Abstract
Purpose
Medication adherence plays an important role in glycemic control in type 2 diabetes mellitus (T2DM) self-management. To analyze the factors influencing medication adherence in T2DM patients and the effect of pharmacist-led interventions, we conducted a study in Beijing, China.
Patients and Methods
T2DM patients with hypoglycemic drugs for at least 6 months were enrolled. A pharmacist-led survey was conducted followed by individualized interventions for those non-adherent patients monthly within 3 months. FPG, HbA1c, and 2hPG were measured as the comprehensive glycemic control. Medication adherence was determined according to the patient’s self-reported compliance with prescribed medication during the last 3 months.
Results
A total of 763 T2DM patients were included. The average age was 63.26±11.89 years, with 363 males. After pharmacist intervention, the patients with good adherence increased from 34.21% to 39.06%, while poor adherence decreased from 32.5% to 24.5% (p < 0.001). The average adherence score was a significant increase (p < 0.001) from 27.846±4.185 to 29.831±7.065. Furthermore, our study demonstrated that pharmacist-led interventions significantly increased glycemic control (FPG from 42.33% to 53.60%, p < 0.001; 2hPG from 41.68% to 48.75%, p = 0.005; HbA1c from 24.12% to 29.23%, p = 0.024). The results found that body mass index (OR 0.643, 95% CI 0.437–0.945), use of medications empirically (occasionally (OR=3.066, 95% CI 2.069–4.543); often (OR=2.984, 95% CI 1.107–8.044)), following the doctor’s advice to visit (OR 2.129, 95% CI 1.079–4.202) and lifestyle compliance (OR 2.835, 95% CI 1.094–7.346) were the independent risk factors of non-adherence (p < 0.05), the area under the ROC curve was 0.716.
Conclusion
Self-reported medication adherence and glycemic control in T2DM patients were poor which can be improved by pharmacist-led interventions. Interventions should focus on empirical medication behavior, non-adherence to lifestyle, and failure to follow the doctor’s advice. The recall bias with self-reported results needs further objective data to verify.
Introduction
Over the past few decades, the incidence of diabetes worldwide has been increasing rapidly year by year, causing a huge burden on people’s lives and the economy.Citation1 Type 2 diabetes mellitus (T2DM) is the most prevalent type of diabetes, accounting for more than 90% of all diabetes cases.Citation2 China is associated with the largest number of patients with diabetes and the fastest-growing diabetes prevalence rate in the world.Citation3 A recent epidemiological survey showed that the prevalence of diabetes in Chinese adults was 12.8%Citation4 and the significant increase is mainly attributed to T2DM.Citation5 T2DM treatment aims to control blood glucose levels and slow down complications. Improvement in medication adherence can result in better health outcomes.Citation6 According to the control criterion for the prevention and treatment of type 2 diabetes in China, the glycemic control rate of T2DM in China was low, as shown by fasting plasma glucose (FPG), 2 h postprandial plasma glucose (2hPG), and glycated hemoglobin (HbA1c) control rates of 25.5%, 22.7%, and 19.5%, respectively.Citation7,Citation8 Poorly controlled diabetes is associated with the development of macrovascular and microvascular complications,Citation9 such as cardiovascular disease,Citation10 sudden death,Citation11 cerebrovascular disease,Citation12 diabetic nephropathy,Citation13 diabetic retinopathy,Citation14 and so on. Previous studies have proved that the severity of vascular complications depends on the duration and degree of hyperglycemia.Citation15,Citation16 Given the substantial clinical impact of diabetes as a risk factor for macrovascular and microvascular injury, successful management of blood glucose levels can reduce the number of vascular events.Citation17
Non-adherence to medication therapy is the major obstacle in the management of T2DM.Citation18 For the successful management of T2DM, medication adherence, and persistence with the treatment are crucial.Citation19 Previous studies have confirmed that pharmacist-led interventions can improve T2DM patients’ medication adherence and glycemic control.Citation20–24 However, other studies have pointed out that the role of pharmacists in improving medication adherence or clinical outcomes remained controversial.Citation25–27 The exact role of pharmacists in improving medication adherence needs further examination, and there are few studies related to this topic in China. In the real world, the current status of medication adherence and glycemic control in patients with T2DM in China is still unclear. Thus, this study aimed to investigate medication adherence and glycemic control in T2DM patients and evaluate the effect of pharmacist-led interventions.
