Abstract
Background
Patients with type 2 diabetes have poor medication adherence. Medication literacy is one of the influencing factors of medication adherence among patients with type 2 diabetes. However, the mechanism by which medication literacy affects medication adherence among patients with type 2 diabetes is unclear. The aim of this study was to verify the mediating role of self-efficacy in the relationship between medication literacy and medication adherence.
Methods
A total of 402 patients with type 2 diabetes were enrolled in this study. The Chinese versions of the Medication Literacy Scale, the Self-Efficacy for Appropriate Medication Use Scale and the Morisky Medication Adherence Scale-8 were used in the survey. Pearson correlation analysis was used to find correlations among medication literacy, self-efficacy and medication adherence. The PROCESS macro (Version 4.1) with Model 4 for SPSS was used to verify the mediating role of self-efficacy.
Results
Twenty-four percent of the participants had poor medication adherence. Self-efficacy and medication literacy (r=0.499, p < 0.01) and medication adherence (r=0.499, p < 0.01) were significantly and positively correlated. Self-efficacy partially mediated the relationship between medication knowledge and medication adherence among patients with type 2 diabetes, accounting for 36.7% of the total effect.
Conclusion
Self-efficacy had a partial mediating effect on the relationship between medication literacy and medication adherence among patients with type 2 diabetes. Self-efficacy should be improved through effective measures to increase patients’ confidence in adherence to antihyperglycemic drugs.
Introduction
Diabetes mellitus is a major health burden worldwide and its prevalence is increasing. There were an estimated 536.6 million people with diabetes worldwide in 2021 and this is expected to increase to 783.2 million by 2045.Citation1 Patients with type 2 diabetes account for 90% of all patients with diabetes.Citation2 In addition, global health expenditure related to diabetes was estimated at US $966 billion in 2021 and is projected to increase to US $1045 billion by 2045.Citation1 Therefore, the prevention and control of type 2 diabetes is an urgent problem to be solved in current health care.
Glycemic control plays a crucial role in reducing the cost of diabetes treatment and preventing complications.Citation3 Lifestyle modification is an important measure to control blood glucose. Measures include moderate exercise, a healthy diet, blood glucose monitoring, and adherence to medication. Medication adherence is an important way to achieve glycemic control, which requires patients to take medication as planned for a long time. However, medication nonadherence is very common among patients with diabetes.
Patients with type 2 diabetes have poor medication adherence. Medication adherence refers to the extent to which patients take their medications correctly and as prescribed by their physicians.Citation4 Poor adherence to oral antihyperglycemic drugs is common.Citation5 Due to the long duration and complexity of medication, patients with type 2 diabetes frequently forget to take their medications and have difficulty adhering to them. Pooled rates of nonadherence to antidiabetic medications were 43.4% in low - and middle-income countries.Citation6 In North Africa, the combined proportion of nonadherence among patients with type 2 diabetes was 38%.Citation7 Education level, social security coverage, treatment education, drug cost, socioeconomic level, duration of disease, unbalanced diabetic diet, female sex, family support and age are related factors to adherence.Citation7 Poor medication adherence can lead to many adverse outcomes. Poor medication adherence is associated with higher HbA1c levels and lower quality of life,Citation8,Citation9 as well as with adverse outcomes such as morbidity, mortality, and increased health care costs.Citation10 Therefore, it is urgent to identify the factors influencing medication adherence and develop effective interventions.
Medication literacy may be an influencing factor of medication adherence among patients with type 2 diabetes. Medication literacy is defined as
The degree to which individuals can access, understand, communicate, calculate and process patient-specific information about medications to make informed medication and health decisions in order to use their medications safely and effectively, regardless of how the content is provided. (e.g. written, oral, and visual)Citation11
The latest research has added “digital information” to the definition of medication literacy, which enriches the connotation of medication literacy.Citation12 Among patients with hypertension and coronary heart disease, medication literacy is an influencing factor of medication adherence.Citation13,Citation14 In addition, a study noted that limited health literacy is one of the common barriers to treatment adherence among patients with type 2 diabetes.Citation15 Illness perception is also significantly associated with medication adherence among patients with type 2 diabetes.Citation16 However, broad health literacy and similar illness perception are not substitutes for medication literacy. Medication literacy, as a comprehensive concept of patients’ medication ability, may be related to medication adherence among patients with type 2 diabetes, but the specific mechanism is still unclear, which needs further research.
Medication self-efficacy may mediate the relationship between medication literacy and medication adherence. Self-efficacy refers to patients’ beliefs about their ability to follow a prescribed medication regimen to improve health outcomes and is considered an important component of diabetes education programs.Citation17 A previous study showed that self-efficacy directly affects medication adherence among patients with type 2 diabetes.Citation18 Having a greater sense of self-efficacy is necessary for better medication adherence.Citation19 In addition, medication self-efficacy is found to mediate the relationship between health literacy and medication adherence among patients with type 2 diabetes.Citation20 Patients with higher health literacy may develop higher levels of medication self-efficacy, which in turn may lead to higher levels of diabetes medication adherence and lower HbA1c levels.Citation20 Self-efficacy is also found to mediate and moderate the relationship between medication beliefs and adherence among patients with type 2 diabetes.Citation21 Participants with lower general harm medication beliefs are likely to have higher self-efficacy and higher levels of medication adherence.Citation21 In addition, Fisher proposed the Information-Motivation-Behavioral Skills (IMB) model in 1996, which states that behavior is influenced by information, motivation, and behavioral skills, with self-efficacy playing an important role as an important factor in behavioral skills.Citation22 For this study, medication literacy could directly influence medication adherence behaviors among patients with type 2 diabetes or indirectly by increasing self-efficacy. Considering that medication literacy is the specific manifestation of health literacy in the field of medication, self-efficacy may be an important mediating factor in the relationship between medication literacy and medication adherence among patients with type 2 diabetes.
