Abstract
Purpose
The World Health Organization (WHO) concluded that poor adherence to treatment is the most important cause of uncontrolled high blood pressure, with approximately 75% of patients not achieving optimum blood pressure control. The WHO estimates that between 20% and 80% of patients receiving treatment for hypertension are adherent. As such, the first objective of our study was to quantify the proportion of nonadherence to antihypertensive therapy in real-world observational study settings. The second objective was to provide estimates of independent risk indicators associated with nonadherence to antihypertensive therapy.
Materials and methods
We performed a systematic literature review and meta-analysis of all studies published between database inception and December 31, 2011 that reviewed adherence, and risk indicators associated with nonadherence, to antihypertensive medications.
Results
In the end, 26 studies met our inclusion and exclusion criteria and passed our methodological quality evaluation. Of the 26 studies, 48.5% (95% confidence interval 47.7%–49.2%) of patients were adherent to antihypertensive medications at 1 year of follow-up. The associations between 114 variables and nonadherence to antihypertensive medications were reviewed. After meta-analysis, nine variables were associated with nonadherence to antihypertensive medications: diuretics in comparison to angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) and calcium channel blockers (CCBs), ACE inhibitors in comparison to ARBs, CCBs in comparison to ARBs, those with depression or using antidepressants, not having diabetes, lower income status, and minority cultural status.
Conclusion
This study clarifies the extent of adherence along with determining nine independent risk indicators associated with nonadherence to antihypertensive medications.
Keywords:
Introduction
In a comprehensive report on nonadherence to long term therapies, the World Health Organization (WHO) stated that treatment of hypertension can reduce the risk of stroke by 30%–43% and myocardial infarction by 15%, along with reducing the risk of a number of other chronic conditions.Citation1 Similarly, in a meta-analysis of 147 randomized trials, the authors found that patients who received treatment with antihypertensive medications observed a 22% reduction in coronary heart disease events and a 41% reduction in stroke.Citation2 However, the WHO also concluded that poor adherence to treatment is the most important cause of uncontrolled high blood pressure, with approximately 75% of patients not achieving optimum blood pressure control.Citation1 The implications are vast. A meta-analysis on interventions for enhancing medication adherence completed by the Cochrane Collaboration concluded that effective ways to help patients follow medical treatments could have far larger effects on health outcomes than any individual treatment by itself.Citation3 For example, one review estimated that better adherence to antihypertensive therapy could prevent 89,000 premature deaths in the US alone on an annual basis.Citation4
In a meta-analysis on proportion and risk indicators for statin therapy, the authors found that only 49% of patients are adherent in real-world observational studies. After reviewing 147 variables, only six covariates were found to be independently associated with nonadherence to statin therapy: primary prevention, new statin users, copayment, lower income status, fewer than two lipid tests performed, and not having a comorbidity of hypertension.Citation5
To date, a systematic literature review and meta-analysis has not been performed on the extent of nonadherence to antihypertensive therapy. As such, the WHO had to estimate that between 20%–80% of patients receiving treatment for hypertension are adherent.Citation1 In other words, the true extent of nonadherence is not known and is a justification for this review.
The WHO also concluded that there is an urgent need for research to fill gaps in knowledge on the determinants of adherence.Citation1 Two systematic reviews have been published on variables associated with nonadherence to antihypertensive therapy. The first reviewed the impact of depression, but included self-report adherence information.Citation6 The second reviewed differences in adherence between angiotensin receptor blockers (ARBs) and other antihypertensive drug classes. However, the authors used filters to limit the search strategy and excluded studies that used a single point in time (ie, 1 year) to define adherence.Citation7 As well, both studies modified established quality-assessment rating checklists for their quality review.Citation6,Citation7
The first objective of our study was to quantify the proportion of adherence to antihypertensive therapy in real-world observational study settings. The second objective was to provide estimates of independent risk indicators associated with nonadherence to antihypertensive therapy.
