Abstract
Aim
The authors examined a cohort of HIV-positive outpatients at the AIDS Center of Palermo University in Italy in order to identify factors related to the frequency of their visits to the outpatient facility for health care services.
Methods
Two hundred and twenty-four HIV-infected subjects were enrolled in the study. Demographic and HIV disease characteristics were recorded and assessed with the number of days accessed to our outpatients unit in univariate and multivariate analyses. The potential relationship with immunological status was also analyzed stratifying the patients into groups according to their CD4+ T-cell counts (≥500 vs <500/mm3, and ≥200 vs <200/mm3).
Results
Both univariate and multivariate analyses showed that duration of antiretroviral therapy <5 years and hypertension were significantly associated with a CD4+ T-cell count of <500/mm3, whereas geographic origin (Africa) was associated with a CD4+ T-cell count of <200/mm3. Mean number of days the patients sought access to day-care services for laboratory tests was negatively associated with CD4+ T-cell count.
Conclusion
Patients with low CD4+ T-cell counts showed higher use of health care services, demonstrating how early HIV diagnosis can help to reduce health care costs. The CD4+ T-cell cut-off of 200 cells emphasizes the importance of identifying and managing HIV infection among hard-to-reach groups like vulnerable migrants. In our sample, the illegal status of immigrants does not influence the management of their HIV/AIDS condition, but the lack of European health card that documents the current antiretroviral status, could interfere with the efforts to eradicate AIDS. A better understanding of the major determinants of HIV treatment costs has led to appropriate large-scale actions, which in turn has increased resources and expanded intervention programs. Further guidance should be offered to hard-to-reach groups in order to improve early AIDS diagnosis, and procedures for identifying and managing these vulnerable subjects should be made available to care commissioners and service providers.
Introduction
The advent of antiretroviral therapy (ART) has effectively changed the clinical course of HIV and patient life expectancy. The 2013 Joint United Nations Programme on HIV and AIDS report estimated that 35 million people are living with HIV and 1.5 million have died of AIDS worldwide.Citation1
The number of new infections, which is currently 2.1 million per year worldwide, is falling.Citation1 However, because of socioeconomic reasons, there are discernible disparities between subequatorial countries and other parts of the world. This is demonstrated by differences in way and time of access to health care services in different countries.Citation1
In Europe, access to health care is a key factor in promoting and safeguarding the individual’s health. In Western and Northern Europe as well as in the US, preventing transmission of HIV infection and attempting early diagnosis have become the order of the day. However, since 2007, European health care systems have been affected by the global economic crisis, resulting in changes involving access to health care and to preventive services. The biggest challenge is how to provide optimal care for HIV patients at the lowest possible cost. In the US, the RESPECT program sponsored by the American Centers for Disease Control and Prevention has provided guidelines about the identification of patients whose risk factors justify carrying out anti-HIV testing, and about correct diagnostic and therapeutic procedures. The problem of migration, mainly from sub-Saharan Africa, is an issue with which many European countries and Italy and Spain are currently contending; this reality inevitably contributes to the significant change in HIV epidemiology.Citation2–Citation4
Migrants represent an independent risk factor for HIV infection, and at the same time, they are more likely to receive a delayed diagnosis due to late presentation with the disease. This makes clinical management more onerous and health care costs higher. In 2010, 49% of new infections diagnosed in Europe were among migrants. The Dublin Declaration guarantees the right of citizens to ART.Citation5,Citation6
The delivery of health care services in Italy is patchy, and is financed and organized at a regional level; consequently, the cost of HIV treatment varies significantly across regions and between medical centers. In Southern Italy and in Sicily in particular, immigration can be considered an epidemiologically relevant phenomenon as far as health structures and institutional approaches are concerned, with an average of ≥24.1/100,000 new HIV infections per year.Citation7
In this study, we examined a cohort of HIV outpatients in Southern Italy between 2011 and 2013 in order to identify the factors that determined their utilization of health care resources. Consequently, we propose a way to better control the costs of managing these patients. We evaluated key factors by dividing the patients according to their CD4+ T-cell counts.