Few studies have investigated the role of self-efficacy in mediating medication literacy and medication adherence among patients with type 2 diabetes. Exploring the role of self-efficacy in the relationship between medication literacy and medication adherence is helpful to understand the specific influencing mechanism of medication literacy and to develop effective interventions to improve medication adherence of patients with type 2 diabetes. Therefore, this study aimed to explore the mediating effect of self-efficacy between medication literacy and medication adherence among patients with type 2 diabetes.
Methods
Study Design
This cross-sectional study was conducted from October 2022 to January 2023 in four general hospitals and four community healthcare centers in Hunan Province, China.
Participants
Outpatients with type 2 diabetes diagnosed by endocrinologists according to the Guideline for the Prevention and Treatment of Type 2 Diabetes Mellitus in China (2020 edition)Citation23 were recruited by purposive sampling method. The above guidelines for the diagnosis of diabetes are typical diabetes symptoms with random blood glucose ≥ 11.1 mmol/L, or fasting blood glucose ≥ 7.0 mmol/L, or 2-h oral glucose tolerance test (2-h OGTT) blood glucose ≥ 7.0 mmol/L, or glycated hemoglobin (HbA1C) ≥ 6.5%. The purposive sampling method was used to perform a survey study with a smaller sample with certain characteristics, including a small number of subjects selected from the majority of potential subjects according to specific conditions. In this study, sampling was based on the characteristics of patients with type 2 diabetes who received outpatient services. The inclusion criteria were as follow: (1) age 18 years or older; (2) diagnosis of type 2 diabetes by an endocrinologist; (3) basic verbal communication skills; and (4) understanding of the study purpose and process and consent to participate in this study. The exclusion criteria were as follow: (1) other serious diseases, such as cancer, and acute myocardial infarction; and (2) a diagnosed of psychiatric disorders that affect the patient’s ability to communicate and respond according to the International Classification of Diseases guidelines and the current use of medication, such as those for schizophrenia, and bipolar disorder. Written informed consent was obtained from all participants.
Procedures
Five master’s students who were trained in the questionnaire were employed as researchers to collect data in this study. Eligible patients were invited to participate in this study. Patients were provided with information about the content and purpose of this study, and informed of the survey procedure and the principle of anonymity. Participants completed the questionnaire independently after signing the informed consent form. Illiterate participants were informed verbatim of the questionnaire by the researcher and their answers were recorded. All questionnaires were retrieved immediately after completion by the participants, and were checked for missing information by the researcher. If missing information was present, participants were asked to complete it.
Materials
Sociodemographic Data and Clinical Characteristics
A self-designed questionnaire was used to collect the sociodemographic and clinical characteristics of the participants, including age, gender, body mass index (BMI), education level, marital status, annual income, residence area, medical insurance, employment status, smoking, drinking, exercise, disease duration, therapy method, number of antihyperglycemic drugs taken, HbA1c and family history.
The Chinese Version of the Medication Literacy Scale
The Medication Literacy Assessment in English and Spanish (MedLitRxSE) was developed by Sauceda, a professor at the University of Texas, and his team.Citation24 The scale is specifically used to assess the medication literacy of patients, and has good reliability and validity. It is the best assessment tool for medication literacy at present.Citation25 The scale consists of four scenarios: injectable medication for diabetes, medication for children, antibiotic use, and over-The-counter and supplementary prescriptions. Case 1 includes the following five questions: According to this prescription list, how many times every day does your friend need to inject this medication? Please look at this prescription and syringe and tell me how many units of arginine biosynthetic human insulin injection your friend should take in the morning with this syringe and indicate the scale on the syringe. If your friend has run out of the medication, which doctor should he contact to write a new prescription for the medication based on the above prescription? Using the medication instructions, into which parts of the body can your friend inject insulin? According to the above medication instructions, what is the angle of subcutaneous insulin injection? The scale includes 14 items, and correct responses are scored with 1 point and incorrect responses with 0 point. The total score is calculated by adding the scores of each item, which ranges from 0 to 14. A score of > 10 is considered adequate medication literacy, a score of 4 to 10 is considered moderate, and a score of < 4 is considered inadequate. In 2016, MedLitRxSE was translated into Chinese by Zheng et al.Citation26 The test-retest reliability of the Chinese version of the Medication Literacy Assessment Scale is 0.885, the split-half reliability is 0.840, and the correlation coefficient between each item of the scale and the total score of the scale is 0.427–0.587.Citation26
Chinese Version of the Morisky Medication Adherence Scale-8 (C-MMAS-8)
The Morisky Medication Adherence Scale-8 (MMAS-8) was developed by Morisky and his research team.Citation27 The scale has been used to assess the level of medication adherence of patients, while being concise, practical and cost-effective. The scale has eight items, with yes and no answers to the first seven items and a 5-point Likert scale for the final question. The first seven items relate to patients’ medication adherence behaviors: Do you sometimes forget to take your medication? Have you reduced or stopped taking your medication without telling your doctor? Do you forget to take your medication with you when you go out for long periods of time? Did you take your medication yesterday? Have you stopped taking your medication? Do you find it difficult to adhere to your treatment plan? The total score of the scale ranges from 0 to 8, with higher scores indicating greater medication adherence. A score of 8 represents high adherence, a score of < 6 is considered low adherence, and a score of ≥ 6 and < 8 is considered moderate adherence. The Chinese version of the Morisky Medication Adherence Scale-8 was translated by Yan and the reliability and validity were tested in patients with myocardial infarction.Citation28 The Cronbach’s α of the C-MMAS-8 is 0.77, and the pretest and posttest correlation coefficient is 0.88.Citation28 The scale has been widely used in the measurement of medication adherence for various types of patients, such as those with hypertension, elderly individuals with multimorbidity and those with type 2 diabetes.Citation13,Citation29,Citation30 Each item of the MMAS-8 used in this study had only language differences from the original English version.