Materials and Methods
Patients Enrollment
This study was a multicenter, prospective survey of T2DM outpatients conducted in 35 medical institutions (including 5 tertiary hospitals, 6 secondary hospitals, and 24 community health service centers) in Beijing, China, with Beijing Tiantan Hospital affiliated to Capital Medical University as the main investigator. Written informed consent was obtained from each patient. All data were collected between May 2020 and April 2021. Before the initiation of this study, the questionnaire, research plan, and informed consent form were reviewed and approved by the Ethics Committee of Beijing Tiantan Hospital (Approval No.: KY2020-085-02, 2020-8-23) and all participating institutions.
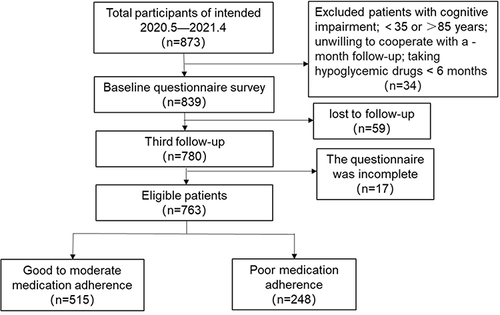
The following inclusion criteria were used: (1) T2DM patients (aged between 35 and 85 years) who were treated with hypoglycemic drugs for at least 6 months, (2) patients with no cognitive impairment and ability to communicate independently and participate in the research voluntarily, (3) patients with the ability to record medicine information, monitor blood glucose levels regularly, and follow-up for at least 3 months, and (4) patients that understand the questionnaire or scale after explanation and cooperate with pharmacists to complete the questionnaire. Patients who did not follow up and/or had incomplete follow-up were excluded from the analysis. The screening flow chart of enrolled patients was listed in .
Study Design
The experts of the research group designed the Questionnaire of Medication Adherence and Glycemic Control Rate of T2DM (QMAGCR) concerning the reported common factors influencing medication adherence. The QMAGCR included the following five parts (38 items): (1) demographic and sociological characteristics of the patients, (2) diabetes and medication information, (3) medication records, (4) medication adherence, and (5) behavior and lifestyle compliance.
Medication Adherence Assessment
Medication adherence was determined according to the patient’s compliance with prescribed medication during the last 3 months. There were nine items with four options (score of 1–4). The answers followed Likert’s four categories where 1 point and 4 points signify “never” and “always”, or the reverse. Here, the total is the sum of the scores for each question, with the highest score of 36. A higher score represents better adherence, scores of 36, 27 – ˂ 36, and ˂ 27 were defined as good, moderate, and poor adherence (Supplementary Table S1).
Lifestyle Compliance Assessment and Glycemic Control Criteria
A total of 9 questions were set, and the scoring standard of question options was consistent with the scoring rules of medication adherence above. (See Supplementary Table S2 for more details).
Fasting Plasma Glucose, 2hPG, and HbA1c levels were used to assess the glycemic control of the patients. The glycemic control criteria were according to the guidelines for the prevention and treatment of T2DM in China formulated by the diabetes branch of the Chinese Medical Association;Citation8 successful glycemic control was defined as HbA1c <7% or FPG <7.0 mmol/L; the goal of 2hPG was 4.4~10 mmol/L. The results of FPG and 2hPG were based on the latest day results self-reported by the patient or the patient’s laboratory test results at baseline and the third follow-up; HbA1c was obtained from the patient’s laboratory test results within the last month.