Materials and methods
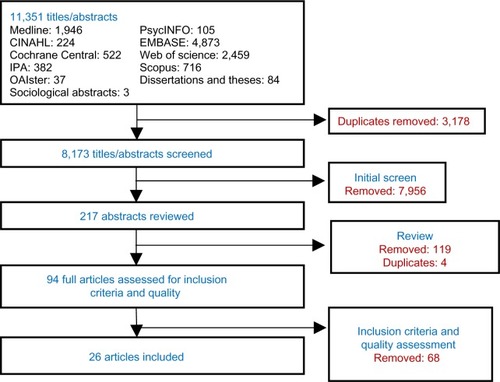
We performed a systematic literature review of electronic databases: Medline (Ovid), Embase (Ovid), International Pharmaceutical Abstracts (Ovid), the Cochrane Library, Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycINFO, Sociological Abstracts (ProQuest), ProQuest Dissertations and Theses, Theses Canada, and OAIster from inception to December 31, 2011. Multiple combinations of search terms and keywords were used to maximize the ability to capture relevant articles. Papers that were not published electronically were not included in our search. Reference sections of each article were reviewed for additional papers ().
Figure 1 Systematic literature-review process.
Studies were included if they satisfied the following criteria: 1) nonadherence to antihypertensive medications as an outcome, 2) antihypertensive medications included angiotensin-converting enzyme inhibitors (ACEIs), ARBs, beta blockers, calcium channel blockers (CCBs), or thiazide diuretics for any indication, 3) dispensation records as the source of objective nonadherence information, 4) conducted multivariable modeling to determine the independent effect of covariates on the outcome of nonadherence, and 5) published in the English language.
Abstracts and full-text articles were assessed by two reviewers for relevance (MWA and ML). Study quality was reviewed with a checklist developed by the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) for database studies. The checklist was developed for the specific purpose of critically evaluating the unique complexity of administrative datasets analyzing medication adherence.Citation8,Citation9 This checklist has been used in other systematic reviews.Citation10 It consists of 27 quality-review questions related to data source, research design, study population, variable definitions, statistics, and discussion. We established a rule a priori that studies scoring 14/27 or higher (greater than 50%) on the quality checklist would be included in the meta-analysis, unless there was a major methodological violation.
Disagreement between the two reviewers was resolved by additional review and discussion, and then, if required, with the senior author (ML) making a final decision. We assessed agreement between reviewers with κ-statistics.Citation11
We conducted a random-effects model meta-analysis using the inverse-variance method to estimate the effect of a risk indicator on medication adherence. A random-effects model accounts for potential heterogeneity between the populations and unmeasured confounding.Citation12–Citation15 Given that rates of adherence were being compared, rate ratios (RRs) were computed instead of odds ratios. Four or more articles were required for meta-analysis.
Sensitivity analysis reviewed the individual influence of a study by repeating the meta-analysis without studies with the largest and smallest relative weights. If this produced little change in inference (less than 15% change in rate ratio), inclusion of the study would not warrant caution in the interpretation. Sensitivity analysis also included country of origin and measures used to calculate adherence. We used the Z-test for overall effects and the χ2 statistic to test for differences in between-group effects. We included every risk indicator tested in other studies, but we obviously have no information on indicators that were not tested.
Results
A total of 11,351 titles and abstracts were identified. After review, and after removing duplicates, 217 abstracts were considered relevant to our study. From these, 94 articles were relevant, reviewed in full and evaluated for quality with the ISPOR checklist.Citation8,Citation9 Of these 94 articles, 26 passed the methodological quality reviewCitation16–Citation41 (). The κ-statistic for agreement between the reviewers for the final articles was 0.73. Even among approved studies, the methodological quality was low, with an average score of 16.8 out of a maximum of 27.
Of the 26 studies included for analysis, the most common follow-up duration was 12 months, for which 17 studies and 20 cohorts had data. Among these, with a total sample size of 1,522,203, 48.5% (95% confidence interval [CI] 47.7%–49.2%) of patients were adherent to antihypertensive medications at 1 year of follow-up, with a range from 20% to 88%. One study had a sample size of 725,220, which contributed 47.6% of the total sample. Removal of this one large study resulted in an adherence level of 56.9% (95% CI 56.7%–57.1%). This paper was also the only study conducted outside of North America and Europe with follow-up duration of 12 months. The two most common adherence measures were proportion of days covered and discontinuation, with adherence levels of 62.2% (95% CI 61.9%–62.5%) for proportion of days covered and 55.1% (95% CI 55.0%–55.2%) for discontinuation.