The Self-Efficacy for Appropriate Medication Use Scale (SEAMS)
The Self-efficacy for Appropriate Medication Use Scale was developed by Risser and his research team.Citation31 The SEAMS can be used to measure the self-efficacy of rational medication taking among patients with various chronic diseases, and it is suitable for testing the confidence of adherence to medication. The Cronbach’s α coefficient of the scale is 0.89.Citation31 The scale includes 13 items and asks subjects to report their confidence in adhering to reasonable and correct medication under 13 circumstances. It assesses 2 dimensions of medication self-efficacy, self-efficacy to take medication in difficult situations (eg, when your doctor changes your medication, when you find that the medication you bought again differs from your previous medication in the way you take it, when you need to take several different types of medication each day) and self-efficacy to continue taking medication when the medication environment is uncertain (eg, when you are out of town, when you are busy one day, when no one reminds you). A 3-point Likert scale was used to score the scale, with a score of 1 indicating no confidence, 2 indicating little confidence, and 3 indicating a great deal of confidence. The total score of the scale is the sum of the scores of each item, with higher scores indicating better medication self-efficacy. The SEAMS was translated into Chinese by Dong et al in 2015.Citation32 The Chinese version of the SEAMS has good internal consistency (Cronbach’s α= 0.826–0.915) and validity.Citation32
The pretest was conducted before the formal survey. Twelve participants were able to complete the questionnaire within 15 minutes and indicated that they were able to understand its content. Therefore, the research instrument used in this study was comprehensible and applicable to the study participants.
Ethical Considerations
This study complied with the Declaration of Helsinki and was approved by the Research Ethics Committee of the Third Xiangya Hospital, Central South University (Project number: 22241). All participants signed an informed consent form and agreed to participate in this study. All participants had the right to decline to participate in this study and opt out at any time.
Statistical Analysis
SPSS (version 26.0, Chicago, IL, United States) software was used to analyze all the data. Means and standard deviations were used to describe all continuous variables that had a normal distribution, and numbers or percentages were used to describe categorical variables. Two independent sample t-tests or ANOVA were used to compare the scores of medication literacy, self-efficacy, and medication adherence among patients with type 2 diabetes with different demographic and clinical characteristics. Pearson correlation analysis was used to determine the correlation between medication literacy, self-efficacy, and medication adherence. The mediation analysis framework described by Baron and Kenny guided the analysis plan.Citation33 According to this approach, a mediation effect existed if (1) the independent variable (medication literacy) significantly predicted the mediating variable (self-efficacy) (, Path a), (2) the mediating variable (self-efficacy) significantly predicted the dependent variable (medication adherence) (, Path b), and (3) the independent variable (medication literacy) significantly predicted the dependent variable (medication adherence) (, Path c). Path c’ represents the direct influence of the independent variable on the dependent variable after controlling for the mediating variable (, Path c’). If the direct effect was not significant, the effect of the mediating variable was a full mediating effect. If the direct effect was significant, the effect of the mediating variable was a partial mediating effect. a*b was used to calculate the mediation effect value, and a*b/c was used to represent the ratio of the mediation effect to the total effect. PROCESS macro (Version 4.1) with Model 4 for SPSS was used to test for mediation effects using 5000 bootstrap samples. Mediation effects were considered to be significant if the 95% bootstrap confidence interval did not include zero. In addition, sociodemographic and clinical characteristics were included in the model as control variables. p <0.05 was considered statistically significant.
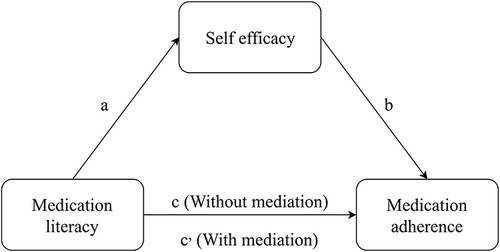
Figure 1 The theoretical framework of this study. (a) Effect of medication literacy on self-efficacy; (b) Effect of self-efficacy on medication adherence; (c) Effect of medication literacy on medication adherence (Without mediation); (c’) Effect of medication literacy on medication adherence (With mediation).
