Abstract
Background
Adherence to treatment is an important issue in chronic disease management and an indicator of patients’ ability to self-manage their condition and treatment. Some drug-dispensing and drug-delivery devices have been designed to support patients’ medication-taking behavior by including dose-memory and combined dose-memory and dose-reminder functions, which electronically store, and visually display dose-history information, enabling the patient to review, monitor, and/or be actively reminded about their medication doses.
Purpose
This literature review explored the role and impact of these devices on patients’ treatment adherence, confidence with, and self-management of their condition and treatment.
Materials and methods
A search of MEDLINE, Embase, and PsycINFO was performed to identify articles published in English from 2003–2013 that studied the effect of devices with dose-memory and combined dose-memory and dose-reminder functions on treatment adherence and users’ (patients, health care professionals [HCPs], and caregivers) confidence, self-management behavior, and attitudes.
Results
The database searches yielded 940 abstracts from which 13 articles met the inclusion criteria and were retained. Devices with dose-memory and combined dose-memory and dose-reminder functions were found to improve self-reported and electronically monitored treatment adherence in chronic conditions such as asthma, diabetes, and HIV. The ability of the devices to provide dose-history information and active medication reminders was considered valuable in disease management by patients, caregivers, and HCPs. The devices were found to enhance patients’ confidence in, and motivation to manage their medication and condition, and help reduce forgotten or incorrect medication dosing.
Conclusion
The incorporation of dose-memory and combined dose-memory and dose-reminder functions in drug-delivery devices can improve patients’ adherence, confidence, and self-management behavior. They can target non-intentional barriers to adherence and can provide a means of improving disease control and clinical outcomes, thereby offering clinical and economic value. This review highlights the importance of conducting further qualitative and quantitative research to further understand the value and impact of these types of devices on patients’ long-term adherence to, and self-management of treatment.
Introduction
Patient adherence (or lack thereof) to prescribed medication regimens is a complex and multidimensional behavior. Patient adherence is one of the most widely researched topics of recent times and attempts to understand, measure, predict, and enhance patients’ medication-taking behavior have been documented throughout the literature.Citation1,Citation2
Adherence can be defined as the degree to which a patient’s medication-taking behavior and/or executing of lifestyle changes (eg, following a diet) correspond with agreed recommendations from a health care professional (HCP) with respect to timing, dosage, and frequency.Citation1,Citation3 The term adherence is often used interchangeably with the term “compliance”;Citation3 however, their connotations differ: adherence presumes that the patient is an active collaborator in the treatment process, whereas compliance suggests that the patient is not part of a therapeutic alliance and is passively following the orders of a HCP.Citation4–Citation6
Nonadherence to prescribed treatment regimens (eg, medications, screening, exercise, diet) is problematic, with estimates across empirical studies averaging 25%.Citation7 Reviews have shown that nonadherence is a prevalent problem in patients with chronic conditions such as diabetes, asthma, hypertension, and HIV/AIDs. Adherence rates are typically lower within this population as compared to those with acute conditions, with patients with chronic conditions achieving an average of only 50% adherence to prescribed medication, regardless of prognosis or disease progression.Citation8
Nonadherence to medication regimens, whether willful or inadvertent can include taking an incorrect dose, taking the medication at the wrong time, forgetting to take the medication, polypharmacy, and improper use of a medication administration device (eg, auto-injector or inhaler).Citation5,Citation9 Poor adherence compromises treatment efficacy and leads to suboptimal disease control and poor clinical outcomes such as preventable disease progression and complications, adverse events, reductions in health-related quality of life, disability, and even death.Citation1,Citation10 Poor adherence also results in poor economic outcomes, contributing to an increased use of health care services and expenditures.Citation1,Citation11,Citation12 Within the US alone, nonadherence is estimated to account for 10% of hospitalizations and 23% of nursing home admissions,Citation13 with resultant costs of approximately US$100 billion per year.Citation14–Citation16
The barriers to patient adherence are multidimensional and can include a complex interplay of patient-centered factors and external factors relating to the patients’ HCP, condition, and medication and/or society and economy.Citation1,Citation16,Citation17 For example, the act of forgetting is one of the most frequently cited reasons for poor adherence,Citation18 whether due to lifestyle factors such as having a busy routine or being tired, or clinical factors such as dementia. Fear of or experience of treatment side effects are also reported as major reasons for nonadherence.Citation18 In addition, poor adherence is often observed among patients who have complex or variable treatment regimens, with adherence rates shown to decrease as the number of required daily medication doses increases.Citation19 Other reasons for patient nonadherence include having poor communication and lack of a relationship with a HCP, having a lack of understanding and knowledge about their condition, strong cultural or lay beliefs, or a lack of self-confidence to manage their treatment regimen.Citation5,Citation20–Citation23
