrome patients: a comparison of patient health questionnaire-9 versus hospital anxiety and depression scale–depression. J Psychosom Res. 2019;121:24–28. doi:10.1016/j.jpsychores.2019.03.018
- Kong LN, Zhu WF, He S, Yao Y, Yang L. Relationships among social support, coping strategy, and depressive symptoms in older adults with diabetes. J Gerontol Nurs. 2019;45(4):40–46. doi:10.3928/00989134-20190305-03
- Risser J, Jacobson TA, Kripalani S. Development and psychometric evaluation of the Self-Efficacy for Appropriate Medication Use Scale (SEAMS) in low-literacy patients with chronic disease. J Nurs Meas. 2007;15(3):203–219. doi:10.1891/106137407783095757
- Dong XF, Liu YJ, Wand AX, Lv PH. Psychometric properties of the Chinese version of the self-efficacy for appropriate medication use scale in patients with stroke. Patient Prefer Adher. 2016;10:321–327. doi:10.2147/PPA.S101844
- Chen B, Chen L. Reliability and validity of Chinese version self-efficacy for appropriate medication use scale in the coronary heart disease patients. Chin J Modern Nurs. 2017;23(14):1837–1842. Chinese.
- Hu DY. Chinese Cardiovascular Disease Rehabilitation/Secondary Prevention Guidelines (2015 Edition). Beijing Science and Technology Press; 2015. Chinese.
- Zhang WY, Zhou Y, Cui SS, Shi QS, Lou SN, Wang Y. Development and validation of secondary prevention medication compliance questionnaire for patients with coronary heart disease. Chin Nurs Res. 2021. In press [http://www.hlyjzz.com]. Chinese.
- Morisky DE, Ang A, Krousel-wood M, Ward HJ. Predictive validity of a medication adherence measure for hypertension control. J Clin Hypertens. 2008;10(5):348–354. doi:10.1111/j.1751-7176.2008.07572.x
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi:10.3758/BRM.40.3.879
- Smith SC, Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: endorsed by the National Heart, Lung, and Blood Institute. J Am Coll Cardiol. 2006;47(10):2130–2139. doi:10.1016/j.jacc.2006.04.026
- DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160(14):2101–2107. doi:10.1001/archinte.160.14.2101
- Tovar E, Rayens MK, Gokun Y, Clark M. Mediators of adherence among adults with comorbid diabetes and depression: the role of self-efficacy and social support. J Health Psychol. 2015;20(11):1405–1415. doi:10.1177/1359105313512514
- Garett JG. The Relationship Among Social Support, Self-Efficacy and Medication Adherence in Adults with Hypertension. San Diego: Northcentral University; 2016.
- Hussain S, Jamal SZ, Qadir F. Medication adherence in post myocardial infarction patients. J Ayub Med Coll Abbottabad. 2018;30(4):552–557.
- Bansilal S, Castellano JM, Fuster V. Global burden of CVD: focus on secondary prevention of cardiovascular disease. Int J Cardiol. 2015;201:S1–S7. doi:10.1016/S0167-5273(15)31026-3