Abstract
Background
Nonadherence is common among patients with schizophrenia, although the rates vary according to means of assessment and patient population. Failure to adhere to medication can have a major impact on the course of illness and treatment outcomes, including increasing the risk of relapse and rehospitalization. Understanding psychiatrists’ perception of the causes and consequences of nonadherence is crucial to addressing adherence problems effectively.
Methods
The Europe, the Middle East, and Africa (EMEA) Spanish Adherencia Terapéutica en la Esquizofrenia (ADHES) survey was conducted by questionnaire during January–March 2010 among psychiatrists treating patients with schizophrenia in 36 countries. The survey comprised 20 questions. In addition to recording the demographic details of the 4722 respondents (~12% response rate), it canvassed their preferred methods of assessing adherence, their perceptions of adherence rates, reasons for nonadherence, and strategies to improve adherence.
Results
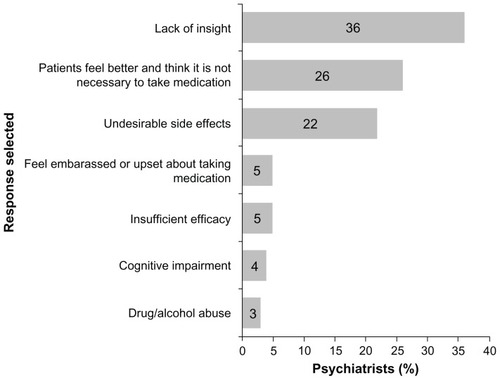
Psychiatrists estimated that 53% of their patients with schizophrenia were partially/nonadherent during the previous month. They estimated only one-third of patients who deteriorated after stopping medication were able to attribute this to nonadherence. Psychiatrists assessed adherence most often by patient interview. Lack of insight was viewed as the most important cause of medication discontinuation, followed by patients feeling better and thinking their medication unnecessary, and experiencing undesirable side effects. Considerably fewer psychiatrists viewed insufficient efficacy, cognitive impairment, or drug/alcohol abuse as the most important reasons for their patients stopping medication.
Conclusion
Psychiatrists throughout EMEA recognize the impact of partial/nonadherence to medication, with patient enquiry being the most commonly used means of assessment. There remains a need for more proactive management of patients with schizophrenia, particularly in increasing patient insight of their illness in order to improve adherence and minimize the consequences of relapse. Strategies focused on raising awareness of the importance of adherence are also warranted, with the aim of improving patient outcomes in schizophrenia.
Ensuring patients continue with their medication over the long term is a considerable challenge in psychiatry.Citation1 There is a range of often overlapping patient-, treatment-, environment-, and physician-related factors that contribute to partial or nonadherence to medication.Citation2 These factors include patients’ lack of insight, attitudes toward and previous experiences of medication, comorbidity and symptom severity, the level of social and family support, and the strength of the therapeutic alliance between patient and physician.Citation3
Health care professionals (HCPs) may positively influence treatment adherence by focusing on the positive aspects of medication, on enhancing insight, and on fostering a positive therapeutic relationship with patients.Citation4 There is growing evidence that patients who remain on antipsychotic treatment experience additional benefits beyond symptomatic control. For instance, important health-related quality of life benefits were observed with continuous antipsychotic treatment at 3 years in the European Schizophrenia Outpatients Health Outcomes study.Citation5
Partial or nonadherence to medication can have a major impact on the course of illness and treatment outcomesCitation6,Citation7 and is associated with an increased risk of relapse, persistence of symptoms, functional impairments, and increased hospitalization.Citation3,Citation8 As with other chronic somatic disorders, where as many as 76% of patients may be nonadherent to medication,Citation9 partial or nonadherence to medication is high among patients with psychiatric disorders. Definitions of medication adherence among patients with schizophrenia vary greatly, with reported rates of nonadherence of up to 72% being reported depending on the definition adopted, the method used to assess adherence, and the patient population evaluated.Citation10
Considerable research effort has focused on the impact of psychosocial, pharmacological and programmatic interventions on addressing adherence problems.Citation3 A systematic review of 24 controlled trials of psychosocial strategies (largely educational programs) to improve adherence to appointments and medication in patients with psychosis showed that these interventions were effective in both areas.Citation11 When nonadherence is due to forgetting medication, supplying medication in a daily compartmentalized medication container can help.Citation3 Involving patients in the choice of an antipsychotic and in reviews of effectiveness are important strategies to try to improve adherence.Citation3 Some studies, including one conducted among patients with early psychosis,Citation12 and a nationwide cohort study in Finland,Citation13 have shown significantly lower discontinuation rates for injectable formulations versus their equivalent oral antipsychotics (pooled analysis), with patients in the Finnish cohort almost twice as likely to discontinue oral antipsychotic treatment than treatment with the equivalent injectable formulation.Citation13
The Spanish Adherencia Terapéutica en la Esquizofrenia (ADHES) program commenced in 2003 and was aimed at raising awareness of the problem of partial and nonadherence to medication in the treatment of mental illness in Spain. As part of this program, a survey was developed and conducted in Spain to compare patients’, relatives’, and psychiatrists’ opinions on treatment adherence in schizophrenia.Citation14 Based on this initiative in Spain, a larger ADHES survey was developed, designed to canvas opinions of psychiatrists treating patients with schizophrenia across Europe, the Middle East, and Africa (EMEA) and ascertain their perceptions of potential reasons for partial or nonadherence to medication among their patients. This manuscript describes the methodology and findings of the ADHES survey of psychiatrists for the whole EMEA region; results from the individual countries within EMEA will be reported elsewhere.