The second objective was to provide estimates of risk indicators associated with nonadherence to antihypertensive therapy. In total, the associations between 114 variables and nonadherence to antihypertensive medications were reviewed. In the end, nine variables were associated with nonadherence to antihypertensive medications, with five representing drug class and four from variables other than drug class ( and ).
Figure 2 Covariates independently associated with nonadherence to antihypertensives.
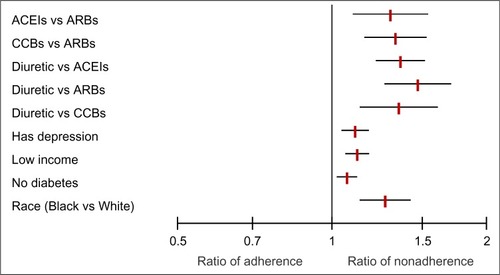
Table 1 Results of individual studies
For five studies and seven cohorts with a total sample size of 1,082,417, patients who were dispensed diuretics, in comparison to ACEIs, were 36% more likely to be nonadherent (RR 1.36, 95% CI 1.22–1.51). Among five studies and seven cohorts with a total sample size of 1,028,044, patients who were dispensed diuretics, in comparison to ARBs, were 47% more likely to be nonadherent (RR 1.47, 95% CI 1.27–1.70). For three studies and five cohorts with a total sample size of 295,512, patients who were dispensed diuretics, in comparison to CCBs, were 35% more likely to be nonadherent (RR 1.35, 95% CI 1.14–1.60). Pooling of four studies with a total sample size of 232,665 revealed that patients who were dispensed ACEIs, in comparison to ARBs, were 30% more likely to be nonadherent (RR 1.30, 95% CI 1.10–1.54). Analysis of four studies with a total sample size of 936,162 showed that patients who were dispensed CCBs, in comparison to ARBs, were 33% more likely to be nonadherent (RR 1.33, 95% CI 1.16–1.54).
There were five studies and eight cohorts that reviewed the association between depression or the use of antidepressants and nonadherence. With a total sample size of 206,673, patients who were either depressed or dispensed antidepressants were 11% more likely to be nonadherent to antihypertensive medications (RR 1.11, 95% CI 1.05–1.18).
Comparing lowest-income to highest-income groups among nine studies and 13 cohorts with a sample size of 623,444, we found that lower-income groups were 12% more likely to be nonadherent (RR 1.12, 95% CI 1.06–1.18). Some studies reviewed race. Analysis of five studies and seven cohorts with a sample size of 1,771,428 revealed that residents who were of minority cultural status (African American race in American studies) in comparison to Caucasian (White) were 27% more likely to be nonadherent (RR 1.27, 95% CI 1.14–1.42).
There were eight studies and 13 cohorts that reviewed the association between having diabetes and nonadherence. With a total sample size of 252,306, patients without diabetes were 7% more likely to be nonadherent to antihypertensive medications (RR 1.07, 95% CI 1.02–1.11).
There was no known association between the other 105 variables and nonadherence to antihypertensive medications. For example, patients with ischemic heart disease were only 3% more likely to be nonadherent to antihypertensive medications (RR 1.03, 95% CI 0.90–1.18). As another example, patients with heart failure were 5% more likely to be nonadherent to antihypertensive medications (RR 1.05, 95% CI 0.98–1.12).Citation42
Tests of homogeneity of variance for the nine variables associated with nonadherence were all P<0.001. This suggests highly significant heterogeneity between the studies. Stratification by country of origin and measure of adherence did not alter estimates to a significant degree. As well, sensitivity analysis of removing studies with the largest and smallest relative weights did not alter estimates to a significant degree. For example, removing non-North American and -European studies and removing the study with the largest sample size modified the odds ratio between diuretics and ACEIs from 1.36 (95% CI 1.22–1.51) to 1.40 (95% CI 1.24–1.56).
Only three variables had negative estimates or results contrary to the other studies in the meta-analysis. Among eight cohorts that reviewed the association between depression or the use of antidepressants and nonadherence, one estimate was inconsistent with the other seven. For the thirteen cohorts that reviewed income, two estimates were inconsistent with the other eleven estimates. Among thirteen cohorts that reviewed the association between diabetes and nonadherence, two estimates were inconsistent with the other eleven.
