Abstract
Introduction
The objective was to assess the effects of different orthodontic treatment needs on the oral health-related quality of life (OHRQoL) of Saudi children seeking orthodontic treatment as perceived by the children and their parents.
Methods
A cross-sectional evaluation of orthodontic patients and their attending parents was conducted to assess the relationship between orthodontic treatment needs and the OHRQoL. The study sample comprised 120 young orthodontic patients (36 boys, 84 girls; age range, 12–15 years). Each participant was assessed for orthodontic treatment needs and OHRQoL using the Dental Health Component of the Index of Orthodontic Treatment Needs and the Michigan Oral Health-related Quality of Life Scales–Version C (child) and Version PG (parent/guardian), respectively.
Results
Orthodontic treatment needs significantly affected mouth aching, chewing and biting, going to school, and playing. Higher income and borderline index of orthodontic treatment needs are significantly related to oral health impact on quality of life perceived by the child, while younger age and high school education are related to oral health impact on quality of life as perceived by the parent/guardians.
Conclusion
These findings emphasize the impact of malocclusion on OHRQoL in children.
Keywords:
Introduction
Malocclusion is a highly prevalent dental deformity, which was shown to have several consequences: physical, economic, social, and psychological impacts.Citation1 Malocclusion was also blamed as an etiological factor behind sleep-related breathing disordersCitation2 and was found to be interrelated with developmental dyslexia.Citation3 Malocclusion can influence the quality of life (QoL) in many people and affect various aspects of life, including function, appearance, and interpersonal relationships.Citation2 Recently, subjective patient-based measures such as perceived functional status and psychological well-being have become as important as clinician-based outcome measures in dental research. This is due to the fact that clinical measures alone are insufficient to assess oral health and oral health needs.Citation3 Currently, researchers have focused on the measurement of oral health impacts on QoL including perceived needs, particularly in relation to patients’ perceptions of their oral status.Citation4–Citation37
According to the concept of oral health-related quality of life (OHRQoL), good oral health is no longer seen as the absence of oral diseases and dysfunction. However, it indicates the absence of negative impacts of oral conditions on social life and self-confidence.Citation4
OHRQoL measurement is highly recommended for orthodontists to supplement clinical findings, because OHRQoL outcome does not always correlate with such objective findings.Citation5 In addition, it provides more understanding of the demand for orthodontic treatment beyond clinicians’ parameters.Citation6 Actually, OHRQoL can be considered as a valid parameter in the assessment of orthodontic patients in the area of oral health and malocclusion, because social and psychological effects are the key motives for seeking orthodontic treatment.Citation7
OHRQoL as related to malocclusion was assessed in many previous studies in both adults and children, in different populations.Citation8–Citation17 Results were controversial; some found that malocclusion has physical and psychological consequences, and others denied such correlation. This could be attributed to different interpretations of what these impacts constitute, sample size and age, and the lack of standardized approaches for assessment.Citation16
Several orthodontic indexes were used to evaluate malocclusion. The index of orthodontic treatment needs (IOTN), which includes the two independent components, the dental health component (DHC) and the esthetic component,Citation17 has been used extensively in the literature to evaluate actual and perceived orthodontic treatment needs.Citation4,Citation6,Citation7,Citation36,Citation38 The DHC grades patients’ treatment needs as either no treatment need, little treatment need, borderline need, or treatment required.Citation17
Several instruments were developed to assess OHRQoL, of which five were developed to be used in children. These are the Child Perception Questionnaire (CPQ 11–14),Citation32 Michigan Oral Health-related Quality of Life Scale,Citation6 Child Oral Health Impact Profile,Citation33 Early Childhood Oral Health Impact Scale,Citation34 and the Child Oral Impact on Daily Performance.Citation35 The Michigan OHRQoL Scales–Version C (child) and Version PG (parent/guardian) have the advantage of incorporating both parents’ and children’s perception of the children’s OHRQoL by including both functional and psychological aspects.Citation6 In fact, OHRQoL measures cannot replace normative needs in children. Instead, using both parents’ and children’s perceptions might give more valuable feedback to cover different dimensions.
