Abstract
Of several newer delivery systems under development and investigation for the administration of opioids, the intranasal route has received a substantial amount of attention. Intranasal administration is a convenient form of delivery that is applicable to several opioids. It has the potential for self-administration, combined with a rapid onset of action, allowing for patient-controlled analgesia. In clinical practice, intranasal administration has been found to be a reliable drug delivery method that is familiar to patients. Intranasal opioids have proven to be useful in both in-hospital and out-of-hospital pain management settings. Fentanyl, a highly lipophilic step 3 opioid, has been evaluated for intranasal administration. The purpose of this review is to examine the role of the nasal route of opioid administration and examine the evidence base for the use of fentanyl intranasally.
Keywords:
Introduction
Pain is a common symptom in the general population and has a substantial impact on quality of life. Pain can be a major burden to patients and society. Opioids are among the most potent analgesics available and are the cornerstone of treatment for moderate to severe pain associated with cancer.Citation1 Opioids can decrease pain and improve function.Citation2 Most commonly recommended is the oral route of administration. There are times when nonoral routes of administration are necessary, such as in patients with advanced illness or in the postoperative period. Nonoral routes of administration have been shown to be more effective than the oral route by providing enhanced absorption and avoidance of first-pass effects. The nonoral routes of opioid administration include parenteral (subcutaneous, intravenous), rectal, sublingual, and transmucosal. The parenteral routes of administration are associated with rapid onset of action but can be associated with pain and inconvenience. The rectal route of administration has been evaluated for opioid administration and, although effective, can have limitations in terms of dignity for the patient and lack of uniform absorption. The sublingual and transmucosal routes are effective nonoral routes that have the advantage of avoiding presystemic elimination, yet can have suboptimal absorption due to swallowing. Lack of salivary production may impede the absorption of opioids when given by the transmucosal route.
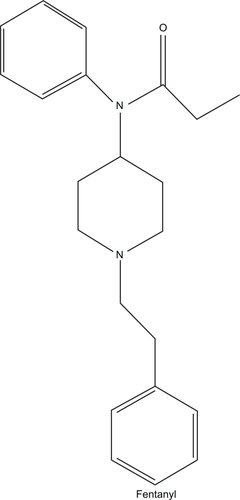
The intranasal route has increasingly been viewed as a new alternative route for drug administration. The intranasal route is a convenient form of delivery that is applicable to several opioids and has the potential for self-administration, combined with a rapid onset of action. In clinical practice, intranasal administration has been found to be a reliable drug delivery method that is familiar to patients. Intranasal opioids have proven to be useful in both in-hospital and out-of-hospital pain management settings. Fentanyl () is a step 3 opioid that is used for acute and chronic pain of both malignant and nonmalignant origin. It is a lipophilic, short-acting, synthetic opioid with a piperidine chemical structure.Citation3 Fentanyl can be administered by the transdermal, transmucosal, or sublingual routes, in addition to the traditional parenteral routes. Recently, fentanyl has been evaluated for intranasal administration. The purpose of this review is to examine the role of the nasal route of opioid administration and examine the evidence base for the use of fentanyl intranasally.
