Abstract
Purpose
To explore the feasibility of a research-based program for patient-centered consultations to improve medical adherence and blood glucose control in patients with type 2 diabetes.
Patients and methods
The patient-centered empowerment, motivation, and medical adherence (EMMA) consultation program consisted of three individual consultations and one phone call with a single health care professional (HCP). Nineteen patients with type 2 diabetes completed the feasibility study. Feasibility was assessed by a questionnaire-based interview with patients 2 months after the final consultation and interviews with HCPs. Patient participation was measured by 10-second event coding based on digital recordings and observations of the consultations.
Results
HCPs reported that EMMA supported patient-centered consultations by facilitating dialogue, reflection, and patient activity. Patients reported that they experienced valuable learning during the consultations, felt understood, and listened to and felt a trusting relationship with HCPs. Consultations became more person-specific, which helped patients and HCPs to discover inadequate diabetes self-management through shared decision-making. Compared with routine consultations, HCPs talked less and patients talked more. Seven of ten dialogue tools were used by all patients. It was difficult to complete the EMMA consultations within the scheduled time.
Conclusion
The EMMA program was feasible, usable, and acceptable to patients and HCPs. The use of tools elicited patients’ perspectives and facilitated patient participation and shared decision-making.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
The management of type 2 diabetes mellitus (T2DM) comprises several elements, such as poly-pharmacy including insulin administration, self-monitoring of blood glucose, diet, and physical exercise to prevent or postpone long-term complications.Citation1 The adherence to prescribed therapies is an important but often neglected issue in the management of T2DM.Citation2 It is estimated that 20%–50% of patients with chronic conditions such as diabetes are not adherent to their prescribed medication regimen, with non-adherence being defined as <80% adherence to relevant prescribed medication.Citation3,Citation4
However, adherence is not just a matter of taking medication; it requires lifestyle changes, knowledge and competence, and internal motivation for self-management. Accordingly, the recommended approach to diabetes management has recently shifted from an emphasis on standardized measures of adherence to an individualized, patient-centered approach.Citation1 A patient-centered approach is defined as:
Providing care that is respectful of and responsive to individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions (p. 8).Citation5
However, little guidance is provided as to how health care professionals (HCPs) should accomplish this in a clinical setting.Citation6
Studies indicate that patient–provider collaboration can be enhanced by HCP use of educational material and communication skills training and patient use of notes about their concerns that provide specific information about disease and attention to emotion.Citation7,Citation8 It is also suggested that decision aids or tools that help to involve patients in shared decision-making may facilitate patient-centered care.Citation9,Citation10
We developed a patient-centered consultation program based on dialogue tools – EMMA (for empowerment, motivation, and medical adherence). It aims to support medication adherence and blood glucose control by facilitating rapport, exploring patient concerns and challenges, enabling knowledge exchange, and supporting goal setting and action planning. EMMA’s effect on glycemic control is reported elsewhere.Citation11 We report here the results from a feasibility study investigating the perspectives of patients and HCPs.
Theoretical framework
The theoretical framework for the EMMA program builds on three key concepts: empowerment, motivation, and medical adherence.