Pharmacist-Led Interventions
The pharmacists involved in the study were consultant pharmacists with more than 5 years of work experience or clinical pharmacists with more than 2 years of work experience; they were fully informed and trained about the study. Pharmacists conducted baseline surveys in the form of face-to-face interviews after patients’ informed consent. All patients were followed up by phone or WeChat for 3 months, and the QMAGCR was filled out at baseline and the third visit. The first survey was used as a baseline study, and three follow-up visits were conducted in the first, second, and third months after the baseline study. At the first and second follow-up visits, only any medication related problems or adjustments were recorded. Simple medication consultation and diabetes medication education were provided for patients with good adherence at baseline. Patients with moderate and poor adherence were provided with individualized pharmacist-led interventions, which included medication reconciliations, time and dosage adjustments, education on diabetes medication, proper use of insulin, medication reminders, adverse reactions and management of drugs, diet control, exercise recommendations, and so on.
Statistical Analysis
Statistical analyses were performed using Microsoft Excel and IBM SPSS Statistics 22.0. The data were plotted using GraphPad Prism v5.0. Enumeration data were statistically described by frequency and rate (%), while the measurement data were expressed as the mean ± SD. Descriptive statistics, chi-square (χ2) test, t-test, and rank sum test, were used to evaluate the results. Results were considered statistically significant if the p value < 0.05.
Results
Demographic and Sociological Characteristics of Patients
A total of 763 T2DM patients were included in the study, with 363 male (47.58%) and 400 female (52.42%). The average age of the patients was 63.26 ± 11.89 years. There were 488 cases (63.96%) that had diabetes for more than 5 years, while 266 cases (34.86%) received hypoglycemic drugs for more than 10 years. Among 763 patients, 276 (36.17%) patients got more than 3 kinds of combined chronic diseases, and 455 (59.63%) patients received more than 2 categories of hypoglycemic drugs. The demographic and sociological characteristics of the patients were summarized in .
Table 1 Demographic and Sociological Characteristics of T2DM Patients
Medication Adherence
Baseline and 3-month follow-up investigations were considered for pre- and post-intervention, respectively. A paired sample t-test was used to compare medication adherence scores before and after the intervention. The number of patients with good, moderate, and poor adherence at baseline was 261 (34.21%), 254 (33.29%), and 248 (32.50%), respectively. Post-intervention, the patients with good adherence increased (261 (34.21%) to 298 (39.06%)), while with poor adherence decreased (248 (32.5%) to 187 (24.5%)); the average score of medication adherence increased significantly (p < 0.001) from 27.846±4.185 to 29.831±7.065 ().
Table 2 Comparison of Medication Adherence of Patients Pre- and Post-Intervention
Glycemic Control of T2DM Patients
Before the intervention, the number (percentage) of patients with FPG between 4.4 and 7.0 mmol/L and HbA1c<7% were 323 (42.33%) and 184 (24.12%), respectively; 318 cases (41.68%) reached the goal of 2hPG between 4.4 and 10 mmol/L. Patients were divided into four categories according to blood glucose control qualified and unqualified, before and after the intervention, and the chi-square test was used for comparison between groups. The results showed statistically significant differences to that of post-intervention (P ˂ 0.05), where the number of patients with FPG, 2hPG, and HbA1c reaching the standard was 409(53.06%), 372(48.75%), and 223(29.23%), respectively ().
Table 3 Comparison of the Glycemic Control of T2DM Patients Pre- and Post-Intervention
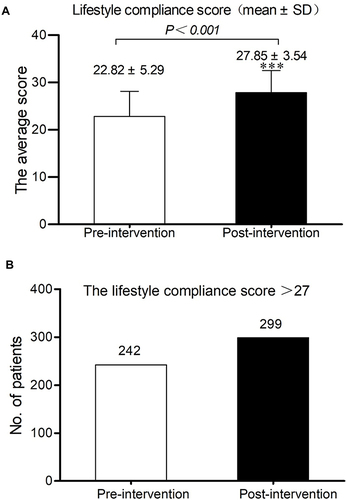
Lifestyle Compliance of T2DM Patients
After the pharmacist-led interventions, the number of patients with a lifestyle compliance score of more than 27 increased from 242 to 299, and the average score of patients’ lifestyle compliance increased from 22.82±5.29 to 27.85±3.54. An Independent sample T-test was used to compare the changes in lifestyle compliance scores before and after pharmacists’ intervention, and the results were a significant statistical difference (p < 0.001) ().