Methods
The EMEA ADHES schizophrenia survey was developed and conducted as part of the ADHES program in collaboration with a steering committee comprising a group of psychiatrists with an interest in addressing problems of adherence to treatment by patients with schizophrenia.
The surveys were completed anonymously and responses were based on psychiatrists’ perceptions. Individual patient information was not collected. The survey comprised a 20-item questionnaire taking approximately 20 minutes to complete. The survey was conducted from January to March 2010 among EMEA psychiatrists (including neurologists with a psychiatric background in Germany) who were treating patients with schizophrenia.
Thirty-nine thousand copies of the survey were prepared for distribution to psychiatrists in 36 countries across the EMEA region. Mostly, the surveys were delivered to psychiatrists by Janssen Pharmaceutica NV personnel or by mail. The psychiatrists to whom the survey was distributed were identified from a database of psychiatrists held by Janssen. In France and Germany the survey was distributed at an open congress. Psychiatrists received a sealed pack containing the survey, a prepaid envelope, and a letter signed by the steering committee explaining the aims of the survey. No further follow-up was made in order to obtain responses from recipients of the survey who did not initially respond. The survey was translated from English into local languages when required. Completed surveys were returned directly and blinded to a third-party agency for data analysis. The survey was not designed to allow statistical analysis of the differences in responses, and the respective versions of the questionnaire were not validated against each other following translation. Interpretation of the results reported here is based on qualitative comparison of the responses obtained.
In addition to recording the gender, age, and practice setting of the respondents, the survey contained questions relating directly to the issue of partial/nonadherence to medication in patients with schizophrenia. In recording their responses, psychiatrists were required to estimate (open field) the adherence status of the patients they had seen in the preceding month according to each of the following categories: adherent (≥90% recommended treatment dose), partially adherent (≥30%–,90% recommended treatment dose), or nonadherent (<30% recommended treatment dose). Psychiatrists may have based these responses upon patient interview, clinical experience, their own estimation, or other means. Overall calculations of the proportions of patients who were fully, partially, or nonadherent to treatment were calculated as the arithmetic mean of the values entered for each of the above categories.
Respondents were asked to estimate the proportion of patients, seen by them during the previous month, affected by potential contributors to partial or nonadherence according to three groupings: less than 20% of patients, between 20% and 50% of patients, more than 50% of patients.
Results
Results were obtained from 4722 psychiatrists across the EMEA region, representing an estimated response rate of approximately 12%, based on the method and number of surveys distributed. The demographics of respondents in terms of their sex, age, and practice setting are shown in .
Table 1 Demographics of respondents (N = 4722)
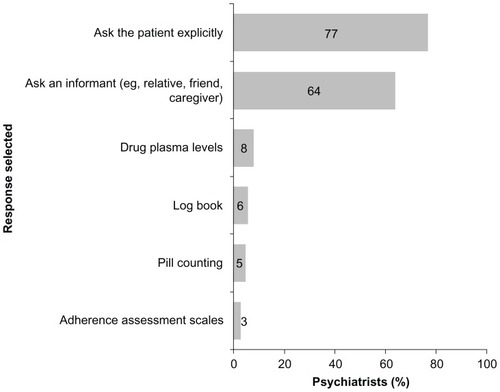
Seventy-six percent of respondents stated that they assessed adherence of their patients at each visit (). Fifty-three percent of the patients seen by psychiatrists in the prior month were considered to be either partially or nonadherent (). When assessing adherence, asking patients (77%) or a close informant (64%) were the methods used most often by the respondents ().
