Abstract
Purpose
Long-acting inhalers are the mainstay maintenance therapy for stable chronic obstructive pulmonary disease (COPD) management. The aim of this study was to assess adherence to inhalers among adults with COPD in China and to develop strategies to improve adherence for the next step.
Patients and Methods
A cross-sectional study was conducted among 246 adult patients with COPD using long-acting inhalers to explore different demographic characteristics, disease characteristics and medication regimens. Adherence to inhalers was assessed using the Medication Adherence Report Scale (MARS).
Results
Among the 246 patients included in the present study, 93 (37.80%) had good adherence, while 153 (62.20%) had poor adherence. From the comparison of patients with good and poor adherence, we found that the course of disease and education background had a significant effect on adherence (p < 0.05). Among the LAMA therapy group, inhaled tiotropium bromide spray (Ingelheim am Rhein, Germany) with active release technology had better adherence than inhaled tiotropium bromide powder (Ingelheim am Rhein, Germany) (p < 0.05). Moreover, COPD patients with good adherence had better pulmonary function and fewer moderate or severe exacerbations in the past year (p < 0.05).
Conclusion
The factors affecting the use of inhalers in patients with stable COPD are complicated. Medical staff should select appropriate inhalers according to the patient’s disease status and duration and provide medication education to improve adherence.
Introduction
Chronic obstructive pulmonary disease (COPD) is a clinically frequent and common chronic disease characterized by incompletely reversible airflow restriction and persistent respiratory symptoms.Citation1 Currently, COPD is the third leading cause of death and the fifth leading economic burden in the world,Citation2,Citation3 and the spirometry-defined prevalence of COPD in China in 2015 was 8.6%.Citation4 The Global Initiative for Chronic Obstructive Lung Disease recommends that the treatment of choice for long-term control of COPD is long-acting inhalers therapy.Citation5 Three main classes of drugs are commonly used alone and in combination to manage COPD: long-acting beta-adrenoceptor agonists (LABA), long-acting muscarinic antagonists (LAMA) and inhaled corticosteroids (ICS). Poor adherence to inhaled therapy has now been clearly established as a main risk factor for the exacerbation of COPD and the effect on the hospitalization rate.Citation6,Citation7 However, the adherent group had a lower all-cause cost and a lower COPD-related cost versus those of the poor-adherent group.Citation8 Although there are some studies focusing on the adherence and factors affecting inhaled medications in COPD patients,Citation9,Citation10 they are inconclusive, and comprehensive systematic studies are lacking. Therefore, we collected data from patients with stable COPD to assess the patient adherence by the MARS and investigated the differences in patient adherence under different demographic characteristics, disease characteristics and medication regimens. We further analyzed the possible reasons for poor adherence, and made suggestions for improvement, meanwhile, aiming to provide some reference implications for the management strategies of patients with stable COPD.
Materials and Methods
Study Objects
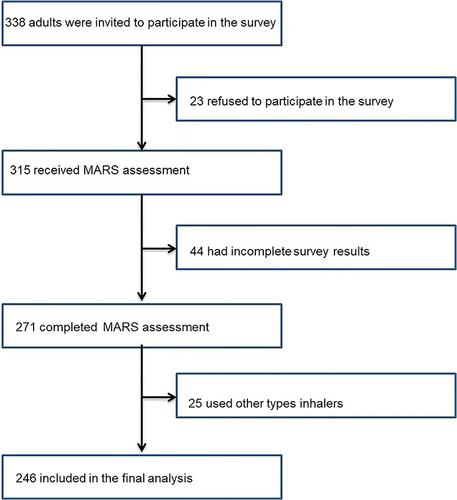
This cross-sectional study was conducted in the First Hospital of Changsha from November 2020 to February 2021. The study enrolled patients ≥40 years old with spirometric confirmation of COPDCitation5 who had used any type of inhaler for more than 1 month. We excluded individuals diagnosed of other chronic respiratory diseases such as active pulmonary tuberculosis, lung tumor and pulmonary interstitial diseases, and were unable to communicate due to mental illness, impaired consciousness, psychological disorder, cognitive impairment, or other reasons. COPD patients who completed study period were finally analyzed as shown in . The 246 patients used dry powder inhaler (DPIs) and soft mist inhaler (SMI). In this real-world study, we evaluated inhaler adherence and determinants of high adherence in patients.