Factors Influencing Medication Adherence
Patients were divided into 2 groups, one was with good to moderate adherence and the other was patients with poor adherence. Our results show that gender, age, BMI, smoking, monthly income, blood glucose monitoring, duration of hypoglycemic drug used, use of medications empirically, following the doctor’s advice to visit, and lifestyle compliance were the significant influencing factors (p < 0.05) according to univariate analysis (Supplementary Table S3). To reduce the effect of confounding factors, the factors identified above were further analyzed by binary logistic regression. As shown in , BMI, use of medications empirically, following the doctor’s advice to visit, and lifestyle compliance were the factors showing a significant influence on medication adherence after controlling other variables. Use of medications empirically (occasionally (OR 3.066, 95% CI 2.069–4.543); often (OR 2.984, 95% CI 1.107–8.044)), occasionally following the doctor’s advice to visit (OR 2.129, 95% CI 1.079–4.202) and lifestyle compliance score of less than 18 (OR 2.835, 95% CI 1.094–7.346) were positively correlated with the risk of poor medication adherence. BMI displayed a negative effect on the risk of poor adherence (OR 0.643, 95% CI 0.437–0.945).
Table 4 Binary Logistic Regression Analysis of Risk Factors of Medication Adherence
According to the logistic regression analysis, the adherence probability test result variables were generated, and the probability result variables were drawn into receiver operating characteristic (ROC) curves to predict adherence results. The area under the ROC curve was 0.716 (range 0.7–0.9), indicating the model with good predictive value. At the same time, the model showed a certain explanatory ability since the significance p-value of the model was <0.001. Furthermore, the model was also found to display high prediction accuracy (correct prediction samples accounted for 72.1% of all the samples).
Discussion
Medication adherence directly influences glycemic control and clinical consequences, with suboptimal glycemic control leading to vascular complications. Non-adherence to medication therapy remains a challenge to achieving optimal clinical outcomes. Our study provides data for getting the whole picture of the current status of medication adherence and glycemic control in patients with type 2 diabetes in Beijing. To the best of our knowledge, this was the first prospective study from Beijing that proved the value of pharmacist-led interventions on medication adherence in T2DM patients. Although a few studies had assessed adherence in T2DM patients, they were either cross-sectional studies,Citation28–31 or retrospective studiesCitation32,Citation33 and none of them had to consider the effect of pharmacist-led interventions. Our findings highlighted the importance of pharmacist-led interventions in T2DM patients, which were consistent with those of previous studies.Citation34,Citation35
We found that the overall glycemic control with HbA1c ˂ 7% at baseline was 24.12%, higher than that reported in a previous study in China, where the control rate of HbA1c was 19.5%.Citation7 In 2011, a multicenter cross-sectional study of 238,639 T2DM patients in China showed that 31.78% of the patients had achieved the goal of HbA1<7.0%.Citation28 These findings illustrated that there was no significant improvement in glycemic control of Chinese T2DM patients over the past 10 years, although the variations between studies can be partially explained by differences in sample size, regional distribution, and study design. Therefore, it is urgently required to strengthen the interventions on medication adherence of T2DM patients and improve glycemic control. Non-adherence to medication can result in poor glycemic control,Citation36 as also observed in our study. Pharmacist-led interventions should be encouraged in the treatment of non-adherence T2DM patients, and this strategy should be further promoted and applied. With the implementation of graded diagnosis and treatment political strategy in China, chronic disease management is sinking into the community. How to take advantage of this opportunity, give full play to the professional advantages of family pharmacists, and improve the medication adherence and glycemic control of T2DM patients deserves our thinking.
