Abstract
Background
Persistence of anti-tumor necrosis factor (TNF) therapy in rheumatoid arthritis (RA) is an overall marker of treatment success.
Objective
To assess the survival of anti-TNF treatment and to define the potential predictors of drug discontinuation in RA, in order to verify the adequacy of current practices.
Design
An observational, descriptive, longitudinal, retrospective study.
Setting
The Hospital Clínico Universitario de Valladolid, Valladolid, Spain.
Patients
RA patients treated with anti-TNF therapy between January 2011 and January 2012.
Measurements
Demographic information and therapy assessments were gathered from medical and pharmaceutical records. Data is expressed as means (standard deviations) for quantitative variables and frequency distribution for qualitative variables. Kaplan–Meier survival analysis was used to assess persistence, and Cox multivariate regression models were used to assess potential predictors of treatment discontinuation.
Results
In total, 126 treatment series with infliximab (n = 53), etanercept (n = 51) or adalimumab (n = 22) were administered to 91 patients. Infliximab has mostly been used as a first-line treatment, but it was the drug with the shortest time until a change of treatment. Significant predictors of drug survival were: age; the anti-TNF agent; and the previous response to an anti-TNF drug.
Limitation
The small sample size.
Conclusion
The overall efficacy of anti-TNF drugs diminishes with time, with infliximab having the shortest time until a change of treatment. The management of biologic therapy in patients with RA should be reconsidered in order to achieve disease control with a reduction in costs.
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory disease that is characterized by persistent synovitis, systemic inflammation, and autoantibodies, particularly rheumatoid factor and antibodies to citrullinated peptide. It is a highly incapacitating disease that can lead to premature death.
The pharmacological treatment of RA is aimed at reducing or minimizing the progression of the disease. Patients require various medications, and on some occasions they do not have a sufficient tolerance or response to disease-modifying antirheumatic drugs. Biologic agents are drugs that are obtained through biotechnological processes, and these have revolutionized the way in which RA is treated and monitored. Anti-tumor necrosis factor (TNF) agents are used with patients who have not responded to disease-modifying antirheumatic drugs.Citation1 However, as many as 50% of patients treated with these drugs either do not respond to them or experience side effects, causing treatment to be stopped. In these cases, the best strategy is still a matter for debate, although trying another anti-TNF is thought to be one good option.Citation2–Citation4
Drug survival is a general marker of the success of a treatment, as it depends on the efficacy of the drug, its side effects, and patient preferences.Citation5 The information available on anti-TNF survival in patients with RA is very limited. Moreover, it may be the case that data from randomized clinical trials are not ideal for studying survival, due to inherent bias in such clinical trials relating to the fundamental characteristics of patients and restrictive selection criteria. As a result, data from clinical trials does not reflect actual clinical practice.Citation6
The main objective of this study was to evaluate anti-TNF treatment survival and to define the factors predictive of drug discontinuation in patients with RA who attended the Pharmacy Service or the Outpatient Department at the Hospital Clínico Universitario de Valladolid (HCUV; Val-ladoid, Spain) and who were given at least one dose of an anti-TNF drug during the study period. The aim was to confirm whether or not current normal clinical practice in terms of the choice of anti-TNF therapy for treating patients with RA is appropriate.
Method
This retrospective, longitudinal, descriptive, observational study on the persistence of anti-TNF therapies used to treat RA was carried out in the Pharmacy Service at the HCUV, over a period of 12 months from January 2011 to January 2012.
All patients aged 18 years or older, diagnosed with RA who went to the Pharmacy or the Outpatient Department, and who were given at least one dose of anti-TNF therapy (infliximab, etanercept, or adalimumab) during the study period were selected, provided that they were treated on an ongoing basis at the HCUV. Each patient’s diagnosis with RA was checked in his or her medical record, using the criteria established by the American College of Rheumatology:Citation7 presence of synovitis in at least one joint, absence of an alternative diagnosis that better explained the synovitis, and achievement of a total score of 6 or greater (of a possible 10) from the individual scores in four domains: number and site of involved joints (score range 0–5), serological abnormality (score range 0–3), elevated acute-phase response (score range 0–1), and symptom duration (two levels; range 0–1). All of the patients signed an informed consent agreement and the study was approved by the Hospital Clínico Universitario de Valladolid Ethics Committee.
