Abstract
Objectives
Patient adherence and persistence is important to improve outcomes in chronic conditions, including inflammatory and immunologic (I&I) diseases. Patient programs that aim at improving medication adherence or persistence play an essential role in optimizing care. This meta-analysis assessed the effectiveness of patient programs in the therapeutic area of I&I diseases.
Methods
A global systematic literature review was conducted with inclusion criteria of: patient programs in I&I diseases; published in English language between January 2008 and September 2013; and reporting measures of adherence or persistence, including medication possession ratio >80% and persistence rate. A meta-analysis was performed using a random effects model. Subgroup analyses based on the type of program was performed whenever feasible.
Results
Of 67 studies reviewed for eligibility, a total of 17 studies qualified for inclusion in the meta-analysis. Overall, patient programs increased adherence (odds ratio [OR]=2.48, 95% confidence interval [CI]=1.68–3.64, P<0.00001) as compared with standard of care. Combination patient programs that used both informational and behavioral strategies were superior in improving adherence (OR=3.68, 95% CI=2.20–6.16, P<0.00001) compared with programs that used only informational (OR=2.16, 95% CI=1.36–3.44, P=0.001) or only behavioral approaches (OR=1.85, 95% CI=1.00–3.45, P=0.05). Additionally, patients were more likely to be persistent (OR=2.26, 95% CI=1.16–4.39, P=0.02) in the intervention group as compared with the control group. Persistence (in days) was significantly (P=0.007) longer, by 42 additional days, in the intervention group than in the control group.
Conclusions
Patient programs can significantly improve adherence as well as persistence in the therapeutic area of I&I diseases. Programs employing a multimodal approach are more effective in improving adherence than programs with informational or behavioral strategies alone. This in turn may improve patient outcomes.
Introduction
Patient adherence and persistence to treatment are important for effective disease management, especially in chronic diseases that may become more severe over time, such as autoimmune and inflammatory conditions. Adherence refers to the act of conforming to recommendations made by the provider with respect to timing, dose, and frequency of administration.Citation1 Persistence is defined as the duration of time from initiation to discontinuation of therapy.Citation1 Significant evidence suggests that nonadherence is highly prevalent in medical careCitation2 and is a rising concern to health care providers and payers because it increases the cost of care and results in poor patient outcomes.Citation3 Patients are nonadherent to treatment due to various self-identified reasons, including fear of side effects; poor memory; inability to pay for medications; concerns about medications, due to little or no education regarding the disease or regimen; and lack of perceived need.Citation4
Inflammatory and immunologic (I&I) diseases share common characteristics in that these disorders are caused by an immune system attack on the body’s own tissues, leading to increased inflammation. Prevalence rates of autoimmune diseases range from five to 500 per 100,000.Citation5 Inflammatory diseases are a significant clinical burden due to the high prevalence and incidence rates and the chronic nature of these conditions. In the USA, over seven million individuals suffer from inflammatory rheumatic diseases, which are the most severe among the inflammatory diseases.Citation6
Adherence and persistence to long-term treatment are commonly required for optimal disease management. However, patient adherence has been shown to be suboptimal in I&I diseases, such as psoriatic and rheumatic diseases, multiple sclerosis (MS), osteoporosis, and inflammatory bowel disease.Citation7–Citation10 Only about 50% of patients adhere to prescribed medications, while 30% of patients with I&I chronic diseases miss at least one dose intentionally or unintentionally.Citation11 Nonadherence rates range from 43% to 72% in inflammatory bowel disease,Citation12 from 14% to 67% in psoriasis,Citation13 and from 30% to 80% in rheumatoid arthritis (RA).Citation14,Citation15 These rates highlight the need to improve adherence in patients who require long-term treatment.
A number of simple and complex programs have been developed to improve medication adherence and persistence, focusing on informational, behavioral, and combined strategies.Citation16 Informational programs focus on increasing patient knowledge of their disease, treatments, and management tools, through educational brochures, group-based discussion sessions,Citation17 and web-based presentations.Citation9,Citation18 Behavioral programs involve individually tailored adherence-focused sessions and nurse-assisted patient support programs.Citation10,Citation19
The effectiveness of these programs in improving adherence and persistence has not been previously assessed using a systematic approach. Therefore, a meta-analysis was undertaken to quantify and compare the impact of informational, behavioral, and combined patient programs on adherence and persistence.