Patients with chronic conditions play a large role in the management of their condition. Patients with diabetes, for example, provide close to 95% of their own care, which includes the integration of a series of complex daily actions such as measuring blood glucose levels, administering variable doses of insulin, and dietary control.Citation24,Citation25 Such self-management involves the medical, social, and emotional aspects of living with, adjusting to, and monitoring of a long-term chronic condition over a lifetime in a dynamic and continual state of self-regulation.Citation26 Together, self-management and adherence encompass the activities that patients must carry out to regulate their illness and cope with the impact of their condition and treatment on themselves and others. Adherence to these complex regimens is a crucial factor in the success of a treatment, and therefore, the suboptimal adherence rates seen among patients with chronic conditions are seen as an indication of patients’ (in)ability to self-manage their condition and treatment.Citation27
Across the literature, there is a consistent and unequivocal finding that adherence problems occur across all situations where the self-administration and self-management of treatment is required, regardless of disease type, disease severity, and access to health care resources.Citation1 In chronic conditions such as type 1 diabetes for example, approximately one in three patients are nonadherent to insulin regimens, which can lead to poor glycemic control and an increase in hemoglobin A1c (HbA1c) above the target level of 6.5%.Citation28,Citation29 It has been demonstrated that forgetting or omitting 2.1 meal-related insulin injections per week can cause an increase in HbA1c of 0.3%–0.4% points, thus contributing to decreased glycemic control.Citation29 To further illustrate the magnitude of poor glycemic control within this population, only 37% of US patients with diabetes are estimated to achieve the clinical outcome of less than 7% HbA1c.Citation30 Similarly, across other chronic disease areas, nonadherence to hypertensive medication compromises the clinical goal of controlling high blood pressure to a level of <140/90 mmHg and doubles the risk of stroke, myocardial infarction, and cardiovascular mortality.Citation1,Citation31 Therefore, better understanding of nonadherence is important in order to accurately monitor, evaluate, and manage treatment outcomes and improve patient care.Citation32 It has been suggested that “increasing the effectiveness of adherence interventions may have a far greater impact on the health of the population than any improvement in specific medical treatments.”Citation8
A multitude of drug-dispensing, drug-delivery, and reminder devices have been developed over the years, aimed at monitoring and improving patients’ self-management and adherence behavior. At the forefront of adherence monitoring are medication event monitoring systems (MEMS), which are widely reported within the literature as the gold standard measure of patient adherence. MEMS typically compile the dose-history of patients prescribed oral medications via a microprocessor included in the medication bottle top/device, which provides time-stamped records of the numbers of opening or actuations. This information can then be transferred and analyzed via computer, enabling a HCP or researcher to track a patient’s adherence. MEMS do not, however, provide non-clinician–controlled “real time” dose-history information directly to the patient, enabling them to self-monitor their medication-taking behavior and facilitate adherence. Devices designed to directly improve adherence range from simple calendar pillboxes and blister packaging, aimed at assisting patients with medication scheduling, to electronic devices with inbuilt dose-count and dose-memory functions that provide the patient with predetermined audio and/or visual medication monitoring and dose-reminders, or information about the date, time, and volume of their last medication dose to facilitate successive dose-taking.Citation2,Citation8,Citation33
A new wave of drug-delivery technology now exists, primarily in conditions requiring the use of auto-injectors such as diabetes (eg, NovoPen Echo®, Novo Nordisk A/S, Bagsværd, Denmark) and growth hormone deficiency (eg, Easypod®, Merck Serono, International SA, Geneva, Switzerland) which now feature inbuilt or aftermarket device dose-memory functions (eg, InsulCheck®, Innovation Zed Ltd., Dublin, Ireland) to facilitate treatment self-management and variable dose-monitoring. These devices enable the patient to directly record and monitor their own medication-taking behavior without involvement from a HCP. Use of electronic dose-memory and combined dose-memory and dose-reminder devices to facilitate patient self-management can also reduce the burden on caregivers and offer a solution for patients who are unintentionally nonadherent.Citation32,Citation33 In addition, such devices could potentially reduce the cognitive, emotional, and physical burdens associated with a condition that contribute to nonadherence, and promote increased confidence in patients by helping them deal with these barriers to adherence.Citation32
A vast array of adherence literature exists relating to MEMS and medication reminder systems; however, despite new developments and the increasing recognition of the potential value devices with dose-memory functions may have, little has been done to consolidate evidence regarding their link with adherence as well as other benefits for patients and the wider health care system. Thus, a targeted literature review was conducted to explore the role and impact of medical devices with dose-memory and combined dose-memory and dose-reminder functions on patients’ treatment adherence, confidence with, and self-management of their condition and treatment.
Materials and methods
Published peer-reviewed articles were identified via searches performed in MEDLINE, Embase, and PsycINFO electronic bibliographic databases. Searches were performed across the three databases using device, memory, and patient-related terms combined using Boolean logic commands (). Searches were conducted on January 6, 2013, and limited to articles published between 2003 to 2013, published in the English language, and limited to humans.