Up-to-date, OHRQoL measures were never assessed using both parents’ and children’s perceptions, especially among Saudi children. The objective of this study was to assess the effects of different orthodontic treatment needs on the OHRQoL of a sample of Saudi children seeking orthodontic treatment, as perceived by the children and their parents.
Materials and methods
Ethical approval was obtained for this study from the Research Ethics Committee of the Faculty of Dentistry at King Abdulaziz University, Jeddah, Saudi Arabia. A cross-sectional evaluation of orthodontic patients and their attending parents was conducted to assess the relationship between orthodontic treatment needs, as assessed by the DHC of the IOTN, and the OHRQoL, as assessed by the Michigan OHRQoL Scales–Version C and Version PG. A sample of 120 young patients (36 males and 84 females) ranging in age between 12 years and 15 years, who were seeking orthodontic treatment at the Faculty of Dentistry, King Abdulaziz University, was collected according to the order of registration on the waiting list and was included in the present study. Only those who were willing to participate in the study, were in the permanent stage of eruption, had a perceived need for orthodontic treatment, and were about to undergo orthodontic therapy were included. Participants were informed about the nature of the study and the examination procedures, and were assured of the confidentiality of the collected information. Exclusion criteria were chronic medical conditions, previous orthodontic treatment, craniofacial anomalies such as cleft lip and palate, and poor periodontal health status as indicated by a community periodontal index score of 3 or more.Citation19 This was to prevent possible confounding effects of those conditions on the participants’ QoL. Patients attending without their parents or who refused giving consent were also excluded. The data collected included socio-demographic data (parents/guardians’ education and income), orthodontic treatment needs, and OHRQoL. Each child enrolled in the study had a dental clinical examination, self-completion questionnaire, and an interview. Parents of children enrolled in the study also had a self-completion questionnaire and an interview.
Assessment of orthodontic treatment needs
Patients were examined for orthodontic treatment needs using the DHC of the IOTN. Two examiners were calibrated to use it (kappa =0.85). They were orthodontists and were trained and underwent a calibration exercise. The calibration exercise took place at the Department of Orthodontics at King Abdulaziz University by an expert in using the IOTN. Treatment needs of the patients were categorized as 1) little or no treatment need, 2) borderline need, and 3) treatment required. The DHC uses a simple ruler and an acronym – MOCDO (missing teeth, overjet, crossbite, displacements of contact points, overbite) to identify the most severe occlusal trait of each patient. The final overall score for IOTN category was given to the patient according to the most severe trait.Citation17
Assessment of OHRQoL
The data collection instrument for the assessment of OHRQoL was the Michigan OHRQoL Scales–Version C () and Version PG ().Citation6 The scales were translated into Arabic versions by experts in both Arabic and English languages and then back-translated into English to confirm the consistency of Arabic and English versions, and were carefully revised to ensure proper translation. Validity of the scale was assessed by correlation of the scales with IOTN and also by correlation between parent and child forms. Reliability was assessed by internal consistency. The questionnaires were administered by the examiners before the clinical examination. Each patient and her/his attending parent were asked to fill out the questionnaire separately to exclude any possible influence on the children by their parents. Responses were made on a 0–1 scale for children and a 5-point Likert-type scale (never, hardly ever, occasionally, fairly often, and very often) for parent/guardians, which were then transformed into a score 1–3. A threshold of occasionally, fairly often, and very often was used to dichotomize responses, thereby indicating participants who had experienced at least some oral health impact.
Table 1 IOTN and COHRQoL among study children
Table 2 IOTN and PGOHRQoL among study children
The daily activities included the following: teeth sensitivity to cold/hot, sensitivity to sweet, toothache preventing sleeping, difficulty in chewing, difficulty biting hard objects, pain preventing playing or going to school, satisfaction with the teeth shape, complaining about his/her teeth, being teased by others.