Materials and methods
Design and setting
We conducted a retrospective study of 224 HIV-positive individuals who attended the Infectious Diseases Outpatient Clinic of the “Paolo Giaccone” University Hospital in Palermo, Italy, for follow-up blood tests related to their HIV status between 2011 and 2013. Demographic and HIV disease characteristics were recorded and assessed with the number of days patients sought access to our outpatients unit in univariate and multivariate analyses. Potential relationship between immunological status was also analyzed stratifying the patients into groups according to their CD4+ T-cell counts (≥500 vs <500/mm3 and ≥200 vs <200/mm3).
Approximately 700 patients are admitted to this clinic each year for HIV management. Committed to the prevention and care of HIV infection, it is the regional AIDS referral center. Between 2009 and 2013, 980 new cases of HIV infection were registered in Sicily (270 of these in Palermo), with an average incidence rate of 3.92/100,000 per year.Citation8,Citation9
Virological and immunological follow-up is performed every 3 or 6 months, depending on clinical and immunological parameters. Patients receive free comprehensive care, including treatment for opportunistic infections (including tuberculosis [TB]), macro- and micronutrient supplementation, psychosocial counseling, adherence counseling, and education about prevention strategies, and defaulter tracing is also carried out. According to Italian, European, and International guidelines,Citation10 ART is typically initiated when CD4+ T-cell count is <350/mm3 (patients in clinical stage 3 or 4) and when CD4+ T-cell count is >350/mm3 but <500/mm3. ART is recommended to prevent transmission, or in the event of pregnancy, coinfections (hepatitis B virus–hepatitis C virus [HBV-HCV], HIV-AN, HIV-associated neurocognitive disorder [HAND]), or non-AIDS-related tumor. On the contrary, when CD4+ T-cell count is >500/mm3, ART is recommended when there is a rapid decline in CD4+ T-cell count (≥100/mm3 annually) or when the count of HIV-RNA is ≥100,000 copies/mL. During each visit to the clinic, adherence is assessed by self-report. Adherence is considered “perfect” when the patients indicate that they have taken every dose as prescribed since starting ART.
Patient medical records were collected and entered into a hospital medical record database.
Informed consent, including consent to publication of patient details, was signed by all individuals before they accessed the day health care services, in accordance with the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of the “Paolo Giaccone” University Hospital in Palermo, Italy.
Patients
Data on patients who were followed up at the AIDS Center of the “Paolo Giaccone” University Hospital in Palermo, Italy, in the day care or outpatient facility between January 2011 and May 2013 were extracted from the hospital’s medical record database.
We gathered clinical documentation on 224 HIV-positive subjects with complete follow-up data for the under-review period. The following data were collected and entered into the specially designed database: (a) demographic and clinical characteristics of patients: age, gender, geographic origin (namely patient’s geographical origin stated in their document certified by the Italian institutions), lifestyle habits (including educational level, drug abuse history, sexual behavior), body mass index (BMI), comorbidities such as HCV coinfection, osteoporosis biomarker, treatment for dyslipidemia (total cholesterol ≥300 mg/dL and total cholesterol-to-high-density lipoprotein ratio >5 in males and >4 in females), diabetes, renal function, and hypertension; (b) current CD4+ T lymphocyte counts (cells/µL) were determined by flow cytometry, and HIV RNA viral load (VL) was measured in plasma by reverse transcriptase polymerase chain reaction (Roche Amplicor; lower limit of quantitation 20 copies/mL, 1.3 log10) as previously reported;Citation11 and (c) variables related to ART: date of ART initiation, total time on ART, antiretroviral (ARV) drugs received and degree of adherence, as well as protease inhibitors and non-nucleoside reverse transcriptase inhibitors, and exposure to tenofovir and other ARV drugs (ie, raltegravir, maraviroc). These data were obtained from medical records and previously published investigations.Citation11–Citation13
All patients except the treatment-naïve subjects had started ART during previous inpatient stays.
None of the migrants enrolled in the study had a general practitioner (GP).
Statistical analysis
Statistical analysis of quantitative and qualitative data, including descriptive statistics, was performed for all items. Continuous data are expressed as mean ± standard deviation (SD), unless otherwise specified. Frequency analysis was performed with chi-square test or Fisher’s exact test, as needed. The intergroup differences were assessed by one-way analysis of variance and Mann–Whitney U statistic test for parametric and nonparametric variables, respectively.