The factors leading to non-adherence are complex and can be divided into the patient, social and economic, medication treatment, health providers, and health system-related factors.Citation37 Our study found that BMI, use of medications empirically, following the doctor’s advice to visit, and lifestyle compliance were independent risk factors of non-adherence. Obesity and overweight are two important risk factors for T2DM, and changes in these factors could contribute to the prevalence of total factors.Citation38 A study in the USA found that adults with T2DM who lost weight had better medication adherence as compared to those who gained weight.Citation39 However, our study found that the risk of poor adherence was lower in patients with BMI between 24 and 28 kg/m2 than those with a BMI of <24 kg/m2. There could be several reasons for this finding. First, the prevalence of obesity and overweight increased greatly in China with a mean annual rate of 5.8%, and obesity contributes to the rise of diabetes.Citation40 This trend may be related to the fact that people tend to start taking hypoglycemic drugs when they realize that obesity has greatly affected their health. Second, national diabetes control education is becoming increasingly popular, especially for obese people. The more education this group received, the higher the adherence. Third, some types of hypoglycemic drugs can reduce body weight. Hence, obese patients with diabetes are more willing to accept hypoglycemic drug treatment, and their adherence is relatively high. A study in Papua New Guinea found that age was a risk factor for non-adherence in T2DM patients.Citation36 Our study found no significant effect of age on medication adherence. This could explain by most of the patients in this study being between 60 and 75 years, and the age distribution was uneven.
Logistic regression in our study showed that the patients who always take medicines empirically and occasionally visit doctors were associated with poor medication adherence. These findings suggest that strategies that reduce the use of medications empirically, increase following doctor’s advice to visit, and improve lifestyle compliance, may improve medication adherence.
There were limitations of this study: (1). First, we excluded patients who were unwilling to participate in the study, which may have contributed to the bias in the study population. (2). Second, adherence assessment questions were based on patients’ subjective recollection, and may be biased. In addition, the blood glucose measurement results of some patients were based on self-report and were not validated through biomarkers or other checks, which would affect the accuracy of the study results. (3). Third, there may be some deviation in assessing overall glycemic control when the HbA1c level is <7.0%. Glycemic control should include FPG, non-FPG, and HbA1c.Citation8 In our study, although we collected FPG, 2hPG, and HbA1c, HbA1c <7.0% was selected as the overall glycemic control. HbA1c is the best index used to prove the effect of glycemic control in clinical trials, and can reflect the average blood sugar level in the last three months.Citation8 Both the American Diabetes Diagnosis and Treatment Guidelines and Chinese Diabetes Diagnosis and Treatment GuidelinesCitation8 recommend that the control target value of HbAlc in adult non-gestational diabetes patients is <7.0%. Although there are limitations in the method of assessing overall glycemic control, a consistent threshold is preferred for comparison throughout the study. (4). Fourth, the study focused on statistical significance and was unable to determine whether differences in outcomes represented minimal clinically important differences. Finally, there may be unmeasured confounding variables in our study, which could bias the results. For example, we did not survey information about the patient’s drug and medical costs, which were found to be financial barriers to medication adherence.Citation41
Conclusion
The medication adherence and glycemic control of T2DM patients in Beijing were currently suboptimal, and they could be significantly improved by pharmacist-led interventions. Pharmacist-led interventions should be encouraged in the management of T2DM. Our findings suggest that strategies that reduce the use of medications empirically, increase following doctor’s advice to visit and improve lifestyle compliance, may improve medication adherence. Given that this study was based on patient self-reported adherence and blood glucose monitoring results, the recall bias with self-reported results needs further objective data to verify.
Abbreviations
T2DM, Type 2 Diabetes Mellitus; FPG, Fasting plasma glucose; 2hPG, 2-h postprandial plasma glucose; HbA1c, Glycated hemoglobin; QMAGCR, Medication Adherence and Glycemic Control Rate of T2DM; BMI, Body mass index.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author Zhigang Zhao upon reasonable request.
Ethics Approval and Informed Consent
The research was in accordance with the Declaration of Helsinki. The study was approved by the Ethics Committee of Beijing Tiantan Hospital, the reference number KY2020-085-02. Informed written consent has been obtained from each patient after a full explanation of the purpose and nature of all procedures used.
