Abstract
Background
This study was designed to investigate the preferences for treatment of lobectomy in Chinese lung cancer patients and differences in the psychological and social factors that influence treatment decision-making.
Methods
One hundred and forty patients with stage I lung cancer were recruited from Hebei Cangzhou Central Hospital. Before surgery, the patients completed a questionnaire that surveyed their preferences for treatment and the relevant influencing factors. Differences in psychological and social characteristics were compared between lung cancer patients who chose video-assisted thoracoscopic surgery (VATS) and those who opted for open thoracotomy.
Results
Among the 135 valid questionnaires, 79 patients preferred VATS and 56 patients chose open thoracotomy. Potential side effects, doctors’ recommendation, the prognosticated chance for cure, cosmesis, and financial burden influenced the patients’ decisions.
Conclusion
The minimally invasive advantages of VATS, including lesser trauma to the chest wall, earlier remission of postoperative pain, faster recovery, less bleeding, and improved cardiopulmonary function made VATS more attractive to patients needing lobectomy for lung cancer. However, the choice of VATS over open thoracotomy is still influenced by the degree of prognosticated cure and the feasibility of surgery.
Introduction
Lung cancer has been the leading cause of cancer death since the mid 20th century, with increasing morbidity and mortality around the world.Citation1 Since the 1930s, surgery has been the preferred treatment for lung cancer, in the form of conventional open thoracotomy. With the advent of minimally invasive surgery, video-assisted thoracoscopic surgery (VATS) has been widely adopted as an alternative surgical approach for thoracic disease.Citation2 VATS is a newly developed minimally invasive thoracic procedure that allows complicated operations to be done through a minimal incision and assisted by a video camera. In the past 2 decades, evidence has shown that, compared with open thoracotomy, VATS has several advantages, including earlier remission of postoperative pain, less release of inflammatory factors, less negative effect on pulmonary function, fewer complications, and faster recovery, without compromising the long-term survival and disease-free survival.Citation3–Citation6 However, differences still exist with regard to preference for and acceptance of these two surgical approaches among patients. Plenty of studies have focused on the efficacy of the two surgical treatments but few studies have investigated the preferences for treatment decision-making and the factors that influence the patient’s treatment decision. This study focuses on the preferences for treatment of lobectomy in Chinese lung cancer patients according to differences in performance status, psychological factors, and social factors.
Materials and methods
Participants
One hundred and forty lung cancer patients awaiting lobectomy at Hebei Cangzhou Central Hospital from February 2012 to April 2013 were enrolled. The patients were assessed to be suitable for VATS by preoperative tests. Patients had to be diagnosed with stage I lung cancer and be able to consent to surgical treatment. Patients who were in hospital for less than 5 days, who received neoadjuvant chemotherapy, and who had pleural effusion were excluded. Before the survey, all patients were informed about VATS and open thoracotomy procedures, and were asked to sign an informed consent form for surgery. A total of 140 questionnaires were distributed, with five excluded due to more than three missing values. The statistical analysis included the 135 patients who completed the questionnaires fully.
All patients were explicitly informed of their diagnosis, the possibility of stage I lung cancer seen on computed tomography, emission computed tomography, or magnetic resonance imaging, the need for surgery, and the advantages and disadvantages of VATS and open thoracotomy. Sufficient time was allowed for patients to consider these two different surgical approaches, and the preferred surgical approach was put down on the informed consent form for surgery. The patients were divided into a VATS group and an open thoracotomy group based on their preferred surgical approach. Patient demographics, psychological factors, and social factors contributing to the patients’ decisions were analyzed.
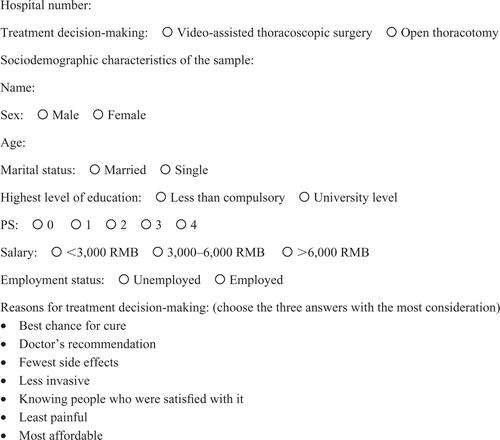
Demographic characteristics included age, sex, marital status, education level, performance status score, family income, and employment status. Based on an earlier study that examined treatment decisions in cancer patientsCitation7 and our own clinical experience, seven factors relevant to treatment decision-making were assessed: the best chance for cure, doctor’s recommendation of the best treatment, side effects, invasiveness, knowing people who were satisfied after having undergone open thoracotomy or VATS, pain, and affordability. All patients self-administered the questionnaire, and the top three factors were chosen and analyzed ().