Methods
Search strategy
Studies published between January 2008 and September 2013 were identified using the PubMed database. Key search terms and Medical Subject Headings (MeSH) terms () for I&I (eg, “ankylosing spondylitis”, “psoriasis”, “psoriatic arthritis”, and “rheumatoid arthritis”) and type of adherence and persistence program interventions (eg, “compliance”, “medication adherence”, “behavioral intervention”, and “persistence”) were used to identify relevant studies. Additionally, an internet search targeting adherence and persistence programs was conducted, and conference proceedings in the I&I therapeutic area were searched.
Inclusion criteria included: (1) studies focused on diseases in the I&I therapeutic area; (2) studies reporting adherence or persistence outcomes; (3) patient programs or interventions comparing exposure with a control group; and (4) studies published in the English language. Studies were not limited to any age range. Two researchers screened the titles and abstracts to determine eligibility for full text review; any disagreements were resolved by consensus with a third researcher. All studies that met our inclusion criteria were reviewed via full-text screening.
Data abstraction
Data from selected studies were abstracted, and information was collected on the country of investigation, disease, study design, sample size in the intervention and control arms, program strategy in brief, study follow-up duration, adherence and persistence definitions, and adherence and persistence results.
Statistical analysis
Statistical analysis was performed using Review Manager 5.2. Cochran Q χ2 and I2 statistics were used to assess the heterogeneity among studies. Since included studies varied in the diseases studied, interventions utilized, study population, and other observable and unobservable factors, a random effects model was employed to allow study outcomes to vary assuming a normal distribution among study populations. If adherence or persistence was reported as a binary measure, then the effect of the intervention was measured as an odds ratio (OR); if it was reported as a continuous measure, then the effect was measured as the mean difference between the intervention and the control group. The pooled effect for each grouping of trials was derived from the OR for each separate trial, weighted by the inverse of the variance (1/standard error of the mean [SE]2), and 95% confidence intervals (CIs) were calculated. In studies reporting discontinuation rates, a persistence rate was calculated as 1 – discontinuation rate.Citation20
Subgroup analyses were performed based on the type of strategy implemented in the patient programs (informational, behavioral, or combined). Informational interventions comprised educational materials administered via various means and formats: oral and telephone communication, written materials, audiovisual presentations, and mailed or emailed materials. Behavioral interventions comprised dosing change, dosing recommendations, and treatment reminders given by telephone or email.Citation21,Citation22
Publication bias was evaluated using funnel plots. The overall risk of bias for an individual study was categorized as low, unclear, or high, as per the Cochrane “Risk of bias” assessment tool in Review Manager.Citation23
Results
Study selection
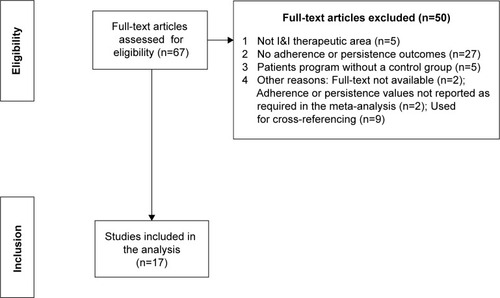
Of the 67 studies that qualified for full-text screening, 17 were included in the meta-analysis.Citation7–Citation9,Citation17–Citation19,Citation24–Citation34 A flow diagram summarizing the study selection and inclusion is reported in .
Study characteristics
lists the characteristics of the 17 studies selected. Among these studies, eight were conducted in an osteoporosis patient population,Citation9,Citation17,Citation24–Citation26,Citation31,Citation33 four in ulcerative colitis (UC),Citation18,Citation19,Citation29,Citation30 two in MS,Citation8,Citation34 and one each in RA,Citation32 childhood-onset systemic lupus erythematosus,Citation28 and RA/psoriasis.Citation7 Of these 17 studies, eight used informational interventions,Citation7,Citation9,Citation17–Citation19,Citation24–Citation26 two used behavioral strategies,Citation27,Citation28 and seven used combined strategies.Citation8,Citation29–Citation34 Nine studies measured only adherence,Citation7,Citation17–Citation19,Citation25,Citation26,Citation28–Citation30 while four studies measured only persistence,Citation8,Citation32–Citation34 and four studies measured both adherence and persistence.Citation9,Citation24,Citation27,Citation31
Table 1 Characteristics of included studies
reports the adherence and persistence data, including their definitions, in the studies. The follow-up period in these studies ranged from 3 to 24 months. The majority of studies used a consistent approach to measure adherence or persistence within the study, except for two studies. Among these two studies, one study by Homer et alCitation7 measured adherence in several ways: patients were asked to record how they took their medications in a dairy; the diaries were checked against pill counts at scheduled monthly follow-up appointments, and pills were counted by investigators. Patients who altered or stopped their medication as a result of contacting the Help line or of medical advice from their general practitioner were considered to be adherent. Another study by Lai et alCitation24 measured adherence by three methods: direct reporting (asking participants how many doses they had missed); pill counts; and self-recording (participants recorded the date on which they took their dose). From both of these studies, only the adherence measures related to pill counts performed by the investigator was used in the meta-analysis.
