Abstract
Objective
Nocturia affects millions of men and women. No prior reviews or meta-analyses have explored the issue of adherence in nocturia patients. The objective of our study was to examine the attributes and their interaction that might impact pharmacological adherence in nocturia care using a conceptual model of adherence.
Materials and methods
A literature search of the Medline, PubMed, Embase, PsycInfo, and CINAHL databases for studies published between January 1990 and June 2014 was conducted. We developed a conceptual model in order to facilitate our review.
Results
Currently, multiple treatment options for nocturia exist, depending on the underlying cause. Adherence to nocturia treatment and outcomes are complex and intertwined, and nonadherence to nocturia treatment is common. In 15 studies meeting eligibility criteria, behavioral and pharmacologic interventions for nocturia were associated with reduced nocturia symptoms. Urinary symptoms that are associated with nocturia need individualized management depending on renal and hepatic function, medical comorbidities, and ongoing medication use in a patient. Another important factor related to adherence is the bother. Although nocturia is defined as nighttime-voiding frequency of one or more, not all persons may find this bothersome. The degree of bother is subjective, and may change from person to person. However, there is no information related to the association between bother and adherence to medication or behavioral treatments for nocturia. Medication dosing convenience, preference, and cost play important roles in adherence. We present a patient-centered conceptual model that brings together the various dimensions of medication adherence for nocturia.
Conclusion
Few studies have explored adherence to medication and related factors in the care of nocturia. Our conceptual model can aid development of interventions to improve adherence to nocturia medications.
Introduction
Nocturia is a highly prevalent and bothersome urologic symptom.Citation1 It is defined by the International Continence Society as “the complaint that the individual has to wake at night one or more times to void”.Citation2 However, measure of bother caused by nocturia is not considered in this definition. Also, no differentiation is made between getting up in the night because of a feeling of the need to urinate versus getting up for some other reason.Citation1,Citation3,Citation4 Among persons living at home, between 15% to 30% report symptoms of nocturia. This range is 30%–50% for those living in assisted living or acute-care facilities, or in nursing homes.Citation5–Citation7 The prevalence of nocturia increases with age, and is high in older men.Citation8 In a systematic review, it was observed that 68.9%–93% of men in their 70s and 80s had void frequency of once per night, and 29%–59.3% had a minimum of two voids per night.Citation5–Citation7 Globally, persons from various ethnicity and nationality experience a high prevalence of nocturia.Citation5–Citation7 Among the elderly, the prevalence of nocturia is higher compared to the prevalence of chronic diseases like coronary artery disease or asthma. However, current knowledge regarding nocturia is somewhat limited. Despite embarrassment, sleep disturbance, bother, and risk of falls, nocturia is often thought of as a usual aging-related process. Women seldom discuss nocturia with their physicians. Based on its pathophysiology, five important contributing factors of nocturia are: 24-hour polyuria or overall increase in urine production, increase in nighttime urine production or nocturnal polyuria, reduced bladder capacity, sleep disturbance, and circadian clock disorders. The reasons for reduced bladder capacity can be many, such as benign prostatic hyperplasia with detrusor overactivity and/or elevated postvoid residual volume, or overactive bladder.Citation2,Citation6,Citation9,Citation10
Nocturia is a bothersome urinary symptom, and can cause substantial impairment to the health and quality of life of a person. Fragmented sleep cycles due to nocturia can negatively impact the quality of sleep, resulting in daytime tiredness.Citation11–Citation15 Nocturnal enuresis, which affects up to 15% of children less than 15 years of age, has been shown to be associated with abnormal sleep patterns.Citation16–Citation20 Nocturia is also associated with falls and fall-related morbidity, as well as mortality. Nocturia may lead to lower work productivity and add to the overall burden on society.Citation12,Citation14 Although traditionally nocturia was considered one among the several urinary tract symptoms that are caused by dysfunction of the lower urinary tract, because of its multidimensional etiopathogenesis, it is now recognized as a distinct clinical condition. For treatments to be responsive to the probable causes, it is important to perform a proper evaluation of the nocturic patient. Treatment options for nocturia include lifestyle and behavioral strategies, pharmacotherapy, and surgery.Citation21 Initial or first-line treatment for nocturia is behavioral therapy, which has been shown to be effective in reducing symptoms of nocturia.Citation13,Citation22–Citation25