Odds ratios (ORs) and their 95% confidence intervals (CIs) were calculated using the univariate and multivariate model of multinomial logistic regression analysis. Data were analyzed with Epi Info software (version 6.0; Centers for Disease Control and Prevention, Atlanta, GA, USA) and IBM SPSS Software version 21.0 (IBM Corporation, Armonk, NY, USA). All P-values were two sided, and P-values <0.05 were considered statistically significant.
Results
depicts the patient parameters collected from the electronic medical record database.
Table 1 Demographic/lifestyle and clinical characteristics of the study participants according to CD4+ cell count
Data were stratified according to CD4+ T-cell count, comparing the characteristics of patients with CD4+ T-cell counts ≥500 vs <500/mm3 and ≥200 vs <200/mm3. The average age of patients enrolled in the study was 45.6±9.2 years; 163 were males (73%), and 61 females (27%); 26 outpatients were African immigrants (12%) (). Nineteen of the 224 patients showed HIV–HCV coinfections (8.5%) (). Fourteen patients were treatment-naïve (6.3%), and the average of current CD4+ T-cell count was 524±292 SD (median 476)/mm3, while mean HIV RNA VL was 1.82 (±1.16; median 1.3) log10 copies/mL.
For the whole group, mean number of days of access to day-care services for laboratory tests (to evaluate stage of HIV and to monitor treatment) was 6.5 (±2.5) days for CD4+ T-cell count measurements and 9.6 (±3.5) for HIV RNA VL.
CD4+ T-cell count ≥500 vs <500/mm3
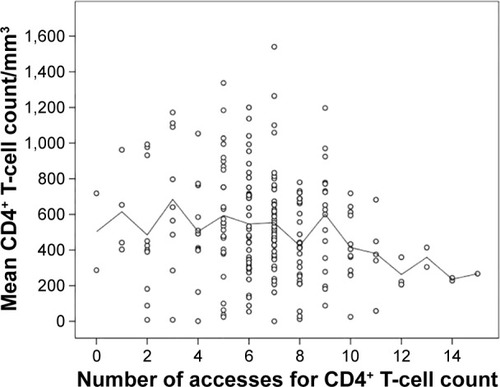
For the patient groups with CD4+ T-cell counts of ≥500 vs <500/mm3, <5 years of ARV treatment and mean number of days of access to day-care services for laboratory tests – to evaluate HIV stage and to monitor treatment – were negatively associated with CD4+ T-cell count (P=0.017 and P=0.026, respectively) (; ).
As far as biochemical and physical parameters were concerned, hypertension was negatively associated with CD4+ T-cell count in the <500/mm3 group (P=0.044) ().
depicts the univariate and multivariate regression analysis of patients with CD4+ T-cell counts of ≥500 vs <500/mm3. Less than 5 years of ART (OR =2.01, 95% CI: 1.15–3.53, P=0.015 and OR =2.21, 95% CI: 1.22–3.99, P=0.009, respectively) and hypertension were significantly associated with a CD4+ T-cell count of <500/mm3 in both univariate and multivariate analyses (OR =2.20, 95% CI: 1.02–4.75, P=0.044 and OR =2.380, 95% CI: 1.05–5.41, P=0.039, respectively).
Table 2 Univariate and multivariate regression analysis of patients stratified by 500/mm3 CD4+ T-cell count
Mean number of days of access to day-care services for laboratory tests was negatively associated with CD4+ T-cell count but only in univariate regression analysis.
CD4+ T-cell count ≥200 vs <200/mm3
We identified African race (P=0.034), low BMI (P=0.001), and drug addiction (P=0.039) as significant risk factors in the <200/mm3 patient group ().
depicts the univariate and multivariate regression analysis of patients with CD4+ T-cell counts of ≥200 vs <200/mm3; we found a significant association between ethnicity (African) and a CD4+ T-cell count of <200/mm3 in both univariate and multivariate analyses (OR =3.19, 95% CI: 1.13–9.03, P=0.028 and OR =10.05, 95% CI: 1.84–54.9, P=0.008, respectively), while a significant association between drug addiction and CD4+ count was detected in univariate regression analysis only ().