Methods
A cross-sectional study was used to explore the differences in adherence among patients with different demographic characteristics, disease characteristics and medication regimens. After signing the informed consent forms, general information about the patients was registered, including name, gender, age, weight, education level, economic status, personal history, past history and duration of illness, number of hospitalizations due to acute exacerbation of COPD in the last year. All patients underwent spirometry and the post-bronchodilator percent predicted forced expiratory volume in the one second (FEV1) was used to determine disease severity.Citation5 Two clinical pharmacists conducted all of the interviews and assessed patients’ adherence to inhalers according to the MARS, which is designed as questions based on negative statements to limit social desire bias,Citation11 had good interitem correlation (Cronbach alpha = 0.85 and 0.86, respectively) and good test-retest reliability (r = 0.65, P < 0.001).Citation12 Responses were scored on a 5-point Likert scale, ranging from always (1 point) to never (5 points). The total MARS score was calculated as the average of 10 specific scores. Good adherence was considered if the MARS score was greater than 4.5 which had a sensitivity of 51% and a specificity of 68%, and poor adherence if the MARS score was less than 4.5.Citation11
This study was conducted in accordance with all relevant tenets of the Declaration of Helsinki. The protocol was approved by the Medical Ethics Committee (registration number kx-2020060) of the First Hospital of Changsha (China).
Statistical Analysis
According to the content of the questionnaire, data entry was performed using EpiData 3.0 software. After auditing, the data were imported into the SPSS 20.0 statistical package for statistical verification, sorting and analysis. Data with normal distribution and homogeneous variance were tested by t-test; uneven variance by corrected t-test; non-normal distribution by Mann Whitney U-test; count data by Chi square test or Fisher exact test. All tests were bilateral. Differences were considered statistically significant when p-values < 0.05.
Results
Subject Characteristics
In the study, 246 patients received inhalers with stable COPD completed the baseline survey and completed the MARS questionnaire. Among 246 patients, mean age was 70.9±9.6 years, and the majority of patients were male (82.1%). Mean duration of COPD was 7.8±6.6 years, 73.6% had two or more acute exacerbations in the previous year, and 58.9% had a history of smoking. Of the included patients, only 50 (20.3%) had graduated from high school or above, 22.4% of the households’ average monthly income was higher than 3000 yuan (). The mean MARS score was 3.97±0.83. While 93 patients (37.80%) with MARS scores ≥4.5 had good adherence, 153 patients (62.20%) had poor adherence. There were no differences in gender, age, weight, income, smoking history and comorbidities between the two groups. However, there were statistically significant differences (p < 0.05) on education background, the duration of illness, moderate or severe exacerbation history in the past year and severity of airflow obstruction between them ().
Table 1 Demographic Features of the Adherence in Patients with Stable COPD
Inhaled Medication
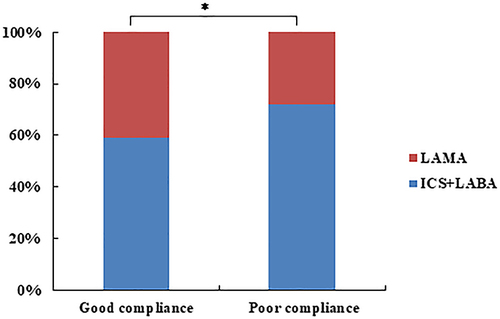
We divided the data into ICS/LABA and LAMA subgroups according to their pharmacological effects to analyze whether there was a difference in patient adherence if different categories of drugs were inhaled. According to , there was a statistical difference when using different inhalers (χ2=4.26, p=0.04), and the proportion of patients with good adherence using LAMA drugs was larger. ICS/LABA drugs include Budesonide and Formoterol Fumarate Powder for Inhalation (II) (Sodertalje, Sweden), and Salmeterol Xinafoate and Fluticasone Propionate Powder for Inhalation (Evreux, France). The study found no significant differences between the MARS scores of patients using budesonide formoterol and salmeterol fluticasone (). Surprisingly, among the LAMA therapy group, there was a statistically significant difference in terms of adherence between inhaled tiotropium bromide powder (Ingelheim am Rhein, Germany) and tiotropium bromide spray (Ingelheim am Rhein, Germany), with better adherence when using the spray ().