Anatomy and physiology of the nose
In adults, the nasal mucosa provides a large mucosal surface area (150–180 cm2) that is closely associated with high blood flow.Citation4 This blood flow is greater per cubic centimeter of tissue than that of muscle, the brain, or the liver.Citation4 The nose has a direct connection to the central nervous system via the olfactory route. Theoretically, the direct delivery of drugs to the brain allows lower doses of drugs to be used, with less delivery to nontargeted organs, and perhaps less toxic side effects.Citation5 The nasal mucosa has a pH of 5.5–6.5, which maintains optimal function of glycoproteins to which drugs attach.Citation4 Drug absorption through the nasal mucosa is also dependent on lipophilicity, drug ionization, and mucociliary clearance.Citation6 These features make the nasal route a potentially useful route for the administration of drugs such as lipophilic opioids. The route avoids first-pass metabolism.Citation4 The intranasal route of drug administration has been used for a variety of drugs, such as vaccines,Citation7 opioids, benzodiazepines, migraine therapies,Citation8 and gene therapy.Citation5 Metabolic enzymes are present in the nasal mucosa and thus are able to metabolize drugs administered there.Citation5
Formulations
Typical formulations of intranasal fentanyl consist of using an intravenous solution either directly or via spray devices.Citation9 The ideal volume recommended is 0.15 mL in one or both nostrils.Citation6 This is important, as run-off from the nasal cavity has the potential to be swallowed. Penetration enhancers have been used to overcome volume limitations, and additives such as polymers and gels or polysaccharides can enhance contact time, improving absorption.Citation10 One study has demonstrated improved fentanyl absorption with polysaccharides such as pectin, chitosan, and chitosan–poloxamer compared with transmucosal fentanyl.Citation11 Biospheres may also increase residence time on the nasal mucosa.Citation11
Intranasal pharmacokinetics compared with other routes of fentanyl administration
The pharmacology of several opioids has been evaluated after intranasal administration.Citation6 Opioids that have been evaluated include the fentanyl series, oxycodone, methadone, buprenorphine, and diacetylmorphine. All the lipophilic opioids show rapid absorption, with time to maximum plasma concentration (tmax) ranging from as short as 9 minutes for alfentanyl to up to 30 minutes for sufentanil. When administered via an intranasal spray, all of the opioids described reach tmax in less than 30 minutes. Bioavailability of lipophilic opioids given intranasally is high and greater than the oral route for all step 3 opioids, with the exception of oxycodone.Citation6 The pharmacokinetic data of all of the studies of opioids support the use of noninvasive intranasal drug delivery when a fast onset is indicated. When fentanyl is administered by the intranasal route, the bioavailability is nearly 70%, with tmax reached in 5–16 minutes.Citation12 Fentanyl levels show dose dependency when administered intranasally. The absorption of fentanyl can be influenced by pH, with greater absorption as the pH increases.Citation13 Temperature can influence absorption, with greater permeation of fentanyl intranasally.Citation14 The half-life is up to 65 minutes when given by intranasal route. Pharmacokinetic comparisons have been made between intranasal fentanyl and other routes of administration, such as transmucosally administered fentanyl. Transmucosal fentanyl has a decreased bioavailability and area under the curve compared with intranasal fentanyl.Citation15 The half-life of transmucosal fentanyl is longer than intranasal fentanyl.Citation15 Compared with intravenous fentanyl, the intranasal route has a slower onset of action. The half-life of the intravenous route is longer than that of the intranasal route.Citation16
Adverse effects
When given intranasally, fentanyl can cause not only local effects specific to the intranasal route but also systemic adverse effects typical for opioids in general.Citation6 The systemic effects of intranasally administered fentanyl can include dizziness, as well as sedation, nausea, and constipation. Local effects include nasal discomfort and irritation, the most common adverse effect with short-term use. There are fewer data on the long-term effects of intranasal opioid administration, but reports exist of epistaxis, pharyngitis, and sinus congestion. Respiratory depression does not occur more frequently with this route.Citation6 Some indications are that polymer fentanyl combinations may prevent a higher incidence of adverse effects.Citation17
Drug interactions
Fentanyl is metabolized by the cytochrome P450 3A4 liver isoenzyme system, and potent inhibitors of this enzyme may produce increased or prolonged opioid side effects.Citation18 The concomitant use of other central nervous system depressants may produce additional sedative effects.
Clinical trials
Intranasal fentanyl has been evaluated for cancer-related breakthrough pain and postoperative pain and has been compared with morphine in several painful clinical conditions. There have been some studies in the management of symptoms in the hospice setting.
Cancer-related breakthrough pain
Breakthrough pain associated with cancer is defined as a transitory exacerbation of pain experienced by a patient who has relatively stable and adequately controlled baseline pain.Citation19 The use of a lipophilic opioid such as fentanyl has been shown to be effective when given by other routes such as the transmucosal routeCitation20 and in formulations such as a buccal tablet,Citation21 due to the lipophilic nature of the drug and its rapid onset of action. The rapid onset of action of fentanyl can match the rapid onset of action for most forms of breakthrough pain. The rapid onset of action by the intranasal route has been evaluated as another alternative route for the management of breakthrough pain.