Statistical analysis
All data were analyzed using Stata version 10.0 software. Chi-square and Wilcoxon rank sum tests were conducted to analyze the difference in treatment decision-making according to demographic characteristics. P<0.05 was considered to be statistically significant with a two-sided test.
Results
Sixty-six (48.9%) of the 135 patients were male and 69 (51.1%) were female, with an average age of 56±12.9 years. One hundred and twenty-seven (94.1%) were married, 98 (72.6%) were employed, and a high number (58.5%) had completed college or higher education. Family income was <3,000 RMB per month, 3,000–6,000 RMB per month, and >6,000 RMB per month for 49 (36.3%), 41 (30.4%), and 45 (33.3%) of patients, respectively.
Comparison of demographics and characteristics between two groups
The 135 valid questionnaires indicated that 79 patients preferred VATS and 56 patients chose open thoracotomy as their treatment. There was a statistically significant effect of sex and age on treatment decision-making (P<0.05). Fewer males (n=30, 38%) than females (n=49, 62%) chose VAT, and both younger patients (aged <35 years) and older patients (.65 years) preferred VATS, while middle-aged patients (aged 35–65 years) preferred open thoracotomy. Family income played a large role in the decision regarding treatment, given that patients in the People’s Republic of China have to pay for their surgery, and are then reimbursed a portion of the medical expenses by an insurance company. Most patients (n=33, 59%) with a low family income (<3,000 RMB per month) chose open thoracotomy, while those with a high family income were more likely to choose VATS ().
Table 1 Comparison of demographic and clinical characteristics between two groups
Factors affecting treatment decision-making
Of the factors deemed to influence patient decisions, having the fewest side effects (n=80, 59%) was rated as the most important reason for choosing treatment, followed by doctor’s recommendation (n=77, 57%) and best chance for the treatment being curative (n=67, 50%). Each treatment preference group had different reasons/factors influencing their decision. Best chance of cure (n=49, 88%) and affordability (n=41, 73%) were the two most important factors influencing the patient’s decision in the open thoracotomy group, while fewest side effects (n=60, 76%), doctor’s recommendation (n=54, 68%), and less invasiveness were regarded as important in the VATS group (n=47, 59%; ). Interestingly, predicted patient satisfaction and pain were the two factors that were rated similarly between the two groups.
Table 2 Factors influencing treatment decision-making
Discussion
A number of studies have analyzed differences in the application and clinical efficacy of VATS and open thoracotomy for lobectomy.Citation8–Citation10 However, few studies have looked at factors that influence the patient’s decision to choose one or the other procedure.
With the development of minimally invasive surgery, more attention has been paid to the clinical application of VATS. VATS emerged as a new technique for thoracic surgery in the 1990s, and since then has been shown to be useful in lobectomy for lung cancer.Citation5,Citation6,Citation8–Citation10 Previous studies have shown significant advantages of VATS over open thoracotomy, including less trauma to the chest wall, faster remission of postoperative pain and recovery, less bleeding, less compromise of cardiopulmonary function, and fewer postoperative complications. As far as we know, patients are less familiar with VATS, and depending on age, sex, and cultural background, they have different attitudes toward VATS versus open thoracotomy.
VATS has been shown to have an important role in the treatment of lung cancer,Citation11,Citation12 and has the potential to become the main type of surgery performed for lung cancer in the future. Patients’ preference for each type of surgery is impacted by various factors. In this study, we discovered a significant difference in age, sex, and income between patients who choose VATS versus open thoracotomy. Middle-aged patients (n=45) were more inclined toward open thoracotomy (P<0.05), while younger patients (n=44) and older patients (n=25) were more likely to opt for VATS. Ninety percent of young patients, 18% of middle-aged patients, and 81% of older patients preferred VATS. These findings might be explained by the fact that middle-aged patients tend to hold traditional views. Further, young patients may attach much importance to decreased invasiveness resulting in improved cosmesis while older patients may value decreased invasiveness resulting in improved recovery, given that older patients are poorer surgical candidates to start with. Further, it was found that female patients (n=49, 62%) chose VATS while male patients (n=30, 38%) preferred open thoracotomy (P<0.05). It is possible that female patients choose VATS because of improved cosmesis. Finally, the financial burden of VATS influences the patient’s decision; patients who chose VATS had a higher family income than those who chose open thoracotomy, with a family income of less than 3,000 RMB per month in a majority of the open thoracotomy group (n=33, 59%).