Results
Participants Characteristics
There were 404 participants in this study, 402 completed the survey, and 2 individuals were excluded because they were under the age of 18 or missing information, so the valid response rate of the questionnaire was 99.51%. presents the sociodemographic and clinical characteristics. The proportion of male participants was 61.9%, 90.0% were married, most participants did not smoke (59.0%) and did not drink alcohol (78.9%), and the vast majority of patients (83.1%) had poor HbA1c control.
Table 1 Participants Characteristics (n=402)
Medication Literacy, Self-Efficacy, and Medication Adherence Scores of the Participants
presents the medication literacy, self-efficacy and medication adherence of the participants. The scores for medication literacy of patients of different genders, ages, education levels, marital statuses, residences, employment, medical insurance, economic statuses, and smoking and drinking statuses were significantly different. Differences in age, employment, and exercise may have led to significant variation in medication adherence. Participants scored 9.44±3.28 on medication literacy, 33.81±2.65 on self-efficacy, and 6.49±1.28 on medication adherence (). Among the participants, 20 (5.0%) had insufficient medication literacy, 203 (50.5%) had moderate medication literacy, and 179 (44.5%) had adequate medication literacy. There were 97 (24.1%) participants with poor medication adherence, 216 (53.7%) with moderate medication adherence, and 89 (22.1%) with high medication adherence.
Table 2 Medication Literacy, Self-Efficacy, and Medication Adherence Scores of the Participants (n=402)
Table 3 Descriptive Statistics and Correlations of Medication Literacy, Self-Efficacy, and Medication Adherence (n=402)
Correlations Among Medication Literacy, Self-Efficacy, and Medication Adherence
Medication literacy scores were positively correlated with self-efficacy scores (r=0.499, p < 0.001), medication literacy scores were positively correlated with medication adherence scores (r=0.227, p < 0.001), and self-efficacy scores were positively correlated with medication adherence scores (r=0.392, p < 0.001) ().
The Mediating Effect of Self-Efficacy on Medication Literacy and Medication Adherence
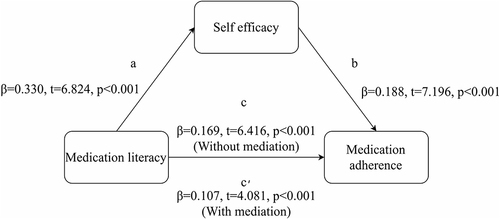
The mediating role of self-efficacy in medication literacy and medication adherence is presented in . The results showed that medication literacy significantly positively predicted self-efficacy (β=0.330, p < 0.001) and medication adherence (β=0.107, p < 0.001). Self-efficacy significantly positively predicted medication adherence (β= 0.188, p < 0.001). Medication literacy had a significant positive effect on medication adherence (β= 0.169, p < 0.001) after controlling for sociodemographic and clinical data. The mediating effect value was 0.062, and the mediating effect accounted for 36.7% of the total effect (). The regression coefficients of each path were significant, so self-efficacy had a partial mediating effect on the relationship between medication literacy and medication adherence.
Table 4 Summary of the Mediating Effects of Self-Efficacy
Figure 2 The mediating effect of self-efficacy on the relationship between medication literacy and medication adherence. (a) Effect of medication literacy on self-efficacy; (b) Effect of self-efficacy on medication adherence; (c) Effect of medication literacy on medication adherence (Without mediation); (c’) Effect of medication literacy on medication adherence (With mediation).
Discussion
Medication adherence plays an important role in improving health outcomes among patients with type 2 diabetes. Studies show that the improvement in medication adherence contributes to the reduction in HbA1c levels.Citation34,Citation35 In addition, good medication adherence can reduce the risk of all-cause mortality and hospitalization among patients with type 2 diabetes.Citation36 However, the prevalence of medication nonadherence is high among patients with type 2 diabetes. The pooled rate of low adherence among patients with type 2 diabetes in Malaysia is 34.2%.Citation37 Therefore, improving medication adherence is very important for patients with type 2 diabetes, and improving strategies to improve medication adherence is an important issue for nursing staff.
The percentage of participants with poor medication adherence was 24.1%. Participants in our study had slightly better medication adherence than the rest of the world.Citation6,Citation7,Citation37 However, only 22.1% of the participants had high medication adherence. Therefore, the medication adherence of patients with type 2 diabetes urgently needs to be improved. In addition, this study found significant differences in medication adherence among participants by age, employment, and exercise. Previous studies have shown that patient demographics are the influencing factors of medication adherence among patients with type 2 diabetes.Citation38 In a study from Bangladesh, nonadherence was higher among participants who were older, experienced household poverty, smoked cigarettes, and had poor glycemic control.Citation39 Age, marital status, occupation, comorbidities and duration of disease were significantly associated with medication adherence among patients with type 2 diabetes in eastern Saudi Arabia.Citation40 Therefore, patients with the characteristics of old age, unemployment and lack of exercise should be regarded as the key population to improve medication adherence.