Patients whose records were incorrect were excluded from the study. Five patients had a diagnosis other than RA: three had juvenile idiopathic arthritis and two had ankylosing spondylitis. Any patient who died during the study period was also excluded, provided that the cause of death was unrelated to the treatment being studied. Three patients died during the study, but only two of these were excluded, as the third patient died as a result of complications arising from a possible case of severe pancytopenia due to etanercept.Citation8
Two lists of day patients and outpatients suffering from RA also were generated using the program Farmatools® v. 2.4 (Informer Technologies, Inc, Vizcaya, Bilbao, Spain). The information from these two lists was checked against the data in the patients’ medical files, in order to filter out any potential errors. Patients who were to be included in the study were added to an Excel 2007 data table (Microsoft; Redmond, WA, USA) and were identified by their initials and their medical record number. The variables of age and sex were obtained from the information stored in hospital archives. The names of the anti-TNF agents being used, or that had been used, to treat each patient were recorded, along with the time until discontinuation and the reasons for this.
Various sources were used to obtain this data: digital records in the day-patient and outpatient modules of the Farmatools® program; the paper records kept by the Pharmacy Service; and the computerized medical records in the patient histories management program, version 3.95 (Gestión de historias clínicas, Spain). The start date of treatment with each drug and the date of the last dose were recorded. If the end date of treatment was not available, it was taken to be the start date of the next treatment.
The reasons for a change of treatment – side effects, drug not effective – were found in the paper records kept on each patient in the Pharmacy Service and in the computerized medical records in the patient histories management program. If the reason had not been recorded, the patient or his or her doctor was contacted in order to find this information out.
Statistical analysis
The quantitative variables are presented as means (standard deviations [SDs]) and the qualitative variables according to their frequency distribution. Pearson’s chi-square test was used to analyze the association of the qualitative variables. In the case of the number of cells with expected values lower than 5 being greater than 20%, Fisher’s exact test was used, or the likelihood ratio test for variables with more than two categories. Comparisons of qualitative values were carried out using the Student’s t-test or analysis of variance of a factor for independent samples, depending on the case.
The analysis of survival was performed using the Kaplan–Meier method. Comparisons between average survival times were carried out using the log-rank test for cases in which survival curves were proportional; in the cases in which they were not, the Tarone-Ware test was used. The probability of not experiencing any change of treatment over a certain period was calculated from survival tables taking 1 year as an interval.
In addition to the aforementioned survival analyses, a Cox multivariate regression model was generated for the study factors, adjusting the results for age (<60 years versus ≥60 years), sex (men versus women), previous anti-TNF treatment versus naïve, infliximab versus etanercept, and infliximab versus adalimumab. The data were analyzed using the statistical program SPSS v. 20.0 for Windows (IBM Corporation, Armonk, NY, USA). P-values <0.05 were considered to be statistically significant.
Results
During the 1-year study period, 91 patients who had been given a total of 126 treatments were included in the study. The average age of patients at enrollment was 58 years (SD, 12.3 years; range, 29–85 years). Women accounted for 72.5% of patients (ratio of 2.6:1.0), with average ages at the point of inclusion of 54.6 (2.2) and 58.8 (1.5) for men and women, respectively. Almost 50% of patients had been given methotrexate concomitantly. Patient characteristics are shown in .
Table 1 Patient demographics and therapy characteristics
Infliximab was prescribed to 53 patients, whereas 51 patients were given etanercept and 22 were given adalimumab; 64 patients (70%) continued with their initial biologic treatment, without needing to change to a different one. The remaining patients had to change treatment for various reasons. shows the changes that occurred in the treatment of the patients included in the study.
Figure 1 Changes in the treatment of patients included in the study.
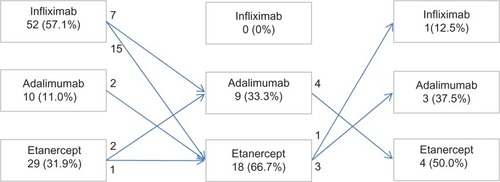
Other non–anti-TNF biologics, such as rituximab, abatacept, and tocilizumab, were also used after anti-TNF therapy had failed, in accordance with the protocol agreed on by the Rheumatology and Pharmacy Services at the HCUV. Certolizumab and golimumab were not used with any patients as these had not been approved by the HCUV’s Pharmacy and Therapeutics Committee.