In this study, several factors were demonstrated to influence a patient’s treatment choice, including side effects (59%), doctor’s recommendation (57%), prognosticated chance for cure (50%), less invasiveness (39%), and financial burden (38%). The choice of open thoracotomy was significantly influenced by the potential for cure and a decreased risk of recurrence of cancer, given that the open approach allows for complete lymph node dissection and tumor resection. Another significant reason why lower income patients choose open thoracotomy was its improved affordability over VATS. In the VATS group, fewer side effects, doctor’s recommendation, and less invasiveness influenced patient choice.
Previous studies have shown that VATS is at least as safe as open thoracotomy.Citation13,Citation14 However, in our study, we found that some patients were concerned about the safety of VATS. In order to shift this misconception, further research is needed to confirm that VATS is a safe surgical approach, and this information needs to be disseminated to educate patients. Finally, because of its superior cosmesis, VATS is preferred by young patients and females. Given that VATS meets patients’ requirements regarding cosmesis and safety, it has the potential to become the main surgical approach in the future.Citation15
The limitations of this study are as follows. In the early phase of the study, during which the patients were learning about VATS versus thoracotomy, different patients received information from different doctors who may have had a bias toward one or the other procedure, which in turn would influence patients’ decision-making. Another limitation is the fact that the subjects were all recruited from the Hebei Cangzhou Central Hospital, and the regional culture could have affected personal preferences, psychology, and intellectual capacity.
Supplementary material
Disclosure
The authors report no conflicts of interest in this work.
References
- LiuJSongZQA review on lung cancerJournal of Guangdong Medical College20115536539
- HaiQMinimally invasive treatment of lung cancerChin Oncol20053213216
- LianYEffect comparison of thoracoscopic lung resection surgery with conventional thoracotomyChinese Journal of Medical Guide2014165657
- HuXCComparative study on complete video-assisted thoracic surgery and the racotomy lobectomy in the treatment of non-small cell lung cancerChina Modern Medicine2013206768
- McKennaRJJrHouckWFullerCBVideo-assisted thoracic surgery lobectomy: experience with 1,100 casesAnn Thorac Surg20068142142516427825
- ZhuRWengGXComparison of surgical trauma between video-assisted thoracoscopic surgery and conventional thoracotomyChin J Clin Thorac Cardiovasc Surg20095357361
- PalmerNRToozeJATurnerARXuJAvisNEAfrican American prostate cancer survivors’ treatment decision-making and quality of lifePatient Educ Couns201390616822940374
- ChangJHYouQJWengYCaiMChangQMini-incision video-assisted thoracoscopic versus conventional surgery for lung cancerChin J Min Inv Surg20077412414
- JiangGYangFLiXVideo-assisted thoracoscopic surgery is more favorable than thoracotomy for administration of adjuvant chemotherapy after lobectomy for non-small cell lung cancerWorld J Surg Oncol2011917022185633
- CaoCManganasCAngSCYanTDA meta-analysis of unmatched and matched patients comparing video-assisted thoracoscopic lobectomy and conventional open lobectomyAnn Cardiothorac Surg20121162323977459
- XuLZhangZVideo-assisted thoracoscopic surgery for lung cancerChin J Surg Oncol20135137140
- LiuLXOpen chest operation will gradually “upgrade” to a supplement to the minimally invasive thoracoscopic operationChin J Clin Thorac Cardiovasc Surg201219109112
- HeYCoonarAGelvez-ZapataSSastryPPageAEvaluation of a robot-assisted video-assisted thoracoscopic surgery programmeExp Ther Med2014787387624669243
- LindenDLindenKOparkaJIn patients with resectable non-small-cell lung cancer, is video-assisted thoracoscopic segmentectomy a suitable alternative to thoracotomy and segmentectomy in terms of morbidity and equivalence of resectionInteract Cardiovasc Thorac Surg20141910711024722517
- ZhaoXGPengCJCongBThe application of thoracoscopic lobectomy in treating lung cancerMedicine and Philosophy (Clinical Decision Making Forum Edition)201191415