Table 3 Univariate and multivariate regression analysis of patients’ characteristics stratified by 200/mm3 CD4+ T-cell count
Discussion
The growing demand for health care services depends on a number of factors: an increase in the life expectancy of HIV patients, management of age-related diseases which requires patients to be monitored two to four times a year for highly active ART efficacy/toxicity, ethnicity and mode of transmission, AIDS-related diseases, and the important role of prevention (testing and counseling).Citation12,Citation14
The mean CD4+ T-cell count of our patients was 524/mm3; therefore, we can consider them to be a well-managed population of individuals treated for HIV, with CD4+ cell counts over 500/mm3, or in any case, with chronic HIV infection and high CD4+ T-cell levels.
Mean access to day-care services for laboratory tests to evaluate stage of HIV infection and to monitor treatment was 6.5 days for CD4+ T-cell count measurements and 9.6 for HIV RNA VL.
These results, which refer to a 25-month follow-up period, comply with standard recommendations if we consider that our cohort consists of patients who are on ART and have undetectable VL levels. Regarding mean and standard deviation calculated for the number of days of access to health care services for VL monitoring, our data demonstrate the importance of ARV drug monitoring and management to assess indicators such as adherence and emergence of HIV drug resistance, and to estimate the time to viral suppression after initiating a first-line regimen.Citation15,Citation16
In our study, mean number of days of access to day care for laboratory tests was negatively associated with CD4+ cell counts. These findings provide further support for early combination ART initiation in order to reduce the costs of health care management.Citation17,Citation18
Stratifying the patients according to CD4+ T-cell count, the 500/mm3 cut-off value helps us to identify the factors that determine manner and time of access to health care for HIV patients, whereas the 200/mm3 cut-off shows the key high-risk HIV groups such as migrants vs natives and drug addiction categories and confirmed the higher frequency of AIDS events in these categories of patients, as reported in other studies and recently by the Italian ICONA cohort study group.Citation19,Citation20
Regarding patient comorbidities, only hypertension was significantly associated with CD4+ T-cell count, highlighting how we can identify the key factors that determine HIV patients’ use of health care services through monitoring other pathologies affecting these subjects, such as cardiovascular disease.Citation21
But how are we to cope with increased demand for these health care resources in a time of economic crisis?
Our study demonstrates that two categories of patients – drug addicts and immigrants – make greater use of health care services.
Data on injection drug users per se emphasize the importance of sustained HIV prevention measures for this category of patients who generally have a poor prognosis.Citation22–Citation24
Nevertheless, we must stress the importance of managing the migrant population if we aim to reduce health care costs related to HIV infection.
Patients in the “frail patient” category and those with sociopsychological issues are most in need of health care. In particular, the influx of immigrants poses a real challenge to public health, other than a significant change in HIV epidemiology. Available literature shows that utilization of health care services is a primary indicator of migrant integration.Citation25
None of the migrants enrolled in the study had a GP, though some of them had been resident in the country for a long time. Generally speaking, not only migrants but also Italian natives are reluctant to go to their GP. The Italian National Health Systems are going through a phase of change, but patients still prefer to go to hospital rather than visit their GP. This has been found in a pediatric study that the first author has published.Citation26
Many of the immigrant patients in the study had just arrived from Libya in a situation of humanitarian emergency, as continues to be the case today. They are then transferred to a migrant reception center where they do not have access to a GP. Even after being in the country for some time, because of their frequent lack of work, they are considered illegal immigrants. Moreover, without a permit to stay in the country, they cannot be assigned to a GP. Regarding the services we provide for these migrants, we want to stress that their status has never influenced ART decisions. Thanks to an exemption granted by the Italian state, these individuals receive the same treatment as Italian natives regardless of cost and based solely on the patient’s state of health. Unfortunately, because there is no European health card for migrants, data about treatment that these patients received in other countries once they had started ART are not available. The same may be said for other pathologies such as TB. Today, data need to be updated to take into account the emergency in Syria, but in general, the incidence of AIDS among African subjects remains high, as the incidence of TB does.
The findings of this study have several limitations. First, we did not determine CD4+ nadir, so we cannot correct the data with other risk factors, and we cannot estimate the time passed from the first diagnosis and the beginning of ARV even if none of migrant population and most of Italian HIV patients had never had a CD4+ count before admission to our hospital. Second, our study shows all the limitations of retrospective studies, and the small number of patients could suggest that our data reflected a local epidemiological situation.