All of the included papers are summarized in detail in Table S1.
Discussion
Of the 26 studies that were included in our study and passed methodological quality review, 48.5% (95% CI 47.7%–49.2%) of patients were adherent to antihypertensive medications at 1 year of follow-up. This clarifies the original WHO estimate that between 20% and 80% of patients receiving treatment for hypertension are adherent.Citation1 This is simply a range from the lowest to the highest rates found during their review. Policy makers and health practitioners could assume that nonadherence is as low as 20% and therefore not a major problem. We quantified the value through meta-analysis in order to clarify the need for action.
Our study also provides estimates of known risk indicators associated with nonadherence to antihypertensive therapy. In total, the associations between 114 variables and nonadherence to antihypertensive medications were reviewed. In the end, nine variables were associated with nonadherence to antihypertensive medications: diuretics in comparison to ACEIs and ARBs and CCBs, ACEIs in comparison to ARBs, CCBs in comparison to ARBs, those with depression or using antidepressants, not having diabetes, lower income status, and minority cultural status (African American race).
Although drug class has been shown to impact adherence, it is not clear if this is due to the properties of the drug class itself. One review suggests that differences may be due to patient selection or that out-of-pocket cost predicts drug choice.Citation7 Also, the reality is that many patients are now started on more than one antihypertensive medication and combinations of drug classes.Citation7 A recent paper found that differences in adherence by drug class were associated with their market availability, and that combination therapy of ARBs with diuretics had the highest proportion of adherence.Citation43 Others would suggest that there are clinical differences like increased urination associated with diuretics.Citation44 Regardless, our results were consistent with a meta-analysis that reviewed adherence of ARBs in comparison to other antihypertensive medications, although our study reviewed all drug classes.Citation7
Depression is known to be associated with a threefold-greater risk of nonadherence to medical treatment in general.Citation45 A previous systematic literature review found that definitive conclusions could not be drawn between depression and nonadherence to antihypertensive therapy, possibly because five of the eight accepted studies included nonobjective and self-report measures to determine nonadherence.Citation6 Our review addressed this limitation.
Not having diabetes was also associated with nonadherence, although the effect was small. Patients who have a low perceived risk of disease have been found less likely to adhere to their medications.Citation5 Lower-income status might also increase nonadherence due to affordability, although low-income status has also been associated with nonadherence to other health-seeking behaviors.Citation46–Citation49 The association between cultural status and adherence is likely to be due to confounding with income.Citation50 In the US, African American cultural status is well known to be more likely associated with lower-income status at the population level.Citation51
The main limitation of our meta-analysis was the inclusion of studies with wide variability and heterogeneity in measuring and defining adherence. Second, although our meta-analysis identified nine variables associated with nonadherence to antihypertensive medications, it remains unclear as to what extent adherence would be improved if these variables were addressed. Third, our interpretation is limited to variables reviewed. It is likely that other untested associations exist.
Conclusion
The known effectiveness of interventions for enhancing chronic disease medication adherence remains surprisingly weak.Citation3 It is possible that this lack of effectiveness is due to not really knowing the risk indicators of nonadherence. This study provides some insight into factors associated, and not associated, with nonadherence to antihypertensive medications.
In summary, it is likely that effective ways to help patients follow medical treatments could have far larger effects on health outcomes than any individual treatment. The first step is to know the extent of nonadherence in patients and populations. The second is to have some idea as to what variables are associated with nonadherence.
Acknowledgments
Thank you to Dr David Blackburn from the College of Pharmacy and Nutrition at the University of Saskatchewan.
Disclosure
MWA’s student position at the University of Saskatchewan is funded through unrestricted financial support from the Government of Saskatchewan’s Ministry of Health, which in turn obtained unrestricted financial support from AstraZeneca Canada, Merck Frosst/Schering, and Pfizer Canada. None of these sponsors had input into the drafting or submission of this manuscript. ML reports no conflicts of interest in this work.