Kaplan–Meier curves were drawn up to analyze the time until a change in anti-TNF treatment, both in general terms and in terms of subgroups. The analysis was performed for 91 patients, but considering that 27 patients were given two or more different treatments, the same patient could be included in the analysis two or three times, to analyze a different anti-TNF agent each time.
Overall analysis
Statistically significant differences were found in the time until a change in treatment for all three anti-TNF agents in general terms (P = 0.015), as shown in .
Figure 2 Drug survival probabilities for infliximab (n = 53), etanercept (n = 51), and adalimumab (n = 22) in the study population.
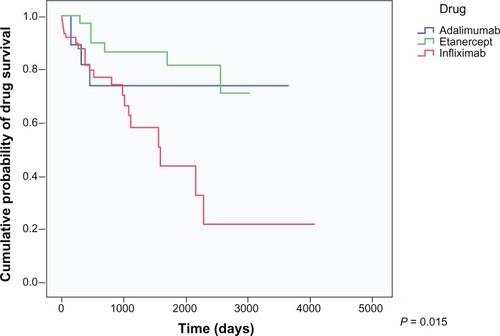
The average time until a change of treatment for infliximab was 1,853.520 (306.88) days. Infliximab was associated with the lowest survival rate, dropping to approximately 20% after 2,200 days.
The average time until a change of treatment for etanercept was 2,561.082 (152.307) days and for adalimumab was 2,769.074 (389.452) days. In terms of survival, etanercept and adalimumab behaved very similarly: they had survival rates of between 75% and 80% during the same time period in which infliximab survival fell to 20%. The overall mean time until a change of treatment for anti-TNF agents was 2,713.058 (202.126) days.
Subgroup analysis
Naïve versus previous anti-TNF treatment
Differences were observed in the time until a change of treatment for all three drugs in naïve patients (P = 0.001) and also in patients who had previously been treated with another anti-TNF therapy (P = 0.000), as shown in .
Figure 3 Drug survival probabilities for adalimumab, etanercept, and infliximab, naïve versus previous anti-TNF treatment.
Abbreviations: n, number; TNF, tumor necrosis factor.
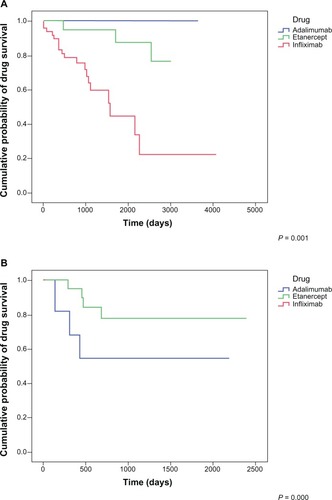
In naïve patients, the average time until a change of treatment for etanercept was greater than that of infliximab, 2,735.677 (152.534) days versus 1,890.816 (310.873) days. It is not possible to draw a comparison with adalimumab because there was only one patient.
Among patients who had already been treated with another anti-TNF agent, the average time until a change of treatment for etanercept was also greater: 1,987.023 (188.054) days, when compared to adalimumab, 1,327.000 (333.219) days. It is not possible to draw a comparison with adalimumab because there was only one patient, who began treatment 26 days before the end of the study, with no discontinuation.
The probability of changing from etanercept to another anti-TNF therapy was very low. The survival tables showed that the cumulative probability of treatment with etanercept being maintained with naïve patients was between 82% and 100%. Among patients who had previously been prescribed another anti-TNF treatment, this probability was lower, as was to be expected, but still high at 78%–95%.
Whereas in naïve patients the probability of treatment with adalimumab being maintained was 100% up to 4 years, among patients who had previously been treated with another anti-TNF agent, the probability of treatment with adalimumab being maintained decreased to 57% after 1 year and then remained the same up to 6 years.
Taking into account the fact that the analysis of infliximab could only be carried out for nonnaïve patients, the probability of treatment being maintained fell over time to 67% after 6 years. Thereafter, the probability of there being no change to treatment remained at 100%.
Sex
When anti-TNF survival in patients with RA was analyzed by sexual subgroups, statistical differences were found (P = 0.036 in men and P = 0.015 in women).
Among women, the longest average time until a change in treatment was for adalimumab, at 3,191.571 (921.327) days, followed by etanercept, 2,659.778 (470.175) days, and infliximab, 1,743.950 (282.907) days.