Empowerment
The EMMA program is based on the empowerment philosophy, an alternative to the pathogenic paradigm.Citation12 Funnell et al have defined the process of empowerment as:
[…] the discovery and development of one’s inborn capacity to be responsible for one’s own life. People are empowered when they have sufficient knowledge to make rational decisions, sufficient control and resources to implement their decisions, and sufficient experience to evaluate the effectiveness of their decisions.Citation12
Empowerment is a patient-centered collaborative approach tailored to match the fundamental realities of diabetes care. The aim of the EMMA program is to facilitate a process supporting patients’ abilities to think critically about the way they live with T2DM and to act autonomously. EMMA is intended to help patients make informed choices about how their lives should be organized with the best possible self-management.Citation13
Motivation
Motivation is the driving force underlying the wish to change behavior. Inner motivation is driven by one’s needs, values, and feelings, whereas external motivation is driven by other people, material goods, penalties, or benefits. People are more likely to work toward goals they set for themselves if behavioral change is driven by inner motivation. EMMA provides tools intended to facilitate inner motivation and focus on identifying patients’ individual needs, values, and feelings. Patients have the experience of making choices, using available information to make decisions according to self-selected goals.Citation14
Medical adherence
Medical adherence has largely replaced the passive notion of compliance and is defined as:
The extent to which a person’s behavior – taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a healthcare provider.Citation15
EMMA aims to improve adherence by providing support for concordance in practice and by boosting patients’ experiences of the comprehensibility, meaningfulness, and manageability of treatment. The term concordance relates to a consultation process in which prescribing is based on shared decision-making between patient and HCP.Citation16 Concordance is defined as:
Agreement between the patient and health care professional, reached after negotiation that respects the beliefs and wishes of the patient in determining whether, when and how their medicines is taken, and (in which) the primacy of the patient’s decision (is recognized).Citation17
Patients and methods
Developing the program
This study was approved by the Danish Data Protection Board and ethics committee, and participant consent was obtained. The program was developed using an action research methodology. A collective learning and development process in cooperation between theory and practice was performed from February 2011 to August 2011.Citation18 Two health education scientists with backgrounds in user-driven innovation and drug management (GE and AV) and two physicians (GA and FP) and a diabetes nurse (LJ) from a specialist diabetes clinic in Denmark participated. The health education scientists were the primary developers of EMMA, but results were discussed and elaborated in the entire group. The process involved multiple workshops using methods such as ideation, prototype development, and role playing. To facilitate patient participation during consultations, dialogue tools were designed to explore specific challenges for medication adherence, perform medical review,Citation19 and facilitate interactive learning and goal-setting and action-planning processes. The dialogue tools included visual and tangible materials such as pictures, peer quotes, questions, illustrations, and worksheets. The idea of using dialogue tools during consultations was inspired by the methodology of cultural probes that encourage participants to reflect, engage in dialogue, and verbalize their experiences and to encompass a variety of patient learning preferences.Citation20,Citation21 The theoretical building blocks of the EMMA program can be explained as consisting of the why, the what, and the how as shown in . The overall theoretical framework of EMMA builds on empowerment, motivation, and medical adherence and explains why the EMMA program is important. To operationalize these concepts into a concrete consultation-based program, the “five-step empowerment model of goal setting”Citation22 formed the basis for the structure of the EMMA program. This involved a step-by-step process encompassing problem identification, problem elucidation, goal setting and exploration, action planning, and finally follow-up describing what steps the EMMA program consists of. And finally, in order to describe how the patient-centered consultations should play out in practice, selected theories, models, and methods relevant for health behavioral change were applied in developing dialogue tools for each step.Citation23 The dialogue tools thus apply elements from different methods, models, and theories such as the WHO model of five dimensions of adherence,Citation15 the health belief model,Citation24,Citation25 the transtheoretical model of change,Citation26 self-efficacy theory,Citation27 narratives,Citation28 and motivational interviewing.Citation29 The development of dialogue tools was also inspired by education material from the DESMOND Programme (eg, discussing blood glucose management by inviting the patient to point out their own level of blood glucose on a continuum) and by the Danish Diabetes Association (eg, illustrating the pathophysiology of diabetes on a human-like figure with the use of icons).Citation30,Citation31 Furthermore, one tool (“My Challenges”) applies the WHO model of five dimensions of adherence. lists the flow of the program including theme and purpose of the included tools. A full description of the entire program and all tools with regard to methodology, anticipated mode of action, and intended outcome is available elsewhere.Citation32 One patient pre-tested and provided feedback on the content and format of the first consultation prior to the initiation of the feasibility study.
Figure 1 “The why”, “the what”, and “the how” of the EMMA program. The overall theoretical framework describes why the EMMA program is important, the five-step empowerment model describes what steps the EMMA program consists of, and the selected techniques, models, and theories describe how the EMMA approach is operationalized into specific dialogue tools.