Table 2 The Adherence of Patients Who Inhaled Different Drugs in ICS/LABA
Table 3 The Adherence of Patients Who Inhaled Different Drugs in LAMA
Medication Adherence Rates
The majority of the patients (62.2%) reported low overall adherence. The MARS scores of the poor adherence patients ranged from 1 to 5, with a mean score of 3.45±0.62. Approximately half of the patients reported that they sometimes or often occurred the following situations: used the inhalers when needed (54.2%) [median (IQR): 3 (2)], or used them when they felt breathless (46.4%) [median (IQR): 4 (1)], or used them as a reserve if other treatment did not work (44.4%) [median (IQR); 4 (2)], or tried to avoid using them (53.6%) [median (IQR): 3 (1)]. In the medication dose adherence evaluation items, more than 50% participants reported that forgot to take the inhalers (66%) [median (IQR): 3 (1)], or took it less than instructed (61.4%) [median (IQR); 3 (1)], or stopped taking the inhalers for a while (62.1%) [median (IQR): 3 (2)], miss out a dose (53.6%) [median (IQR); 3 (1)]. The percentages of patients’ engagements in each action of non-adherence and the mean score for each item are shown in .
Table 4 The Percentage of Patients’ Engagements in Each Action of Adherence and the Mean Score for Each Item*
Discussion
Adherence and Disease Regression
In this study, we analyzed the adherence to inhalers by using MARS score, a previously validated method, among patients with stable COPD. To our knowledge, there were no published studies using the similar method to assess the adherence to inhalers in China. Only 37.8% of the participants reported high adherence to inhalers. Although poor adherence to inhalers is common in the literature, the rate of poor adherence in this study was inconsistent with those reported in other studies.Citation11–14 Adherence with long-acting inhalers is considered to be the foundation of stable COPD treatment.Citation15,Citation16 As our research results show, there were differences in the number of acute exacerbations and degree of airflow limitation severity in COPD patients with different adherence to inhalers. Previous research concluded similarly that subjects with complete adherence to therapy had a significantly lower FEV1 compared to those with low adherence.Citation17 Inhaled medication adherence is used to evaluate the extent to which patients take medication according to medical advice, including whether they are able to take medication consistently at the time, frequency and dose required by medical personnel, without changing medication at will.Citation16,Citation18 Therefore, it is necessary to analyze the factors influencing adherence to inhaled agents in stable COPD patients and to explore the possible and effective strategies to improve adherence.
Factors Influencing the Adherence
Medication adherence is influenced by several factors such as socioeconomic, health-care system, medical condition, therapy-related and patient-related.Citation19 Consistent with previous similar research,Citation14 we found that the patient’s education background and the duration of illness had significant difference on the adherence with inhalers (p < 0.05). However, other observational studies considered no correlation was found between reported adherence and some of the demographic information.Citation20 We believe that stable COPD patients with higher education levels may have a better understanding of COPD and are more likely to adhere to inhalers to reduce COPD episodes. Patients with poor adherence to inhalers generally had a longer COPD course of disease in our study. With the prolongation of disease and the repeated use of inhaled preparations, their expectations for using inhalers to control the progression of the disease may decline, resulting in being reluctant to take medication as prescribed or even refusing medication. It has been reported that treatment adherence in patients with chronic airway disease gradually decreases with prolonged disease duration.Citation21 For these patients, medical staff need optimize treatment strategies and implement medication education covering the period of hospitalization and after discharge, then track through telephone follow-up, mobile phone applications and other new mobile management modes to further improve patients’ treatment adherence.Citation5,Citation18
The inhaler device used to play a central role in the management of COPD.Citation16,Citation22 Our analysis suggested that there were significant differences of patients adherence between inhaled ICS/LABA versus LAMA (p < 0.05) and tiotropium bromide powder for inhalation versus tiotropium bromide spray (p < 0.05). The potential reason is that tiotropium bromide spray uses a drug release technology to generate a fine, slow-moving mist, which only requires a lower inhalation velocity but need coordination actuation and inhalation, results in higher lung deposition (up to 50%) and oropharyngeal deposition lower, achieves better adherence, compared to pressurized metered-dose inhalers (pMDIs) and DPI.Citation16,Citation23,Citation24 Some studies showed that patients using a pMDI inhaled ICS/LABA were 28% less likely to experience a COPD exacerbation-related hospital readmission within 60 days postdischarge compared with those using a DPI (OR: 0.72, 95% CI: 0.52–0.99, P < 0.05),Citation25 but our research had not been involved yet. In summary, inspiratory flow rate is a factor that physicians need to consider when choosing inhalers for their patients.Citation26 In the future, we will conduct continuous research to obtain more conclusions.