Intranasal fentanyl and placebo
Intranasal fentanyl spray (INFS) at a dose range of 50–200 μg was evaluated for cancer-related breakthrough pain and compared with placebo. One multicenter, blinded, crossover trialCitation22 focused on adult cancer patients who experienced at least three episodes of severe breakthrough pain per week, and up to a maximum of four episodes per day lasting longer than 15 minutes. Patients had already been receiving strong opioids such as oral morphine, oxycodone, or hydromorphone with dosages ranging from 60 mg to 500 mg per day, and transdermal fentanyl dosages ranging from 25 μg to 200 μg per hour. Patients were required to be at stable opioid dosing levels, with pain scores less than 4 on an 11-point numeric rating scale (NRS) for pain for entry into the trial. Because there is evidence that the breakthrough dose of fentanyl does not correlate with the amount of scheduled opioid, doses of intranasal fentanyl for breakthrough pain were individually titrated. A dose was considered successful if it could treat three of four episodes of breakthrough pain. Responses were measured by categorical scale (0 = poor; 1 = fair; 2 = good; 3 = very good; and 4 = excellent). A successful dose had to get a score of 2 on the categorical scale 60 minutes after the breakthrough dose. There also had to be an absence of adverse effects to qualify for a successful breakthrough dose. Once the breakthrough dose was determined, randomization occurred to treatment sequences composed of two sets of four administrations (numbered 1–4 and 5–8), with each set comprising three INFS administrations and one placebo administration. Patients were instructed to treat eight episodes of breakthrough pain (to a maximum of four episodes daily) using the order in which the spray bottles were numbered (1–8). Patients recorded their pain in a diary using the 11-point NRS at times 10, 20, 40, and 60 minutes after administration. The main endpoint was the difference in the pain score at 10 minutes after administration (pain intensity difference [PID]10), with secondary endpoints being the sum of the pain intensities from baseline to 60 minutes after administration, and the general impression of efficacy at 60 minutes, using the aforementioned categorical scale. Clinically important PID10 scores are a decrease in pain of more than 2 points. Mean response rates were calculated for drug or placebo in each patient as well as reduction in pain intensities by more than 33% and more than 50%, respectively. One-hundred and eleven patients were included in the study from an initial 120 patients. The results favored the intranasal fentanyl, as the PID10 was twice as great as for placebo (P < 0.001). The overall response rate for INFS was 51%, with 20% of responses observed in the placebo arm. Adverse effects were observed in nearly 20% of patients, the most common being nausea (4.5%) and vertigo (1.8%).
Fentanyl pectin formulation
A multicenter, randomized, blinded, placebo-controlled study conducted by the Nasal Spray 043 Study GroupCitation23 evaluated the efficacy of fentanyl pectin nasal spray (FPNS) for cancer breakthrough pain. One-hundred and fourteen cancer patients who were taking at least 60 mg of oral morphine or an equivalent opioid and who had one to four episodes of moderate to severe breakthrough pain were eligible for participation. Patients were titrated to the appropriate breakthrough dose (open label). Once a dose was identified, patients were randomized to receive 10 bottles, seven of which contained the effective dose and three contained placebo in a randomly assigned sequence. Patients could take up to four doses daily with 4 hours separated between doses. If the pain was not controlled in 30 minutes, or an episode of breakthrough pain occurred within the 4-hour period, patients could take their usual breakthrough medication. Pain relief was measured by NRS and categorical scale at baseline and at 5, 10, 15, 30, 45, and 60 minutes after administration. Patients had to rate overall satisfaction. Electronic diaries recorded information on the breakthrough doses. Adverse effect assessment included categorical scoring for local nasal effects.