In men, on the other hand, the longest average time until a change in treatment was for etanercept, at 2,224.926 (214.699) days, followed by infliximab, 1,545.687 (328.521) days. In contrast to the findings with women, adalimumab had the shortest average time until a change in treatment, at 958.625 (226.758) days.
The cumulative probability of treatment with infliximab being maintained decreased over time for both men and women, reaching 28% at 4 years in men and 18% at 6 years in women.
The probability for women of there being no change in treatment at 7 years was greater for adalimumab than for etanercept (85% versus 71%). However, up to that point the probabilities were very similar (85% versus 88%). The opposite was true for men; the probability of there being no change in treatment in the case of adalimumab remained at 57%, whereas with etanercept this decreased over time until it reached 77% at 4 years.
Age
The study population was split into two groups according to age: patients under the age of 60 years, and those aged 60 years and older. Statistical differences were found in both age groups (P = 0.017 for patients aged <60 years and P = 0.031 for patients aged ≥60 years), as shown in .
Figure 4 Drug survival probabilities for adalimumab, etanercept, and infliximab, by age group.
Abbreviation: n, number.
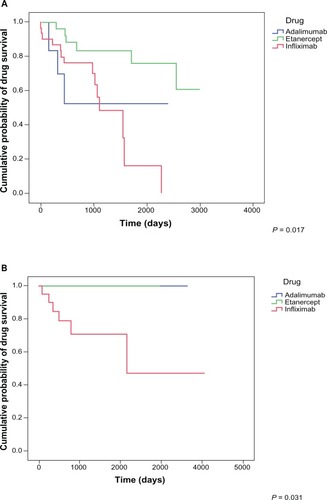
In younger patients (<60 years of age), the anti-TNF agent that endured the longest until a change in treatment was etanercept, with an average of 2,421.833 (206.470) days, followed by adalimumab, with an average of 1,394.938 (393.461) days, and infliximab, with an average of 1,213.096 (170.453) days.
In patients aged 60 years and older, the average time until a change of treatment with infliximab was 2,559 (572.3983) days. Patients who were treated with etanercept or adalimumab did not change to another anti-TNF therapy.
In younger patients, when etanercept was used as a first-line treatment, it had the lowest probability of a change to another anti-TNF treatment (97%), followed by infliximab (86%) and adalimumab (68%). At 6 years, the probability of infliximab being maintained was 0%, whereas after 7 years the likelihood of etanercept being maintained was similar to that of adalimumab (55% versus 49%).
In the case of patients aged 60 years and older, the probability of there being no change in treatment to another anti-TNF therapy remained at 100% for both etanercept and adalimumab, but not for infliximab. In fact, after 5 years of treatment with infliximab, the likelihood of this being maintained was 50%.
Predictors of drug survival
The multivariate regression model showed that the predictors of drug survival in anti-TNF therapy for RA were: being rhematoid-factor negative; being 60 years of age or older; and not having had previous treatment with anti-TNFs. The risk of a change was lower for adalimumab and etanercept than for infliximab, with the latter being statistically significant. It was observed that sex did not have any influence on anti-TNF survival in RA ().
Table 2 Predictors of survival of anti-TNF therapy in RA patients
Discussion
Data on drug survival can be seen as a parameter of treatment success. The results of this study provide new keys to guiding consultants in choosing the best anti-TNF therapy for treating patients with RA, as they specify not only which anti-TNF treatment presents the best survival, but also the factors that are predictors of survival.
This study showed that there were statistical differences between treatments in the time until a change of anti-TNF therapy in the treatment of RA, both generally and in terms of the subgroups of sex, age, and prior treatment with another anti-TNF. The anti-TNF treatment with the lowest survival rate was infliximab, whereas adalimumab and etanercept behaved in very similar ways, with slight differences depending on the subgroup in question, as discussed below.
The literature review was carried out using the online resource PubMed. Search terms were linked by logical operators and implemented using wildcards. The search was limited to articles published between 1977 and 2012, in all languages, concerning research on humans, and with an abstract. Of all of the articles found, those that provided the most valid and important information, on the basis of personal criteria, were selected.
Earlier studies have also analyzed anti-TNF survival in patients suffering from RA, although the results have been varied. In one Swiss observational study,Citation9 patients were monitored from 1997 to 2006 (n = 2,364), and survival was significantly lower in patients who were treated with infliximab, in comparison to etanercept and adalimumab.