Table 1 Search terms for identification of peer-reviewed articles
All abstracts were reviewed by two independent researchers. For consideration for inclusion in the review, selected abstracts were required to make reference to the effects of patient-used medical devices with dose-memory or combined dose-memory and dose-reminder functions on treatment adherence within, but not limited to chronic conditions, device usability, and users’ (patients, HCPs, and caregivers) relationship and attitudes towards the devices. The reference lists of the selected articles were also reviewed to identify additional papers not retrieved from the database searches. The final list of abstract and articles selected for in-depth review was agreed following consensus between the authors. Key information on each selected article regarding the study design, study aims, sample characteristics, device type, methodology, and results were evaluated and summarized in data extraction tables.
Results
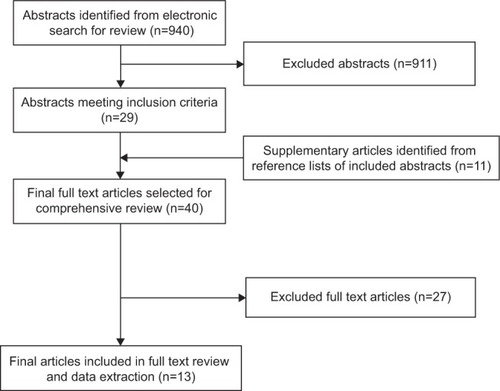
Searches in the electronic bibliographic databases returned a combined total of 940 abstracts; however, due to the niche area under investigation, 911 were excluded. Abstracts were excluded because they either failed to report on patient-used drug-dispensing or drug-delivery devices at all (eg, clinical guidelines, health service evaluation, and medication efficacy reviews) or reported on devices irrelevant to the current study (eg, MEMS, dose-reminder devices without dose-memory functions, clinician-used medical devices, and devices measuring physiological parameters [eg, high blood pressure or blood glucose monitors]). Abstracts were also excluded if they discussed general adherence and compliance monitoring, or non-medical content. A total of 29 articles were selected for full text review, and following review of their reference lists, a further eleven articles were selected for inclusion. Of the 40 articles identified for full text review, 27 were omitted as they did not contain relevant content to the concepts of interest as expected from their abstracts. A final total of 13 articles were selected for inclusion in this review and data extraction ().Citation34–Citation46 Of the 13 included studies, eight (61.5%) utilized patient-used dose-memory function devicesCitation34,Citation38–Citation41,Citation43,Citation44,Citation46 and five utilized combined dose-memory and dose-reminder functionalities (38.5%),Citation35–Citation37,Citation42,Citation45 which electronically store, and visually display dose-history information, enabling the patient to review, monitor, and/or be actively reminded about their medication doses.
The conditions in which these studies were implemented included diabetes (type 1 and/or 2) (n=7, 53.8%),Citation34,Citation39–Citation41,Citation43,Citation44,Citation46 hypertension (n=2, 15.4%),Citation37,Citation45 asthma (n=1, 7.7%),Citation36 HIV/AIDS (n=1, 7.7%),Citation35 growth hormone deficiency (n=1, 7.7%),Citation38 and rhinoconjunctivitis (n=1, 7.7%).Citation42
Different study designs were utilized across the 13 studies such as observational studies and randomized control trials. The studies included research conducted worldwide using ethnically and racially diverse samples and both adult (n=9, 69.2%)Citation35,Citation37–Citation40,Citation42,Citation43,Citation45,Citation46 and adolescent (n=2, 15.4%),Citation34,Citation44 as well as combined age populations (n=2, 15.4%).Citation36,Citation41 The studies, the devices implemented, and their results are presented in .
Table 2 Summary of included studies
The dose-memory function devices comprised three diabetes insulin pens (NovoPen Echo®, NovoPen® 5 [Novo Nordisk A/S], and HumaPen® Memoir™ [Eli Lilly and Company, Indianapolis, IN, USA]) and one recombinant human growth hormone (r-hGH) auto-injector (Easypod®, [Merck Serono]), utilized in sevenCitation34,Citation39–Citation41,Citation43,Citation44,Citation46 and one study, respectively.Citation38 These dose-memory function devices all included an electronic dose-history log that recorded the last dose volume and time since the last injection.
The five devices, which all incorporated a combined dose-memory and dose-reminder function, featured either an auditory reminder (n=4)Citation35,Citation36,Citation42,Citation45 or a combined auditory and visual reminder (n=1)Citation37 that actively reminded the patient to take their medication. The dose-memory function capabilities of these devices included either a detailed dose-memory functionality (eg, electronic dose history log; such as the Disease Management Assistance System [DMAS; HIV/AIDS]Citation35 and Intelligent Drug Administration System [IDAS II; Bang and Olufsen Medicom, Struer, Denmark; hypertension]),Citation45 or provided general feedback about dosing adherence (eg, visual indicators of past adherence; such as the Smartinhaler [Nexus6 Ltd, Auckland, New Zealand; asthma],Citation36 Helping Hand [hypertension; Bang and Olufsen Medicom],Citation37 and Memozax®42 [ALK-Abelló A/S; Hørsholm, Denmark; rhinoconjunctivitis]).