Primary efficacy was measured by outcomes such as pain intensity, pain intensity differences from baseline, sum of pain intensity differences, pain relief, and total pain relief. Patients also evaluated ease and convenience by categorical scales (0–3). Seventy-two percent identified a breakthrough dose. Six percent withdrew due to lack of efficacy, and 5% withdrew due to adverse effects. Baseline pain scores were comparable between placebo and study drug groups. Fentanyl was more effective in reducing pain intensity at all time points and had quicker onset of analgesic effects than placebo. One-third of FPNS-treated episodes had clinically meaningful reduction at 10 minutes (P = 0.01 vs placebo) and had an increase to 66% of episodes at 30 minutes (P < 0.0001 vs placebo). There were more 2-point pain reductions with FPNS at each time point after dosing (P < 0.01). In addition, the FPNS group has a greater number of 1- or 2-point reductions at each time point. There was less need for additional breakthrough medications with FPNS (P < 0.001). Patient acceptability was better for the FPNS group at 30 and 60 minutes than for the placebo group. FPNS was also superior in terms of time to relief than placebo at 30 and 60 minutes (P < 0.0001) for both times. Scores for reliability of pain relief were better for the FPNS group, as were acceptability after the last treated episode and ease of use of the spray formulation in terms of convenience and satisfaction. Adverse effects were greater in the FPNS group. Systemic adverse effects consisted of vomiting (10.6%), nausea (8.8%), and dizziness (8.0%). Local effects consisted of epistaxis (4.4%) and nasopharyngitis (3.5%). Two deaths in the treatment group and one in the placebo group were believed to be unrelated to the drug.
Long-term safety of intranasal fentanyl
Portenoy et alCitation24 assessed the safety aspects of fentanyl pectin for cancer-related breakthrough pain. Patients in the study had chronic cancer pain requiring at least 60 mg of oral morphine equivalent per day and had one to four attacks of breakthrough pain per day. Individual dose titration identified the appropriate breakthrough dose. Dose changes were performed as necessary to optimize comfort, but 90% did not require a dose change. After reviewing the adverse effects of 42,000 episodes of breakthrough pain in 110 patients, 24% experienced adverse effects that were systemic in nature and characterized as mild. There were no significant local nasal effects.
Intranasal versus oral transmucosal fentanyl citrate
Mercadante et alCitation25 conducted an open-label crossover trial comparing intranasal with oral transmucosal fentanyl citrate (OFTC). Patients with cancer pain were screened for breakthrough cancer pain and, if eligible, received a test dose of fentanyl 50 μg. Patients whose pain was opioid responsive were entered into the study and randomized to receive INFS or OFTC. In the study, individual titration was conducted to identify a dose that could successfully treat three of four episodes of breakthrough pain. There was then a final phase lasting approximately 2 weeks, during which the identified doses with each formulation were used and compared with each other for onset of meaningful pain relief, pain intensity, and use. With regard to the intranasal fentanyl, patients could receive a second dose of intranasal analgesic if there was no pain relief after 10 minutes. If the second dose did not help, rescue analgesics were allowed 10 minutes after the second intranasal spray. More rescue analgesics were allowed at 45 and 60 minutes, depending on whether the second intranasal dose was required. The primary outcome was the (stopwatch) measured time to patient-reported meaningful pain relief for either the OFTC or intranasal route of administration. Pain intensity (NRS 0–10) was also measured at time points 5, 10, 15, 20, 30, and 60 minutes after administration of INFS or OTFC. If a rescue dose was taken at 60 minutes, the preceding pain intensity value was carried forward. PID was measured at 5-minute intervals for the first 30 minutes, and the sum of PID was calculated for the 0–15 minute and 0–60 minute intervals.
