Abstract
Blood pressure (BP) telemonitoring systems and pharmacist management programs were introduced into Haruka Community Pharmacy. A 22-year-old healthy male came to the community pharmacy, although he was not in a diseased state, he had been informed previously that he had a moderately high BP during a routine examination. He continued home BP telemonitoring for 28 days. A pharmacist intervention was conducted at 2 week intervals. His average nighttime systolic BP was higher than the daytime systolic BP. The pharmacist consulted a doctor based on the BP telemonitoring results, and ambulatory blood pressure monitoring (ABPM) was initiated. The doctor detected nocturnal hypertension based on the results of ABPM monitoring. BP telemonitoring systems have been introduced into a small percentage of pharmacies in Japan, and this is the first case report for the usefulness of these systems in a community pharmacy.
Introduction
“Out-of-office” blood pressure (BP) monitoring is important in the diagnosis and management of hypertension.Citation1 Out-of-office BP is commonly assessed by ambulatory BP monitoring (ABPM), or home BP monitoring (HBPM) which involves self-measurement. Previous reports suggest that HBPM is readily accepted and conducted by hypertensive patients.Citation2–Citation4 An increasing number of hypertensive patients are using the technique to check HBPM regularly, whereas young healthy subjects seldom check their BP. The rate of HBPM is very low in young healthy people, thus many cases of hypertension have been ignored.
New communication technologies have been introduced in order to facilitate routine BP measurements. In particular, home BP telemonitoring systems can lead to better BP control compared to the traditionally used methods.Citation5–Citation7 Margolis et al suggested that home BP telemonitoring systems and pharmacist case management can result in better BP control compared to usual care.Citation8 However, only a few pharmacies currently use BP telemonitoring systems in Japan.
Pharmacist management programs using BP telemonitoring systems were recently introduced into our community pharmacy (Haruka Community Pharmacy, Nagoya, Japan). This system is based on physician–pharmacist comanagement, and we present a case of a young healthy male who was diagnosed with nocturnal hypertension.
Case presentation
A 22-year-old healthy male came to Haruka Community Pharmacy. Although he was not in a diseased state, he was found to have a moderately high BP during a medical examination at his university. He was not a shift worker, and had normal sleeping patterns. The community pharmacist recommended that he check his HBPM regularly, and hence, he began HBPM. The home BP telemonitoring system involved the use of Medical LINK (Omron Healthcare Co., Ltd., Muko, Kyoto, Japan). This system wirelessly transmits BP data to a central web server via a mobile network. The community pharmacist can examine the patient’s BP data at any time via the Internet.
The pharmacist advised the patient to measure his BP twice per day (when he wakes up and before he goes to bed), and gave him a printed handout outlining the importance of lifestyle modification before starting BP monitoring. A pharmacist intervention was conducted every two weeks during the monitoring period. Briefly, the pharmacist collected information regarding his lifestyle from an interview, and advised him about lifestyle modification. Home BP telemonitoring was continued for a period of 28 days.
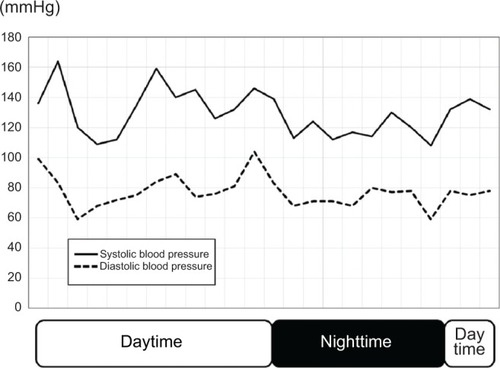
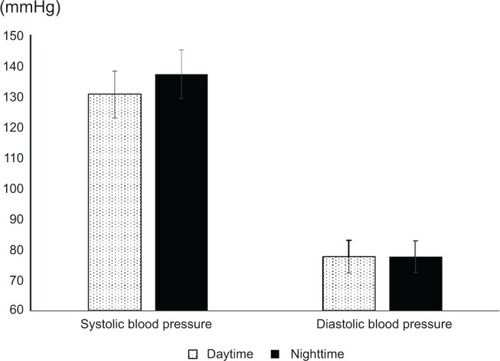
The average values of the patient’s systolic and diastolic BPs are shown in . Although the frequency of measuring his BP at home was 85.7% before the monitoring period (data not shown), it was increased to 96.4% afterward (). The mean values for daytime and nighttime systolic blood pressures were 131 mmHg and 137 mmHg, respectively, and diastolic blood pressure was 78 mmHg. Therefore, the patient did not have daytime hypertension, as shown by the telemonitoring measurements. The average nighttime systolic BP was higher than that of the daytime BP (). The pharmacist consulted a physician based on the results of BP telemonitoring, and ABPM was conducted. BP was measured for a 24-hour period using an FB-270 device (Fukuda Denshi Co., Ltd., Tokyo, Japan). The BP values during ABPM are shown in . “Nighttime” was defined as the patient’s actual sleeping time, based on his diary. The mean daytime and nighttime BP were 135/80 mmHg and 120/73 mmHg, respectively. We defined hypertension as a BP of 135/85 mmHg or higher for daytime BP and 120/70 mmHg or higher for nighttime BP based on the Japanese Hypertension guidelines.Citation9 Thus it was concluded that the patient had nocturnal hypertension.
