Abstract
Purpose
Homeless individuals face unique challenges in health care. Several US initiatives seeking to advance patient-centered primary care for homeless persons are more likely to succeed if they incorporate the priorities of the patients they are to serve. However, there has been no prior research to elicit their priorities in primary care. This study sought to identify aspects of primary care important to persons familiar with homelessness based on personal experience or professional commitment, and to highlight where the priorities of patients and professionals dedicated to their care converge or diverge.
Methods
This qualitative exercise asked 26 homeless patients and ten provider/experts to rank 16 aspects of primary care using a card sort. Patient-level respondents (n=26) were recruited from homeless service organizations across all regions of the USA and from an established board of homeless service users. Provider/expert-level respondents (n=10) were recruited from veteran and non-veteran-focused homeless health care programs with similar geographic diversity.
Results
Both groups gave high priority to accessibility, evidence-based care, coordination, and cooperation. Provider/experts endorsed patient control more strongly than patients. Patients ranked information about their care more highly than provider/experts.
Conclusion
Accessibility and the perception of care based on medical evidence represent priority concerns for homeless patients and provider/experts. Patient control, a concept endorsed by experts, is not strongly endorsed by homeless patients. Understanding how to assure fluid communication, coordination, and team member cooperation could represent more worthy targets for research and quality improvement in this domain.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
A national effort to prioritize patient-centered care has emerged from 2 decades of scholarshipCitation1–Citation4 and is exemplified by the establishment of a Patient-Centered Outcomes Research Institute (PCORI).Citation5,Citation6 Until recently, the potentially unique concerns of homeless patients, a population estimated to number 633,782 nightly,Citation7 have been underrepresented in deliberations on primary care quality. For example, homeless persons are not specified by Congress as a “priority population” for the Agency for Healthcare Research and Quality.Citation5
Persons experiencing homelessness may obtain primary care through federally sponsored and private agencies, including Health Care for the Homeless programs,Citation8 the Department of Veterans Affairs, and charity clinics.Citation9 Several factors lend new impetus to the question of how to assure that their care is patient-centered. First, under new legislation, many homeless persons will acquire Medicaid.Citation10 Additionally, in 2012, the Veterans Health Administration sponsored 37 homeless-tailored primary care clinics, a program whose continuing expansion in 2013 reflects institutional embrace of “homeless-tailored” primary care.Citation11
A premise guiding this study is that any effort to define “patient-centered” primary care for homeless individuals should begin with the declared priorities of homeless patients and those professionals who have focused their careers on advancing their care. Available instruments to assess perceptions of primary care in the general populationCitation12,Citation13 may not reflect those priorities, however.
Accordingly, at the outset of an ongoing effort to develop a new instrument to assess homeless patient experiences, this study sought to identify aspects of primary care important to persons familiar with homelessness based on personal experience or professional commitment. Additionally, we wished to highlight where the priorities of homeless patients and professionals dedicated to their care might converge or diverge.
Methods
This study used a card sort exercise to prioritize constructs related to primary care. Card sorts are formal exercises that attempt to elicit subjective perceptions in a structured manner, and such exercises may seek to identify subjective categories, or priority rankings, the latter being the present goal.Citation14
The development of a list of potentially important quality-related constructs drew on work by expert committees of the Institute of Medicine (IoM), including the “10 Rules for Quality” published in its Crossing the Quality Chasm reportCitation15 and elements of the definition of primary care crafted by the IoM’s Committee on the Future of Primary Care.Citation16 The IoM primary care definition previously guided Safran’s development of a primary care experience survey.Citation17
To produce a sortable list of constructs, a multidisciplinary research team (including experts in psychology, social work, and primary care) reviewed concepts from the IoM reports, winnowed them down to avoid redundancy, and crafted language to express each of 16 constructs in short sentences in order to facilitate self-administration by providers and patients, some with low literacy.
Each resulting statement included the stem “Primary care should …” followed by language encompassing the construct of interest (). Each was printed on a separate card and placed into a packet with a return envelope. We instructed participants to bind the cards in order of priority, and return them.
Table 1 Primary care quality constructs derived from two IoM reports and their ordinal ranking among patients and provider/experts in homeless health careTable Footnotea
Patients who had experienced homelessness were recruited a) from the Consumer Advisory Board of the National Health Care for the Homeless Council (n=5) and b) through veteran-focused homeless service programs in nine US states encompassing all geographic regions of the country, identified primarily from the website of the National Coalition for Homeless Veterans (n=21). For this exercise, homeless-focused provider/experts were persons with significant professional commitment (typically >10 years) to homeless services, or to research and policy in the care of homeless individuals. They were solicited from 17 organizations across 14 states and the District of Columbia with the goal of maximizing participation from all geographic regions of the USA, and assuring a mix of direct service providers and experts (ie, program leaders or homeless health care research experts) in homeless health care from veteran- and non-veteran-focused agencies.