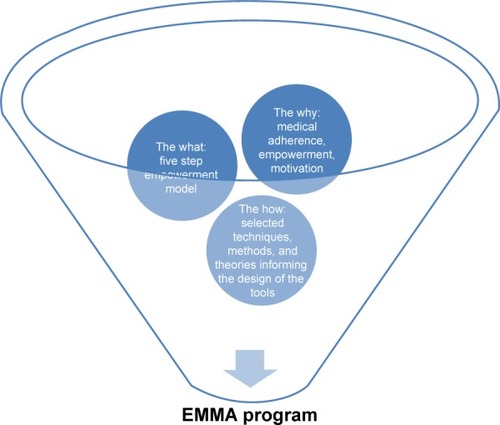
Table 1 Flow of program content and tools across sessions
The EMMA program
The program consisted of a process of three one-to-one consultations with the same HCP (nurse or physician) to ensure continuity. Approximately 4 weeks elapsed between the first and second consultations, and 6 weeks elapsed between the second and third consultations. A follow-up phone call was conducted between the second and the third consultation. The first two consultations were scheduled to last 45 minutes; the third lasted 30 minutes.
The main focus of the program is to explore and resolve challenges patients may have with implementing prescribed medication and in obtaining good glycemic control.
Study sample
Twenty-two Danish-speaking adult patients at a Danish specialist diabetes clinic accepted the invitation to participate in the feasibility study. They were 49–85 years of age, had T2DM, glycosylated hemoglobin A1c of ≥64 mmol/mol (8.0%), and medication possession rate of ≤80%.Citation10 Sixteen were male.
One diabetes nurse (8 years of experience) and one physician (3 years of experience) who had participated in the development and training process of the EMMA program conducted the consultations, assisted by comprehensive step-by-step guidelines outlining the purpose and process of each tool.Citation32
Data collection
Data were collected between June 2011 and September 2012.
Feasibility of EMMA
The methods for assessing feasibility were inspired by Bowen et al’s work and we focused on the acceptability, practicality, and implementation of the program.Citation33 Data collection to assess the feasibility of the EMMA program was guided by the elements in (eg, the implementation of tools, the experience of patients and HCPs of the consultation process). The following data collection methods were used: materials from consultations, interviews with patients based on questionnaires, interviews with HCPs, and 10-second event coding as described in sections Materials from consultations, Interviews with patients based on questionnaires, Interviews with HCPs, and Ten-second event coding.
Table 2 Key areas of focus for the feasibility study of the EMMA program related to acceptability, practicality, and implementation
Materials from consultations
The tools used in the consultations were given to the patients after each consultation and a copy of the material was kept by HCPs.
Interviews with patients based on questionnaires
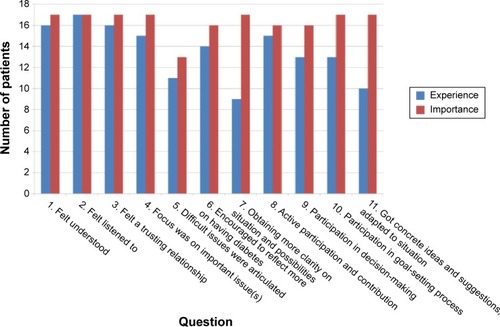
Two months after their last consultation, patients completed a questionnaire as part of face-to-face interviews using a semi-structured interview guide. The purpose was to investigate patients’ experience and appraisal of the consultation process and outcomes (). The two health education scientists constructed the questionnaire in accordance with the theoretical foundation of the program, building on elements from the five-step empowerment model, and the concordance-facilitating strategy.Citation15,Citation21 The questionnaires used four-point Likert scales ranging from “very important” to “not important” or from “to a very large extent” to “to a small extent”. An example question was “Did you get relevant support in regard to living with diabetes?”. Two patients filled in the questionnaires immediately after their last session to guide the development of the final questionnaire.
Interviews with HCPs
The nurse and the physician were interviewed 7 months after completing their first consultation. In the interviews, we explored the acceptability, practicality, and implementation of the program from the HCPs’ point of view and probed specifically about the challenges and barriers experienced to inform the development and refinement of the program (). Interviews included open-ended questions about how they experienced the different tools and how they felt supported in terms of exploring patients’ challenges, knowledge sharing, and shared goal setting and decision-making. They were also asked how many times they had to use the tools before they felt confident in using them. The two interviews lasted 69 and 51 minutes and were digitally recorded.