The mean medication literacy score of the participants was 9.44±3.28, which is at the top of the medium medication literacy level, and 95.0% of the participants had a moderate or adequate medication literacy level. Most of the participants had good medication literacy. Compared with the medication literacy of patients with coronary heart disease (4.96±4.68) and patients with small cell lung cancer (6.54±2.78),Citation41,Citation42 the medication literacy of patients with type 2 diabetes was better than both. The possible reason is that patients with type 2 diabetes are more familiar with injectable medication for diabetes, and the scenario of injectable medication for diabetes is present in the medication literacy assessment scale. Of course, the medication competencies learned by participants during long-term medication use should also not be overlooked. We also found significant differences in medication literacy scores among participants according to gender, age, education level, marital status, residence area, employment, medical insurance, financial status, and smoking and drinking status. Similar findings are seen in studies of medication literacy among patients with hypertension and acute coronary syndrome.Citation43,Citation44 Therefore, patients with characteristics such as female sex, old age, low education level, and poor economic status are more likely to have insufficient medication literacy. Medical staff should pay attention to patients with the above characteristics.
There was a significant positive correlation between medication literacy and medication adherence among patients with type 2 diabetes. Higher medication literacy was associated with better medication adherence. Medication literacy was also positively correlated with medication adherence among patients with hypertension.Citation13 In addition, self-efficacy was found to be one of the influencing factors of medication adherence. Previous studies similarly showed a significant positive relationship between self-efficacy and adherence,Citation45 and health literacy moderated the relationship between illness perception and adherence among patients with type 2 diabetes.Citation45 Thus, participants with higher self-efficacy are more likely to adhere to their antihyperglycemic drugs. A possible reason for this is that patients with higher self-efficacy have more confidence in their medication adherence.
Self-efficacy plays a partial mediating role in the relationship between medication literacy and medication adherence. Medication literacy, as a comprehensive reflection of patients’ medication ability, may affect patients’ medication behavior in many aspects such as knowledge, attitude, skills and behavior. This study also confirmed that medication literacy is one of the predictors of medication adherence among patients with type 2 diabetes. Among patients with hypertension, medication literacy and annual income explain 15.8% of the variance in medication adherence.Citation13 In addition, the self-efficacy of hypertension patients plays a partial mediating role in the relationship between medication literacy and medication adherence, and the mediating effect accounts for 28.7%.Citation46 This study found that the mediating effect of self-efficacy in medication literacy and medication adherence of patients with type 2 diabetes accounted for 36.7%. In addition, a study found that self-efficacy plays a partial mediating role between health literacy and diabetes medication adherence.Citation20 A study demonstrated that self-efficacy also plays a partial mediating role between health beliefs and HbA1c levels among elderly patients with type 2 diabetes.Citation47 Self-efficacy plays a key mediating role in the process of medication literacy affecting medication adherence. A possible explanation is that participants with poor medication literacy feel less confident in medication adherence and are more likely to show low self-efficacy. Thus, participants with poor medication literacy may develop self-doubt with low self-efficacy and a sense of powerlessness about adherence to their medication. Therefore, self-efficacy is an important mediator of medication adherence among patients with type 2 diabetes and its role should be harnessed to improve medication adherence among these patients worldwide.
Information, motivation, and behavioral skills in the IMB model are important factors to promote behavior change. Information is a prerequisite for behavior change and implementation, motivation is the patient’s attitude toward health behavior based on his or her own perceptions, behavioral skills are objective skills that the patient has mastered to effectively implement behavior change in this area, and all three components contribute to behavior change when adequately present.Citation48 In this study, medication literacy affected medication adherence both directly and indirectly through the mediating role of self-efficacy. This result confirms that the IMB theory can be used to explain the pathway of medication literacy on medication adherence among patients with type 2 diabetes, and the IMB model has been proven to predict medication adherence behavior among patients with type 2 diabetes.Citation49 One study assessed barriers to medication adherence among patients with type 2 diabetes based on the IMB model,Citation50 and other studies have been conducted on telephone counseling interventions based on the IMB model that significantly improved self-efficacy and self-management among patients with type 2 diabetes.Citation51 Therefore, it is reasonable for the IMB model to be used to explain medication adherence among patients with type 2 diabetes, and the results of this study provide a research breakthrough for improving medication adherence among these patients.
Self-efficacy can be used to mediate medication literacy and medication adherence among patients with type 2 diabetes. A randomized controlled trial demonstrated that education based on health literacy constructs significantly improved self-efficacy among people with type 2 diabetes.Citation52 Another randomized controlled trial showed that an intervention based on the health action process approach significantly improved medication adherence among patients with type 2 diabetes by improving self-efficacy.Citation53 Therefore, improving medication literacy while increasing self-efficacy among patients with type 2 diabetes can improve their medication adherence. Previous studies have noted that greater self-efficacy is necessary for better medication adherence.Citation19 In addition, low self-efficacy can increase the risk of hospitalization.Citation54 Improving self-efficacy among patients with type 2 diabetes has a positive direct impact on both self-care and quality of life.Citation55 Therefore, measures to improve self-efficacy among patients with type 2 diabetes should be adopted. Previous studies demonstrated that peer support and mobile apps for diabetes management can help people with type 2 diabetes improve their self-efficacy.Citation56,Citation57 Improved medication adherence through self-efficacy contributes to greater reductions in Hba1c levels, lower microvascular and/or macrovascular outcomes, hospitalization rates and lower total healthcare expenditures.Citation58
This study has some limitations. First, self-report instruments were used to measure medication adherence, which may have led to an overestimation of adherence. Future studies could use objective data as an indicator of medication adherence. Second, this was a cross-sectional study using a purposive sampling method, which did not allow us to infer causal relationships among medication literacy, self-efficacy and medication adherence. Finally, this study was conducted in only one region, which limits the generalizability of the findings. Future multicenter studies are warranted.