The Italian government recognizes that migrants are vulnerable to social stigma, lack of community support, isolation, racism, and discrimination for being an HIV-positive migrant. Nevertheless, HIV testing for migrants is not explicitly recommended in Italy. For this reason, from 2009 to 2013, the ARTEMIS project was established to provide a program of social and health integration. COA-ISS data show an increase in the rate of new HIV infections among migrants compared to 1996, and a higher incidence of TB–HIV coinfection (particularly in patients from Eastern Europe).Citation27,Citation28
Total delay in diagnosis and initiation of effective treatment depends on two separate, but in some cases concomitant, elements: the delay attributable to the patient and the delay attributable to the health care system.
Delay attributable to the patient may be due to many factors, including demographics (gender, age), level of education, socioeconomic factors (poverty, loss of income or employment), awareness of the symptoms of disease, logistic factors (accessibility of health services, the structure chosen for first login), stigma associated with infectious disease, and in some populations, cultural and/or religious bias.
Delay attributable to the health care system depends on organizational aspects, such as weaknesses in the service network, lack of coordination and lack of effective and timely flow of information, lack of awareness of the clinical problem within the service network, or infrequent use of rapid diagnostic tools. A “vicious cycle” of repeated access to the same structure or structures of the same level with little diagnostic capacity is one of the main risk factors for delayed diagnosis.
Scientific evidence shows that in countries with a low incidence of the disease, the presence of problematic, vulnerable, and socially marginalized groups is a determining factor of delays in diagnosis and in initiating appropriate treatment, and may represent an epidemiologically relevant source of HIV transmission.
Migrants and refugees from countries with a high incidence of HIV and other coinfections such as TB are exposed to difficulties related to language and cultural barriers, especially in the early years of their stay in Italy; these factors constitute a substantial part of the so-called vulnerable communities.Citation29,Citation30
Sicily’s regional health policy lacks the involvement of cultural associations that can raise awareness and direct migrants to preventive health care services. Most of the immigrants diagnosed with HIV are pregnant women who have undergone tests for sexually transmitted diseases. The delay in diagnosis together with the difficulty of access to preventive health care services may mean that these patients at diagnosis exhibit other HIV-related diseases resulting in a strong burden for the health care system.Citation27,Citation31
Conclusion
A better understanding of the major determinants of HIV treatment costs has led to appropriate large-scale actions, which has increased resources and expanded intervention programs. As is the case for TB, further guidance needs to be offered to hard-to-reach groups in order to diagnose AIDS earlier,Citation32,Citation33 and procedures for identifying and managing these vulnerable subjects should be made available to care commissioners and service providers.Citation34
Acknowledgments
The authors wish to thank Fanny Pojero, PhD, for reviewing the language and the syntax of the manuscript.
Disclosure
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- Global report: UNAIDS report on the global AIDS epidemic 2013 “UNAIDS/JC2502/1/E” – revised and reissued2013 Available from: http://www.unaids.org/sites/default/files/en/media/unaids/con-tentassets/documents/epidemiology/2013/gr2013/UNAIDS_Global_Report_2013_en.pdfAccessed February 27, 2015
- MugaveroMJDavilaJANevinCRGiordanoTPFrom access to engagement: measuring retention in outpatient HIV clinical careAIDS Patient Care STDS20102460761320858055
- CataniaJADolciniMMGandelmanAANarayananVMcKayVRFiscal loss and program fidelity: impact of the economic downturn on HIV/STI prevention program fidelityTransl Behav Med20144344524653775
- OlivaJDíezMGalindoSPredictors of advanced disease and late presentation in new HIV diagnoses reported to the surveillance system in SpainGac Sanit20142811612224365520
- HoyosJFernández-BalbuenaSde la FuenteLMadrid Rapid HIV Testing Group. Never tested for HIV in Latin-American migrants and Spaniards: prevalence and perceived barriersJ Int AIDS Soc2013161856023663441