Categorical scales were used to describe ease of use. Treatment preferences were recorded after the patients completed both arms. The investigators calculated the relationship between doses required for breakthrough pain and scheduled analgesic doses. Finally, the proportion of patients with a greater than 33% and a greater than 50% reduction in pain intensity score was also calculated for each treatment at 5, 10, 15, 20, 30, and 60 minutes postdosing. One-hundred and thirty-nine patients were enrolled in the trial, but 53 did not complete the titration phase. Rates of withdrawal were the same between groups. A total of 577 breakthrough pain episodes were treated with INFS, and 577 episodes were treated with OFTC. Ninety-three percent of patients treated six breakthrough episodes with INFS, and 92% were treated with OFTC. Nearly equal numbers of patients were able to find effective doses of INFS and OFTC (85% and 87%, respectively). In the INFS group, 75% needed doses of 100–200 μg, and 60% in the OFTC group needed 200–400 μg doses for adequate breakthrough coverage. The investigators found a weak association between the amount of INFS taken and the amount of OFTC used for breakthrough pain, in that patients requiring higher INFS doses also needed higher OFTC doses, and those requiring lower doses of INFS needed lower doses of OFTC. Results in respect of the primary endpoint showed that the median time to meaningful pain relief was 11 minutes for INFS and 16 minutes for OFTC. More patients in the INFS group experienced a faster onset of pain relief than the OFTC group (P < 0.001). PID at 10 and 30 minutes was greater for the INFS group than for the OFTC group (P < 0.001) and at other times, such as 5, 15, 20, and 60 minutes postdosing. It appeared that the PIDs were in favor of the INFS group for 60 minutes postdosing (P < 0.001). Statistically significantly greater proportions of the INFS group achieved 33% and 50% reductions in pain scores than the OFTC group. There was a general impression of favorability that was greater with the INFS group. Fifty-six percent of patients experienced at least one adverse effect. The main adverse effect occurring in each arm of the study at a frequency of more than 5% was nausea. Most adverse effects were considered mild. The severe adverse effects were few in number and consisted of a slightly greater number in the INFS group (severe nausea and vomiting). One patient developed nasal ulcers in the INFS group, and the INFS was discontinued with subsequent healing of the wounds. Patients preferred INFS over OFTC (P < 0.001) and also found INFS to be easier to use than OFTC.
Postoperative pain in adults using INFS versus weak opioids
Striebel et alCitation26 evaluated the effects of intranasal fentanyl versus weak opioids as postoperative analgesic therapy in 20 patients receiving orthopedic procedures in a pilot study. On the first postoperative day, patients who had a postoperative pain score of 40 on a visual analog scale (VAS) were randomized to receive either intranasal fentanyl at 0.025 mg every 6 minutes for 4 hours or “standard ward therapy” consisting of agents such as pethidine, tramadol, metamizole, codeine, and diclofenac as single agents or in combination, followed by the alternative regimen. Pain was measured every 30 minutes by VAS, after randomization, up to 480 minutes. The results in both arms of the study showed effective pain control at 30 minutes, but, as time elapsed, pain levels were lower in the intranasal fentanyl arm. Patients also expressed greater satisfaction with fentanyl.
Intravenous fentanyl versus intranasal fentanyl
Patient-controlled analgesia (PCA) with intranasal fentanyl was compared with intravenous fentanyl in the postoperative period in 48 patients undergoing surgery for abdominal, orthopedic, or thyroid surgery.Citation27 Eligible patients had to have a pain score of at least 40 on the VAS. Randomization was to fentanyl 25 μg intranasally and fentanyl 17.5 μg intravenously, with lock-out intervals of 6 minutes. Blinding was achieved by double-dummy design, whereby each patient had an intravenous PCA device and an intranasal PCA device. When in pain, the patient activated both routes and received either fentanyl or saline. Pain intensity was measured by NRS for the duration of the 240-minute study. In the intranasal group, the first reduction in pain score was 21 ±11 minutes (range 15–45 minutes), and in the intravenous group was 22 ±16 minutes (range 15–90 minutes). Overall, there were no differences in overall pain intensity, and patient-rated intranasal analgesia was rated as “excellent” or “good”. Intranasal fentanyl was also compared with intravenous fentanyl for the management of acute and breakthrough pain in patients undergoing molar extractions.Citation28 Patients were randomized to one of four doses (75, 100, 150, or 200 μg) of fentanyl by both intranasal and intravenous routes randomly after two separate extractions at 1 or more weeks apart, with pain scores on an NRS measured before administration and at 15, 30, 45, 60, 75, 90, 105, 120, 150, 180, 210, and 240 minutes. Patients indicated time to meaningful pain relief and duration of analgesia. Plasma fentanyl levels were assessed before and at 1, 3, 5, 7, 9, 12, 15, 25, 40, 60, 90, 120, and 180 minutes after administration. Twenty-four patients were enrolled. Tmax was delayed compared with intravenous dosing (12.8 and 6.0 minutes [P < 0.001]), and onset of analgesia was slower for intranasal analgesia (7 and 2 minutes [P < 0.001]), but duration of analgesia did not differ between groups. There was a relationship between duration of effect and intranasal dose, and there was less use of breakthrough analgesia after the intranasal fentanyl (P < 0.005). Both groups tolerated the therapies well.