Table 2 Adherence and persistence outcomes
Effect of patient programs on adherence measure
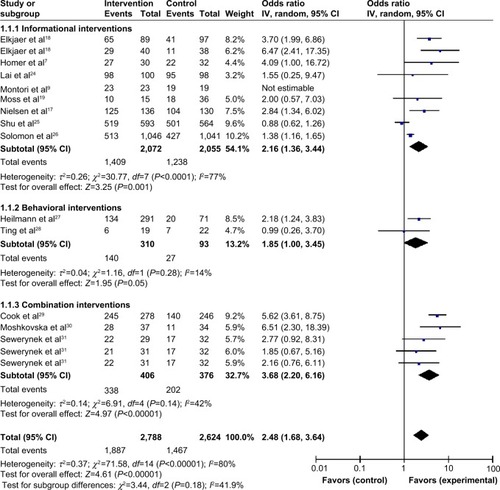
Adherence data (% adherent) were obtained from 13 studies, which were grouped by type of program: informational (n=8); behavioral (n=2); and combined (n=3). Forest plots () were developed in order to compare the ORs from each study. Overall, patient programs increased adherence (OR=2.48, 95% CI=1.68–3.64, P<0.00001) when compared with the control group (standard prescribed care or no intervention). Combination patient programs that used both informational and behavioral strategies were superior in improving adherence (OR=3.68, 95% CI=2.20–6.16, P<0.00001) compared with programs using only informational approaches (OR=2.16, 95% CI=1.36–3.44, P=0.001) or only behavioral approaches (OR=1.85, 95% CI=1.00–3.45, P=0.05). A random effects model was used due to the high level of heterogeneity in the overall analysis (I2=80%).
Figure 2 Program effectiveness on adherence, by type of patient program.
Abbreviations: CI, confidence interval; IV, inverse variance.
Informational patient programs
A total of seven out of eight studies reported higher adherence in the intervention group compared with the control group (). Elkjaer et alCitation18 employed a web-based patient education program to educate UC patients about their disease. Training was provided, and patients could ask their web doctor questions via email or text. During the training, investigators aimed to ensure that each patient understood the web-based training and education, could recognize a relapse, and was able to start the program-recommended treatment. Homer et alCitation7 used group counseling to improve adherence in patients with RA or psoriasis. Patients were allowed to bring a relative, caregiver, or friend to these sessions. They were shown a presentation of “frequently asked questions”, and individualized advice was provided to each. Lai et alCitation24 distributed a “counseling package” to the participants, which consisted of an explanation of osteoporosis, risk factors, lifestyle modifications, goals of osteoporosis therapy, side effects, and the importance of medication adherence. Verbal counseling was reinforced with an osteoporosis booklet, and pharmacists followed up with participants. Montori et alCitation9 used a decision aid, which was a tailored pictographic that illustrated their 10-year fracture risk estimate, absolute risk reduction with bisphosphonates, side effects, and out-of-pocket costs. The decision aid also showed the absolute risk reduction in fracture risk with alendronate, assuming a treatment-related reduction in overall osteoporotic fracture risk of 40%. Moss et alCitation19 assessed patients enrolled in the Script Assist program (an independent treatment adherence program that provides disease-specific information and promotion of medication adherence to patients). Patients received phone calls at 24 hours, 3 weeks, 7 weeks, 15 weeks, and 23 weeks after enrollment, from nurses who were trained to assess patient risk for noncompliance and to intervene with psychological techniques that could improve medication persistence. Nielsen et alCitation17 conducted a group-based educational program in classes of eight to 12 patients each, lasting 3 to 4 hours a week over 4 weeks, conducted by a multidisciplinary team of physicians, dieticians, physiotherapists, and nurses, which were adjusted according to individual patient backgrounds and needs in order to strengthen competence and empowerment. Additionally, patients were invited to participate in a computerized support program, where patients were contacted once a month for 4 months and asked about pain, quality of life, and physical activity. Solomon et alCitation26 sent out seven informational mailings regarding topics such as exercise, fall prevention, and recommended calcium intake to all the study patients. Additionally, the intervention group received ten motivational interview counseling sessions via telephone with a health educator, where each session had a specific educational topic (discussing medications with physician, calcium and vitamin D supplementation, fall prevention, managing adverse effects of medication, etc) and included a series of open-ended questions to elicit subjects’ attitudes toward medication adherence and to determine barriers to long-term osteoporosis medication use.