Adherence to medication is an important factor linked to the successful pharmacologic treatment of nocturia, and has implications for patients’ quality of life and sleep pattern. Overall, adherence is:
The extent to which a person’s behavior (in terms of taking medications, following diets, or executing lifestyle changes) coincides with medical or health advice.Citation26
Ignoring adherence can result in incorrect dosage, changes in medication regimen, and escalated costs of care.Citation6,Citation27–Citation30 In addition to underdiagnosis, lack of adherence is a major concern in nocturia treatment. Recent studies have confirmed that on average, half of the patients do not complete nocturia treatment.Citation29,Citation31–Citation35
Multiple reasons for nonadherence to medication can be identified. Beliefs held by those who decline getting treated for a condition may appear to be inconsistent with those posited by the biomedical model.Citation33 In addition to age, socioeconomic status, and education, other less explored patient-centered factors related to adherence are bother due to the condition, efficacy, and side effects of the medication, and patient preference, attitudes, and beliefs.Citation12,Citation21,Citation33,Citation36 Additionally, health care system-level and provider-level factors play a key role in both underdiagnosis of nocturia and treatment adherence. Therefore, adherence to nocturia treatment is a multifactorial construct that comprises patient-centered and provider-centered components.
Conceptual model: medication adherence and patient-centered care
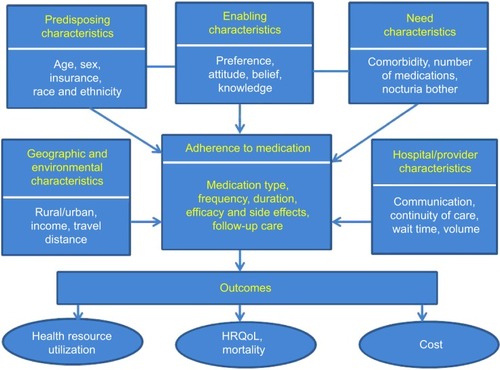
The Institute of Medicine defines patient-centered care as “care that is respectful of and responsive to individual patient preferences, needs, and values”.Citation37 Our patient-centered conceptual model () brings together the various dimensions of medication adherence in nocturia. Our model is based on the Andersen model of health service use. The Andersen model postulates that the use of health services is a function of predisposition, ability, and need.Citation26,Citation38–Citation40 The predisposing component relates to the inclination to use a certain quantity of health services. The enabling component identifies the specific conditions that make health services available to a person. Finally, the need factor refers to the health status. Our adaptation of the Andersen model uniquely takes into account the predisposing factors (age, race/ethnicity, and income), enabling factors (preference, attitude, and knowledge) and need factors (comorbidities, number of medications, and bother of nocturia symptoms). Health care that is patient-centered as well as evidence-based can facilitate improved treatment adherence and treatment outcomes. Medication adherence is dysfunctional among nocturia patients: it is affected by the level of bother, efficacy, and side effects of nocturia medication, disintegrated care, limited information regarding diseases, belief system, cognitive issues, age-related issues such as vision, hearing, and memory, and complicated medication regimens of patients with multiple chronic diseases.Citation3,Citation4 In some cases, a patient may add over-the-counter medications and other therapies to the ones prescribed by his/her doctor, and this in turn may exacerbate nocturia. Additionally, social and environmental factors can also influence medication adherence among nocturia patients. The main goal of our article was to offer an overview of the issue of adherence to medication in the management of nocturia, and present a conceptual model to guide the adherence research in nocturia.
Materials and methods
We conducted a search of the electronic versions of the Medline, PubMed, PsycInfo, and CINAHL databases to obtain English-language articles that were published between 1990 and 2014. We used “nocturia”, “adherence”, “attitude”, “treatment”, and related terms as keywords in our search. Next, we selected articles related to medication adherence and comprehensive strategies for improving adherence to medication. The authors independently reviewed the abstracts. Next, the full text of relevant publications was read to examine whether the study used original data from patients and examined links between nocturia and adherence to medication. Case reports, review articles, and studies in laboratory settings were excluded from the analysis.