Similarly, Markatseli et alCitation10 demonstrated that infliximab, etanercept, and adalimumab were all effective in treating RA and had acceptable safety profiles, although they had different survival patterns. All three anti-TNF treatments had high survival rates during the first year of treatment, but the survival rate of infliximab subsequently decreased significantly, reaching 33% after 7 years, while the rates for etanercept and adalimumab remained at approximately 60% and 50%, respectively.
Gniadecki et alCitation5 concluded that in naïve patients, infliximab was the drug with the longest time until a change of treatment, although this was in relation to patients with psoriasis rather than RA. No evidence was found of statistical differences among patients who had previously been treated with another anti-TNF agent.
Anti-TNF survival in the treatment of psoriasis in naïve patients does not coincide with survival in terms of RA, given that in the present study it was etanercept that had the longest time until a change. This suggests that the type of pathology has an influence on the response to anti-TNF therapies. It would be interesting to assess anti-TNF survival in different diseases.
The results of the present study are consistent with logic; patients who have previously been given another anti-TNF agent may have had an immune response causing them to develop resistance mechanisms, accounting for the fact that being nonnaïve is a predictor of a change in treatment.
On the other hand, data such as the findings published by Finckh et alCitation11 suggests that infliximab is the anti-TNF agent with the greatest risk of acquired resistance, probably because it was the first anti-TNF therapy and due to its chimeric nature. Another study found that patients suffering from severe RA who developed antibodies to infliximab were also prone to developing antibodies to adalimumab, supporting the results of the present study.Citation12
Busquets et alCitation13 studied the effect of age on anti-TNF survival, making use of the Spanish registry of biologics, BIOBADASER. In both RA and ankylosing spondylitis, advanced age was a predictor of treatment discontinuation due to adverse events. Marchesoni et alCitation14 drew the same conclusion about RA patients: among the younger age group there was a higher rate of treatment discontinuation due to inefficacy. Lurati et alCitation15 found that the opposite was true, that survival curves for the two age groups were similar.
In the present study, the rate of discontinuation of treatment due to inefficacy was higher than the rate due to side effects in the group of patients who had previously been treated with at least one anti-TNF agent. It can be observed that, although there was a high proportion of older patients, age decreased with the line of treatment, meaning that it is logical to think that younger patients present a more resistant variant of the disease.
Sex was the only factor that was not shown to have an influence on anti-TNF survival in RA patients. This is consistent with prior research that has shown that age has no effect either on the initiation of biologic treatmentCitation16 or on patients’ response to treatment with anti-TNF therapy.Citation17
Markenson et alCitation6 established that female sex is a predictor of discontinuation for infliximab, although only when it is used as the first biologic agent. In juvenile idiopathic arthritis the risk of discontinuation of firstline anti-TNF treatment is almost three times higher among women than among men.Citation18
Although sex has no effect on anti-TNF survival, these drugs act differently on men and women. This could lead us to think that the sex chromosomes may be involved in drug response.
The main limitation of the present study is the small sample size. Certain differences between the various groups were not statistically significant. A further limitation is the fact that none of the patients were followed up from the beginning of treatment with one anti-TNF until a change to a different one; as such, there may have been a certain element of bias in patient selection. However, the greatest possible effort was made to include as many patients as possible, and we are satisfied that these constitute a fair representation of the total population.
At present, the management of biologic treatment is empirical,Citation19 and it is hoped that in the future it will be based on drug levels and on antibodies to drugs.Citation20 As routine monitoring is unfeasible in the current economic climate, research in this field takes on a vital role in establishing alternative strategies for choosing the optimum biologic treatment for these patients.
Conclusion
In conclusion, choosing infliximab indiscriminately as a firstline anti-TNF therapy is not an appropriate practice, because starting a course of treatment with a drug that will probably become less effective over time will ultimately increase the overall cost of therapy. The long-term management of RA is not only a desirable goal on a medical level; it is also a worthwhile strategy from a pharmacological and economic point of view. Anti-TNF therapies should be chosen on the basis of patient characteristics, in order to ensure that treatment is successful. This study has shown etanercept to be superior to the other anti-TNF agents across most of the subgroups. It would therefore be useful to try to discover the reasons why etanercept is superior among patients suffering from RA, so that treatment can be optimized as a result.
Acknowledgments
The authors would like to thank Mari Fe Muñoz for her support in the statistical analysis.