Shu et alCitation25 reported lower adherence in the intervention group compared with the control group. In this study, randomly selected primary care physicians and their patients received education about osteoporosis diagnosis and treatment. The primary care physicians also received face-to-face education by trained pharmacists, while patients received letters outlining the importance of osteoporosis, its diagnosis, and appropriate treatment, and automated calls inviting them to undergo bone mineral density testing. The pharmacists had participated in a 1-day training session and several follow-up teleconferences about osteoporosis and the principles of one-to-one physician education. The control group received no education.
Behavioral patient programs
Heilmann et alCitation27 used a pharmacy-based management service, where a clinical pharmacist developed a therapeutic plan for treatment recommendations (bone marrow density screening, initiation of osteoporosis therapy, and calcium and vitamin D supplementation) after reviewing the medical history of patients. This plan was then approved by the primary care provider before implementation with patients. Ting et alCitation28 sent daily text messages to patients three times a week prior to each scheduled follow-up clinic appointment. These texts were individualized for each patient by including the scheduled time of the upcoming clinic appointment. Messages were also sent in cases when patients failed to schedule a follow-up visit. A standardized daily reminder was sent to patients based on the prescription (eg once or twice per day), and also received printed information about the benefits and the side effects of the medication.
Combined patient programs
Studies conducted by Sewerynek et al,Citation31 Cook et al,Citation29 and Moshkovska et alCitation30 evaluated the impact of combined strategies on patient adherence. In the study conducted by Cook et alCitation29 telephone follow-up calls were made to UC patients. Within a day of referral, patients received a call from a trained registered nurse who provided an introduction to the program, a preliminary assessment, and offer of a patient program, based on their concerns and readiness for change, using cognitive-behavioral and motivational interviewing counseling techniques. All patients were given a toll-free number for questions, and the referring health care practitioner received a progress note after each call, with notes on the participant’s adherence level and concerns. Moshkovska et alCitation30 employed a tailored patient preference program in which UC patients were given one-on-one education and motivational sessions to deliver individualized support, motivation, and education. At week 4, a brief follow-up telephone call was made to the patient, and at week 24, a 10-minute reinforcement session was held to stress the importance of adherence to medication, to reassess beliefs regarding medicine-taking, and to discuss practical problems. At the end of the session, patients were offered an educational leaflet and a choice of three practical adherence-enhancing patient programs that included medication reminder charts, visual medication reminders for refrigerators and bedside cabinets, daily or weekly electronic pill box organizers with alarms, and a mobile telephone alarm setup.
Sewerynek et alCitation31 randomized patients into four groups, receiving: patient counseling; biochemical information; nurse assistance; or no intervention (control). In the nurse assisted group, a follow-up phone contact was made after 3 and 9 months of treatment, to improve monitoring. In the counseled group, patients were educated and interviewed for 30 minutes about osteoporosis, diagnostic methods, treatment, and preventative behavior. In the biochemical group, patients were educated about serum levels of calcium, phosphorus, alkaline phosphatase, and of urinary calcium and phosphorus concentration levels and diurnal excretion rates.
Effect of patient programs on persistence
Persistence in studies was measured as either percent of patients who were persistent or number of days persistent; the former was a dichotomous variable, while the latter was a continuous variable. As shown in , patients were more likely to be persistent (OR=2.26, 95% CI=1.16–4.39, P=0.02) in the intervention group compared with the control group. A subgroup analysis was not feasible due to the small number of studies reporting persistence. A random effects model was used to adjust for the presence of heterogeneity (I2=86%).