MARS Score
Our study showed that the mean MARS score was 3.97±0.83, which assessed our patients adherence to inhalers, indicating low adherence, which was close to that reported by other studies.Citation11,Citation20 In this study, approximately half of the patients reported that they sometimes or often used the inhalers when needed or felt breathless, or used them as a reserve if other treatment did not work, or tried to avoid using them. They did not understand the necessity for adherence to therapy, indicating that a lack of understanding of the management knowledge of stable COPD may be the main reason for poor adherence to treatment.Citation27 For COPD patients, it is extremely important for telling them to adhere to standardized treatment during the stable phase.Citation5 In addition, in the medication dose adherence evaluation items, more than 50% participants reported that forgot to take the inhalers, or took it less than instructed, or stopped taking the inhalers for a while, miss out a dose. Our data showed a higher rate than other studies.Citation28,Citation29 It also reflects patients in our study both intentional and unintentional non-adherence. On the one hand, current evidence suggests that the beliefs about medicines are more predictive of intentional non-adherence than of unintentional non-adherence.Citation30 It is necessary to consider using a patient accepted approach to repeatedly promote and educate patients about COPD disease knowledge and medication to help them build confidence in disease control. COPD guidelines recommend that inhaler training should be continually assessed at subsequent clinic visits. Where necessary, retraining should be provided.Citation5 Adherent patients were significantly more often trained with a demonstration, who were more often checked and more confident that the correct dose was taken, compared with nonadherent patients.Citation31,Citation32 On the other hand, about the unintentional non-adherence, electronic dose monitoring was found to improve treatment adherence in chronic diseases.Citation33 Charles et al assessed patients using the MDI with an audiovisual reminder function (AVRF) were significantly less likely to “dose dump” (take multiple doses in a short time period) than the control group.Citation34 Yotaro Takaku considered it is necessary to repeat at least three times of instructions to achieve effective inhalation skills in COPD patients.Citation35
This study also has some limitations: (1) there are many factors affecting inhalers adherence to COPD treatment such as health-care system, patients’ general level of cognitive functioning, multi drug treatment and the techniques in using inhalation devices, which were not all included in, so logistic regression analysis was not done. (2) The MARS was based on patient reports, captured patient’s general behaviors at the time of the baseline interview, and may have overestimated medication adherence due to issues with recall. Patients were from older adults with COPD, more likely to experience problems with memory than younger patients without these conditions. (3) The present study was limited by the small sample size. However, the relevant results can still be used as baseline data to provide a reference for further regulating stable COPD management and improving patients’ treatment adherence.
Conclusion
In conclusion, overall adherence to long-acting inhalers for COPD is poor. Poor adherence to inhalers in COPD patients is likely associated with many factors, such as lower education level, long duration of disease and the type of inhalers. Moreover, COPD patients with poor adherence had worse pulmonary function and more episodes. This study suggests that for patients with stable COPD, proper inhaler device should be selected for patients. The findings of this study could help develop interventions designed to increase adherence to long-acting inhaled medications. Medical personnel should focus on the disease itself and the importance of medication adherence, implement medication education covering the whole period and strengthen follow-up of patients to track their condition and medication use, thus improving adherence with inhaler use and improving the quality of life of patients with stable COPD.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
We would like to express our gratitude to Prof. Rob Horne (© Rob Horne, School of Pharmacy, University College London, Great Britain) and TIAN Qingxiu (The First Affiliated Hospital Of Shandong First Medical University, China), YU Lijun (Chinese Academy of Medical Sciences & Peking Union Medical College, China) for providing the MARS. The study was supported by the Natural Science Foundation of Hunan Province (No. 2021JJ70056), Inclusive Policy and Innovation Environment Construction Project of Hunan Provincial Department of Science and Technology-Clinical Medical Technology Innovation Guidance Project (NO.2021SK53101), Inclusive Policy and Innovation Environment Construction Project of Hunan Provincial Department of Science, Technology-Science Popularization Special Project (NO.2022ZK4170) and Science Popularization Special Project of Hunan Provincial Department of Science and Technology (2022ZK4170).