Consent for Publication
All data generated or analyzed during this study are included in this published article and Supplementary Tables. We confirm that the details of any tables, figures, or data can be published and that the person(s) providing consent have been shown the article contents to be published.
Disclosure
Dr Xiaohan Xu and Rongsheng Zhao reports grants from clinical Pharmacy Research fund of Beijing Pharmaceutical Society, during the conduct of the study. Dr Rongsheng Zhao reports grants from Peking University Third Hospital, during the conduct of the study. The authors declare that they have no other competing interests in this work.
Acknowledgments
We thank Peking University third hospital, Xuanwu Hospital Capital Medical University, Beijing Shijitan Hospital, Beijing Tongren Hospital, Beijing Space Center Hospital, Beijing Aviation General Hospital, Beijing Hospital, Beijing People’s Hospital of Daxing, Beijing Yangfangdian Hospital, Beijing Fengtai Hospital, Fengtai Traditional Chinese Medicine Hospital, Beijing Fengtai Maternal and Child Health Care Hospital, Beijing Anzhen Hospital, Tiantan Community Health service center, Yongding Institutes, Beijing Huairou hospital, Beijing Youan Hospital and Beijing Shunyi hospital, Shunyi airport hospital, China petroleum exploration and development research institute clinics, Capital Normal University Hospital, China Meteorological Administration Hospital, Three Rooms Community Health Service Center, of Beijing university Hospital, Tsinghua University Hospital, Dongcheng Yongwai Community Health Service Center, Majiapu Community Health Service Center, Beijing Institute of Technology Community Health Service Center, Wangfu Traditional Chinese and Western medicine hospital, Xibeiwang Community Health Service Center, Community Health Service Center of Capital Normal University, Beijing Language and Culture University Hospital, etc. For continuous support, assistance, and cooperation, we thank all pharmacists who participated in the study.
Additional information
Funding
References
- Ali MK, Pearson-Stuttard J, Selvin E, Gregg EW. Interpreting global trends in type 2 diabetes complications and mortality. Diabetologia. 2022;65(1):3–13. doi:10.1007/s00125-021-05585-2
- Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet. 2017;389(10085):2239–2251. doi:10.1016/S0140-6736(17)30058-2
- Wang Z, Wu Y, Wu J, et al. Trends in prevalence and incidence of type 2 diabetes among adults in Beijing, China, from 2008 to 2017. Diabet Med. 2021;38(9):e14487. doi:10.1111/dme.14487
- Li Y, Teng D, Shi X, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. 2020;369:m997. doi:10.1136/bmj.m997
- Ma R. Epidemiology of diabetes and diabetic complications in China. Diabetologia. 2018;61(6):1249–1260. doi:10.1007/s00125-018-4557-7
- Patel S, Abreu M, Tumyan A, Adams-Huet B, Li X, Lingvay I. Effect of medication adherence on clinical outcomes in type 2 diabetes: analysis of the SIMPLE study. BMJ Open Diabetes Res Care. 2019;7(1):e761. doi:10.1136/bmjdrc-2019-000761
- Dong Q, Huang J, Liu S, et al. A survey on glycemic control rate of type 2 diabetes mellitus with different therapies and patients’ satisfaction in China. Patient Prefer Adherence. 2019;13:1303–1310. doi:10.2147/PPA.S198908
- Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin J Diabetes Mellitus. 2021;13(4):315–409.
- Dal Canto E, Ceriello A, Ryden L, et al. Diabetes as a cardiovascular risk factor: an overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol. 2019;26(2_suppl):25–32. doi:10.1177/2047487319878371
- Viigimaa M, Sachinidis A, Toumpourleka M, Koutsampasopoulos K, Alliksoo S, Titma T. Macrovascular complications of type 2 diabetes mellitus. Curr Vasc Pharmacol. 2020;18(2):110–116. doi:10.2174/1570161117666190405165151
- Rao KSS, Kaptoge S, Thompson A, et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. 2011;364(9):829–841.