Results
Behavioral therapy is first-line therapy for nocturia, followed by pharmacotherapy with or without behavioral therapy.Citation1 However, there is little information regarding bother, acceptability, and adherence to different components of behavioral therapies, which may depend on a tradeoff between the effectiveness versus inconvenience of such therapies. Adherence to medication among nocturia patients is weak. Studies show that only half of chronically ill older adults adhere to the medication regimens prescribed by their health care providers.Citation6,Citation26,Citation41,Citation42 The reasons can be cognitive impairment, comorbidities, access-related barriers such as cost and transportation, personal beliefs, preferences, and attitudes, and communication between patients and providers.Citation6,Citation26,Citation41,Citation43–Citation46 There exists very little research related to medication adherence in nocturia patients. In , we provide a brief overview of some of the studies related to adherence among patients with lower urinary tract symptoms. It is important to note that most of the studies were related to overactive bladder. Based on the conceptual model, we summarized the results of the literature into five broad components that may influence medication adherence: health care-system and provider component, patient component, nocturia-condition component, nocturia-treatment component, and social and economic component.
Table 1 Summary of studies included in the review
Health care-system and provider component
Adherence is a complicated behavioral pattern, and is substantially affected by the health care system- and provider-level factors. Though hospitals are dedicated to meeting the patients’ needs, opportunities exist to make them more patient-centered.Citation29,Citation46–Citation48 To operationalize patient-centered care effectively, hospitals and providers can concentrate on providing cohesive management, educating the patient, and sharing the available information related to nocturia.Citation49 This highlights the necessity of bringing gradual changes to health care systems by responding to crucial care-related factors, such as costs, disparity, and access. These changes include the strategies, resources, and institutional and financial measures that determine if medical services are accessible, available, and acceptable. Adherence to nocturia medication is also affected by the communication between patient and provider regarding risks and benefits of treatment, proper use of medication, and finally, patient-friendly regimens.
Patient-related component
Patient-related factors, such as bother due to nocturia, beliefs, attitude, preferences, and expectations, are vital for nocturia-medication adherence and treatment initiation. The issues of adherence and underdiagnosis of nocturia can be addressed by adopting a patient-centered care approach. In the context of health care, a patient-centered care model must incorporate preferences and needs of patients, encourage patient engagement in decision making, and adapt the treatment to improve outcomes.Citation45 This relatively old concept poses unique challenges and offers opportunities in the continually altering field of medical care.Citation6,Citation11,Citation40,Citation44,Citation47,Citation48 Therefore, five dimensions of a patient-centered care model are: 1) understanding the patient and his/her medical condition, 2) achieving shared understanding of management of the medical condition, 3) offering important information, 4) enhancing the provider– patient relationship, and 5) awareness about resource distribution.
Assessment of patient preferences and communication of these to the provider is fundamental to the patient-centered care of nocturia. There are two main methods of assessing preferences: revealed and stated. Observational data related to a persons’ actual behavior are used to determine revealed preference. The stated preference assessment depends on structured or hypothetical conditions. In this method, surveys are used to obtain data on patients’ preferences for hypothetical experimental scenarios. Therefore, an important criterion of patient-centered nocturia care consists of recognizing the patient as a person and understanding the symptoms of nocturia (specifically bothers) from the patient’s perspective. Therefore, future research needs to address these issues that appear to be stalemating the patient-centered care of nocturia.
Nocturia-condition component
Nocturia is common among older persons, and has an effect on morbidity and mortality. Among the elderly, the syndrome of nocturnal polyuria is a common reason for nocturia, and may be caused by the lower nocturnal secretion of antidiuretic hormone. Though the prevalence of nocturia in younger men and women is low, it can reach 80%–90% by 80 years of age.Citation6,Citation7,Citation28 Nocturia can disrupt sleep, which in turn can lead to drowsiness during daytime, symptoms of depression, and weakened sense of wellness.Citation31,Citation44,Citation49–Citation53 Additionally, nocturia is shown to be linked with greater morbidity and mortality risk. Nocturia is the result of an intricate interaction of age-related changes in the function of urinary and renal systems, patterns of sleep, comorbidities, medications, and personal habits. Appropriate treatment necessitates correct identification of the underlying pathophysiologic cause of nocturia.