Conclusion
Medication adherence is poor among patients with type 2 diabetes, and medication literacy and self-efficacy are factors influencing medication adherence. Moreover, self-efficacy has a partial mediating effect on the relationship between medication literacy and medication adherence among patients with type 2 diabetes, accounting for 36.7% of the total effect. In the process of improving patients’ medication literacy and medication adherence, self-efficacy should also be improved through effective measures to increase patients’ confidence in adhering to the use of antihyperglycemic drugs. Therefore, healthcare professionals should begin to improve medication literacy and self-efficacy among patients with type 2 diabetes as a way to improve medication adherence.
Disclosure
The authors report no conflicts of interest in this work.
References
- Sun H, Saeedi P, Karuranga S, et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. doi:10.1016/j.diabres.2021.109119
- Standl E, Khunti K, Hansen TB, Schnell O. The global epidemics of diabetes in the 21st century: current situation and perspectives. Eur J Prev Cardiol. 2019;26(2_suppl):7–14. doi:10.1177/2047487319881021
- Kikkawa R. Chronic complications in diabetes mellitus. Br J Nutr. 2000;84(2):S183–5. doi:10.1079/096582197388653
- Kim J, Combs K, Downs J, Tillman F. Medication adherence: the elephant in the room. Pharmacist. 2018;43(1):30–34.
- Quisel T, Foschini L, Zbikowski SM, Juusola JL. The association between medication adherence for chronic conditions and digital health activity tracking: retrospective analysis. J Med Internet Res. 2019;21(3):e11486. doi:10.2196/11486
- Azharuddin M, Adil M, Sharma M, Gyawali B. A systematic review and meta-analysis of non-adherence to anti-diabetic medication: evidence from low- and middle-income countries. Int J Clin Pract. 2021;75(11):e14717. doi:10.1111/ijcp.14717
- Achouri MY, Tounsi F, Messaoud M, Senoussaoui A, Ben Abdelaziz A. Prevalence of poor medication adherence in type 2 diabetics in North Africa. Systematic review and meta-analysis. Tunis Med. 2021;99(10):932–945. doi:10.1186/s12863-014-0134-3
- Alshehri KA, Altuwaylie TM, Alqhtani A, Albawab AA, Almalki AH. Type 2 diabetic patients adherence towards their medications. Cureus. 2020;12(2):e6932. doi:10.7759/cureus.6932
- Saudi RA, Abbas RA, Nour-Eldein H, Sayed Ahmed HA. Illness perception, medication adherence and glycemic control among primary health-care patients with type 2 diabetes mellitus at Port Said City, Egypt. Diabetol Int. 2022;13(3):522–530. doi:10.1007/s13340-021-00567-6
- Alkomos MF, Mendez D, Mazzei-Pifano D, et al. Patients’ reasons for missing scheduled clinic appointments and their solutions at a major urban-based academic medical center. J Community Hosp Intern Med Perspect. 2020;10(5):426–430. doi:10.1080/20009666.2020.1796903
- Pouliot A, Vaillancourt R, Stacey D, Suter P. Defining and identifying concepts of medication literacy: an international perspective. Res Social Adm Pharm. 2018;14(9):797–804. doi:10.1016/j.sapharm.2017.11.005
- Neiva Pantuzza LL, Nascimento ED, Crepalde-Ribeiro K, et al. Medication literacy: a conceptual model. Res Social Adm Pharm. 2022;18(4):2675–2682. doi:10.1016/j.sapharm.2021.06.003
- Shi S, Shen Z, Duan Y, Ding S, Zhong Z. Association between medication literacy and medication adherence among patients with hypertension. Front Pharmacol. 2019;10:822. doi:10.3389/fphar.2019.00822
- Zheng F, Ding S, Lai L, et al. Relationship between medication literacy and medication adherence in inpatients with coronary heart disease in Changsha, China. Front Pharmacol. 2019;10:1537. doi:10.3389/fphar.2019.01537
- Pourhabibi N, Mohebbi B, Sadeghi R, et al. Determinants of poor treatment adherence among patients with type 2 diabetes and limited health literacy: a scoping review. J Diabetes Res. 2022;2022:2980250. doi:10.1155/2022/2980250
- Bilondi SS, Noghabi AD, Aalami H. The relationship between illness perception and medication adherence in patients with diabetes mellitus type II: illness perception and medication adherence. J Prev Med Hyg. 2021;62(4):E966–e971. doi:10.15167/2421-4248/jpmh2021.62.4.2277
- Al-Khawaldeh OA, Al-Hassan MA, Froelicher ES. Self-efficacy, self-management, and glycemic control in adults with type 2 diabetes mellitus. J Diabetes Complications. 2012;26(1):10–16. doi:10.1016/j.jdiacomp.2011.11.002
- Huang J, Ding S, Xiong S, Liu Z. Medication adherence and associated factors in patients with type 2 diabetes: a structural equation model. Front Public Health. 2021;9:730845. doi:10.3389/fpubh.2021.730845
- Huang YM, Shiyanbola OO, Chan HY, Smith PD. Patient factors associated with diabetes medication adherence at different health literacy levels: a cross-sectional study at a family medicine clinic. Postgrad Med. 2020;132(4):328–336. doi:10.1080/00325481.2020.1749499
- Huang YM, Shiyanbola OO, Chan HY. A path model linking health literacy, medication self-efficacy, medication adherence, and glycemic control. Patient Educ Couns. 2018;101(11):1906–1913. doi:10.1016/j.pec.2018.06.010
- Wu J, Shen J, Tao Z, Song Z, Chen ZL. Self-efficacy as moderator and mediator between medication beliefs and adherence in elderly patients with type 2 diabetes. Patient Prefer Adherence. 2023;17:217–226. doi:10.2147/ppa.S382362
- Fisher JD, Fisher WA, Misovich SJ, Kimble DL, Malloy TE. Changing AIDS risk behavior: effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychol. 1996;15(2):114–123. doi:10.1037//0278-6133.15.2.114
- Society CD. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin J Diabetes Mellitus. 2021;2021:315–409.