Impact of dose-memory and dose-reminder devices on patient adherence
Five of the 13 (38.5%) studies explored the impact of dose-memory and combined dose-memory and dose-reminder functions on patient adherence: four based on objective measures of adherenceCitation35,Citation36,Citation39,Citation45 using the HumaPen® Memoir™ in type 1 diabetes, or MEMS (eg, electronic-drug exposure caps; see Andrade et al and Santschi et al)Citation35,Citation45 in HIV, asthma, and hypertension, and one study based on subjective self-report questionnaires in type 1 diabetes.Citation34
Objective assessments of adherence
Two of the four studies that used objective measures of adherence in HIVCitation35 and asthmaCitation36 indicated that devices with combined dose-memory and dose-reminder functions improved patients’ adherence to medication when compared to a control group. For example, Charles et alCitation36 assessed whether a metered dose inhaler (MDI) with an audiovisual reminder function (AVRF) improved adherence to inhaled corticosteroid use among asthma patients. A significant improvement in median adherence at 12 weeks (median difference: 18%, P<0.0001) was found among patients using the MDI with an AVRF (93%), compared to a control group using the MDI without an AVRF (74%). They also found that the proportion of patients taking >50%, >80%, and >90% of their medication was significantly higher in patients using the MDI with AVRF, with a ratio of proportions adherent of 1.33 (95% confidence interval [CI]: 1.10–1.61; P=0.003), 2.27 (95% CI: 1.56–3.3; P<0.0001), and 3.25 (95% CI: 1.74–6.1; P<0.0001), respectively. Furthermore, patients using the MDI with AVRF were significantly less likely to “dose dump” (ie, take multiple doses in a short time period) than the control group (0.25, 95% CI: 0.09–0.7; P=0.008).
The effects of combined dose-memory and dose-reminder devices on adherence to highly active antiretroviral therapy (HAART) were assessed in a study implementing the DMAS in HIV patients with clinically confirmed memory impairments.Citation35 Andrade et alCitation35 found significantly higher adherence rates among HIV patients with memory impairments who used the DMAS (77%), compared to a control group who did not (57%). Similarly, there was also a trend for improved adherence among memory-intact HIV patients who used the DMAS (83%), compared to those who did not (77%); however, this finding was not significant. These findings suggest that such devices can be beneficial for all types of patients who cite forgetting as a reason for nonadherence.
Santschi et alCitation45 used an objective measure of adherence, whereby 24 patients with hypertension each used the IDAS II (with combined dose-memory and dose-reminder function) and a MEMS device, which recorded the number of medication bottle openings and time since last opening, for 2 months.Citation45 Over the 4-month study period, adherence to antihypertensive medication was found to be excellent (99.2%), with comparable rates for both devices in terms of the percentage of doses taken, the percentage of days with correct dosing, and the percentage of correct intervals between doses. There was, however, significantly less variation in the regularity of drug intake timing when using the IDAS II (P<0.001) as demonstrated by a small timing distribution index of 0.60, compared to a distribution index of 1.03 when using the MEMS device. This finding indicates that patients using the IDAS II showed stricter adherence to taking their medication at the same time each day and stricter medication persistence, taking it for the duration of the study.
In the last study using objective measures of adherence, however, use of the HumaPen® Memoir™ with dose-memory function was not associated with improved adherence and superior glycemic control in patients with type 1 diabetes when compared to the HumaPen Luxura™ (Eli Lilly and Company) without dose-memory function.Citation39 Although the two HumaPens had identical mechanical platforms and single dosing increments, this finding suggests that adherence to injection schedules was not improved by the additional dose-memory function of the HumaPen® Memoir™. Several limitations were present in this study, however, which affects the validity of the findings. Limitations include the fact that the number of missed injections and number of corrective actions taken based on the dose-memory function were not recorded; therefore, it is unclear how these were associated with increases and reductions in HbA1c, respectively. The HumaPen® Memoir™ was also only used for mealtime insulin injections, which in very poorly controlled diabetes patients, may be insufficient to achieve a relevant HbA1c reduction independently of fasting blood glucose control. Extremely noncompliant patients stand to benefit most from devices targeting improved adherence; however, this population was perhaps overrepresented in the study, as indicated by 40.1% of patients having very poor glycemic control (baseline HbA1c >9%).Citation39 It is possible that this overrepresentation when combined with other methodological limitations of the study, contributed to the failure to discriminate between the assumed benefit of an injection device with dose-memory function, compared to one without.
Subjective assessments of adherence
Adolfsson et alCitation34 explored the impact of the NovoPen Echo® (with a dose-memory function) on adherence to diabetes insulin injections in patients aged 2–18 years old. Forgotten injections administered by patients or their parents were reported for 27% of patients when using the NovoPen Echo®, as compared to 51% of patients using a pre-study insulin pen (unspecified by the authors), without a dose-memory function (P=0.0001). The authors also report that a higher proportion of children and adolescents self-injected rather than relying on parental administration when using the NovoPen Echo® (71%), as compared to their pre-study insulin pen (66%).