References
- World Health OrganizationAdherence to Long-Term Therapies: Evidence for ActionGenevaWHO2003
- LawMRMorrisJKWaldNJUse of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studiesBMJ2009338b166519454737
- HaynesRBYaoXDeganiAKripalaniSGargAMcDonaldHPInterventions for enhancing medication adherenceCochrane Database Syst Rev2005CD00001116235271
- CutlerDMEverettWThinking outside the pillbox – medication adherence as a priority for health care reformN Engl J Med20103621553155520375400
- LemstraMBlackburnDFCrawleyAFungRProportion and risk indicators of non-adherence to statin therapy: a meta-analysisCan J Cardiol201228557458022884278
- Eze-NiliamCMThombsBDLimaBBSmithCGZiegelsteinRCThe association of depression with adherence to antihypertensive medications: a systematic reviewJ Hypertension20102817851795
- KronishIMWoodwardMSergieZOgedegbeGFalzonLMannDMMeta-analysis: impact of drug class on adherence to antihypertensivesCirculation20111231611162121464050
- PetersonAMNauDPCramerJABennerJGwadry-SridharFNicholMA checklist for medication compliance and persistence studies using retrospective databasesValue Health20071031217261111
- MotheralBBrooksJClarkMAA checklist for retrospective database studies – report of the ISPOR task force on retrospective databasesValue Health20036909712641858
- AlsabbaghWLemstraMEurichDSocioeconomic Status and Non Adherence to Anti-Hypertensive Drugs: A Systematic Review and Meta-AnalysisValue in Health2014 Available from: http://www.ispor.org/publications/value/articlesinpress.aspAccessed February 4, 2014
- DouglasGAPractical Statistics for Medical Research1st edNew YorkChapman and Hall1991
- FleissJlThe statistical basis of meta-analysisStat Methods Med Res199321211458261254
- Huedo-MedinaTBSánchez-MecaJMarín-MartínezFBotellaJAssessing heterogeneity in meta-analysis: Q statistic or I2 index?Psychol Methods20061119320616784338
- HigginsJPGreenSCochrane Handbook for Systematic Reviews of InterventionsChichester, UKJohn Wiley & Sons2006
- DerSimonianRLairdNMeta-analysis in clinical trialsControl Clin Trials198671771883802833
- RasmussenJNChongAAlterDARelationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarctionJAMA200729717718617213401
- SetoguchiSChoudhryNKLevinRShrankWHWinkelmayerWCTemporal trends in adherence to cardiovascular medications in elderly patients after hospitalization for heart failureClin Pharmacol Ther20108854855420827266
- MonaneMBohnRLGurwitzJHGlynnRJLevinRAvornJThe effects of initial drug choice and comorbidity on antihypertensive therapy compliance: results from a population-based study in the elderlyAm J Hypertens1997106977049234822
- BloomBSContinuation of initial antihypertensive medication after 1 year of therapyClin Ther1998206716819737827
- Degli EspostiLDegli EspostiEValpianiGA retrospective, population-based analysis of persistence with antihypertensive drug therapy in primary care practice in ItalyClin Ther20022413471357 discussion 134612240784
- YangYThumulaVPacePFBanahanBF3rdWilkinNELobbWBPredictors of medication nonadherence among patients with diabetes in Medicare part D programs: a retrospective cohort studyClin Ther20093121782188 discussion 2150–215119922889
- ShayaFTDuDGbarayorCMFrech-TamasFLauHWeirMRPredictors of compliance with antihypertensive therapy in a high-risk Medicaid populationJ Natl Med Assoc2009101343919245070
- ElliottWJPlauschinatCASkrepnekGHGauseDPersistence, adherence, and risk of discontinuation associated with commonly prescribed antihypertensive drug monotherapiesJ Am Board Fam Med200720728017204738
- PerreaultSLamarreDBlaisLPersistence with treatment in newly treated middle-aged patients with essential hypertensionAnn Pharmacother2005391401140816076920
- TairaDAGelberRPDavisJGronleyKChungRSSetoTBAntihypertensive adherence and drug class among Asian Pacific AmericansEthn Health20071226528117454100
- van WijkBLShrankWHKlungelOHSchneeweissSBrookhartMAAvornJA cross-national study of the persistence of antihypertensive medication use in the elderlyJ Hypertens20082614515318090552
- LambDEurichDMcAlisterFChanges in adherence to evidence-based medications in the first year after initial hospitalization for heart failure: observational cohort study from 1994 to 2003Circ Cardiovasc Qual Outcomes2009222823520031842