- Sauceda JA, Loya AM, Sias JJ, Taylor T, Wiebe JS, Rivera JO. Medication literacy in Spanish and English: psychometric evaluation of a new assessment tool. J Am Pharm Assoc. 2012;52(6):e231–40. doi:10.1331/JAPhA.2012.11264
- Gentizon J, Hirt J, Jaques C, Lang PO, Mabire C. Instruments assessing medication literacy in adult recipients of care: a systematic review of measurement properties. Int J Nurs Stud. 2021;113:103785. doi:10.1016/j.ijnurstu.2020.103785
- Zheng F, Zhong Z, Ding S, Luo A, Liu Z. [Modification and evaluation of assessment of medication literacy] (药物素养评估量表的编译与评价). Zhong Nan da Xue Xue Bao Yi Xue Ban. 2016;41(11):1226–1231. Chinese. doi:10.11817/j.issn.1672-7347.2016.11.019
- Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10(5):348–354. doi:10.1111/j.1751-7176.2008.07572.x
- Yan J, You LM, Yang Q, et al. Translation and validation of a Chinese version of the 8-item Morisky medication adherence scale in myocardial infarction patients. J Eval Clin Pract. 2014;20(4):311–317. doi:10.1111/jep.12125
- Wang W, Luan W, Zhang Z, Mei Y. Association between medication literacy and medication adherence and the mediating effect of self-efficacy in older people with multimorbidity. BMC Geriatr. 2023;23(1):378. doi:10.1186/s12877-023-04072-0
- Yang H, Wu F, Gui M, Cheng Y, Zhang L. The role of medication adherence in the association between depressive symptoms and quality of life in older adults with type 2 diabetes mellitus. BMC Geriatr. 2023;23(1):196. doi:10.1186/s12877-023-03929-8
- Risser J, Jacobson TA, Kripalani S. Development and psychometric evaluation of the Self-efficacy for Appropriate Medication Use Scale (SEAMS) in low-literacy patients with chronic disease. J Nurs Meas. 2007;15(3):203–219. doi:10.1891/106137407783095757
- Dong XF, Liu YJ, Wang AX, Lv PH. Psychometric properties of the Chinese version of the Self-Efficacy for Appropriate Medication Use Scale in patients with stroke. Patient Prefer Adherence. 2016;10:321–327. doi:10.2147/ppa.S101844
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi:10.1037//0022-3514.51.6.1173
- Alison C, Anselm S. The effectiveness of diabetes medication therapy adherence clinic to improve glycaemic control among patients with type 2 diabetes mellitus: a randomised controlled trial. Med J Malaysia. 2020;75(3):246–253.