Ten-second event coding
A researcher was present during consultations to assess patient participation using 10-second event coding to measure the ratio of patient and HCP talk.Citation34 We perceive the talk ratio to be indicative of the feasibility of the program as one of several indicators for patient-centered patient education.Citation35 Every 10 seconds, the researcher noted whether the patient or the HCP was talking or if silence was occurring.
Routine consultations in January 2013 with 21 patients with T2DM (hemoglobin A1c ≥64 mmol/mol [8%]) were digitally recorded and assessed by 10-second event coding to serve as controls. Consultations lasted an average of 27 minutes (range: 11–47 minutes) and were conducted by HCPs who did not participate in EMMA.
Data analysis
Implementation of tools in consultations and examples of output
Tool implementation and examples of patient output were analyzed by inspecting the copied dialogue tools and examining the recordings of consultations.
Analysis of questionnaires
We assessed patient-reported experiences of selected parameters of consultations in relation to their rating of the importance of those parameters, comparing the number of patients reporting they experienced a parameter to a large or very large extent with the number of patients rating it as very important or important. Achieved competencies were assessed by patients. The extent to which they followed the goal and plan 2 months after their final session was calculated as the number of patients who responded “to a very large” or “to a large extent” and the number of patients who responded “to some extent” or “to a small extent”.
Insights from the interviews with HCPs
Interviews were analyzed in accordance with the key elements in (eg, whether HCPs felt at ease using the tools and whether they felt supported in goal-setting processes) to gain insight into the feasibility and usability of the specific tools and the entire program from the perspective of the HCPs.
Analysis of 10-second event coding
For each consultation, the ratio between patient talk and HCP talk was calculated as the number of coded events representing patient or HCP talk divided by the total number of events representing patient and HCP talk. For periods during EMMA consultations in which specific dialogue tools were used, talk ratios were calculated as the number of coded events representing patient or HCP talk divided by the number of all coded events (HCP and patient talk and silence). These calculations also include silent time ratios. The statistical significance of differences in average talk ratios in EMMA and control consultations was calculated using Student’s t-test (SAS 9.2).
Results
Study sample and duration of sessions
Nineteen patients finished the program. In all, three patients dropped out of EMMA due to severe illness (n=2) and referral to a lifestyle clinic (n=1). The mean age of patients completing the program was 68.3 years; 13 were men. The average duration of the first, second, and third consultations was 49 minutes (range: 37.7–77.3), 64 minutes (42.5–106.9), and 34 minutes (23.0–59.9), respectively, with a trend toward shorter consultations as the study progressed and HCPs gained more experience using the tools.
Use of tools
The content of the EMMA program was conducted as planned. The dialogue tools were implemented throughout the consultations and seven out of ten tools were used by all patients. The results and example outcomes are presented in .
Table 3 Overview of dialogue tool use
Patient experiences
The majority of participants felt understood and listened to and felt a trusting relationship (16 (94%), 17 (100%), and 16 (94%) participants, respectively), and they also rated these parameters highly in terms of importance (). Fourteen (82%) participants reported that they felt encouraged to reflect more on having diabetes, nine (53%) reported that they achieved more clarity regarding their situation and possibilities, and eleven (65%) felt that difficult issues were articulated. Feeling encouraged to reflect more on having diabetes and achieving more clarity on their situation and possibilities were also rated as important (by 16 (94%) and 17 (100%), respectively). With regard to the articulation of difficult issues, 13 (76%) participants found it to be important. With respect to participation (questions 8, 9, and 10 in ), one (6%) participant did not report concordance between experience and importance for general participation and contribution. Three (18%) and four (24%) participants expressed inconsistency between their experience and the importance of decision-making and goal-setting processes, respectively.
Almost all participants reported obtaining valuable learning they could use (). However, in terms of more concrete achievements, such as getting ideas and suggestions adapted to their specific situation () and feeling more capable in managing diabetes (), ten (59%) and 12 (63%) patients agreed.
Figure 3 Patient assessment of EMMA intended outcomes (N=19).
Abbreviation: EMMA, empowerment, motivation, and medical adherence.