Card response packets were anonymous, reflecting Institutional Review Board rules typically applicable to VA-sponsored research. Given the anonymous and nonsensitive nature of the packets sent, informed consent was implied by return of the packet to the research team. Response rates were comparable; 65% of patients (26 out of 40) and 53% of provider/experts (ten out of 19). Returned cards were numbered 1–16 with response sequences entered in a spread-sheet. We computed the mean value for each construct (ie, its position within the deck of 16 cards), separately for patients and provider/experts. These means ordered from lowest (1= most important) to highest (16= least important) to illustrate their relative importance to patients and to provider/experts. Because the computation of mean values does not illustrate the range of rankings among patients and provider/experts, we also produced vertical scatterplots to allow visual consideration of response “spread” and overlap between patients and provider/experts, using Tableau software (Tableau, Seattle, WA, USA). This activity had the approval of the Institutional Review Board of the Birmingham VA Medical Center.
Results
With respect to average rankings of constructs, patients and provider/experts agreed on the two most important characteristics of homeless patient care: accessibility and evidence-based decision making (). Cooperation, coordination, and accountability were also ranked in the top six by both groups. Transparency, concerns about minimizing waste of time or money, and matching care to the context of a patient’s community and family were ranked less favorably by both groups.
There were notable divergences in rankings between patients and provider/experts. Patients considered “shared knowledge and the free flow of information” about care to be important (ranked 4th of 16), while provider/experts gave this low priority (14th). Provider/experts assigned high priority to patient control of health care (4th), while patients gave this a far lower priority (10th).
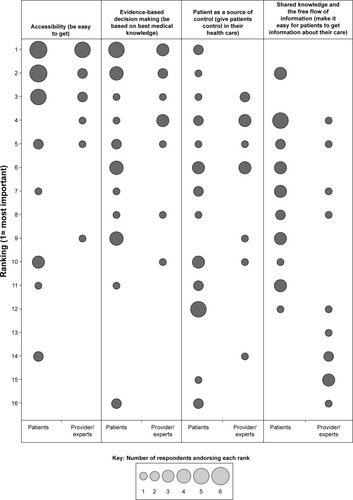
Study of the actual distribution of ranks identified significant spread among patients and among provider/experts. For four constructs where there was notable convergence or divergence, depicts the frequency of rankings from most prioritized (1) to least prioritized (16), with the size of the circle reflecting the number of respondents assigning that ranking. For accessibility and evidence-based decision making, the tendency for both patients and provider/experts to assign high priority is evident. For patient control in their care, lower priority was given by patients, but visual examination shows variation among patients (with predominance toward the less-prioritized end of the scale). For the priority of shared knowledge and free flow of information, despite considerable overlap, patients gave a substantively more favorable ranking than providers.
Figure 1 Frequency of rankings among patients and provider/experts for selected primary care quality constructs.
Discussion
This exercise highlights areas of convergence and divergence in the priorities for primary care embraced by homeless patients and professionals committed to their care. Homeless patients and provider/experts both prioritize easy access to primary care and the concern that such care be based on the best medical knowledge. Shared prioritization of accessibility is unsurprising.Citation18,Citation19 Conversely, there have been fewer efforts to assess whether homeless persons believe their care is evidence-based, and what effect such perceptions may have on adherence, engagement, or other outcomes.
These results notably highlight a divergence between the perceived value of “control” in care (ranked low by patients but high by provider/experts) versus information about care (prioritized by patients but less so by provider/experts). Devaluation of control relative to information has been seen in other populations,Citation20,Citation21 but this is the first study to suggest that a similar divergence applies between homeless patients and provider/experts. We speculate that issues of control may be particularly sensitive for populations where mental illness and addiction issues are common. The relatively low priority assigned to control suggests that the IoM’s explicit embrace of patient controlCitation15 per se may be less resonant for this population.
By contrast, the free flow of information was highly valued by patients. Information and understanding may play roles in alleviating distress, separate from the quality of the treatment administered. Additionally, patient-centered communications may convey respect and inform choices.Citation22
Limitations apply to this study. By their nature, qualitative data do not reflect systematic and representative samples of a population. However, no survey of homeless patients has ever sought to assess their primary care preferences. Moreover, the geographic diversity of participants assigns a degree of credibility to these results in guiding future efforts on this topic.