- Tominaga Y, Aomori T, Hayakawa T, Morisky DE, Takahashi K, Mochizuki M. Relationship between medication adherence and glycemic control in Japanese patients with type 2 diabetes. Die Pharmazie. 2018;73(10):609–612. doi:10.1691/ph.2018.8587
- Khunti K, Seidu S, Kunutsor S, Davies M. Association between adherence to pharmacotherapy and outcomes in type 2 diabetes: a meta-analysis. Diabetes Care. 2017;40(11):1588–1596. doi:10.2337/dc16-1925
- Teng CL, Chan CW, Wong PS. Medication adherence of persons with type 2 diabetes in Malaysia: a scoping review and meta-analysis. J ASEAN Fed Endocr Soc. 2022;37(1):75–82. doi:10.15605/jafes.037.01.14
- Wibowo M, Yasin NM, Kristina SA, Prabandari YS. Exploring of determinants factors of anti-diabetic medication adherence in several regions of Asia - a systematic review. Patient Prefer Adherence. 2022;16:197–215. doi:10.2147/ppa.S347079
- Khan II, Pulock OS, Pinky SD, et al. Treatment noncompliance level among patients with type 2 diabetes mellitus: a hospital based cross-sectional study in Bangladesh. PLoS One. 2022;17(9):e0271107. doi:10.1371/journal.pone.0271107
- Alfulayw MR, Almansour RA, Aljamri SK, et al. Factors contributing to noncompliance with diabetic medications and lifestyle modifications in patients with type 2 diabetes mellitus in the eastern province of Saudi Arabia: a cross-sectional study. Cureus. 2022;14(11):e31965. doi:10.7759/cureus.31965
- Du R, Yang H, Zhou H, et al. The relationship between medication literacy and skin adverse reactions in non-small-cell lung cancer patients undergoing targeted EGFR-TKI therapy. BMC Cancer. 2022;22(1):491. doi:10.1186/s12885-022-09599-w
- Qiao L, Ding S, Zhong Z, Liu X, Lai L, Zheng F. Association between social support and medication literacy in Chinese patients with coronary heart disease. Front Cardiovasc Med. 2021;8:705783. doi:10.3389/fcvm.2021.705783
- Ma G, Luo A, Shen Z, Duan Y, Shi S, Zhong Z. The status of medication literacy and associated factors of hypertensive patients in China: a cross-sectional study. Intern Emerg Med. 2020;15(3):409–419. doi:10.1007/s11739-019-02187-0
- Zhong Z, Zheng F, Guo Y, Luo A. Medication literacy in a cohort of Chinese patients discharged with acute coronary syndrome. Int J Environ Res Public Health. 2016;13(7):720. doi:10.3390/ijerph13070720
- Shiyanbola OO, Unni E, Huang YM, Lanier C. The association of health literacy with illness perceptions, medication beliefs, and medication adherence among individuals with type 2 diabetes. Res Social Adm Pharm. 2018;14(9):824–830. doi:10.1016/j.sapharm.2017.12.005
- Shen Z, Shi S, Ding S, Zhong Z. Mediating effect of self-efficacy on the relationship between medication literacy and medication adherence among patients with hypertension. Front Pharmacol. 2020;11:569092. doi:10.3389/fphar.2020.569092
- Zhang A, Wang J, Wan X, et al. Mediation effect of self-efficacy between health beliefs and glycated haemoglobin levels in elderly patients with type 2 diabetes mellitus: a cross-sectional study. Patient Prefer Adherence. 2022;16:3015–3026. doi:10.2147/ppa.S388967
- Fisher JD, Amico KR, Fisher WA, Harman JJ. The information-motivation-behavioral skills model of antiretroviral adherence and its applications. Curr HIV/AIDS Rep. 2008;5(4):193–203. doi:10.1007/s11904-008-0028-y
- Mayberry LS, Osborn CY. Empirical validation of the information-motivation-behavioral skills model of diabetes medication adherence: a framework for intervention. Diabetes Care. 2014;37(5):1246–1253. doi:10.2337/dc13-1828
- Nelson LA, Wallston KA, Kripalani S, LeStourgeon LM, Williamson SE, Mayberry LS. Assessing barriers to diabetes medication adherence using the information-motivation-behavioral skills model. Diabetes Res Clin Pract. 2018;142:374–384. doi:10.1016/j.diabres.2018.05.046
- Sayin Kasar K, Duru Asiret G, Kutmec Yilmaz C, Canlar Ş. The effect of model-based telephone counseling on HbA1c and self-management for individuals with type 2 diabetes: a randomized controlled trial. Prim Care Diabetes. 2022;16(1):41–48. doi:10.1016/j.pcd.2021.09.005
- Ağralı H, Akyar İ. The effect of health literacy-based, health belief-constructed education on glycated hemoglobin (HbA1c) in people with type 2 diabetes: a randomized controlled study. Prim Care Diabetes. 2022;16(1):173–178. doi:10.1016/j.pcd.2021.12.010
- Ranjbaran S, Shojaeizadeh D, Dehdari T, Yaseri M, Shakibazadeh E. The effectiveness of an intervention designed based on health action process approach on diet and medication adherence among patients with type 2 diabetes: a randomized controlled trial. Diabetol Metab Syndr. 2022;14(1):3. doi:10.1186/s13098-021-00773-x
- Zhao H, Johnson JA, Al Sayah F, Soprovich A, Eurich DT. The association of self-efficacy and hospitalization rates in people with type-2 diabetes: a prospective cohort study. Diabetes Res Clin Pract. 2018;143:113–119. doi:10.1016/j.diabres.2018.07.011
- Fereydouni F, Hajian-Tilaki K, Meftah N, Chehrazi M. A path causal model in the association between self-efficacy and self-care with quality of life in patients with type 2 diabetes: an application of the structural equation model. Health Sci Rep. 2022;5(2):e534. doi:10.1002/hsr2.534
- Liang D, Jia R, Zhou X, et al. The effectiveness of peer support on self-efficacy and self-management in people with type 2 diabetes: a meta-analysis. Patient Educ Couns. 2021;104(4):760–769. doi:10.1016/j.pec.2020.11.011
- Zhai Y, Yu W. A mobile app for diabetes management: impact on self-efficacy among patients with type 2 diabetes at a community hospital. Med Sci Monit. 2020;26:e926719. doi:10.12659/msm.926719
- Evans M, Engberg S, Faurby M, Fernandes J, Hudson P, Polonsky W. Adherence to and persistence with antidiabetic medications and associations with clinical and economic outcomes in people with type 2 diabetes mellitus: a systematic literature review. Diabetes Obes Metab. 2022;24(3):377–390. doi:10.1111/dom.14603