Pediatric analgesia
Intranasal fentanyl was compared with intravenous fentanyl in pediatric patients after abdominal surgery.Citation29 Postoperatively, 36 patients with pain scores greater than 6 according to an objective pain scale (OPS) were randomized into one of two groups. Group A (n = 17) received 0.5 mg/kg of intranasal fentanyl, followed by an intravenous injection of sodium chloride (1 mL of 0.9%). Patients in group B (n = 19) received intranasal normal saline (1 mL of 0.9%), followed by intravenous fentanyl 0.5 μg/kg. Pain scoring was conducted 5 minutes later, and those with scores of 2 or higher received the same protocol once, with scoring conducted every 1 minute. This was repeated 5 minutes later if scores were 2 or higher once again. The goal of such titration was to get to an OPS score of 2 or lower. Sixty minutes after the first administration, the primary scheme was carried out once per hour until 24 hours later. There were no differences between groups in time to achieve a score of less than 2. There was a greater amount of fentanyl used in group A. There were more adverse effects consisting of dizziness (32%) and nausea (21%) in group B than in group A (12% dizziness and 32% nausea [P < 0.05]). Pain scores were equally reduced in both groups at 4 hours postadministration.
Other surgery and pediatrics
INFS has been used for analgesia in pediatric patients undergoing myringotomy.Citation30 When given in conjunction with anesthesia, there is less postoperative agitationCitation31 and analgesia that is equivalent in potency to other modalities such as nerve block.Citation32
Intranasal fentanyl versus morphine
Several studies have been carried out comparing intranasal fentanyl with morphine. An emergency room-based, prospective, randomized, blinded, placebo-controlled studyCitation33 was carried out to evaluate the efficacy of intravenous morphine, intranasal placebo, and intranasal fentanyl for long bone fractures. Sixty-seven children were randomized to intravenous morphine (10 mg/mL) and intranasal placebo or intranasal fentanyl (150 μg/mL) and intravenous placebo. Pain scores by VAS were measured at 0, 5, 10, 20, and 30 minutes with adverse effects recorded. Thirty-four children received intravenous morphine and 33 received intranasal fentanyl. There were no differences in pain intensity reduction between the groups (P = 0.333) at 5 minutes and at time intervals thereafter. The mean dose of INFS was 1.7 μg/kg and the mean morphine dose was 0.11 mg/kg. Another comparison with morphine was conducted in burn patients where 26 adult patients (22 males) with burn surface areas ranging from 1% to 25% were randomized to a placebo-controlled, crossover study over two periods and two treatments.Citation34 Patients requiring identical wound management on consecutive days were randomized to patient-controlled intranasal fentanyl with oral placebo or oral morphine with intranasal placebo on the first day, with the alternating sequence on the subsequent day. Patients reported their pain intensity on an NRS before, during, and after the procedure. The mean dose of intranasal fentanyl given was 1.48 ± 0.57 μg/kg and 0.35 ± 0.12 mg/kg of oral morphine. There were no differences in pain scores between the groups. Two patients in the oral morphine group experienced hypotension, but there was no respiratory depression. Three patients required rescue analgesia, two cases involving morphine and one involving fentanyl.
Other uses
Hospice
The hospice setting may be a place where intranasal routes of administration can have benefit. Twelve hospice patientsCitation35 were evaluated for the analgesic effects of 20 μg of fentanyl for cancer-related breakthrough pain. Pain was rated by VAS before and 3, 5, 10, 15, 30, 45, and 60 minutes after receiving the dose. Eight of 12 experienced a reduction in pain score, four achieved an analgesic response after 5 minutes, and seven achieved an analgesic response within 10 minutes of receiving the dose. Nine patients felt that the analgesia obtained with the intranasal formulation was “good” or “very good”. Two patients experienced local nasal itching or discomfort on first use, but this disappeared with time. Of the three patients who did not experience a good response with the intranasal fentanyl, one had a fracture and two had what was described as “relatively higher baseline opioid doses”. A series of cases has shown efficacy for the use of intranasal fentanyl for the management of dyspnea in hospice patients.Citation36 The cases were notable because the intranasal fentanyl was administered by nasal spray and had a rapid onset on action, usually within 1 minute, with good relief obtained in 1–4 minutes. There was no worsening of pulmonary function during administration of the intranasal fentanyl with any of the cases. Individual titration of the appropriate dose for dyspnea is necessary.