Figure 1 Average of systolic and diastolic blood pressure values.
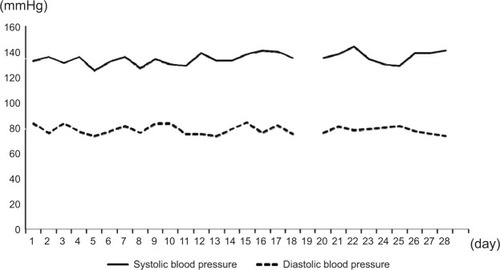
Figure 2 Comparison of average daytime and nighttime blood pressure during the monitoring periods.
Discussion
In the present case report, the pharmacist advised a young healthy male to be on HBPM, and he successfully performed the monitoring at regular intervals. Moreover, the pharmacist consulted with a physician based on the results of BP telemonitoring, and the patient was diagnosed with nocturnal hypertension.
Some young healthy males have elevated brachial systolic BP (≥135 mmHg) and normal values of brachial diastolic BP (≥85 mmHg) but there is no evidence to show that they benefit from antihypertensive treatment.Citation1 Previous reports suggested that the physician–pharmacist comanagement of hypertension can be useful for controlling BP.Citation10,Citation11 In the present case, pharmacist management programs using a BP telemonitoring system improved patient adherence in terms of measuring his BP. BP telemonitoring systems have been introduced into a small percentage of pharmacies in Japan, and this is the first successful case report of the use of such a system in a community pharmacy. Although further studies in patients with hypertension will be needed, these programs in which telemonitoring systems are used might be useful for collaborative drug therapy management in community pharmacies.
Disclosure
The authors declare no conflicts of interest in this work.
References
- ManciaGFagardRNarkiewiczK2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)Eur Heart J201334282159221923771844
- ParatiGStergiouGSAsmarREuropean Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure MonitoringJ Hypertens20082681505152618622223
- PickeringTGMillerNHOgedegbeGKrakoffLRArtinianNTGoffDCall to action on use and reimbursement for home blood pressure monitoring: a joint scientific statement from the American Heart Association, American Society Of Hypertension, and Preventive Cardiovascular Nurses AssociationHypertension2008521102918497370
- ParatiGStergiouGSAsmarREuropean Society of Hypertension practice guidelines for home blood pressure monitoringJ Hum Hypertens2010241277978520520631
- McManusRJMantJBrayEPTelemonitoring and self-management in the control of hypertension (TASMINH2): a randomised controlled trial. Lancet1720103769736163172
- MorakJKumpuschHHaynDModre-OsprianRSchreierGDesign and evaluation of a telemonitoring concept based on NFC-enabled mobile phones and sensor devicesIEEE Trans Inf Technol Biomed2012161172322113811
- ParatiGOmboniSAlbiniFHome blood pressure telemonitoring improves hypertension control in general practice. The TeleBPCare studyJ Hypertens200927119820319145785
- MargolisKLAscheSEBergdallAREffect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trialJAMA20133101465623821088
- OgiharaTKikuchiKMatsuokaHThe Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009)Hypertens Res2009321310719300436
- WeberCAErnstMESezateGSZhengSCarterBLPharmacist- physician comanagement of hypertension and reduction in 24-hour ambulatory blood pressuresArch Intern Med2010170181634163920937921
- ChenZErnstMEArderyGXuYCarterBLPhysician-pharmacist co-management and 24-hour blood pressure controlJ Clin Hypertens (Greenwich)201315533734323614849