Figure 1 Psychiatrists’ responses regarding the frequency with which they assess adherence in their patients.*
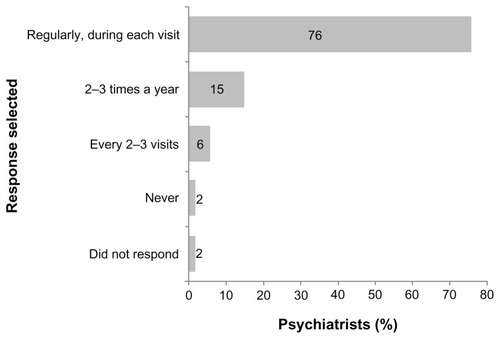
Figure 2 Proportion of patients perceived to be nonadherent, partially adherent, or fully adherent.*
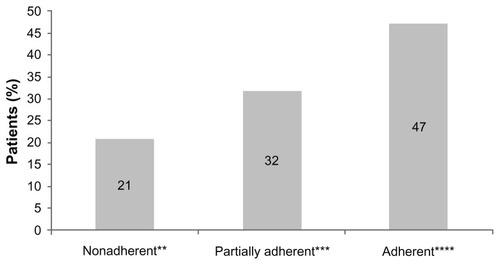
Figure 3 Psychiatrists’ views on the approach they normally used to assess adherence (ie, selected the respective methods as their first or second preference).*
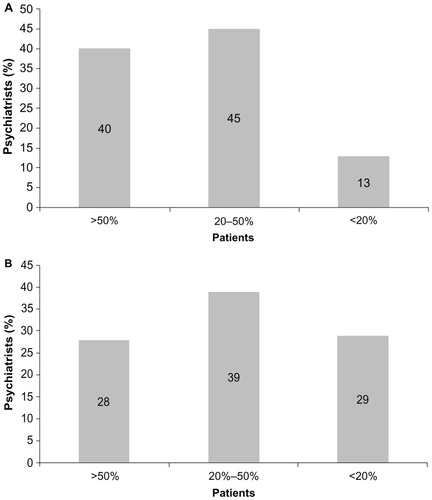
Forty percent of psychiatrists reported that most of their patients needed reminding by family members/carers to take their medication as prescribed (). Fewer psychiatrists (28%) thought that most of their patients relied on a nurse, psychiatrist, or professional carer to do so ().
Figure 4 (A) Psychiatrists’ views on the burden on family members or carers in reminding patients to take their medication.* (B) Psychiatrists’ views on the burden on health care professionals in reminding patients to take their medication.** (A) (2% of respondents to the survey did not complete this question). (B) (4% of respondents to the survey did not complete this question).
Psychiatrists’ views, based on their experience, as to the most important reasons for their patients discontinuing medication are shown in . Thirty-six percent of psychiatrists viewed lack of insight as the most important reason for their patients stopping medication. Patients feeling better and thinking it unnecessary to take medication, and undesirable side effects, were viewed as the most important reasons for their patients stopping medication by 26% and 22% of psychiatrists, respectively. Five percent or fewer of psychiatrists viewed feeling embarrassed or upset about taking medication, insufficient efficacy, cognitive impairment, or drug/alcohol abuse as the most important reasons for their patients stopping medication.
Figure 5 Psychiatrist’s views on the most important reason for their patients discontinuing medication.*
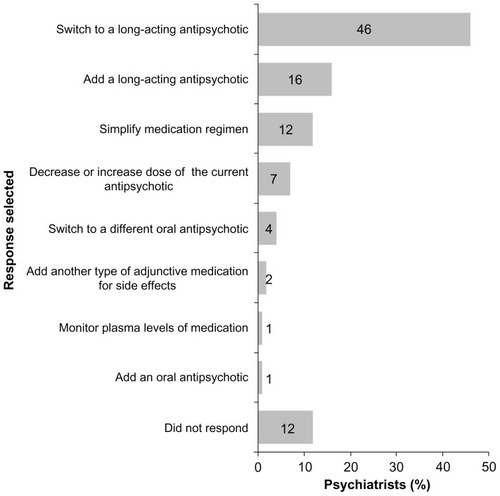
Switching to or adding a long-acting injectable antipsychotic was the preferred pharmacological approach used by 62% of psychiatrists for addressing adherence problems ().