Satisfaction with the usability, functionality, and user/prescriber impact of dose-memory and dose-reminder devices
A total of nine studies reported patients’ and clinicians’ attitudes towards the usability, functionality, and impact of devices with dose-memory and combined dose-memory and dose-reminder device functions.Citation37,Citation38,Citation40–Citation46
Attitudes to dose-memory devices
Favorable responses were reported for devices with a dose-memory function among patients with diabetes and those requiring r-hGH. Guo et alCitation40 found that patients reported feeling considerably more confident managing their daily insulin injections using the NovoPen® 5 (with dose-memory function) than the HumaPen Luxura™ and ClikSTAR® (Sanofi-Aventis, Paris, France) (both without dose-memory function) because the NovoPen® 5 allowed them to review the volume (42%) and time (39%) of their last dose. This was supported by HCPs, with 75% agreeing that the dose-memory device function was particularly valuable for patients who tended to forget to perform injections.
The NovoPen® 5 (with dose-memory function) was also rated by patients and HCPs as their preferred insulin pen (82% and 79%, P<0.0001, respectively) versus the HumaPen Luxura®, which does not contain a dose-memory function (17% and 19%, P<0.0001, respectively).Citation43 The dose-memory function was cited by 56% of patients as their primary reason for preferring the NovoPen® 5. Patients reported feeling that the NovoPen® 5 would improve their daily diabetes management and enable them to feel more confident about the time and volume of their last dose. Patients also felt that the device would help promote successful control of their blood glucose levels.
Olsen et alCitation44 also concluded that the dose-memory function of the NovoPen® 5 “completely met” the needs of patients with diabetes (including children and adolescents) as well as the needs of their parents and HCPs. In addition, 89% of all participants in the study preferred the NovoPen® 5 compared with the NovoPen® Junior (Novo Nordisk A/S) and HumaPen® Luxura™ HD (Eli Lilly and Company), which did not have a dose-memory function. Participants reported that they found the NovoPen® 5 easier to use, making them feel more certain that they had administered a full dose of their injection.
Preference for an insulin pen that included a dose-memory function (HumaPen Memoir®) was also found in a study reported by Venekamp et alCitation46 and Ignaut and Venekamp.Citation41 In this study, 54% of patients and 75% of HCPs reported that they would recommend this device to other patients because of the dose-memory function.Citation46 The dose-memory function was considered beneficial by HCPs because patients could confirm that an injection had been taken, view the units of the previous dose, and view the time of the previous dose. Only 15% of patients in this study felt that the dose-memory function was not an important feature at all.
Similarly, in a study that explored the acceptability of the Easypod® auto-injector with dose-memory function for r-hGH, 96% of patients reported having a display of their last injection date “useful” or “very useful” and 69% reported having access to their dose history “useful” or “very useful”.Citation38
Attitudes to combined dose-memory and dose-reminder devices
Similar findings were found in studies looking at devices with combined dose-memory and dose-reminder functions. For example, hypertensive patients rated the dose-memory function of the IDAS II as a contributing factor for their medication adherence. Specifically, 64% of patients commented that it was useful to know the number of doses they had previously taken and 46% reported that knowing how much time had elapsed since their last dose was valuable.Citation45
Combined devices that include visual feedback about the regularity of medication dosing have also been studied and have received mixed results in terms of their acceptability. In one study, the majority of patients with hypertension (75%) felt that a traffic light visual feedback system, indicated by a colored light, was helpful.Citation37 Furthermore, Jansen et alCitation42 found that just under one-third (32%) of patients in their study with rhinoconjunctivitis reported that the Memozax® with traffic light function motivated them to keep taking their medication. The majority of patients (79%) within this study also found the device easy to use and 46% of patients felt that it made remembering to take their medication “easier” or “much easier”.
In contrast, in a study by Santschi et alCitation45 who trialed the effect of both the IDAS II (with combined dose-memory and dose-reminder function) and a MEMS device on patient adherence to hypertension medication, half of their patients reported that a combined dose-memory and dose-reminder device helped them maintain a more regular dose intake. Similar findings were reported in a study by Christensen et alCitation37 in which 65% of patients with hypertension commented that the combined dose-memory and dose-reminder device positively influenced the regularity of their drug intake. Christensen et alCitation37 also found that clinicians were generally positive about the functions of a combined dose-memory and dose-reminder function, and overall, were more positive than patients were. For example, a significantly greater proportion of clinicians positively rated the dose-reminder function of the device (83%, P<0.001) and its feedback functions (78%, P<0.001), than patients (78% and 75%, respectively). In addition, a significantly greater proportion of clinicians felt that the device would influence the regularity of patients’ drug intake versus the patients themselves (64.9% of patients versus 70.4% of clinicians, P<0.001).
Impact on patients’ confidence with and self-management of their treatment and condition
As well as exploring the impact of these devices on treatment adherence and attitudes, some studies have also examined the potential benefits on other areas of health and well-being, particularly in terms of self-confidence. In one study, patients with diabetes reported feeling more confident that they would not miss their injections and would better manage their daily medication when using the NovoPen Echo® versus their previous device (unspecified by the authors), which did not have a dose-memory function.Citation34 In a different study where very similar findings were revealed, Klausmann et alCitation43 report that patients attribute this increased confidence to the NovoPen Echo’s® ability to provide dose-history information.