Statistical analysis
Data were analyzed using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA). Post hoc power analysis was performed using G*Power 3.1.5. A logistic regression of oral health impact on any categorical predictor (as IOTN categories) assuming 50% with oral health impact among those who need treatment with a sample size of at least 120 achieves 0.709 power at a 0.05 significance level to detect an odds ratio of 2, assuming multi-collinearity among independent variables of 10%. The median, interquartile range, and proportion were used as summary statistics. Cronbach’s alpha coefficient was used to test reliability of the scales used. Overall OHRQoL scale was calculated by summation of items after reversing the score of negative items. Spearman’s rank correlation was used to test the consistency of OHRQoL reported by child and parent/guardians. The intra-class correlation (ICC) was calculated for the total children’s OHRQoL and parent/guardian’s OHRQoL scores. It was also determined by each independent variable. Accordingly, agreement of the two scales was classified as poor (ICC <0.2), fair (ICC 0.21–0.40), moderate (ICC 0.41–0.60), substantial (ICC 0.61–0.80), or excellent to perfect (ICC 0.81–1.0). Chi-square test was used for testing differences in OHRQoL score by IOTN and in case of small cell frequency, Monte Carlo exact test was displayed. Crude and adjusted odds ratios (by multiple logistic regression) with their 95% confidence interval (CI) were used to compare the odds of oral health impact among different study groups. All tests were two-sided, and the 0.05 level was used to indicate statistical significance.
Results
This study included 120 child–parent/guardian pairs with a median age of children being 13 years (interquartile range: 12–15 years); males constituted 30%, 25.8% with less than high school education and 19.2% with low family income. Considering IOTN, 21.7% did not need treatment, 25.8% needed borderline treatment, and 52.5% definitely needed treatment. No significant relationship () could be detected between orthodontic treatment needs and studied socio-demographic variables, though children who needed treatment constituted a higher percentage of the older age group (61.2%) than the younger age group (41.5%). ICC was fair-to-moderate for the total sample and for all study groups.
Table 3 IOTN by socio-demographic characteristics of the study children
Oral health impacts as reported by children showed a statistically significant relationship to IOTN in four items: “Is it hard for you to chew or bite?”, “Do you like your teeth?”, “Are you happy with your teeth and smile?”, and “Do kids make fun of your teeth?”. The median total oral health impact on the children scale was higher but insignificant among those who needed orthodontic treatment (median =3, interquartile range [2–5]) than those who did not need treatment (median =2, interquartile range [1–5]). The median parent/guardian’s OHRQoL scale showing the same pattern as those who needed treatment had a median of 18 (interquartile range: 14–20) while those who did not need treatment had a median of 16.5 (interquartile range: 14.75–19) (Mann–Whitney test =0.60, P=0.548).
The relationship between IOTN and items of QoL as perceived by parents/guardians () was significant with four items: “My child had difficulty biting hard”, “My child had difficulty chewing”, “My child’s teeth are sensitive to hot or cold”, and “My child’s teeth keep him/her from learning at school”. Children with impact on those items represented a higher percentage of those who were borderline or needed orthodontic treatment.
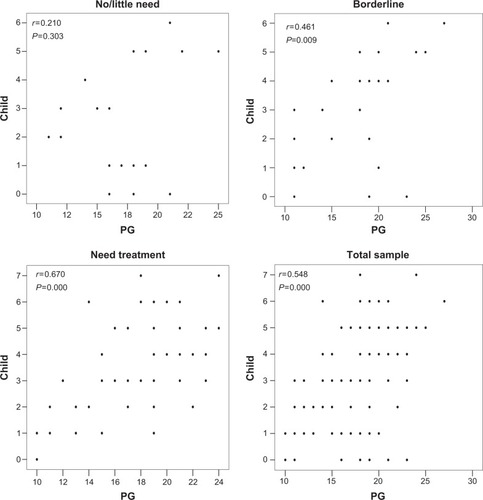
Cronbach’s alpha indicated reasonable reliability of the scale for children’s OHRQoL (0.640) and acceptable reliability for the parent/guardian’s OHRQoL (0.739). indicated significant positive correlation between the child version and the PG version of OHRQoL (r=0.548, P=0.000), which increased in strength with the degree of orthodontic treatment need varying from weak insignificant (r=0.210, P=0.303) for those with no/little need to moderate significant with borderline (r=0.461, P=0.009) or definite IOTN (r=0.670, P=0.000).