- GogovorADragomirASavoieMPerreaultSComparison of persistence rates with angiotensin-converting enzyme inhibitors used in secondary and primary prevention of cardiovascular diseaseValue Health20071043144117888108
- SiegelDLopezJMeierJAntihypertensive medication adherence in the Department of Veterans AffairsAm J Med2007120263217208076
- FriedmanOMcAlisterFAYunLCampbellNRTuKAntihypertensive drug persistence and compliance among newly treated elderly hypertensives in OntarioAm J Med201012317318120103027
- CorraoGZambonAParodiADo socioeconomic disparities affect accessing and keeping antihypertensive drug therapy? Evidence from an Italian population-based studyJ Hum Hypertens20092323824418668127
- EagleKAKline-RogersEGoodmanSGAdherence to evidence-based therapies after discharge for acute coronary syndromes: an ongoing prospective, observational studyAm J Med2004117738115234641
- WogenJKreilickCALivorneseRCYokoyamaKFrechFPatient adherence with amlodipine, lisinopril, or valsartan therapy in a usual-care settingJ Manag Care Pharm2009942442914613440
- YangYThumulaVPacePFBanahanBF3rdWilkinNELobbWBNonadherence to angiotensin-converting enzyme inhibitors and/or angiotensin II receptor blockers among high-risk patients with diabetes in Medicare part D programsJ Am Pharm Assoc201050527531
- KramerJMHammillBAnstromKJNational evaluation of adherence to beta-blocker therapy for 1 year after acute myocardial infarction in patients with commercial health insuranceAm Heart J2006152454e1e816923412
- Degli EspostiESturaniADi MartinoMLong-term persistence with antihypertensive drugs in new patientsJ Hum Hypertens20021643944412037702
- WongMCJiangJYSuXWangHTangJLGriffithsSMIndividuals at risk of beta-blocker discontinuation: a cohort study in 19,177 Chinese patientsClin Res Cardiol20109927728420174812
- SungSKLeeSGLeeKSKimDSKimKHKimKYFirst-year treatment adherence among outpatients initiating antihypertensive medication in Korea: results of a retrospective claims reviewClin Ther2009311309132019695396
- EvansCDEurichDTRemillardAJShevchukYMBlackburnDFirst-fill medication discontinuations and nonadherence to antihypertensive therapy: an observational studyAm J Hypertens20122519520322089108
- RasmussenJNGislasonGHRasmussenSUse of statins and beta-blockers after acute myocardial infarction according to income and educationJ Epidemiol Community Health2007611091109718000133
- CarraoGParodiAZambonAReduced discontinuation of anti-hypertensive therapy by two-drug combination as first step. Evidence from daily life practiceJ Hypertens2010281584159020543716
- World Health OrganizationICD-10: International Statistical Classification of Diseases and Related Health ProblemsNew YorkWHO2008
- EvansCDEurichDTLuXRemillardAJShevchukYMBlackburnDThe association between market availability and adherence to antihypertensive medications: an observational studyAm J Hypertens20132618019023382402
- Canadian Pharmacists AssociationCompendium of Pharmaceuticals and Specialties: Thiazide Diuretics – Product MonographOttawaCanadian Pharmacists Association2012
- DiMatteoMRLepperHSCroghanTWDepression is a risk factor for noncompliance with medical treatment: a meta-analysis of the effects of anxiety and depression on patient adherenceArch Intern Med20001602101210710904452
- OsterbergLBlaschkeTAdherence to medicationN Engl J Med200535348749716079372
- O’MalleyASForrestCBMandelblattJAdherence of low-income women to cancer screening recommendationsJ Gen Intern Med20021714415411841530
- CelanoMGellerRJPhillipsKMZimanRTreatment adherence among low-income children with asthmaJ Pediatr Psychol1998233453499824922
- OrlandiMAPromoting health and preventing disease in health care settings: an analysis of barriersPrev Med1987161191303823010
- DiamondJGuns, Germs, and Steel: The Fates of Human SocietiesNew YorkWW Norton1999
- US Census BureauPeople below poverty level and below 125 percent of poverty level by race and Hispanic origin: 1980 to 2009–2012 Available from: http://www.census.gov/compendia/statab/2012/tables/12s0711.pdfAccessed January 24, 2013