Nocturia-treatment component
Isolating the cause is the basic step in the treatment of nocturia. For some patients, treatments in the form of behavioral and lifestyle changes can be beneficial, while for others pharmacological treatment may be necessary.Citation5,Citation11,Citation21,Citation41,Citation49,Citation54–Citation58 Just as with selecting the optimal treatment, it is essential to understand that nocturia is one of the reasons for sleep disorders. At the same time, it is important to acknowledge the limitations of drugs, as side effects may occur in spite of enhanced quality of life and sleep.Citation49,Citation50,Citation59,Citation60 New physiotherapy techniques to treat nocturia, overactive bladder, and urinary incontinence symptoms involve improving the awareness of overactivity in the pelvic floor and controlling the detrusor.Citation31,Citation33,Citation52,Citation53,Citation61 The majority of therapies for nocturia have predominantly focused on or are related to overactive bladder care. One of the pharmacologic treatments involves the use of anticholinergics or antimuscarinics. However, these have very limited efficacy for nocturia, and may be appropriate for those without nocturnal polyuria and with severe urgency as the reason for awakening.Citation62,Citation63
Since most anticholinergics have such side effects as constipation and dryness of the mouth and eyes, other therapies that lack these side effects have been developed (eg, mirabegron, botulinum toxin, and vasopressin). In order to decrease involuntary detrusor contractions, the medication treatment for overactive bladder has mostly concentrated on blocking the postsynaptic muscarinic receptors on the detrusor muscle. At the same time, efficacy, acceptance, and adherence in the long run can affect the utilization of these medications. Earlier research on effects of botulinum-toxin treatment for nocturia has reported mixed results.Citation14,Citation64–Citation67 Overall, insufficient symptom control, bother, unfulfilled or impractical expectations, and insufficient posttreatment follow-up are important contributors to medication nonadherence.Citation68
Social and economic component
Social and economic factors that affect medication adherence are a patients’ home environment, neighborhood structure, support level, and costs.Citation5,Citation12,Citation43,Citation46,Citation69,Citation70 Specifically, these factors are the living conditions of the patient, relationships he/she shares with the family and neighborhood, the magnitude of stress and violence in the neighborhood, and economic condition of the neighborhood. Other important socioeconomic factors that merit consideration in the context of medication adherence are travel distance, aging of the community, and race and ethnicity.
Discussion
A common and bothersome symptom, nocturia is associated with many health conditions. Given its chronic nature, nocturia symptoms can deteriorate in the absence of treatment, and health benefits could be higher with good adherence.Citation12,Citation31,Citation33,Citation52 Several treatment options are available for nocturia, depending on the underlying cause.Citation6,Citation31,Citation71,Citation72 This review shows that both adherence to nocturia treatment and outcomes are complex and intertwined. Nonadherence to nocturia treatment is common. Though the burden exerted by nocturia is substantial, research indicates that a considerable proportion of nocturia patients cease pharmacological treatment.Citation12,Citation33,Citation34,Citation52,Citation61,Citation73,Citation74 Association between adherence to nocturia treatment, side effects, and adverse events have been observed.Citation6,Citation41,Citation49,Citation57,Citation75,Citation76 Adverse events can affect the production of hormones that control diuresis and alter the structure of the lower urinary tract. Adverse events are most frequent in persons aged 65 years or older, women in the postmenopausal stage, and men with prostatic hyperplasia. Therefore, age has a strong association with nocturia. Multivariate analyses have indicated a strong association between better adherence and lower costs of care, after adjusting for demographic attributes and comorbidity.Citation55 At the same time, there is uncertainty regarding the association between nocturia-induced sleep disruptions and frequent nighttime urination. Research indicates that nocturnal enuresis is a complex condition in children that is linked with abnormal sleep patterns and motor coordination, and visuomotor condition, disordered respiration, and mild reading difficulties.Citation16–Citation20,Citation77,Citation78
One important factor related to adherence is the bother of the symptoms. Although by definition, nocturia refers to at least one nighttime voiding, not all persons may find this bothersome. The degree of bother is subjective, and may change from person to person. Generally speaking, the higher the frequency, the more bothersome the symptoms. However, there is no information related to the association between bothers and adherence to medication or behavioral treatments. Behavioral modifications have been observed to work well. Unless the nocturia is associated with true severe nocturnal urgency, antimuscarinics or α-adrenergic blocking agents are not effective. The “optimal medication” would be one that significantly decreases urine output, but for a very short period of time and without any chance of hyponatremia, which is the major cause of significant adverse events. Probably the most significant parameter to measure is the first period of uninterrupted sleep. Although there has been little research about what is the minimum for an ideal, most sleep experts estimate this at 240 minutes.