Figure 1 Correlation of oral health impact reported by children and parent/guardians according to the index of orthodontic treatment need.
shows the results of simple and multivariate logistic regression analysis of OHRQoL as reported by children and parent/guardians, controlling for socio-demographic characteristics of children. Crude odds ratios indicated significantly higher odds of oral health impact reported by children among those with IOTN compared to those without need (odds ratio [OR] =3.6, 95% CI: 1.0–12.6). On the other hand, with multivariate logistic regression, both income and IOTN were statistically significant with higher odds of oral health impact among children with IOTN compared to those without need (OR =4.6, 95% CI: 1.4–15.0) and of high-income families compared to low-income families (OR =3.7, 95% CI: 1.0–13.0). Crude odds ratios of oral health impact reported by parent/guardian indicated significant higher odds of oral health impact among younger children compared to older children (OR =3.6, 95% CI: 1.7–7.6), boys rather than girls (OR =2.3, 95% CI: 1.0–5.0) and children with parent/guardian of high school level compared to university level (OR =3.4, 95% CI: 1.3–9.4). Adjusted odds ratios revealed significant effect of only age of child and educational level of parent/guardian.
Table 4 Multiple logistic regression analysis of factors associated with oral health impact as reported by children and PG
Discussion
The measurement of OHRQoL is an important component of oral health studies, which helps to design oral health preventive and treatment programs.Citation5 Currently, more emphasis is placed on patient-based evaluations of health–related QoL, especially in esthetic and elective treatments.Citation18,Citation20 Although it is generally accepted that malocclusion has physical and psychological consequences, there are still conflicting data about the extent of these effects, especially in children due to the major life changes occurring during this period, which affect the children’s judgment of which daily activities are influenced by the need for orthodontic treatment.Citation5,Citation18 Therefore, the present study was done to assess the impact of orthodontic treatment needs on OHRQoL in young orthodontic patients, using both the children and their parents’ perceptions of how malocclusion affected their OHRQoL. This is the first study to use the Michigan OHRQoL Scales–Version C and Version PG to assess the association between OHRQoL and IOTNs.
The study indicates that orthodontic treatment need does not differ by age, sex, parent/guardian education, or family income. Being our study sample of the same socioeconomic level (most of parent/guardians are high school or university educated and the majority with medium to high income) may explain absence of the effect of social variables. The same was true for demographic data as the age range in the present study is narrow and the majority of children were females (70%).
Reliability of the used scale is medium for the child version (0.64), whereas for the PG version, it is optimum (0.74). This may be partly attributed to the more detailed scoring (1–5 for adult version and 0–1 for the child version) used.
The percentage of children who needed orthodontic treatment constituted more than 50% of our sample. A percentage which is higher than that reported by de Oliveira and SheihamCitation7 as 38.5% of the adolescents were clinically assessed as needing orthodontic treatment.