Finally, Guo et alCitation40 found that more patients with diabetes felt “very confident” managing their daily insulin injections using the NovoPen® 5 compared with their previous device because the visual confirmation of the dose and the audible end-of-dose sound provided reassurance that they had injected the full dose.
Discussion
The purpose of this review was to explore the impact of drug-delivery devices with dose-memory or combined dose-memory and dose-reminder functions on patients’ treatment adherence, confidence with, and self-management of their condition and treatment. Drug-delivery devices with dose-memory or combined dose-memory and dose-reminder functions, capable of recording and displaying dose-history information, and actively reminding patients to take their medication (eg, inhalers and auto-injectors) are available for patients being treated for a range of chronic conditions such as asthma, HIV, and diabetes.
This review provides evidence for the effectiveness and benefits of these device functions in improving patients’ medication adherence, their attitude towards the device, confidence in managing their condition, and ultimately, the value these products can have to patients, clinicians, and the wider health care system.
The number of published studies reporting adherence data was quite limited; however, devices with dose-memory and combined dose-memory and dose-reminder functions were found to improve objective and subjective adherence to daily medication when compared to either a control group or pre-study drug-delivery device without a dose-memory or dose-reminder function.Citation34–Citation36 From a methodological standpoint, these studies are reflective of adherence data collected over a 6-month period or less. However, patients who are initially adherent can become nonadherent over time and adherence rates are subject to dramatic decline and/or variability within the first 6 months of treatment.Citation3,Citation8,Citation47 Therefore, in order to assess the true long-term impact and value of these device functions, they need to be tested longitudinally.
In addition, a limitation of the reviewed studies is that they failed to consider how other features of the study devices may also impact adherence, beyond obtaining usability or preference data. For example, many of the reviewed devices, most notably insulin pens, had identical or comparable features such as mechanical platforms; however, some insulin pens offered slightly different functionalities such as the number of dosing increments that patients could select. Insulin pens such as the HumaPen® Memoir™ and HumaPen Luxura® offered single-unit dose increments, whereas the NovoPen Echo® offered half-unit dose increments. It is unclear from the reviewed literature what impact such additional and differentiating devices features have on adherence and this is something that should be explored further in future studies in this area.
This literature review has revealed that these devices have widespread value among those involved in the administration of medications in the management of chronic conditions. They have been shown to be beneficial for patients who self-administer their medication and parents/caregivers who administer medication for a patient. These devices have also been shown to be beneficial to patients susceptible to unintentional nonadherence (eg, forgetting), whether they are memory-intact patients who experience forgetfulness due to lifestyle factors or patients with clinical memory impairments. For example, Andrade et alCitation35 found that HIV patients who had memory impairments were significantly more adherent when using the DMAS device with combined functions than memory-intact patients.Citation35 These devices may also be of value to younger patients transitioning from assisted care to self-management, who may need additional reassurance and positive reinforcement about the time and volume of their last medication dose,Citation34 as well as the elderly and those with multiple chronic conditions requiring polypharmacy. This review suggests that devices with dose-memory and combined dose-memory and dose-reminder functions may be most useful in modifying the behavior of patients who are unintentionally nonadherent, and therefore, further targeted research within this population may be of value.
As well as improving adherence to treatment, devices with combined functions have been shown to significantly reduce the potentially dangerous practice of dose dumping, thus demonstrating the capability of such devices to enhance patients’ safety in the self-management of their treatment and reduce patients’ susceptibility to adverse events.Citation1,Citation36
Taken together, these devices may represent additional value for parents and caregivers by reducing the burden and expectation on these individuals to care for the patient. For example, following use of a device with a combined dose-memory and dose-reminder function, caregivers in one study reported reduced burden as the device promoted better self-management by the patient themselves.Citation35 This highlights a need for clinicians to consider the impact on caregivers when making decisions about the patients’ treatment options, especially caregivers at risk of experiencing high levels of burden.
Psychological benefits were also salient in the literature review, with dose-memory and combined dose-memory and dose-reminder functions seen as important and useful attributes of the product for both patients and clinicians. For example, patients felt that being able to review the time and volume of their last dose was valuable and usefulCitation37,Citation38,Citation45 in that it positively influenced the regularity of their medication intake.Citation37,Citation45 The devices were found to make patients feel more confident in managing their treatment and condition by assuring them that a dose had been taken correctly,Citation34,Citation40,Citation43,Citation44 thus providing peace of mind and security. The devices were also found to motivate patients to keep taking their medication.Citation42
Similarly, HCPs considered dose-memory function devices to be beneficial to their patients and of particular value to those patients who forget to take their medication.Citation37,Citation41,Citation46 Indeed, HCPs in some cases put greater emphasis on the importance of the dose-memory and dose-reminder functions on patient self-management than the patients themselves.Citation37 This highlights a need for increased and improved concomitant patient education in improving adherence and promoting the value and benefit of such devices on patients’ self-management behavior and well-being.