As with any other health conditions, adherence to medication is important in nocturia care to achieve improved patient functioning and quality of life. Factors that may influence adherence are the type of drug and its formulation, provider-level factors (ie, communication and attitude), and patient-level factors (ie, comorbidity, preference, access, cost, and family/social support).Citation11,Citation27,Citation29,Citation32,Citation34,Citation45,Citation47–Citation49,Citation68,Citation79–Citation82 Additionally, these factors can have differing or additive effects. Current pharmacological treatments report rather weak side effects, and lower doses were observed to improve acceptability without affecting efficacy, especially among elderly patients with multiple chronic illnesses.Citation6,Citation7,Citation31,Citation33,Citation34,Citation42,Citation47,Citation52,Citation53,Citation61,Citation73,Citation83,Citation84 For optimizing dosing and improving adherence, medication titration can be a useful approach. However, the association between dose titration and adherence remains to be established. Studies have reported that it is important to educate nocturia patients so that they do not accept their symptoms as an unavoidable aspect of aging, and also to increase their knowledge of the various treatments available to them.Citation6,Citation7,Citation31,Citation33,Citation34,Citation47,Citation52,Citation61,Citation73,Citation83 Patients who are offered educational intervention are significantly more likely to have their prescriptions filled and to accept behavior-modification treatments.Citation57,Citation69 Providers need to interact with those patients who are observed to be nonadherent. This will create an opportunity to understand the patients’ treatment expectations, and at the same time educate the patient regarding available treatment options.
Need for future research
Despite the considerable effect of nocturia on patients’ health and well-being, high rates of treatment interruption, and low medication adherence, only limited information exists regarding the overall implications of pharmacologic nonadherence for nocturia.Citation1,Citation61,Citation73 Before any specific conclusions can be made regarding the immediate and long-term impact of medication adherence in nocturia patients, further research is necessary to: 1) develop agreement across various disciplines regarding the contribution made by each evaluation and diagnostic instrument in providing an accurate diagnosis of nocturia; 2) highlight the necessity of the appropriate assessment of nocturia tied to measurable outcomes; 3) systematically evaluate quality of life with validated tools, as well as sleep quality, level of bother, and health resource utilization and cost parameters, using population-based prospective studies (and clinical trials); 4) refine the role of behavioral therapies and assess the efficacy versus acceptability of their components in the management of nocturia; and 5) study the effect of adherence to nocturia medication on short- and long-term outcomes across various clinical settings.
Disclosure
The authors report no conflicts of interest in this work.
References
- OsmanNIChappleCRWeinAJNocturia: current concepts and future perspectivesActa Physiol (Oxf)2013207536523033860
- AbramsPCardozoLFallMThe standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence SocietyNeurourol Urodyn20022116717811857671
- WeissJPBlaivasJGBliwiseDLThe evaluation and treatment of nocturia: a consensus statementBJU Int201110862121676145
- WeissJPBlaivasJGBlankerMHThe New England Research Institutes, Inc. (NERI) Nocturia Advisory Conference 2012: focus on outcomes of therapyBJU Int201311170071623360086
- BoschJLWeissJPThe prevalence and causes of nocturiaJ Urol2012189S86S9223234639
- van DoornBBoschJLNocturia in older menMaturitas20127181222079871
- GoessaertASDenysMADeryckereSEveraertKNocturnal polyuria in a nursing home and effect on quality of lifeJ Am Geriatr Soc2013611812181324117293