Our study indicates that malocclusion has an impact on OHRQoL in certain aspects. This is in agreement with Ukra et alCitation10 and others.Citation5,Citation16,Citation29,Citation30 It disagrees with Taylor et alCitation17 and Carvalho et al and others.Citation11,Citation13,Citation15 This could be due to the different sample size, age, racial background, and whether they used orthodontic patients or general population type of sample. In the present study, children’s OHRQoL was significant in relation to IOTN for an item related to difficulty in chewing or biting and two items related to psychological impact: (unhappiness with their smile and teeth; and other children making fun the child’s teeth). PG version indicates significant relation with IOTN on hurting with hot or cold food items, difficulty in chewing and biting, and one social item (“My child teeth keep him from learning at school”). This may be understood and expected from Arab mothers who are always concerned about children’s functions and school activities. Although in a British study it was found that mothers overreported the impact of oral health with regard to emotional items, a systematic review indicated that agreement between parents and child’s oral health impact on QoL appears to be dependent on the tested domain, with good agreement on domains reflecting physical effect, function, and symptoms, and poor agreement on domains reflecting social and psychological items.Citation21 Bellot-Arcís et alCitation32 and elaborated more on the relationship of the different occlusal conditions of the DHC with the psychosocial impact, and they found that increased overjet, tooth displacement, and increased overbite were the occlusal conditions that had a higher psychosocial impact. In the present study, such correlation was not made; however, we found that the most reported occlusal traits among those who needed orthodontic treatment were tooth displacement (75%), increased overjet (59%), and deep bite (34%), respectively, which agree with the findings of Bellot-Arcís et al.Citation32
Children usually report a higher impact of oral health on QoL than their parent/guardian did.Citation21 In the current study, the agreement between a child and the parent/guardian’s perceived effect of oral health on QoL was moderate. ICC was higher among males, older children, more educated parent/guardians, and higher income families. An interesting observation also was that agreement between the two scales increases by increasing orthodontic treatment needs. A Brazilian study with the same age group and setting but using different scales (The Parental-Caregiver Perceptions Questionnaire and the short form of the Child Perceptions Questionnaire) reported almost identical level of agreement as the current study.Citation22 Our findings, however, disagree with the findings of Jokovic et alCitation25 who found a disagreement in most of the questions between the children and their parents. This was attributed to either the fact that children in this age group experience life changes which make it difficult to identify which daily activities are affected solely by the need for orthodontic treatment,Citation5 or to the fact that some parents have limited knowledge concerning their children’s OHRQoL.Citation23 That is why both parents and their children’s reports were included in the present study. Because OHRQoL scales are relative rather than absolute measures, these results were expressed as comparisons of the impacts on daily activities between patients with different orthodontic treatment needs.Citation24 An important fact that should be emphasized is that the evaluation of agreement between parent and children scales is far more complex and requires additional procedures, such as the calculation of mean directional and absolute differences as well as the standardized difference, and not the ICC alone. Future detailed study should be considered to evaluate the level of agreement between the Michigan OHRQoL Scales–Version C and Version PG.
Difficulty in chewing food and biting hard objects were significantly related to IOTNs of the children. This was in agreement with the results of Hassan and Amin,Citation18 who found that malocclusion negatively affects subjects’ ability to process and break down foods in younger adults.
The appearance of the face plays an important psychosocial role in human life and interpersonal relationships. Furthermore, the features most commonly associated with facial attraction are the eyes and the mouth.Citation25 The present study found that dissatisfaction of the examined children with the way their teeth look was significantly associated with orthodontic treatment needs. This disagrees with the findings of DiBiase and SandlerCitation28 and Lazaridou-Terzoudi et al,Citation29 who reported no significant associations between malocclusion and self-consciousness. On the other hand, it agrees with the observation of Hassan and AminCitation18 and Dion et al,Citation30 who found that self-consciousness was significantly affected by orthodontic status. In addition, it seems that dental esthetics and smile do affect QoL measures at this age group, as confirmed by the parents’ and children’s opinions when asked about being teased about the shape of the teeth.