- Georgakis MK, Harshfield EL, Malik R, et al. Diabetes mellitus, glycemic traits, and cerebrovascular disease: a Mendelian randomization study. Neurology. 2021;96(13):e1732–e1742. doi:10.1212/WNL.0000000000011555
- Thipsawat S. Early detection of a diabetic nephropathy in patient with type 2 diabetes mellitus: a review of the literature. Diab Vasc Dis Res. 2021;18(6):1476901544. doi:10.1177/14791641211058856
- Vujosevic S, Aldington SJ, Silva P, et al. Screening for diabetic retinopathy: new perspectives and challenges. Lancet Diabetes Endocrinol. 2020;8(4):337–347. doi:10.1016/S2213-8587(19)30411-5
- Nanayakkara N, Curtis AJ, Heritier S, et al. Impact of age at type 2 diabetes mellitus diagnosis on mortality and vascular complications: systematic review and meta-analyses. Diabetologia. 2021;64(2):275–287. doi:10.1007/s00125-020-05319-w
- Beckman JA, Creager MA. Vascular complications of diabetes. Circ Res. 2016;118(11):1771–1785. doi:10.1161/CIRCRESAHA.115.306884
- Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–1589. doi:10.1056/NEJMoa0806470
- Feldman BS, Cohen-Stavi CJ, Leibowitz M, Hoshen MB, Singer SR, Bitterman H. Defining the role of medication adherence in poor glycemic control among a general adult population with diabetes. PLoS One. 2014;9(9):e108145. doi:10.1371/journal.pone.0108145
- Capoccia K, Odegard PS, Letassy N. Medication adherence with diabetes medication: a systematic review of the literature. Diabetes Educ. 2016;42(1):34–71. doi:10.1177/0145721715619038
- Presley B, Groot W, Pavlova M. Pharmacy-led interventions to improve medication adherence among adults with diabetes: a systematic review and meta-analysis. Res Social Adm Pharm. 2019;15(9):1057–1067. doi:10.1016/j.sapharm.2018.09.021
- Sartori AC, Rodrigues LT, Lopes CT, Picinin BM, Yamaguchi MU. Educational intervention using whatsapp on medication adherence in hypertension and diabetes patients: a randomized clinical trial. Telemed J E Health. 2020;26(12):1526–1532. doi:10.1089/tmj.2019.0305
- Zhuang Q, Chen F, Wang T. Effectiveness of short message service intervention to improve glycated hemoglobin control and medication adherence in type-2 diabetes: a meta-analysis of prospective studies. Prim Care Diabetes. 2020;14(4):356–363. doi:10.1016/j.pcd.2019.09.007
- Ting CY, Ahmad ZAS, Lim CJ, Abd JA, Ting RS, Ting H. Effectiveness of a pharmacist-led structured group-based intervention in improving medication adherence and glycaemic control among type 2 diabetes mellitus patients: a randomized controlled trial. Res Social Adm Pharm. 2021;17(2):344–355. doi:10.1016/j.sapharm.2020.03.026
- Hirsch JD, Kong N, Nguyen KT, Cadiz CL, Zhou C, Bajorek SA. Improved patient-reported medication adherence, patient satisfaction, and glycemic control in a collaborative care pharmacist-led diabetes “tune-up” clinic. Int J Environ Res Public Health. 2021;18:17. doi:10.3390/ijerph18179242
- Kocarnik BM, Liu CF, Wong ES, Perkins M, Maciejewski ML, Yano EM. Does the presence of a pharmacist in primary care clinics improve diabetes medication adherence? Bmc Health Serv Res. 2012;12:391. doi:10.1186/1472-6963-12-391
- Alfian SD, van Boven J, Abdulah R, Sukandar H, Denig P, Hak E. Effectiveness of a targeted and tailored pharmacist-led intervention to improve adherence to antihypertensive drugs among patients with type 2 diabetes in Indonesia: a cluster randomised controlled trial. Br J Clin Pharmacol. 2021;87(4):2032–2042. doi:10.1111/bcp.14610