Figure 3 Program effectiveness measured as % persistence.
Abbreviations: CI, confidence interval; IV, inverse variance.
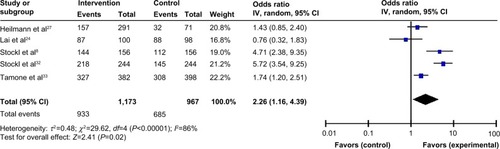
Five studies measured persistence in terms of percent of patients persistent over follow up. Stockl et alCitation8 studied MS patients in a disease therapy management (DTM) program, who received telephone consultations, mailed care plans, and educational materials, based on a predefined schedule for level of intensity of the program (regular-intensity versus high-intensity). In another study by Stockl et al patients with RA were enrolled in a DTM program in which they were given a brochure detailing medication ordering and storage, monitoring, proper disposal of ancillary supplies, mail service medication delivery, refill reminders by patient care coordinators, and access to a pharmacist 24 hours a day, 7 days a week.Citation32 The program used a patient-centric approach providing education and support, to assist patients in developing self-management skills for symptom and treatment management. Each patient was assigned a clinician for the entirety of the program and received telephone consultations (licensed pharmacist or registered nurse) providing education on the medical condition and treatment options, and promoting medication adherence. Tamone et alCitation33 implemented an educational telephone program. At the beginning of treatment, nurses trained patients on self-injection, then, every 2 months, nurses gave new drug pens to the patients; this guaranteed the surveillance of compliance. Nurses called patients to help resolve any issues, schedule the next visit, and, if applicable, collect adverse events information, dates, and reasons for treatment discontinuation.
In a small number of studies, persistence was also reported as number of days persistent (). When measured as persistent days, persistence was significantly longer, by 41.96 additional days (P=0.007), in the intervention group than in the control group.
Figure 4 Effect of intervention vs control on persistence (in days) in I&I.
Abbreviations: CI, confidence interval; I&I, inflammatory and immunologic; SD, standard deviation; IV, inverse variance.
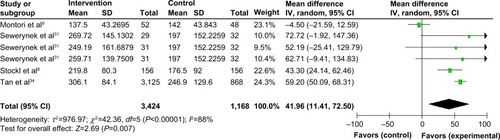
As described above, Montori et alCitation9 employed a pictographic decision aid; Sewerynek et alCitation31 employed three intervention groups in which patients received either nurse assistance, information about their biochemical charts, or counseling; and the study by Stockl et alCitation8 of (MS), utilized a DTM program. Tan et alCitation34 provided a specialty care management program service, including mail order medications, disease-specific patient education materials, refill reminder calls, and assessment calls by nurses at the beginning of the program and at months 3, 6, and 12, and every 12 months thereafter.
Risk of bias in the reviewed studies
The common types of biases evaluated in this analysis were selection bias, performance bias, detection bias, attrition bias, reporting bias, and other biases inherent in interventional study designs. Selection bias was determined if patients were not assigned to an intervention or control group using random sequence generation and if the allocation of participants were not concealed. Performance bias referred to the lack of blinding of participants and personnel – blinding ensures that the control group receives similar attention, treatment, and diagnostic investigations as the intervention group. Detection bias referred to blinding of investigators, which reduces confounding related to the knowledge of intervention assignment. Reporting bias is often related to selective reporting of study measures (publications more often report statistically significant differences than nonsignificant differences, leading to reporting bias), while attrition bias is due to incomplete outcomes data, due to omission of some participants from the reports of analyses. Other biases included bias due to study designs, and inclusion and exclusion of patients.
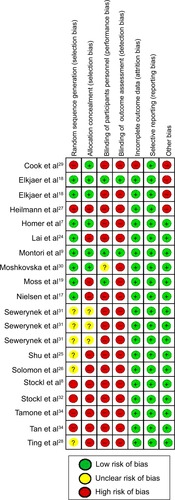
As depicted in , sixCitation8,Citation27,Citation29,Citation32–Citation34 out of the 17 studies did not perform random sequence generation, and elevenCitation8,Citation17,Citation19,Citation24–Citation28,Citation32–Citation34 did not conceal the allocation of participants, resulting in selection bias. Although blinding of participants and personnel, as well as that of outcomes assessed in the study, is not usually possible in patient programs, it was addressed by two studies.Citation9,Citation18 There was no attrition or reporting bias in the selected studies. However, other types of biases related to study designs were observed in three studies.