The literature review also revealed a potential for discordance between patients’ perceptions of their adherence/compliance and the clinicians’ understanding of adherence/compliance. The lack of robust and systematic adherence data reflects both measurement limitations (ie, how best to measure adherence, objectively and subjectively) and a lack of real world and longitudinal research in this area. Ultimately, understanding, monitoring, and evaluating patients’ adherent/nonadherent behavior in an ecological or epidemiological study is the best approach to determine the true impact of a device on patients’, caregivers’, and clinicians’ disease management.
Conclusion
This literature review has provided supportive evidence that dose-memory and combined dose-memory and dose-reminder function devices that enable the patient to record, monitor, and/or be actively reminded about their dose-history, can improve patients’ adherence to treatment and self-management of their condition. The evidence suggests that the incorporation of such functions into drug-delivery devices can work to target some non-intentional barriers to adherence such as forgetting, whether caused by lifestyle factors, such as having a busy routine, or clinical factors, such as dementia.
These devices therefore offer clinical and economic value by helping to improve disease control (eg, lowering high blood pressure), clinical outcomes (eg, reducing risk factors associated with a condition such as stroke in the case of hypertension), as well as patients’ health-related quality of life, and self-management skills. These devices also have the potential to reduce patients’ exposure to adverse events and reduce the number of avoidable clinician visits and hospital admissions caused by nonadherence.
It is apparent that whilst the incorporation of dose-memory functions in drug-delivery devices is presently limited, they may provide a valuable addition for patients who require long-term treatment regimens and who self-manage their condition. There does, however, remain considerable scope for further targeted quantitative and qualitative research in this area, particularly in terms of assessing the effect these devices can have on adherence from real world device use outside of the study environment, their effect on long-term adherence, and their impact on patients’ confidence with and self-management of their treatment and condition.
Disclosure
The authors report no conflicts of interest in this work.
References
- World Health Organization (WHO)Adherence to Long-Term Therapies: Evidence for ActionGeneva, SwitzerlandWorld Health Organization2003 Available from: http://www.who.int/chp/knowledge/publications/adherence_report/en/Accessed April 23, 2014
- FenertySDWestCDavisSAKaplanSGFeldmanSRThe effect of reminder systems on patients’ adherence to treatmentPatient Prefer Adherence2012612713522379363
- CramerJARoyABurrellAMedication compliance and persistence: terminology and definitionsValue Health2008111444718237359
- GouldEMittyEMedication adherence is a partnership, medication compliance is notGeriatri Nurs2010314290298
- American Society on Aging and American Society of Consultant Pharmacist FoundationAdult Meducation: Improving Medication Adherenced in Older Adults: Medication Adherence – Where We Are Today?2006 Available from: http://www.adultmeducation.com/downloads/Adult_Meducation.pdfAccessed January 7, 2013
- BrownMTBussellJKMedication adherence: WHO cares?Mayo Clin Proc201186430431421389250
- DiMatteoMRVariations in patients’ adherence to medical recommendations: a quantitative review of 50 years of researchMed Care200442320020915076819
- HaynesRBMcDonaldHGargAXMontaguePInterventions for helping patients to follow prescriptions for medicationsCochrane Database Syst Rev20022CD00001112076376
- WroeALIntentional and unintentional nonadherence: a study of decision makingJ Behav Med200225435537212136497
- Dunbar-JacobJMortimer-StephensMKTreatment adherence in chronic diseaseJ Clin Epidemiol200154 Suppl 1S57S6011750211
- ElliottRAShinogleJAPeelePBhosleMHughesDAUnderstanding medication compliance and persistence from an economics perspectiveValue Health200811460061018194403
- SokolMCMcGuiganKAVerbruggeRREpsteinRSImpact of medication adherence on hospitalization risk and healthcare costMed Care200543652153015908846
- National Pharmaceutical Council Noncompliance with medication regimensAn economic tragedy Emerging issues in pharmaceutical cost containingWashington, DCNational Pharmaceutical Council1992116
- PetersonAMTakiyaLFinleyRMeta-analysis of trials of interventions to improve medication adherenceAm J Health Syst Pharm200360765766512701547
- VermeireEHearnshawHVan RoyenPDenekensJPatient adherence to treatment: three decades of research. A comprehensive reviewJ Clin Pharm Ther200126533134211679023
- OsterbergLBlaschkeTAdherence to medicationN Engl J Med2005353548749716079372
- KruegerKPBergerBAFelkeryBMedication adherence and persistence: a comprehensive reviewAdv Ther200522431335616418141
- The Boston Consulting GroupThe Hidden Epidemic: Finding a Cure for Unfilled Prescriptions and Missed DosesBoston, MAThe Boston Consulting Group200318 Available at: http://www.bcg.com/documents/file14265.pdfAccessed April 23, 2014