- Fu M, Hu J, Cai X. Effectiveness of a community-based diabetes self-management intervention for Chinese adults with type 2 diabetes: a pilot study. Int J Nurs Pract. 2015;21(Suppl 2):132–140. doi:10.1111/ijn.12373
- Ji LN, Lu JM, Guo XH, Yang WY, Weng JP, Jia WP. Glycemic control among patients in China with type 2 diabetes mellitus receiving oral drugs or injectables. Bmc Public Health. 2013;13:602. doi:10.1186/1471-2458-13-602
- Huang J, Ding S, Xiong S, Liu Z. Medication adherence and associated factors in patients with type 2 diabetes: a structural equation model. Front Public Health. 2021;9:730845. doi:10.3389/fpubh.2021.730845
- Lee CS, Tan J, Sankari U, Koh Y, Tan NC. Assessing oral medication adherence among patients with type 2 diabetes mellitus treated with polytherapy in a developed Asian community: a cross-sectional study. BMJ Open. 2017;7(9):e16317. doi:10.1136/bmjopen-2017-016317
- Wu P, Liu N. Association between patients’ beliefs and oral antidiabetic medication adherence in a Chinese type 2 diabetic population. Patient Prefer Adherence. 2016;10:1161–1167. doi:10.2147/PPA.S105600
- Wang FC, Chang W, Nie SL, Shen BX, He CY, Zhao WC. Predicting medication nonadherence risk in the Chinese type 2 diabetes mellitus population - establishment of a new risk nomogram model: a retrospective study. J Int Med Res. 2021;49(9):675863866.
- Guo Z, Zheng L, Fu M, et al. Effects of the full coverage policy of essential medicines on inequality in medication adherence: a longitudinal study in Taizhou, China. Front Pharmacol. 2022;13:802219. doi:10.3389/fphar.2022.802219
- Bukhsh A, Tan XY, Chan KG, Lee LH, Goh BH, Khan TM. Effectiveness of pharmacist-led educational interventions on self-care activities and glycemic control of type 2 diabetes patients: a systematic review and meta-analysis. Patient Prefer Adherence. 2018;12:2457–2474. doi:10.2147/PPA.S180256
- Shao H, Chen G, Zhu C, et al. Effect of pharmaceutical care on clinical outcomes of outpatients with type 2 diabetes mellitus. Patient Prefer Adherence. 2017;11:897–903. doi:10.2147/PPA.S92533
- Pihau-Tulo ST, Parsons RW, Hughes JD. An evaluation of patients’ adherence with hypoglycemic medications among Papua New Guineans with type 2 diabetes: influencing factors. Patient Prefer Adherence. 2014;8:1229–1237. doi:10.2147/PPA.S66655
- Marzec LN, Maddox TM. Medication adherence in patients with diabetes and dyslipidemia: associated factors and strategies for improvement. Curr Cardiol Rep. 2013;15(11):418. doi:10.1007/s11886-013-0418-7
- Mokdad AH, Ford ES, Bowman BA, et al. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289(1):76–79. doi:10.1001/jama.289.1.76
- Grandy S, Fox KM, Hardy E. Association of weight loss and medication adherence among adults with type 2 diabetes mellitus: SHIELD (study to help improve early evaluation and management of risk factors leading to diabetes). Curr Ther Res Clin Exp. 2013;75:77–82. doi:10.1016/j.curtheres.2013.06.004
- Wang M, Xu PS, Liu W, et al. Prevalence and changes of BMI categories in China and related chronic diseases: cross-sectional National Health Service Surveys (NHSSs) from 2013 to 2018. EClinicalMedicine. 2020;26:100521. doi:10.1016/j.eclinm.2020.100521
- Cong M, Chaisson J, Cantrell D, Mohundro BL, Carby M, Ford M. Association of co-pay elimination with medication adherence and total cost. Am J Manag Care. 2021;27(6):249–254.