Among these studies, Cook et alCitation29 divided the intervention population into two groups: with high risk and low risk. However, the results were aggregated for the two groups and were not presented separately for the high- and low-risk patients. The study by Elkjaer et alCitation18 only selected patients who suffered from mild to moderate UC; those with severe UC were not included, and yet, they are an important target population for adherence. Participants in the study conducted by Heilmann et alCitation27 required continuous enrollment in their health plan (no membership gaps greater than 45 days), therefore, members who did not have continuous membership were not included in the study.
Discussion
Key findings
Though various patient programs have been developed with the goal of improving adherence and persistence, little has been published on the overall effectiveness of these programs in the therapeutic area of I&I diseases. The results of this meta-analysis show that patient programs incorporating combined strategies (informational and behavioral techniques together) were more likely to improve adherence compared with informational or behavioral strategies alone.
Among the combination patient programs, two out of three studies significantly increased adherence, using cognitive-behavioral and motivational interview counseling over the telephone and tailoring the program as per patient preference to include individualized education, support sessions, and problem solving.Citation29,Citation30 Patient counseling and motivational sessions formed a major part of all combination patient programs, suggesting that a greater degree of communication may have existed between patients and health care practitioners in these instances. Combined strategies also focused on providing education about the disease and treatment. Therefore, behavior modification as well disease knowledge was targeted to improve adherence.
Among the eight informational patient programs, three significantly increased adherence in the intervention group as compared with the control group. These programs included strategies for web-based patient education, group counseling, and group-based education.Citation7,Citation17,Citation18 We found that patient education and counseling, more so in a group-based setting, can be an effective strategy to enhance adherence. One study reported lower adherence in the intervention group as compared with the control group.Citation25 This intervention focused on physicians more than patients and suggested that adherence programs might be more effective when they are patient-centric. In the study, researchers suspected that their inability to observe a difference in adherence was due to a high rate of baseline adherence in the control group, and the 10-month follow-up period. In the study by Homer et alCitation7 reports by the participants – the use of diary and self-reports of pill count – were used, which may lead to biases. Hence, the pill count data recorded by the health care professional, considered to be unbiased, was used for the meta-analysis.
Behavioral techniques suggest a positive impact on adherence benefits when data were pooled, though our finding is based on only two studies. Of the two studies, Ting et alCitation28 did not show a positive benefit; however, the study included a small sample size, of 19 patients in the intervention group and 22 patients in the control group. In contrast, Heilmann et alCitation27 did show a significant improvement in adherence, and the study was weighted more heavily due to the much larger sample size (N=362). The strategy included pharmacy-based management services that provided recommendations on screening and medication. Also, Heilmann et alCitation27 followed patients for 6 months, while Ting et alCitation28 followed their patients for 12 months. The longer follow-up period may have influenced level of adherence. There was also a major difference in the patient population, with the study by Heilmann et alCitation27 consisting of elderly and potentially more severe patients. Heilmann et alCitation27 studied women patients suffering from osteoporosis, aged 67 years or older, while Ting et alCitation28 included patients with childhood-onset systemic lupus erythematosus, aged between 13 and 25 years, with unlimited access to cellular text messaging.
Persistence could be enhanced significantly by DTM programs, self-injection training, disease and treatment education over the telephone, and specialty care management. DTM, as well as specialty care management programs, involve a combination of services, such as consultation, care plans, educational material mailings, reminders, mail-service medication delivery, access to the pharmacist, and thorough follow-up.Citation8,Citation32–Citation34 Hence, they prove to be exhaustive programs that can improve persistence.
Overall, programs that empower patients, through counseling, education, reminders, and support, improve adherence and persistence. Additionally, active participation of pharmacists, registered nurses, and primary care physicians can further enhance adherence. Follow up is an important part of patient programs as it gives patients a chance to ask questions and resolve any issues. A systematic review conducted by Haynes et alCitation21 confirms our findings and reported that patient programs that consisted of both informational and behavioral techniques, such as counseling, reminders, reinforcement, and individualized plans, commonly improved patient adherence. However, the review by Haynes et alCitation21 only included randomized controlled trials and made no attempt to pool data to evaluate the effectiveness of these programs in a meta-analysis.