Figure 6 Psychiatrists’ views on the preferred pharmacological approach they would use to address an adherence problem in their patients.*
Discussion
The EMEA ADHES schizophrenia survey provides insight to the perceptions of a large number of psychiatrists across a broad geographical area on the assessment, causes, and management of partial and nonadherence to medication in patients with schizophrenia. The response rate was similar to another postal survey conducted among psychiatrists concerning their attitudes toward medication.Citation15 There is good agreement among psychiatrists that asking patients explicitly about the amount of medication taken is the preferred method of assessing adherence; however, definitions of medication adherence vary greatly.Citation3 Upper and lower limits for the levels of adherence have recently been recommended, to increase comparability across studies.Citation3 Arbitrary levels were chosen to assign categories of patient adherence to treatment in the EMEA ADHES survey; nevertheless, the estimated level of partially or nonadherent patients is in line with other assessments of adherence levels among patients with schizophreniaCitation16 and similar surveys conducted with smaller groups of psychiatrists.Citation14,Citation17 In addition, while psychiatrists also estimated that the majority of their patients may not have stopped medication altogether (>5 consecutive days) without consulting them, a number of patients were perceived to have done so (see ). However, incorrect estimates may result from relying on physician reports of patient decision-making,Citation18 and physician perceptions of suspected rather than known nonadherence may not serve as accurate predictors of patient behavior. Indeed, there is evidence to show that psychiatrists can overestimate levels of adherence.Citation19,Citation20
The high frequency with which psychiatrists claim to assess adherence suggests that it is considered an important aspect of managing the patient’s disorder; however, since the respondents to the survey particularly favor subjective methods over potentially more accurate methods, such as the use of adherence scales, pill counts, or drug plasma level monitoring, and given that all methods of assessment can underestimate the true extent of poor adherence,Citation19 the extent of partial and nonadherence may be even greater. It is important that when clinicians enquire about adherence they do so in a nonjudgmental way that encourages patients to discuss adherence openly.Citation21
The survey findings highlight the extent to which patients are perceived to rely on a HCP, and to an even greater extent on family members/carers, to remind them to take their medication as prescribed, illustrating the additional burden nonadherence to medication by patients places on those around them.Citation8
The impact of lack of insight on adherence is highlighted in the current survey since psychiatrists considered, in their experience, it was the most important reason for patients discontinuing medication. Moreover, 23% of psychiatrists perceived that most of their patients showed lack of insight in the previous month (see ). Poor insight is a common feature of schizophrenia and has a complex relationship to other symptoms of the illness.Citation22 Patients with a lack of insight usually do not recognize that they are ill, while those with partial insight demonstrate poor awareness of being ill and the need for medication.Citation23 One assessment suggested that between 50% and 80% of patients with schizophrenia do not believe they have a disorder.Citation24 Recent research has illustrated the impact that poor insight and irregular daily routines have on medication adherence, with poor insight shown to increase the risk of nonadherence twofold.Citation25 Thus, poor insight can prevent treatment, destabilize the patient, and lead to a poor prognosis.Citation2,Citation26 Three out of four psychiatrists who responded to the EMEA ADHES survey perceived that most of their patients were unable to attribute clinical deterioration to medication nonadherence (see ) and two out of five psychiatrists considered that most of their patients understood there is a risk of relapse if they did not take their medication regularly (see ).
Respondents to the survey (26%) also considered their patients feeling better and thinking it unnecessary to take medication was a relatively important reason for patients discontinuing medication. This factor has been shown to influence treatment adherence more widely,Citation27 particularly following recovery from a first psychotic episode.Citation28 Irregular daily routine or difficult living circumstances were also considered by psychiatrists to be important reasons for partial/nonadherence to treatment among most of their patients during this period. Irregular daily routines can include aspects such as shift work, unemployment, and irregularities in family relationships and environment. Unemployment and social isolation have been shown to be strongly associated with nonadherence,Citation29 while nonsupportive family structures were predictive of poor adherence in first-episode psychosis.Citation30
The occurrence of undesirable side effects was cited as an important reason for their patients discontinuing their medication. This is consistent with other studies in which this factor was found to be associated with nonadherence.Citation28,Citation31 When considering the impact of treatment side effects on adherence, the attitudes of physicians toward the tolerability of antipsychotics must be borne in mind since these have previously been shown to be markedly different to those of the general population.Citation32
Among a variety of pharmacological options available to address adherence problems in their patients, the majority of psychiatrists favored switching to or adding a long-acting antipsychotic; however, it is unclear whether this preference occurs in clinical practice since in many countries fewer than 20% of individuals with schizophrenia receive long-acting or depot antipsychotics.Citation15 This finding may be partly influenced by attitudes toward treatment and awareness of the available options. Before a decision can be made on the most appropriate treatment strategy, some understanding of the possible reasons for nonadherence is required through discussion with the patient, which must be weighed against the likelihood that individual adherence problems are influenced by multiple and often different factors.
Limitations
The results reported and discussed here are based on the clinical opinions of the psychiatrists surveyed. The psychiatrists to whom the surveys were distributed were identified from a database held by Janssen. A large proportion of the psychiatrists surveyed here worked in a hospital setting and therefore may be more likely to have treated seriously ill patients or patients with suboptimal adherence. However, the demographics of the patients (for instance, whether they were living independently or providing their own care) and clinical status of the patients to whom the psychiatrists’ answers related, are not known. The psychiatrists who responded may have a greater awareness of adherence problems and a more pessimistic view of the extent of partial/nonadherence by patients with schizophrenia than the broader population of psychiatrists across the EMEA region. The extent to which the demographics (in terms of gender, age, and practice setting) of the respondents may differ from those of psychiatrists across the EMEA region as a whole, and the impact on the survey results, are not known.