References
- Labaki WW, Rosenberg SR. Chronic obstructive pulmonary disease. Ann Intern Med. 2020;173(3):ITC17–ITC32. doi:10.7326/AITC202008040
- Stolz D. Chronic obstructive pulmonary disease risk: does genetics hold the answer? Lancet Respir Med. 2020;8(7):653–654. doi:10.1016/S2213-2600(20)30191-0
- Dai J, Yang P, Cox A, Jiang G. Lung cancer and chronic obstructive pulmonary disease: from a clinical perspective. Oncotarget. 2017;8(11):18513–18524. doi:10.18632/oncotarget.14505
- Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet. 2018;391(10131):1706–1717. doi:10.1016/S0140-6736(18)30841-9
- GOLD. From the Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease; 2021. Available from: http://goldcopd.org. Accessed June 12, 2023.
- Wiśniewski D, Porzezińska M, Gruchała-Niedoszytko M, Niedoszytko M, Słomiński JM, Jassem E. Factors influencing adherence to treatment in COPD patients and its relationship with disease exacerbations. Pneumonol Alergol Pol. 2014;82(2):96–104. doi:10.5603/PiAP.2014.0015
- Van Boven JF, Tommelein E, Boussery K, et al. Improving inhaler adherence in patients with chronic obstructive pulmonary disease: a cost-effectiveness analysis. Respir Res. 2014;15(1):66. doi:10.1186/1465-9921-15-66
- Kim JA, Lim MK, Kim K, Park J, Rhee CK. Adherence to inhaled medications and its effect on healthcare utilization and costs among high-grade chronic obstructive pulmonary disease patients. Clin Drug Investig. 2018;38(4):333–340. doi:10.1007/s40261-017-0612-2
- Koehorst-Ter Huurne K, Kort S, van der Palen J, et al. Quality of life and adherence to inhaled corticosteroids and tiotropium in COPD are related. Int J Chron Obstruct Pulmon Dis. 2016;11:1679–1688. doi:10.2147/COPD.S107303
- Jang JG, Lee KH, Chung JH, et al. Assessment of inhaler satisfaction and determinants of high satisfaction among Korean COPD patients. J Korean Med Sci. 2022;37(46):e327. doi:10.3346/jkms.2022.37.e327
- Tangirala NC, O’Conor R, Wolf MS, Wisnivesky JP, Federman AD. Validity of the medication adherence rating scale for adherence to inhaled corticosteroids among older adults with asthma or chronic obstructive pulmonary disease. COPD. 2020;17(1):74–80. doi:10.1080/15412555.2020.1712688
- Cohen JL, Mann DM, Wisnivesky JP, et al. Assessing the validity of self-reported medication adherence among inner-city asthmatic adults: the medication adherence report scale for asthma. Ann Allergy Asthma Immunol. 2009;103(4):325–331. doi:10.1016/s1081-1206(10)60532-7
- Tashkin DP, Fabbri LM. Long-acting beta-agonists in the management of chronic obstructive pulmonary disease: current and future agents. Respir Res. 2010;11(1):149. doi:10.1186/1465-9921-11-149
- Cecere LM, Slatore CG, Uman JE, et al. Adherence to long-acting inhaled therapies among patients with chronic obstructive pulmonary disease (COPD). COPD. 2012;9(3):251–258. doi:10.3109/15412555.2011.650241
- Koehorst-Ter Huurne K, Groothuis-Oudshoorn CG, vanderValk PD, Movig KL, van der Palen J, Brusse-Keizer M. Association between poor therapy adherence to inhaled corticosteroids and tiotropium and morbidity and mortality in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:1683–1690. doi:10.2147/COPD.S161374
- Sorino C, Negri S, Spanevello A, Visca D, Scichilone N. Inhalation therapy devices for the treatment of obstructive lung diseases: the history of inhalers towards the ideal inhaler. Eur J Intern Med. 2020;75(75):15–18. doi:10.1016/j.ejim.2020.02.023
- Humenberger M, Horner A, Labek A, et al. Adherence to inhaled therapy and its impact on chronic obstructive pulmonary disease (COPD). BMC Pulm Med. 2018;18(1):163. doi:10.1186/s12890-018-0724-3
- Jia X, Zhou S, Luo D, Zhao X, Zhou Y, Cui YM. Effect of pharmacist-led interventions on medication adherence and inhalation technique in adult patients with asthma or COPD: a systematic review and meta-analysis. J Clin Pharm Ther. 2020;45(5):904–917. doi:10.1111/jcpt.13126
- World Health Organization. Adherence to long-term therapies: evidence for action; 2003. Available from: http://apps.who.int/medicinedocs/pdf/s4883e/s4883e.pdf. Accessed July 31, 2017.