Methods of administration
Fentanyl doses have been administered in one or both nostrils using fentanyl solutions of 0.5, 1.0, and 2.0 mg/mL, corresponding to doses of 50, 100, and 200 μg of fentanyl.Citation15 The clinical trials for breakthrough pain suggest the use of nasal spray devices, which can provide more uniform dosing with patients.
Conclusion
The intranasal route of opioid administration shows great promise as an alternative to the traditional routes of administration. It appears to be especially compatible with highly lipophilic agents such as fentanyl. Overall, the use of the intranasal route appears to be of low burden to patients, is amenable for pain management for a variety of analgesic issues ranging from postoperative pain to cancer-related breakthrough pain, and is applicable to both adult and pediatric patient populations. In all likelihood, the intranasal route of opioid administration will replace the oral route as an option for several types of breakthrough pain.
Disclosure
The authors report no conflicts of interest in this work.
References
- PattRBBurtonAWPain associated with advanced malignancy, including adjuvant analgesic drugs in cancer pain managementEvaluation and Treatment of Chronic PainNew YorkLippincott, Williams & Wilkins1998337376
- KalsoEEdwardsJEMooreRAMcQuayHJOpioids in chronic non-cancer pain: systematic review of efficacy and safetyPain200411237238015561393
- Dosen-MicovicLIvanovicMMicovicVSteric interactions and the activity of fentanyl analogs at the [mu]-opioid receptorBioorg Med Chem2006142887289516376082
- ShelleyKPaechMJThe clinical applications of intranasal opioidsCurr Drug Deliv200855518220551
- VyasTKShahiwalaAMaratheSMisraAIntranasal drug delivery for brain targetingCurr Drug Deliv2005216517516305417
- DaleOHjortkjaerRKharaschEDNasal administration of opioids for pain management in adultsActa Anaesthesiol Scand20024675977012139528
- BirkhoffMLeitzMMarxDAdvantages of intranasal vaccination and considerations on device selectionIndian J Pharm Sci200971729
- Veldhorst-JanssenNMLFiddelersAAAvan der KuyPHMA review of the clinical pharmacokinetics of opioids, benzodiazepines, and antimigraine drugs delivered intranasallyClin Ther2009312954298720110035
- SchwagmeierROelmannTDannappelTStriebelHWPatientenakzeptanz gegennber der patientenkontrollierten intranasalen Analgesie (PCINA)Der Anaesthesist1996452312348919895
- PenningtonAKRatcliffeJHWilsonCGHardyJGThe influence of solution viscosity on nasal spray deposition and clearanceInt J Pharm198843221224
- IllumLJorgensenHBisgaardHBioadhesive microspheres as a potential nasal drug delivery systemInt J Pharm198739189199
- Veldhorst-JanssenNMLFiddelersAAAvan der KuyPHMPharmacokinetics, analgesic effect, and tolerability of a single preprocedural dose of intranasal fentanyl in patients undergoing drain removal after breast reduction or augmentation surgery: a prospective, randomized, double-blind, placebo-controlled studyClin Ther2010321427143620678689
- PaechMJLimCBBanksSLA new formulation of nasal fentanyl spray for postoperative analgesia: a pilot studyAnaesthesia20035874074412859464
- GrapeSSchugSALauerSSchugBSFormulations of fentanyl for the management of painDrugs201070577220030425
- PanagiotouIMystakidouKIntranasal fentanyl: from pharmacokinetics and bioavailability to current treatment applicationsExpert Rev Anticancer Ther2010101009102120645689
- ChristrupLLFosterDPopperLDPharmacokinetics, efficacy, and tolerability of fentanyl following intranasal versus intravenous administration in adults undergoing third-molar extraction: a randomized, double-blind, double-dummy, two-way, crossover studyClin Ther20083046948118405786