Conclusion
The EMEA ADHES schizophrenia survey is the first survey of the perceptions of the assessment, causes, and management of partial and nonadherence to medication within such a large number of psychiatrists across EMEA. The survey findings confirm psychiatrists perceive that partial and nonadherence to treatment remains a considerable problem for patients with schizophrenia. Psychiatrists consider assessment of adherence to be an important aspect of patient management and show considerable agreement on the main reasons that influence patient adherence.
The survey findings suggest that focusing on factors such as improving patient insight and patients’ daily routine and living circumstances may lead to a reduction in the high level of partial or nonadherence among patients reported here. Similarly, steps to ensure that appropriate pharmacological treatment options are offered to patients, and that patients continue with their medication even when they feel better, are also warranted if improved clinical outcomes in the treatment of patients with schizophrenia are to be achieved.
Acknowledgments
The EMEA ADHES survey and this manuscript were supported by funding from Janssen Pharmaceutica NV. Medical writing support was provided by ApotheCom ScopeMedical, Sevenoaks, UK, funded by Janssen. All authors approved the design and reviewed the results of the survey. All authors developed the draft of the manuscript, participated in subsequent revisions, and read and approved the final manuscript.
Supplementary figures
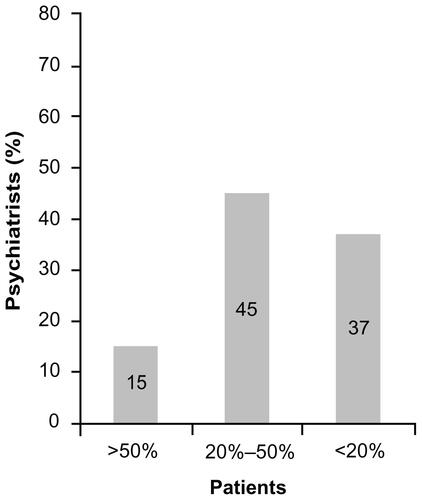
Figure S1 What percentage of your patients may have stopped medication altogether (>5 consecutive days) without consulting you?
Note: 1% of respondents to the survey did not complete this question.
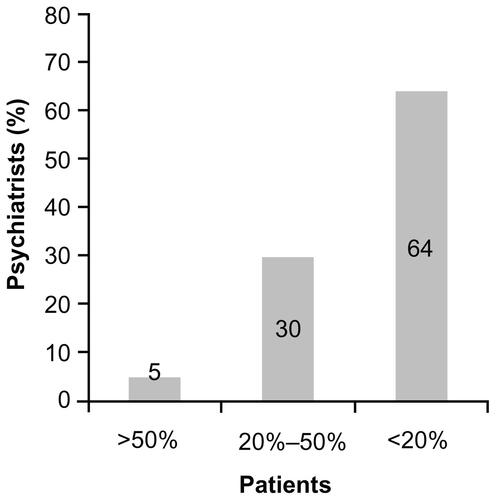
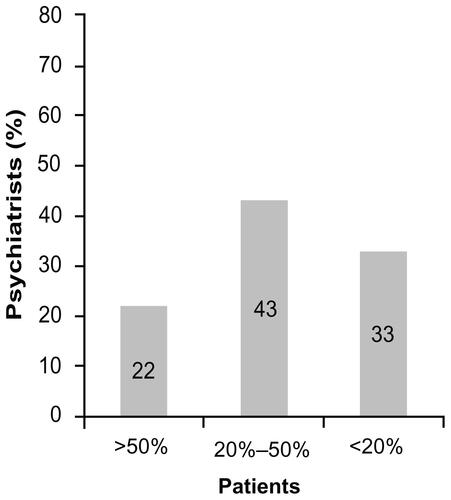
Figure S2 What percentage of your patients who deteriorated after stopping medication were able to attribute this to medication nonadherence?
Note: 5% of respondents to the survey did not complete this question.
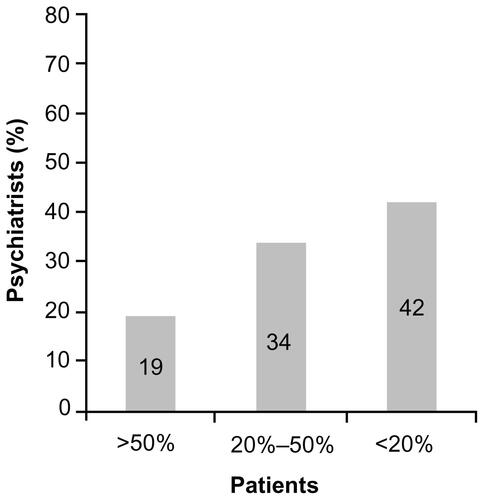
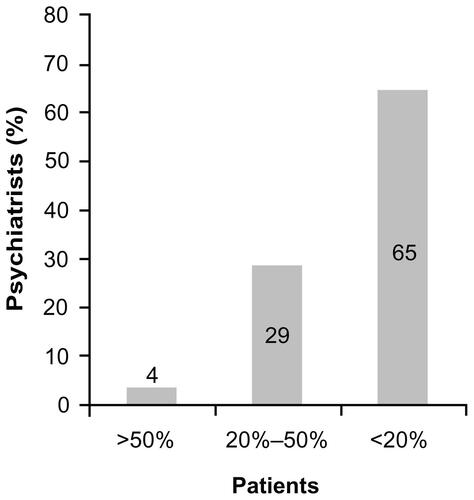
Figure S3 What percentage of your patients have told you that they understand there is a risk of relapse if they don’t take their medication regularly?