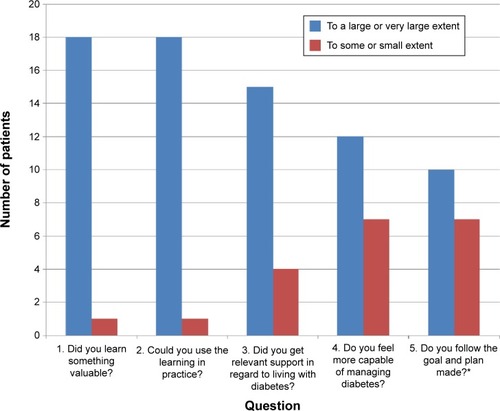
All patients identified a goal (). Two months after their final session, ten (59%) participants stated that they followed the goal and plan to a high or very high extent.
HCP experiences
HCPs felt confident in conducting the first consultation after their initial three patients. One HCP expressed the need for more training to become confident in using the tools for the second consultation.
I needed to get some hands-on experience with the tools and also to see them in use. [quote from HCP]
Furthermore, taking notes in connection to the use of tools was unfamiliar to one HCP, who needed more practice. The HCPs reported that most patients became active participants during the consultation and expressed that, in general, they felt the tools were usable and feasible and ensured a patient-centered approach while guiding the flow of visits.
I feel that I got to know the patients better than what I remember from usual consultations. [quote from HCP]
However, both HCPs expressed concerns about working with the “goal and plan” tool for some patients. One HCP reported that for less motivated patients, the final goal was often defined by the HCP, not by the patient. The other HCP would have liked to be more proficient at challenging patients to engage in the goal-setting process. Generally, HCPs experienced a lack of communication skills that would have allowed them to avoid taking control during consultations with unmotivated patients. Both HCPs found it difficult to complete the consultations within the scheduled time due to the number of tools allocated to each consultation and because the tools were new to the HCPs.
Patient and HCP talk ratios
Talk ratios supplemented qualitative assessments by patients and HCPs. shows the average talk ratios for each of the three EMMA consultations, the total EMMA program, and control consultations. On average, HCPs talked 48% of the total talk time during EMMA consultations, compared with 54% during routine consultations. The average HCP talk ratio for the first, second, and third consultations was 42%, 53%, and 50%, respectively. When talk ratios were examined for specific tools, wide differences were found (data not shown). The HCP talk ratio ranged from 22% for “My Day”, in which patients were invited to talk about a typical day with diabetes to 47% for the goal-setting exercise, and 53% while working with diabetes education tools in the second consultation. The amount of silent time also differed substantially, depending on the amount of writing and reflection related to each tool. The silent time ratio was especially high for the tool “My Challenges” (23%), due to the time spent selecting cards.
Table 4 Average talk ratios
Discussion
In an effort to rethink medical adherence from a patient-centered perspective, we explored the feasibility of a research-based consultation program using dialogue tools to improve medication adherence and blood glucose control in patients with T2DM. Overall, patients and HCPs found the EMMA program to be feasible and usable, and the dialogue tools were highly used in consultations. The HCPs reported that the tools supported patient-centered consultations by facilitating dialogue, reflection, and patient activity. Patients reported that they obtained valuable learning during consultations, felt understood and listened to, and felt a trusting relationship with the HCPs.
To assess the extent to which EMMA facilitated patient-centered consultations, we triangulated data from different sources. One source was the degree of patient talk in the consultations as assessed by 10-second event coding described by Skinner et al.Citation31 We included this assessment as an indicator of patient participation. According to Roter et al, patients generally talk less than do physicians (40% vs 60%), although less HCP talk has been associated with a greater improvement in participants’ knowledge about diabetes.Citation31,Citation34 The average HCP talk ratio during EMMA consultations was 48%, whereas control consultations had an HCP talk ratio of 54% (P=0.059).