Disclosure
We certify that there is no conflict of interest with any financial organization regarding the material discussed in the manuscript. The authors report no other conflicts of interest in this work.
References
- González-GayMAAgudoMFármacos antifactor de necrosis tumoral alfa en pacientes con artritis reumatoide refractaria a tratamientos convencionales [Anti-TNF alpha agents in patients with rheumatoid arthritis refractory to conventional therapies]Med Clin (Barc)201013415684685 Spanish20176386
- ScottDLWolfeFHuizingaTWRheumatoid arthritisLancet201037697461094110820870100
- National Collaborating Centre for Chronic Conditions (UK)Rheumatoid Arthritis: National Clinical Guideline for Management and Treatment in AdultsLondon, UKRoyal College of Physicians2009
- SinghJAFurstDEBharatA2012 update of the 2008 American College of Rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritisArthritis Care Res (Hoboken)201264562563922473917
- GniadeckiRKragballeKDamTNSkovLComparison of drug survival rates for adalimumab, etanercept and infliximab in patients with psoriasis vulgarisBr J Dermatol201116451091109621219290
- MarkensonJAGibofskyAPalmerWRPersistence with antitumor necrosis factor therapies in patients with rheumatoid arthritis: observations from the RADIUS registryJ Rheumatol20113871273128121572150
- AletahaDNeogiTSilmanAJ2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiativeArthritis Rheum20106292569258120872595
- Martínez SantanaVIzquierdo NavarroMCallejaHernández MÁSánchez SánchezTSainz GilMSevere pancytopenia following etanercept administration in rheumatoid arthritisInt J Rheum Dis2012154e78e7922898233
- Du PanSMDehlerSCiureaAZiswilerHRGabayCFinckhASwiss Clinical Quality Management PhysiciansComparison of drug retention rates and causes of drug discontinuation between antitumor necrosis factor agents in rheumatoid arthritisArthritis Rheum200961556056819405000
- MarkatseliTEAlamanosYSaougouIVoulgariPVDrososAASurvival of TNF-alpha antagonists in rheumatoid arthritis: a long-term studyClin Exp Rheumatol2012301313822153557
- FinckhASimardJFGabayCGuernePASCQM physiciansEvidence for differential acquired drug resistance to anti-tumour necrosis factor agents in rheumatoid arthritisAnn Rheum Dis200665674675216339288
- BarteldsGMWijbrandtsCANurmohamedMTAnti-infliximab and anti-adalimumab antibodies in relation to response to adalimumab in infliximab switchers and anti-tumour necrosis factor naive patients: a cohort studyAnn Rheum Dis201069581782119581278
- BusquetsNTomeroEDescalzoMÁBIOBADASER 2.0 Study GroupAge at treatment predicts reason for discontinuation of TNF antagonists: data from the BIOBADASER 2.0 registryRheumatology (Oxford)201150111999200421856725
- MarchesoniAZaccaraEGorlaRTNF-alpha antagonist survival rate in a cohort of rheumatoid arthritis patients observed under conditions of standard clinical practiceAnn N Y Acad Sci2009117383784619758236
- LuratiAMarrazzaMAngelaKScarpelliniMSafety of etanercept in elderly subjects with rheumatoid arthritisBiologics201041420161980
- DeWittEMLinLGlickHAAnstromKJSchulmanKAReedSDPattern and predictors of the initiation of biologic agents for the treatment of rheumatoid arthritis in the United States: an analysis using a large observational data bankClin Ther200931818711880 discussion 185819808146
- KristensenLEKapetanovicMCGülfeASöderlinMSaxneTGeborekPPredictors of response to anti-TNF therapy according to ACR and EULAR criteria in patients with established RA: results from the South Swedish Arthritis Treatment Group RegisterRheumatology (Oxford)200847449549918316338
- TynjäläPVähäsaloPHonkanenVLahdennePDrug survival of the first and second course of anti-tumour necrosis factor agents in juvenile idiopathic arthritisAnn Rheum Dis200968455255718467515
- MihellerPKissLSLorinczyKLakatosPLAnti-TNF trough levels and detection of antibodies to anti-TNF in inflammatory bowel disease: are they ready for everyday clinical use?Expert Opin Biol Ther201212217919222149260
- LorinczyKMihellerPKissSLLakatosPL[Epidemiology, predictors and clinical aspects of loss of response to biological therapy]Orv Hetil20121535163173 Hungarian [with English abstract]22275731