Strengths and limitations of the study
This meta-analysis adds to the current body of evidence by assessing the effectiveness of programs on adherence and persistence outcomes in diseases that require long-term management. One of the strengths of this study is the comprehensive, structured, and systematic approach undertaken to search the literature and conference proceedings to identify all studies that assessed adherence-focused patient programs. Furthermore, to our knowledge, this is the first meta-analysis in the therapeutic area of I&I diseases to study the effect of such programs, based on the type of the patient program used.
Although this review provides a comprehensive understanding of the effect of patient programs on adherence and persistence, some limitations should be considered when interpreting our findings. Although osteoporosis has not been categorized as an I&I disease, emerging molecular and clinical evidence highlights that inflammation exerts significant influence on bone turnover, which induces osteoporosis.Citation35 Transplantation was not included in this analysis, due to the unique clinical and treatment characteristics in the transplant population, which may not be generalizable and comparable to populations with chronic I&I disease. A limitation inherent in meta-analyses is that we could not control for potential confounding variables such as age, socioeconomic level, education level, disease severity, and comorbidities. Also, studies that reported persistence as a medication possession ratio were not included in the meta-analysis. However, excluding these studies did not likely bias our finding for an overall benefit because these studies reported a significant increase in the medication possession ratio in the intervention group compared with the control group. Additionally, a number of studies focused on a specific population segment, for example, patients with internet access or unlimited access to cellular text messaging, and results may not be generalizable to the general population. Although these patient programs were associated with improvements in adherence and persistence, it is worth noting that they were conducted in controlled settings. The actual effect of such complex patient programs on patients may be different in real-world clinical practice.
Overall, we found that patient programs can significantly improve adherence as well as persistence, in I&I diseases. Programs employing a multimodal approach seem to be the most effective, given that they address multiple aspects of treatment management; however, informational or behavioral strategies alone also appear to be beneficial by themselves. Supporting and implementing similar patient programs may in turn improve patient outcomes in those with chronic I&I disease.
Supplementary material
Table S1 Search terms
Disclosure
Market Access Solutions, LLC, a consulting company, received funding from Celgene Corporation to conduct the research, analysis, and develop the manuscript. Zeba M Khan and Satyin Kaura are employees of Celgene Corporation. Chakkarin Burudpakdee was formerly employed by Market Access Solutions, LLC, and is currently a Principal at IMS Health. Smeet Gala and Merena Nanavaty are employed at Market Access Solutions, LLC. The authors report no other conflicts of interest.
References
- CramerJARoyABurrellAMedication compliance and persistence: terminology and definitionsValue Health2008111444718237359
- FischerMAStedmanMRLiiJPrimary medication non-adherence: analysis of 195,930 electronic prescriptionsJ Gen Intern Med201025428429020131023
- HoPMBrysonCLRumsfeldJSMedication adherence: its importance in cardiovascular outcomesCirculation2009119233028303519528344
- McHorneyCASpainCVFrequency of and reasons for medication non-fulfillment and non-persistence among American adults with chronic disease in 2008Health Expect201114330732020860775
- CooperGSStroehlaBCThe epidemiology of autoimmune diseasesAutoimmun Rev20032311912512848952
- HelmickCGFelsonDTLawrenceRCNational Arthritis Data WorkgroupEstimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part IArthritis Rheum2008581152518163481
- HomerDNightingalePJobanputraPProviding patients with information about disease-modifying anti-rheumatic drugs: Individually or in groups? A pilot randomized controlled trial comparing adherence and satisfactionMusculoskeletal Care200972789218792423
- StocklKMShinJSGongSHaradaASSolowBKLewHCImproving patient self-management of multiple sclerosis through a disease therapy management programAm J Manag Care201016213914420148619
- MontoriVMShahNDPencilleLJUse of a decision aid to improve treatment decisions in osteoporosis: the osteoporosis choice randomized trialAm J Med2011124654955621605732