Roter et al also point out that reports on the distribution of patient and HCP talk throughout consultations are lacking.Citation34 Consequently, we calculated separate talk ratios for the first, second, and third consultations and for selected tools (). Skinner et al suggested that the maximum standard proportion of educator talk should be 40%–65%, depending on the theme of the session.Citation31 For patient stories, the standard for educator talk is 40%, while the standard for educator talk is 65% for professional stories and 50% for goal setting.Citation31
Overall, the talk ratios of the specific sessions in EMMA are very consistent with targets suggested by Skinner et al. For the first EMMA consultation, in which all tools focus on exploring patients’ challenges and daily life with diabetes and medication, the HCP ratio was 42%, close to Skinner et al’s suggested standard for patient stories. In the second EMMA consultation, consisting of educational exercises with more learning-intensive tools that are comparable to Skinner et al’s professional stories, the HCP talk ratio was 53%. For the goal-setting exercise in the same consultation, the share of HCP talk was 47%, which is close to Skinner et al’s suggested standard of 50%.Citation31
The HCP talk ratio of the first EMMA consultation is significantly lower than the average HCP talk ratio of the control visits and much lower than HCP talk ratios of the second and third EMMA consultations, leading to an average EMMA HCP talk ratio that approaches a statistically significant decrease from the control consultations (0.059). While the control consultations have a rather low HCP talk ratio of 54%, compared with the typical 60% described by Roter et al,Citation34 the EMMA average HCP talk ratio of 48% is even lower. We attribute this, at least in part, to the structured flow facilitated by the tools that provide room for the patient story. However, Skinner et al’s study was based on group sessions and the EMMA program is based on one-to-one consultations; Skinner et al’s suggested targets may not be entirely applicable to our findings. Future research could explore correlations between participation as measured by the talk ratio and both medication adherence and blood glucose control.
However, talk time only indicates who is doing the talking and does not address talk quality or content. Another data source was the assessment of patients’ experience and appraisal of the consultation process and patient-centered outcomes in the questionnaire-based interviews. Almost all patients in EMMA felt a trusting relationship with HCPs. Trust has been suggested as an important determinant in patient–provider communication, and it has been related to an enhanced patient desire to participate.Citation36,Citation37 In EMMA, trust may be promoted by the initial exercise “My Day”, which elicits patients’ perspectives at the beginning of the program. This could relate to patients’ high ratings of feeling understood and listened to and experiencing a focus on issues that were important to them. Although this dialogue tool might seem time consuming, it forms a foundation for later collaboration and shared decision-making to establish an optimal treatment plan in keeping with a patient-centered approach.Citation5
The patient assessment supports the high degree of patient participation revealed by 10-second event coding; 15 of 17 patients reported that they participated and contributed actively in EMMA consultations. Fewer patients (13 of 17) reported participating to a high or very high degree in the goal-setting process, which is confirmed by the experience of the HCPs. They felt that they either took too much control of the process or did not challenge unmotivated patients to engage in goal setting. The fact that the goal-setting process did not work with all patients may also be illustrated by the fact that ten of 17 patients stated that they continued to pursue the goal and plan 2 months after program completion. We conclude that, although the EMMA program works in terms of creating rapport and giving voice to patients, room for improvement exists in terms of achieving patient-centered support in goal setting and planning with all patients.
Limitations and strengths of the study
Some limitations of this study merit consideration. First, the consultations lasted much longer than planned, which limits program feasibility. This likely indicates that too many tools were allocated for each consultation or more training in using the tools is needed before the start of the program. An option is to allow patients to prepare by giving them the tools before and between consultations. Another limitation relates to the study design. Collection of data over time or the inclusion of a control group could have increased the validity of the results in terms of patient assessment and outcomes.
Strengths of the study include transparency about the theoretical foundation of the program, an element that is often missing.Citation8,Citation38 It is also a strong point that, despite its relatively small size and scope, the study involves many different data sources and the triangulation of these data. Finally, it is a strength that the tools use different learning styles and preferences, such as visual and tangible methods for reaching vulnerable patients needing extra resources and support.
Modifications based on the feasibility study
The feasibility study gave rise to a revised version of the tools, based on the feedback from patients and HCPs.Citation39 Some tools were simplified by, for instance, being made more interactive (and less susceptible to writing preferences/training) through the use of icons to illustrate biological symptoms and processes. The program format was revisited based on the time pressure experienced by HCPs. Finally, the entire program was formatted by a graphic designer to create an attractive uniform presentation.