- MarklandADVaughanCPJohnsonTM2ndGoodePSReddenDTBurgioKLPrevalence of nocturia in United States men: results from the National Health and Nutritional Examination SurveyJ Urol2011185998100221251675
- van KerrebroeckPAbramsPChaikinDThe standardization of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence SocietyNeurourol Urodyn20022117918311857672
- KerrebroeckPVAnderssonKETerminology, epidemiology, etiology, and pathophysiology of nocturiaNeurourol Urodyn201433S2S524729150
- BennerJSNicholMBRovnerESPatient-reported reasons for discontinuing overactive bladder medicationBJU Int20101051276128219912188
- KobeltGBorgströmFMattiassonAProductivity, vitality and utility in a group of healthy professionally active individuals with nocturiaBJU Int20039119019412581002
- LoseGLalosOFreemanRMvan KerrebroeckPEfficacy of desmopressin (Minirin) in the treatment of nocturia: a double-blind placebo-controlled study in womenAm J Obstet Gynecol20031891106111314586363
- WeissJPWeinAJvan KerrebroeckPNocturia: new directionsNeurourol Urodyn20113070070321661016
- BliwiseDLRosenRCBauNImpact of nocturia on sleep and quality of life: a brief, selected review for the International Consultation on Incontinence Research Society (ICI-RS) nocturia think tankNeurourol Urodyn201433S15S1824729148
- CarotenutoMEspositoMPascottoAMigraine and enuresis in children: an unusual correlation?Med Hypotheses20107512012220185246
- CarotenutoMEspositoMPascottoAFacial patterns and primary nocturnal enuresis in childrenSleep Breath20111522122720607423
- EspositoMCarotenutoMRoccellaMPrimary nocturnal enuresis and learning disabilityMinerva Pediatr2011639910421487372
- EspositoMGallaiBParisiLPrimary nocturnal enuresis as a risk factor for sleep disorders: an observational questionnaire-based multicenter studyNeuropsychiatr Dis Treat2013943744323579788
- EspositoMGallaiBParisiLVisuomotor competencies and primary monosymptomatic nocturnal enuresis in prepubertal aged childrenNeuropsychiatr Dis Treat2013992192923847418
- CornuJNAbramsPChappleCRA contemporary assessment of nocturia: definition, epidemiology, pathophysiology, and management – a systematic review and meta analysisEur Urol20126287789022840350
- JohnsonTM2ndBurgioKLReddenDTWrightKCGoodePSEffects of behavioral and drug therapy on nocturia in older incontinent womenJ Am Geriatr Soc20055384685015877562
- JohnsonTM2ndMarklandADGoodePSEfficacy of adding behavioural treatment or antimuscarinic drug therapy to α-blocker therapy in men with nocturiaBJU Int201311210010823448285
- JohnsonTM2ndJonesKWillifordWOKutnerMHIssaMMLeporHChanges in nocturia from medical treatment of BPH. Secondary analysis of the VA Cooperative Study TrialJ Urol2003170140148
- MattiassonAAbramsPVan KerrebroeckPWalterSWeissJEfficacy of desmopressin in the treatment of nocturia: a double-blind placebo-controlled study in menBJU Int20028985586212010228
- OsterbergLBlaschkeTAdherence to medicationN Engl J Med200535348749716079372
- D’SouzaAOSmithMJMillerLADoyleJArielyRPersistence, adherence, and switch rates among extended-release and immediate-release overactive bladder medications in a regional managed care planJ Manag Care Pharm20081429130118439051
- EasterlingSAMasterVCarneyKJEvaluation and management of patients with nocturiaJAAPA201427364224463749
- YuYFNicholMBYuAPAhnJPersistence and adherence of medications for chronic overactive bladder/urinary incontinence in the California Medicaid programValue Health2005849550516091027
- PelletierEMVatsVClemensMJPharmacotherapy adherence and costs versus nonpharmacologic management in overactive bladderAm J Manag Care200915S108S11419355799
- RosenRCHolm-LarsenTKupelianVWeinAJConsequences of nocturiaPostgrad Med2013125384623841962
- SearsCLLewisCNoelKAlbrightTSFischerJROveractive bladder medication adherence when medication is free to patientsJ Urol20101831077108120092838
- TikkinenKAAuvinenAJohnsonTM2ndA systematic evaluation of factors associated with nocturia – the population based FINNO studyAm J Epidemiol200917036136819515794
- VeenboerPWBoschJLLong-term adherence to antimuscarinic therapy in everyday practice: a systematic reviewJ Urol20101911003100824140548