Note: 2% of respondents to the survey did not complete this question.
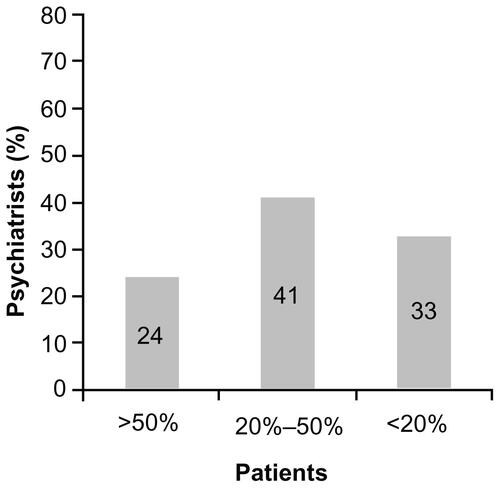
Figure S4 What percentage of your patients show, or has at any time in the past month, shown some lack of insight?
Note: 4% of respondents to the survey did not complete this question.
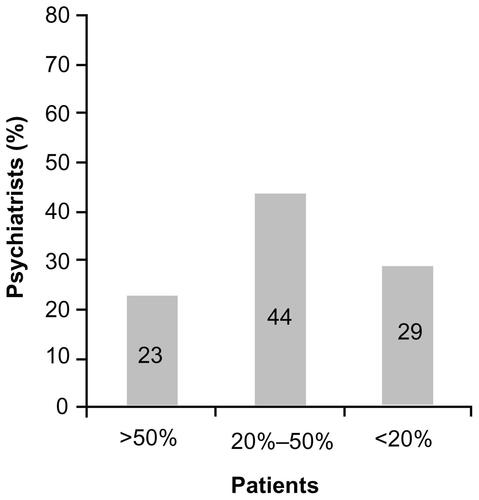
Figure S5 What percentage of your patients has an irregular daily routine or lives in circumstances that might affect proper daily compliance with their treatment?
Note: 4% of respondents to the survey did not complete this question.
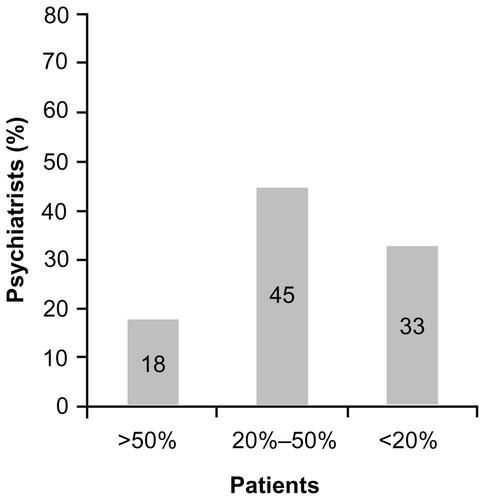
Figure S6 When your patients felt better, what percentage said that medication was unnecessary and stopped taking it?
Note: 2% of respondents to the survey did not complete this question.
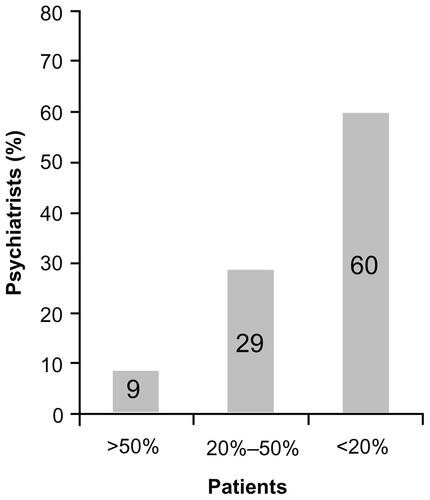
Figure S7 What percentage of your patients has not taken their medication due to psychotic symptoms?
Note: 2% of respondents to the survey did not complete this question.