Implications for practice
The EMMA program and, in particular, the EMMA tools guide HCPs in achieving an individualized, patient-centered approach to diabetes management with the ultimate goal of improving medical adherence and blood glucose control in patients with T2DM. However, HCP adherence to the program is not simply a matter of applying the tools. Hulvej Rod et al have coined the term “the spirit of the intervention” to describe the intangible “something” that constitutes the social effectiveness of an intervention (p. 303).Citation40 In this context, the spirit of the EMMA program is largely synonymous with the patient-centered approach built into the tools. However, the feasibility study showed that, although dialogue tools are useful in facilitating patient participation, they are not sufficient for achieving a patient-centered approach. Therefore, adequate communication skills training for HCPs is an important part of being able to practice the EMMA program. This is especially important for patients who are less motivated for changing health behavior and those who are hardly reached by HCPs.
Conclusion
The EMMA program is feasible for patients with T2DM and HCPs, and should be tested for effectiveness in a large-scale study.
Acknowledgments
The authors want to acknowledge and thank Peter Rossing, Lone Jelstrup, Frederik Persson, and Gitte Engelund for their great contributions in the process of developing the program, executing the consultations, and drafting the paper. The authors also wish to thank Kirsten Engelhard Nielsen and Birthe Marie Jørgensen and the rest of the Clinic for support to the study and all the patients who participated in the study. The authors acknowledge Jennifer Green and Caduceus Strategies for proofreading the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- InzucchiSEBergenstalRMBuseJBManagement of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD)Diabetes Care20123561364137922517736
- BaileyCJKodackMPatient adherence to medication requirements for therapy of type 2 diabetesInt J Clin Pract201165331432221314869
- VrijensBDe GeestSHughesDAA new taxonomy for describing and defining adherence to medicationsBr J Clin Pharmacol201273569170522486599
- KripalaniSYaoXHayesRBInterventions to enhance medication adherence in chronic medical conditions: a systematic reviewArch Intern Med2007167654055017389285
- Committee on the Quality of Health Care in AmericaCrossing the Quality Chasm: A New Health System for the 21st CenturyWashington, DCNational Academies Press2001
- Ismail-BeigiFMoghissiETiktinMHirschIBInzucchiSEGenuthSIndividualizing glycemic targets in type 2 diabetes mellitus: implications of recent clinical trialsAnn Intern Med2011154855455921502652
- HaywoodKMarshallSFitzpatrickRPatient participation in the consultation process: a structured review of intervention strategiesPatient Educ Couns2006631–2122316406464
- GriffinSJKinmonthALVeltmanMWGillardSGrantJStewartMEffect on health-related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trialsAnn Fam Med20042659560815576546
- StaceyDBennettCLBarryMJDecision aids for people facing health treatment or screening decisionsCochrane Database Syst Rev201110CD00143121975733
- KoenigsbergMRBartlettDCramerJSFacilitating treatment adherence with lifestyle changes in diabetesAm Fam Physician200469230931614765768
- AndrésdóttirGImproving Adherence, Prediction and Prognosis in Diabetes – With Emphasis on Neuropathy [dissertation]CopenhagenUniversity of Copenhagen2014
- FunnellMMAndersonRMArnoldMSEmpowerment: an idea whose time has come in diabetes educationDiabetes Educ19917137411986902
- AndersonRMFunnellMMPatient empowerment: myths and misconceptionsPatient Educ Couns201079327728219682830
- DeciELRyanRMThe “what” and “why” of goal pursuits: human needs and the self-determination of behaviorPsychol Inq2000114227268
- World Health OrganizationAdherence to Long-Term Therapies: Evidence for ActionGenevaWorld Health Organization2003 Available from http://www.who.int/chp/knowledge/publications/adherence_report/en/Accessed March 21, 2015