- Van HerzeeleCAlovaIEvansJPoor compliance with primary nocturnal enuresis therapy may contribute to insufficient desmopressin responseJ Urol20091822045204919695639
- GourovaLWvan de BeekCSpigtMGNiemanFHvan KerrebroeckPEPredictive factors for nocturia in elderly men: a cross sectional study in 21 general practicesBJU Int20069752853216469020
- Institute of Medicine of the National AcademiesCrossing the Quality Chasm: A New Health System for the 21st CenturyWashingtonNational Academies2001
- AndersenRMRevisiting behavioral model and access to medical care: does it matter?J Health Soc Behav1995361107738325
- AdayLAAndersenRA framework for the study of access to medical careHealth Serv Res197492082204436074
- MurrayMDMorrowDGWeinerMA conceptual framework to study medication adherence in older adultsAm J Geriatr Pharmacother20042364315555477
- BasraRKWaggAChappleCA review of adherence to drug therapy in patients with overactive bladderBJU Int200810277477918616691
- YeawJBennerJSWaltJGSianSSmithDBComparing adherence and persistence across 6 chronic medication classesJ Manag Care Pharm20091572874019954264
- Vecchioli ScaldazzaCMorosettiCPaceGAziziBGiannubiloWFerraraVHas the cost of anti-muscarinic a key role in the success rate of patients diagnosed with overactive bladder syndrome?Arch Ital Urol Androl201284687322908774
- BrubakerLFanningKGoldbergELPredictors of discontinuing overactive bladder medicationsBJU Int20101051283129019912189
- GambleTSandPPatient perspectives in the management of overactive bladder, focus on transdermal oxybutyninPatient Prefer Adherence2008234935619920982
- ShayaFTBlumeSGuAZyczynskiTJumadilovaZPersistence with overactive bladder pharmacotherapy in a Medicaid populationAm J Manag Care200511S121S12916161385
- RobinsonJHCallisterLCBerryJADearingKAPatient-centered care and adherence: definitions and applications to improve outcomesJ Am Acad Nurse Pract20082060060719120591
- MeadNBowerPPatient-centeredness: a conceptual framework and review of the empirical literatureSoc Sci Med2000511087111011005395
- HofmeesterIKollenBJSteffensMGThe association between nocturia and nocturnal polyuria in clinical and epidemiological studies: a systematic review and meta analysesJ Urol20131911028103324184367
- RaheemOAOroscoRKDavidsonTMLakinCClinical predictors of nocturia in the sleep apnea populationUrol Ann20146313524669119
- SongMHongBSChunJYHanJYChooMSSafety and efficacy of desmopressin for the treatment of nocturia in elderly patients: a cohort studyInt Urol Nephrol2014461495149924595604
- TikkinenKAJohnsonTM2ndTammelaTLNocturia frequency, bother, and quality of life: how often is too often? A population-based study in FinlandEur Urol20105748849819361907
- YokoyamaOHiroSHottaSMogamiSYamagamiHEfficacy of fesoterodine on nocturia and quality of sleep in Asian patients with overactive bladderUrology20148375075524518285
- AdayLAAndersenRA framework for the study of access to medical careHealth Serv Res197492082204436074
- BalkrishnanRBhosleMJCamachoFTAndersonRTPredictors of medication adherence and associated health care costs in an older population with overactive bladder syndrome: a longitudinal cohort studyJ Urol20061751067107216469620
- BreyerBNShindelAWEricksonBABlaschkoSDSteersWDRosenRCThe association of depression, anxiety and nocturia: a systematic reviewJ Urol201319095395723680309
- ChancellorMBMigliaccio-WalleKBramleyTJChaudhariSLCorbellCGlobeDLong-term patterns of use and treatment failure with anticholinergic agents for overactive bladderClin Ther2013351744175124091072
- ChungMSChuangYCLeeJJLeeWCChancellorMBLiuRTPrevalence and associated risk factors of nocturia and subsequent mortality in 1,301 patients with type 2 diabetesInt Urol Nephrol2014461269127524595602
- YoshimuraKOharaHIchiokaKNocturia and benign prostatic hyperplasiaUrology20036178679012670566
- JohnsonTM2ndBurrowsPKKusekJWThe effect of doxazosin, finasteride and combination therapy on nocturia in men with benign prostatic hyperplasiaJ Urol20071782045205017869295
- WeissJPWeinAJVan KerrebroeckPFuture research guidance for nocturiaNeurourol Urodyn201433Suppl 1S2524375762