- ClaxtonAJCramerJPierceCA systematic review of the associations between dose regimens and medication complianceClin Ther20012381296131011558866
- PeyrotMRubinRRLauritzenTSnoekFJMatthewsDRSkovlundSEPsychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN) StudyDiabet Med200522101379138516176200
- ZgiborJCSimmonsDBarriers to blood glucose monitoring in a multiethnic communityDiabetes Care200225101772177712351476
- BaylissEASteinerJFFernaldDHCraneLAMainDSDescriptions of barriers to self-care by persons with comorbid chronic diseasesAnn Family Med2003111521
- OnwudiweNCMullinsCDWinstonRABarriers to self-management of diabetes: a qualitative study among low-income minority diabeticsEthn Dis2011211273221462726
- FunnellMMAndersonRMMSJAMA: the problem with compliance in diabetesJAMA200028413170911015809
- McNabbWLAdherence in diabetes: can we define it and can we measure it?Diabetes Care19972022152189118777
- BarlowJWrightCSheasbyJTurnerAHainsworthJSelf-management approaches for people with chronic conditions: a reviewPatient Educ Couns200248217718712401421
- WalkerEAUsherJAUnderstanding and enhancing adherence in adults with diabetesCurr Diab Rep20033214114812728640
- CramerJAA systematic review of adherence with medications for diabetesDiabetes Care20042751218122415111553
- RandløvJPoulsenJUHow much do forgotten insulin injections matter to hemoglobin A1c in people with diabetes? A simulation studyJ Diabetes Sci Technol20082222923519885347
- KhawKTWarehamNBinghamSLubenRWelchADayNAssociation of hemoglobin A1c with cardiovascular disease and mortality in adults: the European prospective investigation into cancer in NorfolkAnn Intern Med2004141641342015381514
- HoPMMagidDJShetterlySMMedication nonadherence is associated with a broad range of adverse outcomes in patients with coronary artery diseaseAm Heart J2008155477277918371492
- FryAElectronically enabled drug-delivery devices: are they part of the future?Ther Deliv20123780580722900463
- VervloetMLinnAJvan WeertJCde BakkerDHBouvyMLvan DijkLThe effectiveness of interventions using electronic reminders to improve adherence to chronic medication: a systematic review of the literatureJ Am Med Inform Assoc201219569670422534082
- AdolfssonPVeijolaRHuotCHansenHDLademannJBPhillipMSafety and patient perception of an insulin pen with simple memory function for children and adolescents with type 1 diabetes – the REMIND studyCurr Med Res Opin20122891455146322640459
- AndradeASMcGruderHFWuAWA programmable prompting device improves adherence to highly active antiretroviral therapy in HIV-infected subjects with memory impairmentClin Infect Dis200541687588216107989
- CharlesTQuinnDWeatherallMAldingtonSBeasleyRHoltSAn audiovisual reminder function improves adherence with inhaled corticosteroid therapy in asthmaJ Allergy Clin Immunol2007119481181617320942
- ChristensenAChristrupLLFabriciusPESurvey of patient and physician assessment of a compliance reminder device in the treatment of hypertensionBlood Press200918528028519919400
- DahlgrenJVeimoDJohanssonLBechIPatient acceptance of a novel electronic auto-injector device to administer recombinant human growth hormone: results from an open-label, user survey of everyday useCurr Med Res Opin20072371649165517559757
- DanneTForstTDeinhardJRoseLMoennigEHauptANo effect of insulin pen with memory function on glycemic control in a patient cohort with poorly controlled type 1 diabetes: a randomized open-label studyJ Diabetes Sci Technol2012661392139723294785
- GuoXSommavillaBVanterpoolGQvistMBethienMLilleøreSKEvaluation of a new durable insulin pen with memory function among people with diabetes and healthcare professionalsExpert Opin Drug Deliv20129435535622432521
- IgnautDAVenekampWJHumaPen Memoir: a novel insulin-injecting pen with a dose-memory featureExpert Rev Med Devices20074679380218035945
- JansenAAndersenKFBrüningHEvaluation of a compliance device in a subgroup of adult patients receiving specific immunotherapy with grass allergen tablets (GRAZAX) in a randomized, open-label, controlled study: an a priori subgroup analysisClin Ther200931232132719302904
- KlausmannGHramiakIQvistMMikkelsenKHGuoXEvaluation of preference for a novel durable insulin pen with memory function among patients with diabetes and health care professionalsPatient Prefer Adherence2013728529223630416
- OlsenBSLilleøreSKKorsholmCNKrachtTNovopen Echo® for the delivery of insulin: a comparison of usability, functionality and preference among pediatric subjects, their parents, and health care professionalsJ Diabetes Sci Technol2010461468147521129343
- SantschiVWuerznerGSchneiderMPBugnonOBurnierMClinical evaluation of IDAS II, a new electronic device enabling drug adherence monitoringEur J Clin Pharmacol200763121179118417899047
- VenekampWJKerrLDowsettSAFunctionality and acceptability of a new electronic insulin injection pen with a memory featureCurr Med Res Opin200622231532516466603
- VrijensBVinczeGKristantoPUrquhartJBurnierMAdherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing historiesBMJ200833676531114111718480115