- CushingAMetcalfeROptimizing medicines management: from compliance to concordanceTher Clin Risk Manag2007360471058
- MarinkerMBlenkinsoppABondCFrom Compliance to Concordance: Achieving Shared Goals in Medicine TakingLondonRoyal Pharmaceutical Society of Great Britain1997
- WagnerLTwo decades of integrated health care in Denmark: clinical action research with respect for the autonomy of individual citizensTidsskrift for Sygeplejeforskning200621320
- KjeldsenLJBjerrumLDamPSafe and effective use of medicines for patients with type 2 diabetes – a randomized controlled trial of two interventions delivered by local pharmaciesRes Social Adm Pharm201511476224798710
- CrabtreeAHemmingsTRoddenTUsing Probes as Exploratory Devices in Care Settings. 2003 [database on the Internet] Available from http://bscw.cs.ncl.ac.uk/pub/nj_bscw.cgi/d50067/Crabtree,%20Hemmings,%20Rodden,%20Cheverst,%20Clarke%20and%20Dewsbury-Using%20Probes%20as%20Exploratory%20Devices%20in%20Care%20Settings.pdfAccessed March 21, 2015
- GaverBDunneTPacentiECultural probesInteractions1999612129
- AndersonRMFunnellMMAikensJEEvaluating the efficacy of an empowerment-based self-management consultant intervention: results of a two-year randomized controlled trialTher Patient Educ20091131120076768
- LenzTLDeveloping lifestyle medicine tools from psychological theoriesAm J Lifestyle Med2014812830
- DiMatteoMRHaskardKBWilliamsSLHealth beliefs, disease severity, and patient adherence: a meta-analysisMed Care200745652152817515779
- GattiMEJacobsonKLGazmararianJASchmotzerBKripalaniSRelationships between beliefs about medications and adherenceAm J Health Syst Pharm200966765766419299373
- ProchaskaJODiClimenteCCTranstheoretical therapy: toward a more integrative model of changePsychotherapy1982193276288
- BanduraASelf-efficacy mechanism in human agencyAm Psychol1982372122147
- CharonRThe patient-physician relationship. Narrative medicine: a model for empathy, reflection, profession, and trustJAMA2001286151897190211597295
- RollnickSMillerWRButlerCCMotivational Interviewing in Health Care: Helping Patients Change BehaviorNew YorkThe Guilford Press2008
- Diabetes foreningen (Diabetes association) [database on the Internet] Available from http://www.diabetes.dk/fagfolk/materiale/undervisningsmaterialer/tegninger-til-undervisningsbrug.aspxAccessed March 21, 2015
- SkinnerTCCareyMECradockS‘Educator talk’ and patient change: some insights from the DESMOND (Diabetes Education and Self Management for Ongoing and Newly Diagnosed) randomized controlled trialDiabet Med20082591117112019183318
- VarmingARDevelopment and Usability of a Participatory Adherence Programme Aimed at Patients with Type 2 Diabetes in Poor Glycemic Control [thesis]CopenhagenUniversity of Copenhagen2012
- BowenDJKreuterMSpringBHow we design feasibility studiesAm J Prev Med200936545245719362699
- RoterDLHallJAKatzNRPatient-physician communication: a descriptive summary of the literaturePatient Educ19881299119
- StenovVHenriksenJEFolkerAPSkinnerTCWillaingIEducator talk ratio as a quality indicator in group-based patient educationHealth Educ J Epub201541
- KraetschmerNSharpeNUrowitzSDeberRBHow does trust affect patient preferences for participation in decision-making?Health Expect20047431732615544684
- StreetRLJrMakoulGAroraNKEpsteinRMHow does communication heal? Pathways linking clinician-patient communication to health outcomesPatient Educ Couns200974329530119150199
- CraigPDieppePMacintyreSMichieSNazarethIPetticrewMDeveloping and evaluating complex interventions: the new Medical Research Council guidanceInt J Nurs Stud201350558759223159157
- Download dialogue tools from EMMA. [webpage on the Internet]GentofteSteno Diabetes Center Available from: https://steno.dk/en/pages/sundhedsprofessionelle/pages/download_dialogvaerktoj_emma.aspxAccessed March 30, 2015
- Hulvej RodMIngholtLSørensenBBTjørnhøj-ThomsenTThe spirit of the intervention: reflections on social effectiveness in public health intervention researchCrit Public Health2014243296307