The present study being based on a clinical sample, and collected from one clinical setting, indicates that our results cannot be generalized to all children selected for orthodontic treatment. Further studies involving different clinical settings are indicated. The cross-sectional nature of the current study prevents exploring the effect of orthodontic treatment on future OHRQoL. The narrow range of age used in the present study did not allow for comparison by age. The scales used, the Michigan OHRQoL Scales–Version C and Version PG, seem to lack some of the important QoL measures such as pronunciation and speech, which were reported as not significantly associated with orthodontic treatment needs.Citation16 Possibly, different instruments should be used to give more definitive conclusions about the children’s overall QoL measures. In addition, this study was not conducted to calibrate the Arabic version of Michigan OHRQoL Scales–Version C and Version PG. However, to ensure reliability and validity of the Arabic version of the scales, they were translated into Arabic by experts in both Arabic and English languages and then back-translated into English to confirm the consistency of Arabic and English versions, and were carefully revised to ensure proper translation. In addition, validity of the scales was also assessed by correlation of the scales with IOTN and also by correlation between parent and child forms. Cronbach’s alpha indicated reasonable reliability of the scale for CHRQL (0.640) and acceptable reliability for the PG version (0.739). Still, future study is required to calibrate the Arabic version of the scale used. The present study being based on a clinical sample, and collected from one clinical setting, indicates that our results cannot be generalized to all children selected for orthodontic treatment. Further studies involving different clinical settings are indicated. The cross-sectional nature of the current study prevents exploring the effect on orthodontic treatment on future OHRQoL. The narrow range of age did not allow for comparison by age.
Conclusion
The modest agreement between child and parent/guardian perception of OHRQoL indicates that none of them can be used solely but they may be complementary to each other. With more suffering on the oral health side, the agreement between child and parent/guardian increases. Higher income and borderline IOTN are significantly related to oral health impact on QoL perceived by children, while younger age and high school education are related to oral health impact on QoL perceived by parent/guardians. The findings of the present study emphasize the importance of the assessment of OHRQoL measures in children, which has the potential to provide a greater understanding of the consequences of malocclusion, the effects of malocclusion if left untreated, and also the benefits of orthodontic care and its effect on children.
Acknowledgments
The authors thank the Deanship of Scientific Research at King Abdulaziz University for providing the fund for this research: project no. 429/016-9. The authors also thank Dr Arwa Radwan, an intern at King Abdulaziz University, Faculty of Dentistry, for her great assistance during this research.
Disclosure
The authors declare that they have no competing interests in this work.
References
- BediRGulatiNMcGrathCA study of satisfaction with dental services among adults in the United KingdomBr Dent J200519843343715870803
- CarotenutoMEspositoMPascottoAFacial patterns and primary nocturnal enuresis in childrenSleep Breath201115222122720607423
- PerilloLEspositoMContielloMLuccheseASantiniACCarotenutoMOcclusal traits in developmental dyslexia: a preliminary studyNeuropsychiatr Dis Treat201391231123724009421
- LockerDConcept of oral health, disease and the quality of lifeSladeGDMeasuring Oral Health and Quality of LifeChapel HillUniversity of North Carolina19971123
- CunninghamSJHuntNPQuality of life and its importance in orthodonticsJ Orthod20012815215811395531
- AhmedBGilthorpeMSBediRAgreement between normative and perceived orthodontic need amongst deprived multiethnic school children in LondonClin Orthod Res20014657111553087
- de OliveiraCMSheihamAOrthodontic treatment and its impact on oral health-related quality of life in Brazilian adolescentsJ Orthod200431202715071148
- FilstrupSLBriskieDda FonsecaMLawrenceLWanderaAInglehartMEarly childhood caries and quality of life: child and parent perspectivesPediatr Dent20032543144014649606