- HommelKAHerzerMIngerskiLMHenteEDensonLAIndividually tailored treatment of medication nonadherenceJ Pediatr Gastroenterol Nutr201153443543921519282
- BarberNParsonsJCliffordSDarracottRHorneRPatients’ problems with new medication for chronic conditionsQual Saf Health Care200413317217515175485
- HawthorneABRubinGGhoshSReview article: medication non-adherence in ulcerative colitis – strategies to improve adherence with mesalazine and other maintenance therapiesAliment Pharmacol Ther200827121157116618384664
- ThorneloeRJBundyCGriffithsCEAshcroftDMCordingleyLAdherence to medication in patients with psoriasis: a systematic literature reviewBr J Dermatol20131681203122963128
- van den BemtBJZwikkerHEvan den EndeCHMedication adherence in patients with rheumatoid arthritis: a critical appraisal of the existing literatureExpert Rev Clin Immunol20128433735122607180
- BartonJLCriswellLAKaiserRChenYHSchillingerDSystematic review and metaanalysis of patient self-report versus trained assessor joint counts in rheumatoid arthritisJ Rheumatol200936122635264119918045
- KripalaniSYaoXHaynesRBInterventions to enhance medication adherence in chronic medical conditions: a systematic reviewArch Intern Med2007167654055017389285
- NielsenDRygJNielsenWKnoldBNissenNBrixenKPatient education in groups increases knowledge of osteoporosis and adherence to treatment: a two-year randomized controlled trialPatient Educ Couns201081215516020400258
- ElkjaerMShuhaibarMBurischJE-health empowers patients with ulcerative colitis: a randomised controlled trial of the web-guided ‘Constant-care’ approachGut201059121652166121071584
- MossACChaudharyNTukeyMImpact of a patient-support program on mesalamine adherence in patients with ulcerative colitis – a prospective studyJ Crohns Colitis20104217117521122501
- KothawalaPBadamgaravERyuSMillerRMHalbertRJSystematic review and meta-analysis of real-world adherence to drug therapy for osteoporosisMayo Clin Proc200782121493150118053457
- HaynesRBMcKibbonKAKananiRSystematic review of randomised trials of interventions to assist patients to follow prescriptions for medicationsLancet199634890243833868709739
- PetersonAMTakiyaLFinleyRMeta-analysis of trials of interventions to improve medication adherenceAm J Health Syst Pharm200360765766512701547
- HigginsJPTGreenSCochrane handbook for systematic reviews of interventions. Version 5.1.0The Cochrane Collaboration2011 [updated March 2011]. Available from: www.cochrane-handbook.orgAccessed December 24, 2014
- LaiPChuaSSChanSPA systematic review of interventions by healthcare professionals on community-dwelling postmenopausal women with osteoporosisOsteoporos Int201021101637165620379700
- ShuADStedmanMRPolinskiJMAdherence to osteoporosis medications after patient and physician brief education: post hoc analysis of a randomized controlled trialAm J Manag Care200915741742419589009
- SolomonDHIversenMDAvornJOsteoporosis telephonic intervention to improve medication regimen adherence: a large, pragmatic, randomized controlled trialArch Intern Med2012172647748322371876
- HeilmannRMFrieslebenCRBillupsSJImpact of a pharmacist-directed intervention in postmenopausal women after fractureAm J Health Syst Pharm201269650450922382482
- TingTVKudalkarDNelsonSUsefulness of cellular text messaging for improving adherence among adolescents and young adults with systemic lupus erythematosusJ Rheumatol201239117417922089460
- CookPFEmiliozziSEl-HajjDMcCabeMMTelephone nurse counseling for medication adherence in ulcerative colitis: a preliminary studyPatient Educ Couns201081218218620079598
- MoshkovskaTStoneMASmithRMBankartJBakerRMayberryJFImpact of a tailored patient preference intervention in adherence to 5-aminosalicylic acid medication in ulcerative colitis: results from an exploratory randomized controlled trialInflamm Bowel Dis20111791874188121830265
- SewerynekEHorst-SikorskaHStępień-KłosWThe role of counselling and other factors in compliance of postmenopausal osteoporotic patients to alendronate 70 therapyArch Med Sci20139228829623671440
- StocklKMShinJSLewHCOutcomes of a rheumatoid arthritis disease therapy management program focusing on medication adherenceJ Manag Care Pharm201016859360420866164
- TamoneCFonteGPanicoAMolinattiPAD’AmelioPIsaiaGCImpact of a phone follow-up program on persistence with teriparatide or PTH(1–84) treatmentCalcif Tissue Int201290427227822322409
- TanHYuJTabbyDDevriesASingerJClinical and economic impact of a specialty care management program among patients with multiple sclerosis: a cohort studyMult Scler201016895696320595246
- GinaldiLDi BenedettoMCDe MartinisMOsteoporosis, inflammation and ageingImmun Ageing2005211416271143