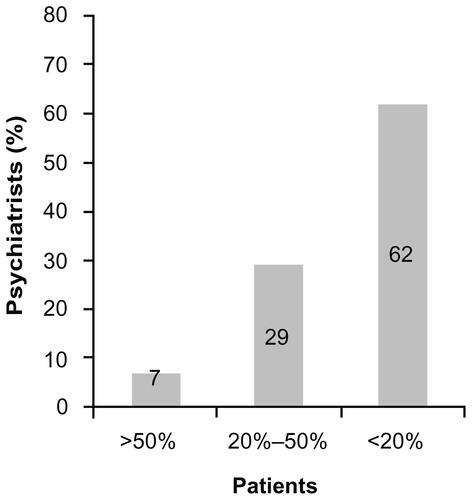
Figure S8 What percentage of your patients has not taken their medication due to cognitive impairment?
Note: 4% of respondents to the survey did not complete this question.
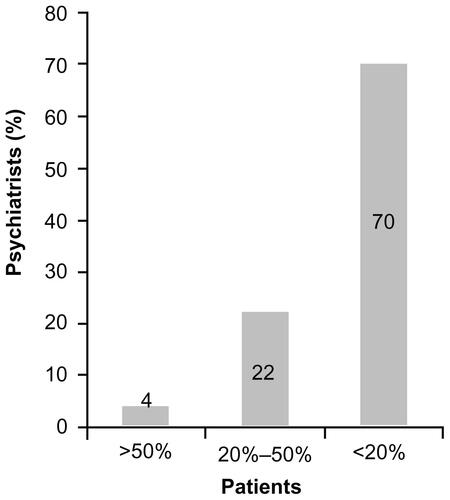
Figure S9 What percentage of your patients stopped taking their medication due to undesirable side effects?
Note: 4% of respondents to the survey did not complete this question.
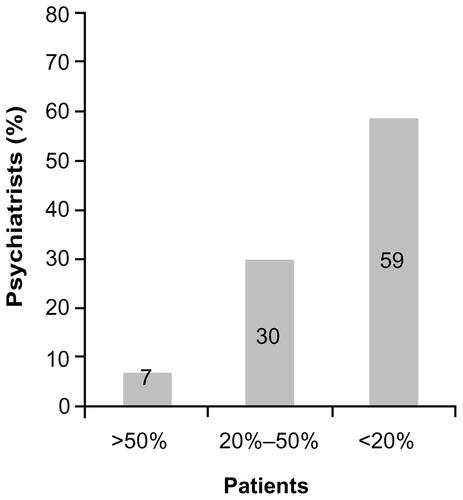
Figure S10 What percentage of your patients has a drug or alcohol consumption that may have impacted on their adherence to medication?
Note: 2% of respondents to the survey did not complete this question.
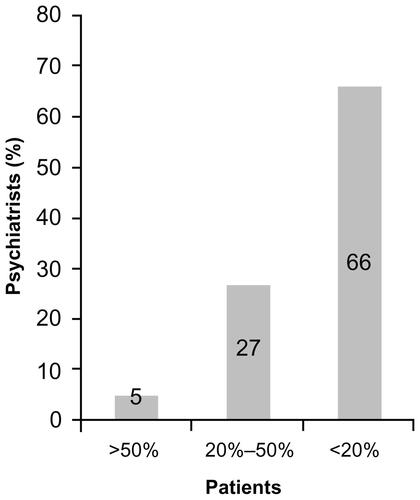
Figure S11 What percentage of your patients have families with negative views about medication?
Note: 2% of respondents to the survey did not complete this question.
Disclosure
GM and AS are employees of Janssen Pharmaceutica NV, Medical Affairs. JMO, KA, JMA, FC, VD, RE, PG, PMH, DN, GP, MR, and PT have been members of advisory boards, involved in designing and participating in clinical trials, or received educational grants for research, honoraria, and travel from Janssen as well as other pharmaceutical companies.
The authors’ involvement in the ADHES program, described in this paper, was part of paid consultancy work with Janssen, who provided travel expenses for authors to attend advisory boards where the project was discussed. Authors were not remunerated for their involvement in the preparation of this manuscript.