- Albassam A, Alharbi A, Awaisu A. Assessing adherence to inhaled corticosteroids among adults with asthma in Kuwait using the medication adherence report scale for asthma. Patient Prefer Adherence. 2020;14:963–970. doi:10.2147/PPA.S248655
- Smith IJ, Bell J, Bowman N, Everard M, Stein S, Weers JG. Inhaler devices: what remains to be done? J Aerosol Med Pulm Drug Deliv. 2010;23(Suppl 2):S25–S37. doi:10.1089/jamp.2010.0853
- Mahler DA. The role of inspiratory flow in selection and use of inhaled therapy for patients with chronic obstructive pulmonary disease. Respir Med. 2020;161:105857. doi:10.1016/j.rmed.2019.105857
- Anzueto A, Wise R, Calverley P, et al. The Tiotropium Safety and Performance in Respimat® (TIOSPIR®) trial: spirometry outcomes. Respir Res. 2015;16(1):107. doi:10.1186/s12931-015-0269-4
- Brand P, Hederer B, Austen G, Dewberry H, Meyer T. Higher lung deposition with respimat soft mist inhaler than HFA-MDI in COPD patients with poor technique. Int J Chron Obstruct Pulmon Dis. 2008;3(4):763–770. doi:10.2147/COPD.S3930
- Wittbrodt ET, Millette LA, Evans KA, Bonafede M, Tkacz J, Ferguson GT. Differences in health care outcomes between postdischarge COPD patients treated with inhaled corticosteroid/long-acting β2-agonist via dry-powder inhalers and pressurized metered-dose inhalers. Int J Chron Obstruct Pulmon Dis. 2018;14:101–114. doi:10.2147/COPD.S177213
- González-Torralba F, Baloira A, Abad A, et al. FIDEPOC: consensus on inspiratory flow and lung deposition as key decision factors in COPD inhaled therapy. Int J Chron Obstruct Pulmon Dis. 2022;17:1005–1015. doi:10.2147/COPD.S360938
- Williams LK, Joseph CL, Peterson EL, et al. Patients with asthma who do not fill their inhaled corticosteroids: a study of primary nonadherence. J Allergy Clin Immunol. 2007;120(5):1153–1159. doi:10.1016/j.jaci.2007.08.020
- Horne R, Weinman J. Self regulation and self management in asthma: exploring the role of illness perceptions and treatment beliefs in explaining non-adherence to preventer medication. Psychol Health. 2002;17(1):17–32. doi:10.1080/08870440290001502
- Laforest L, El Hasnaoui A, Pribil C, et al. Asthma patients’ self-reported behaviours toward inhaled corticosteroids. Respir Med. 2009;103(9):1366–1375. doi:10.1016/j.rmed.2009.03.010
- Clifford S, Barber N, Horne R. Understanding different beliefs held by adherers, unintentional nonadherers, and intentional nonadherers: application of the necessity-concerns framework. J Psychosom Res. 2008;64(1):41–46. doi:10.1016/j.jpsychores.2007.05.004
- Price D, Keininger DL, Viswanad B, Gasser M, Walda S, Gutzwiller FS. Factors associated with appropriate inhaler use in patients with COPD - lessons from the REAL survey. Int J Chron Obstruct Pulmon Dis. 2018;13:695–702. doi:10.2147/COPD.S149404
- Jang JG, Kim JS, Chung JH, et al. Comprehensive effects of organized education for patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2019;14:2603–2609. doi:10.2147/COPD.S221673
- Hall RL, Willgoss T, Humphrey LJ, Kongsø JH. The effect of medical device dose-memory functions on patients’ adherence to treatment, confidence, and disease self-management. Patient Prefer Adherence. 2014;8:775–788. doi:10.2147/PPA.S61248
- Charles T, Quinn D, Weatherall M, Aldington S, Beasley R, Holt S. An audiovisual reminder function improves adherence with inhaled corticosteroid therapy in asthma. J Allergy Clin Immunol. 2007;119(4):811–816. doi:10.1016/j.jaci.2006.11.700
- Takaku Y, Kurashima K, Ohta C, et al. How many instructions are required to correct inhalation errors in patients with asthma and chronic obstructive pulmonary disease? Respir Med. 2017;123:110–115. doi:10.1016/j.rmed.2016.12.012