Separately, it should be acknowledged that revelation of priorities through a sorting exercise necessarily cannot render a rich portrait of personalized meanings respondents might assign to each concept. Detailed interview work would be an appropriate next step. Nonetheless, the brief declarative format used for the cards (eg, “Primary care should be easy to get”) limits the potential for unexpected interpretations.
Despite these limitations, the present findings identify several concepts of importance to the primary care of homeless individuals, if that care is to embody the ideal of patient-centeredness. They suggest that measures of care from the patient’s perspective must seek to operationalize several priority concerns, including perceptions of whether care is accessible, evidence-based care, and characterized by the free flow of information. The findings also invite further research concerning how providers and patients might assign different meanings and interpretations to concepts such as control, information, and cooperation.
Acknowledgments
This study is sponsored by the Department of Veterans Affairs, Health Services Research and Development Branch, Merit Award 07-969. Opinions expressed within this manuscript are those of the authors alone and do not represent positions of the Veterans Health Administration or any entity within the US federal government.
Disclosure
The authors report no conflicts of interest in this work.
References
- GerteisMEdgman-LevitanSDaleyJDelbancoTLThrough the Patient’s Eyes: Understanding and Promoting Patient-Centered CareSan Francisco, CAJossey-Bass1993
- BechelDLMyersWASmithDGDoes patient-centered care pay off?Jt Comm J Qual Improv20002640040910897457
- WeinerSJSchwartzAWeaverFContextual errors and failures in individualizing patient care: a multicenter studyAnn Intern Med2010153697520643988
- SofaerSFirmingerKPatient perceptions of the quality of health servicesAnnu Rev Public Health20052651355915760300
- Patient Protection and Affordable Care Act (Public Law 111–148)Washington, DCThe U.S. Government Publishing Office2010
- WashingtonAELipsteinSHThe Patient-Centered Outcomes Research Institute – promoting better information, decisions, and healthN Engl J Med2011365e3121992473
- Office of Planning and Community Development2012 Point-in-Time Estimates of Homelessness: Volume 1 of the 2012 Annual Homeless Assessment ReportWashington, DCUnited States Department of Housing and Urban Development2012
- National Health Care for the Homeless CouncilFrequently Asked Questions About Health Care for the HomelessNashville, TNNHCHC2011
- KerteszSGMcNeilWCashJJUnmet need for medical care and safety net accessibility among Birmingham’s homelessJ Urban Health201491334523620012
- Kaiser Commission on Medicaid and the UninsuredMedicaid Coverage and Care for the Homeless Population: Key Lessons to Consider for the 2014 Medicaid ExpansionWashington, DCThe Henry J. Kaiser Family Foundation2012
- O’TooleTPBuckelLBourgaultCApplying the chronic care model to homeless veterans: can a population approach to primary care impact utilization and clinical outcomes?Am J Public Health20101002493249920966377
- HaysRDShaulJAWilliamsVSPsychometric properties of the CAHPS 1.0 survey measures. Consumer Assessment of Health Plans StudyMed Care199937MS22MS3110098556
- Agency for Healthcare Research and QualityCAHPS Clinician & Group Surveys: 12-Month Survey with Patient Centered Medical Home (PCMH) ItemsWashington, DCUnited States Department of Health and Human Services2012
- McKeownBThomasDQ MethodologyNewbury Park, CASage Publications1988
- IoM Committee on Quality of Health Care in AmericaCrossing the Quality Chasm: A New Health System for the 21st CenturyWashington, DCNational Academy Press2001
- Committee on the Future of Primary Care for the Institute of MedicinePrimary Care: America’s Health in a New EraWashington, DCNational Academy Press1996
- SafranDGKosinskiMTarlovARThe Primary Care Assessment Survey: tests of data quality and measurement performanceMed Care1998367287399596063
- BaggettTPO’ConnellJJSingerDERigottiNAThe unmet health care needs of homeless adults: a national studyAm J Public Health20101001326133320466953
- KushelMBVittingoffEHaasJSFactors associated with the health care utilization of homeless personsJAMA200128520020611176814
- EndeJKazisLAshAMoskowitzMAMeasuring patients’ desire for autonomy: decision making and information-seeking preferences among medical patientsJ Gen Intern Med1989423302644407
- LevinsonWKaoAKubyAThistedRANot all patients want to participate in decision making. A national study of public preferencesJ Gen Intern Med20052053153515987329
- MansonNCWhy do patients want information if not to take part in decision making?J Med Ethics20103683483720826868