- FisherAWatlingMSmithAKnightAPharmacokinetic comparisons of three nasal fentanyl formulations; pectin, chitosan and chitosan-poloxamer 188Int J Clin Pharmacol Ther20104813820137766
- PrommerEThe role of fentanyl in cancer-related painJ Palliat Med20091294795419807240
- PortenoyRKHagenNABreakthrough pain: definition, prevalence and characteristicsPain1990412732811697056
- ColuzziPHSchwartzbergLBreakthrough cancer pain: a randomized trial comparing oral transmucosal fentanyl citrate (OTFC) and morphine sulfate immediate release (MSIR)Pain20019112313011240084
- PortenoyRKTaylorDMessinaJTremmelLA randomized, placebo-controlled study of fentanyl buccal tablet for breakthrough pain in opioid-treated patients with cancerClin J Pain20062280517057563
- KressHGOronskaAKaczmarekZEfficacy and tolerability of intranasal fentanyl spray 50 to 200 [mu] g for breakthrough pain in patients with cancer: a phase III, multinational, randomized, double-blind, placebo-controlled, crossover trial with a 10-month, open-label extension treatment periodClin Ther2009311177119119695386
- TaylorDGalanVWeinsteinSMFentanyl pectin nasal spray in breakthrough cancer painJ Support Oncol2010818420822038
- PortenoyRKRaffaeliWTorresLMLong-term safety, tolerability, and consistency of effect of fentanyl pectin nasal spray for breakthrough cancer pain in opioid-tolerant patientsJ Opioid Manag2010631921046929
- MercadanteSRadbruchLDaviesAA comparison of intranasal fentanyl spray with oral transmucosal fentanyl citrate for the treatment of breakthrough cancer pain: an open-label, randomised, crossover trialCurr Med Res Opin2009252805281519792837
- StriebelHWOlmannTSpiesCBrummerGPatient-controlled intranasal analgesia (PCINA) for the management of postoperative pain: a pilot studyJ Clin Anesth19968488695078
- ToussaintSMaidlJSchwagmeierRStriebelHWPatient-controlled intranasal analgesia: effective alternative to intravenous PCA for postoperative pain reliefCan J Anaesth20004729930210764171
- ChristrupLLFosterDPopperLDPharmacokinetics, efficacy, and tolerability of fentanyl following intranasal versus intravenous administration in adults undergoing third-molar extraction: a randomized, double-blind, double-dummy, two-way, crossover studyClin Ther20083046948118405786
- ChengXLiJHEffects of fentanyl administrated nasally and intravenously in post-operative analgesia in pediatric children: a comparative study of 36 casesZhonghua Yi Xue Za Zhi200888289819080094
- GalinkinJLFaziLMCuyRMUse of intranasal fentanyl in children undergoing myringotomy and tube placement during halothane and sevoflurane anesthesiaAnesthesiology200093137811149429
- FinkelJCCohenITHannallahRSThe effect of intranasal fentanyl on the emergence characteristics after sevoflurane anesthesia in children undergoing surgery for bilateral myringotomy tube placementAnaesth Analg2001921164
- VoronovPTobinMJBillingsKPostoperative pain relief in infants undergoing myringotomy and tube placement: comparison of a novel regional anesthetic block to intranasal fentanylûa pilot analysisPediatric Anesthesia2008181196120119076574
- BorlandMJacobsIKingBO’BrienDA randomized controlled trial comparing intranasal fentanyl to intravenous morphine for managing acute pain in children in the emergency departmentAnn Emerg Med20074933534017067720
- BorlandMLBergesioRPascoeEMIntranasal fentanyl is an equivalent analgesic to oral morphine in paediatric burns patients for dressing changes: a randomised double blind crossover studyBurns20053183183716005154
- ZeppetellaGO’DohertyCACollinsSPrevalence and characteristics of breakthrough pain in cancer patients admitted to a hospiceJ Pain Symptom Manage200020879210989246
- SitteTBauseweinCIntranasal fentanyl for episodic breathlessnessJ Pain Symptom Manage.200836e318954962