- RackleyRWeissJPRovnerESWangJTGuanZNighttime dosing with tolterodine reduces overactive bladder-related nocturnal micturitions in patients with overactive bladder and nocturiaUrology20066773173616618562
- BrubakerLFitzGeraldMPNocturnal polyuria and nocturia relief in patients treated with solifenacin for overactive bladder symptomsInt Urogynecol J Pelvic Floor Dysfunct20071873774117131169
- HirstGRWatkinsAJGuerreroKBotulinum toxin B is not an effective treatment of refractory overactive bladderUrology200769697317270619
- SchmidDMSauermannPWernerMExperience with 100 cases treated with botulinum-A toxin injections in the detrusor muscle for idiopathic overactive bladder syndrome refractory to anticholinergicsJournal of Urology200617617718516753396
- ApostolidisADasguptaPDenysPRecommendations on the use of botulinum toxin in the treatment of lower urinary tract disorders and pelvic floor dysfunctions: a European consensus reportEur Urol20095510012018823697
- DuthieJBVincentMHerbisonGPWilsonDIWilsonDBotulinum toxin injections for adults with overactive bladder syndromeCochrane Database Syst Rev201112CD00549322161392
- WeissJPJuulKVWeinAJManagement of nocturia: the role of antidiuretic pharmacotherapyNeurourol Urodyn201433S19S2424729149
- ChenFYDaiYTLiuCKYuHJLiuCYChenTHPerception of nocturia and medical consulting behavior among community-dwelling womenInt Urogynecol J Pelvic Floor Dysfunct20071843143616874440
- SextonCCNotteSMMaroulisCPersistence and adherence in the treatment of overactive bladder syndrome with anticholinergic therapy: a systematic review of the literatureInt J Clin Pract20116556758521489081
- GulurDMMevchaAMDrakeMJNocturia as a manifestation of systemic diseaseBJU Int201010770271321355977
- NevéusTLeissnerLRudbladSBazarganiFOrthodontic widening of the palate may provide a cure for selected children with therapy-resistant enuresisActa Paediatr201410311871191
- van KerrebroeckPNocturia: current status and future perspectivesCurr Opin Obstet Gynecol20112337638521897234
- WaggACompionGFaheyASiddiquiEPersistence with prescribed antimuscarinic therapy for overactive bladder: a UK experienceBJU Int20121101767177422409769
- EisenhardtASchneiderTCruzFOelkeMConsistent and significant improvement of nighttime voiding frequency (nocturia) with silodosin in men with LUTS suggestive of BPH: pooled analysis of three randomized, placebo-controlled, double-blind phase III studiesWorld J Urol2014321119112524442560
- AsplundRPharmacotherapy for nocturia in the elderly patientDrugs Aging20072432534317432926
- NevéusTLeissnerLRudbladSBazarganiFRespiration during sleep in children with therapy-resistant enuresisActa Paediatr201410330030424236639
- CederbladMSarkadiAEngvallGNevéusTInfrequent enuresis, the uninvestigated majority comparisons between children with enuresis of varying severityJ Pediatr Urol Epub ahead of print2014
- GomelskyADmochowskiRRUpdate on the management of overactive bladder: patient considerations and adherenceOpen Access J Urol2010371724198630
- JohnstonSJanningSWHaasGPComparative persistence and adherence to overactive bladder medications in patients with and without diabetesInt J Clin Pract2012661042105123067028
- HaaFCastro-DiazDPersistence with antimuscarinic therapy in patients with overactive bladderInt J Clin Pract20055993193716033615
- HampelCLong-term management of overactive bladder with anti-muscarinic agentsEur Urol Suppl20076432437
- MobleyDFBaumNEtiology, evaluation, and management of nocturia in elderly men and womenPostgrad Med201412614715324685979
- JundtKSchreyerKFrieseKPeschersUAnticholinergic therapy: do the patients take the pills prescribed?Arch Gynecol Obstet201128466366621046135
- FilipettoFAFuldaKGHolthusenAEMcKeithenTMMcFaddenPThe patient perspective on overactive bladder: a mixed methods needs assessmentBMC Fam Pract2014159624885491
- MausethSASkurtveitSSpigsetOAdherence, persistence and switch rates for anticholinergic drugs used for overactive bladder in women: data from the Norwegian Prescription DatabaseActa Obstet Gynecol Scand2013921208121523763552