- PerilloLEspositoMCaprioglioAAttanasioSSantiniACCarotenutoMOrthodontic treatment need for adolescents in the Campania region: the malocclusion impact on self-conceptPatient Prefer Adherence2014835335924672229
- UkraAFoster PageLAThomsonWMFarellaMTawse SmithABeckVImpact of malocclusion on quality of life among New Zealand adolescentsN Z Dent J2013109182323923152
- PalomaresNBCelesteRKOliveiraBHMiguelJAHow does orthodontic treatment affect young adults’ oral health-related quality of life?Am J Orthod Dentofacial Orthop201214175175822640677
- SladeGDAssessing change in quality of life using the oral health impact profileCommunity Dent Oral Epidemiol19982652619511843
- CarvalhoACPalivaSMViegasCMScarpelliACFerreiraFMPordeusIAImpact of malocclusion on oral health related quality of life among Brazilian preschool children: a population studyBraz Dent J20132465566124474365
- MurrayHLockerDMockDTenenbaumHCPain and the quality of life in patients referred to a craniofacial pain unitJ Orofac Pain1996103163239161236
- EnglishJDBuschangPHThrockmortonGSDoes malocclusion affect masticatory performance?Angle Orthod200272212711843269
- LeeASWhitehillTLCioccaVSammanNAcoustic and perceptual analysis of the sibilant sound/s/before and after orthognathic surgeryJ Oral Maxillofac Surg20026036437211928089
- TaylorKRKiyakAHuangGJGreenleeGMJolleyCJKingGJEffects of malocclusion and treatment on the quality of life of adolescentsAm J Orthod Dentaofacial Orthop2009136382392
- HassanAHAminHel-SAssociation of orthodontic treatment needs and oral health-related quality of life in young adultsAm J Orthod Dentofacial Orthop2010137424720122429
- BrookPHShawWCThe development of an index of orthodontic treatment priorityEur J Orthod1989113093202792220
- TsakosGGherunpongSSheihamACan oral health-related quality of life measures substitute for normative needs assessments in 11 to 12-year-old children?J Public Health Dent20066626326817225821
- World Health OrganizationWHO Basic Oral Health Survey4th edGeneva, SwitzerlandWorld Health Organization1997
- MandallNAVineSHullandRWorthingtonHVThe impact of fixed orthodontic appliances on daily lifeCommunity Dent Health200623697416800360
- EiserCMorseRCan parents rate their child’s health-related quality of life? Results of a systematic reviewQual Life Res200110434735711763247
- FerreiraMCGoursandDBendoCBRamos-JorgeMLPordeusIAPaivaSMAgreement between adolescents’ and their mothers’ reports of oral health-related quality of lifeBraz Oral Res201226211211822473345
- JokovicALockerDGuyattGHow well do parents know their children? Implications for proxy reporting of child health-related quality of lifeQual Life Res2004131297130715473508
- RobertsEEBealesJGDixonLWillcocksAJWillmotDRThe orthodontic condition and treatment status of a sample of 14-year old children in North DerbyshireCommunity Dent Health198962492562804762
- EtcoffNSurvival of the Prettiest. The Science of BeautyLondonLittle, Brown and Company1999
- DiBiaseATSandlerPJMalocclusion, orthodontics and bullyingDent Update20012846446611806190
- Lazaridou-TerzoudiTKiyakHAMooreRAthanasiouAEMelsenBLong-term assessment of psychologic outcomes of orthognathic surgeryJ Oral Maxillofac Surg20036154555212730832
- DionKLDionKKKeelanJAppearance anxiety as a dimension of social-evaluation anxiety: exploring the ugly duckling syndromeContemp Soc Psychol199014220224
- FeuDMiquelJACelesteRKOliveiraBHEffect of orthodontic treatment on oral health-related quality of lifeAngle Orthod20138389289823593976
- Bellot-ArcísCMontiel-CompanyJMAlmerich-SillaJMPsychosocial impact of malocclusion in Spanish adolescentsKorean J Orthod20134319320024015389
- JokovicALockerDStephensMKennyDTompsonBGuyattGValidity and reliability of a questionnaire for measuring child oral-health-related quality of lifeJ Dent Res20028145946312161456
- OliveiraBHNadanovskyPPsychometric properties of the Brazilian version of the oral health impact profile-short formCommunity Dent Oral Epidemiol20053330731416008638
- TalekarBSRozierRGSladeGDDevelopment of an OHRQoL 9 instrument for preschool childrenJ Dent Res200483Special Issue A686
- BroderHLJanalMWilson-GendersonMReisineSTPhillipsCReliability and validity of the child oral health impact profileJ Dent Res200583Special Issue A2652
- HassanAHOrthodontic treatment needs in the western region of Saudi Arabia: a research reportHead Face Med20062216420691
- PatelRRTootlaRInglehartMRDoes oral health affect self perceptions, parental ratings and video-based assessments of children’s smiles?Community Dent Oral Epidemiol2007351445217244137