References
- KaneJMReview of treatments that can ameliorate nonadherence in patients with schizophreniaJ Clin Psychiatry200667Suppl 591416822091
- LlorcaPMPartial compliance in schizophrenia and the impact on patient outcomesPsychiatry Res200816123524718849080
- VelliganDIWeidenPJSajatovicMExpert Consensus Panel on Adherence Problems in Serious and Persistent Mental Illness: The expert consensus guideline series: adherence problems in patients with serious and persistent mental illnessJ Clin Psychiatry200970Suppl 414619686636
- KikkertMJScheneAHKoeterMWJMedication adherence in schizophrenia: exploring patients’, carers’ and professionals’ viewsSchizophr Bull20063278679416887889
- AlonsoJCroudaceTBrownJHealth-related quality of life (HRQL) and continuous antipsychotic treatment: 3-year results from the Schizophrenia Health Outcomes (SOHO) studyValue Health20091253654319900255
- KeithSJKaneJMPartial compliance and patient consequences in schizophrenia: our patients can do betterJ Clin Psychiatry2003641308131514658944
- MasandPSRocaMTurnerMSKaneJMPartial adherence to antipsychotic medication impacts the course of illness in patients with schizophrenia: a review. Prim Care CompanionJ Clin Psychiatry200911147154
- NovickDHaroJMSuarezDPerezVDittmannRWHaddadPMPredictors and clinical consequences of non-adherence with antipsychotic medication in the outpatient treatment of schizophreniaPsychiatry Res201017610911320185182
- CramerJARosenheckRCompliance with medication regimens for mental and physical disordersPsychiatr Serv1998491962019575004
- LacroJPDunnLBDolderCRLeckbandSGJesteDVPrevalence of and Risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literatureJ Clin Psychiatry20026389290912416599
- NoséMBarbuiCGrayRTansellaMClinical interventions for treatment non-adherence in psychosis: meta-analysisBr J Psychiatry200318319720612948991
- EmsleyROosthuizenPKoenLNiehausDJHMedoriRRabinowitzJOral versus injectable antipsychotic treatment in early psychosis: post hoc comparison of two studiesClin Ther2008302378238619167596
- TiihonenJHaukkaJTaylorMHaddadPMPatelMXKorhonenPA nationwide cohort study of oral and depot antipsychotics after first hospitalization for schizophreniaAm J Psychiatry201116860360921362741
- GinerJCañasFOlivaresJMTreatment adherence in schizophrenia. A comparison between patient’s, relative’s and psychiatrist’s opinionsActas Esp Psiquiatr20063438639217117335
- JaegerMRosslerWAttitudes towards long-acting depot antipsychotics: a survey of patients, relatives and psychiatristsPsychiatry Res2010175586220004980
- MarderSROverview of partial complianceJ Clin Psychiatry200364Suppl 163914680412
- TurnerMMasandPRocaMKaneJResults of a study on psychiatrists’ perceptions of adherence to medication among patients with schizophrenia: the ADHES surveyEur Neuropsychopharmacol200717Suppl 4S455S456
- RosenheckRChangSChoeYMedication continuation and compliance: a comparison of patients treated with clozapine and haloperidolJ Clin Psychiatry20006138238610847315
- VelliganDILamY-WFGlahnDCDefining and assessing adherence to oral antipsychotics: a review of the literatureSchizophr Bull20063272474216707778
- VelliganDIWangMDiamondPRelationships among subjective and objective measures of adherence to oral antipsychotic medicationsPsychiatric Services2007581187119217766564
- CanasFAlptekinKAzorinJMImproving treatment adherence in your patients with schizophrenia: the STAY initiativeClin Drug Invest2012
- SevySNathansonKVisweswaraiahHAmadorXThe relationship between insight and symptoms in schizophreniaCompr Psychiatry200445161914671732
- AgugliaEDe VannaMOnorMLFerraraDInsight in persons with schizophrenia: effects of switching from conventional neuroleptics to atypical antipsychoticsProg Neuropsychopharmacol Biol Psychiatry2002261229123312502008
- DamJInsight in schizophrenia: a reviewNord J Psychiatry20066011412016635929
- Novak-GrubicVTavcarRPredictors of noncompliance in males with first-episode schizophrenia, schizophreniform and schizoaffective disorderEur Psychiatry20021714815412052575
- LysakerPHBuckKDSalvatoreGPopoloRDimaggioGLack of awareness of illness in schizophrenia: conceptualizations, correlates and treatment approachesExpert Rev Neurother200991035104319589052
- FleischhackerWWEerdekensMKarcherKTreatment of schizophrenia with long-acting injectable risperidone: a 12-month open-label trial of the first long-acting second-generation antipsychoticJ Clin Psychiatry2003641250125714658976
- PerkinsDOGuHWeidenPJMcEvoyJPHamerRMLiebermanJAon behalf of the Comparison of Atypicals in First Episode study groupPredictors of treatment discontinuation and medication nonadherence in patients recovering from a first episode of schizophrenia, schizophreniform disorder, schizoaffective disorder: A randomized double-blind, flexible-dose, multicenter studyJ Clin Psychiatry20086910611318312044
- TacchiM-JScottJImproving Adherence in Schizophrenia and Bipolar DisordersChichester, EnglandJohn Wiley and Sons Ltd2005
- RabinovitchMBéchard-EvansLSchmitzNJooberRMallaAEarly predictors of nonadherence to antipsychotic therapy in first-episode psychosisCan J Psychiatry200954283519175977
- RobinsonDGWoernerMGAlvirJMBilderRMHinrichsenGALiebermanJAPredictors of medication discontinuation by patients with first-episode schizophrenia and schizoaffective disorderSchizophr Res20025720921912223252
- HelblingJAjdacic-GrossVLauberCWeyermannRBurnsTRösslerWAttitudes to antipsychotic drugs and their side effects: a comparison between general practitioners and the general populationBMC Psychiatry200664217049093