- ECDC – migrants monitoring implementation of the Dublin Declaration on Partnership to fight HIV/AIDS in Europe and Central Asia: 2012 progress report Available from: http://ecdc.europa.eu/en/publications/Publications/dublin-migrants-evidence-brief-september-2013.pdfAccessed February 27, 2015
- Update new diagnostic is HIV infection and cases of AIDS in Italy at 31 December 2011 Available from: http://www.iss.it/binary/ccoa/cont/Report_COA_2012_corretto.pdfAccessed February 27, 2015
- Surveillance of HIV in Sicily, Italy – 2013 Available from: http://pti.regione.sicilia.it/portal/page/portal/PIR_PORTALE/PIR_LaStrutturaRegionale/PIR_AssessoratoSalute/PIR_AreeTematiche/PIR_Epidemiologia/PIR_Registridipatologia/PIR_RegistrosorveglianzaHIV/Report_HIV_2014.pdfAccessed February 27, 2015
- CamoniLBorosSRegineVAggiornamento delle nuove diagnosi di infezione da HIV e dei casi di AIDS in Italia al 31 dicembre 2013 [Update of new diagnoses of HIV infection and AIDS cases in Italy on 31 December 2013]Not Ist Super Sanità2014279 Suppl 1347 Italian
- Panel on Antiretroviral Guidelines for Adults and AdolescentsGuidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescentsDepartment of Health and Human Services Available from: http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdfAccessed April 27, 2016
- Li VecchiVSoresiMGiannitrapaniLDairy calcium intake and lifestyle risk factors for bone loss in hiv-infected and uninfected Mediterranean subjectsBMC Infect Dis20121219222894751
- RestelliUAndreoniMAntinoriABudget impact analysis of antiretroviral less drug regimen simplification in HIV-positive patients on the Italian National Health ServiceClinicoecon Outcomes Res2014640941425285019
- Li VecchiVGiannitrapaniLDi CarloPNon-invasive assessment of liver steatosis and fibrosis in HIV/HCV- and HCV-infected patientsAnn Hepatol20131274074824018492
- RizzardiniGBonfantiPCarenziLCost-effectiveness analysis of HIV treatment in the clinical practice of a public hospital in northern ItalyTher Clin Risk Manag2012837738423028230
- World Health Organization (WHO)National AIDS programmes: a guide to indicators for monitoring and evaluating national antiretroviral programmesGenevaWHO2006 Available from: http://www.who.int/hiv/enAccessed February 27, 2015
- World Health Organization (WHO)Patient monitoring guidelines for HIV care and antiretroviral therapy (ART)GenevaHIV/AIDS Department, WHO2008 Available from: http://www.who.int/hiv/pub/guidelines/patientmonitoring.pdfAccessed February 27, 2015
- SidibéMZunigaJMMontanerJLeveraging HIV treatment to end AIDS, stop new HIV infections, and avoid the cost of inactionClin Infect Dis201459Suppl 1S3S624926030
- WHOConsolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health ApproachGenevaWorld Health Organization2013
- SaracinoALorenziniPLo CaputoSICONA Foundation Study GroupIncreased risk of virologic failure to the first antiretroviral regimen in HIV-infected migrants compared to natives: data from the ICONA cohortClin Microbiol Infect201622288.e1288.e826551839
- PezzoliMCHamadIEScarcellaCPRISHMA Study GroupHIV infection among illegal migrants, Italy, 2004–2007Emerg Infect Dis2009151802180419891869
- BrennanAMorleyDO’LearyACBerginCJHorganMDeterminants of HIV outpatient service utilization: a systematic reviewAIDS Behav20141910411924907780
- MilloyMJMarshallBDKerrTSocial and structural factors associated with HIV disease progression among illicit drug users: a systematic reviewAIDS2012261049106322333747
- BoothREDvoryakSSung-JoonMLaw enforcement practices associated with HIV infection among injection drug users in Odessa, UkraineAIDS Behav2013172604261423754613
- CamoniLRaimondoMRegineVSalfaMCSuligoiBregional representatives of the HIV Surveillance SystemLate presenters among persons with a new HIV diagnosis in Italy, 2010–2011BMC Public Health20131328123537210
- WasserfallenJBHyjaziACavassiniMComparison of HIV-infected patients’ characteristics, healthcare resources use and cost between native and migrant patientsInt J Public Health20095451019142582
- Di CarloPRomanoAPlanoMRChildren, parents and Respiratory Syncytial Virus in Palermo, Italy: prevention is primaryJ Child Health Care20101439640720395316
- Alvarez-Del ArcoDMongeSCaro-MurilloAMStudy Working GroupHIV testing policies for migrants and ethnic minorities in EU/EFTA Member StatesEur J Public Health20142413914423921295
- ARTEMIS: Associations & Territorial Networks for Intercultural Mediation Health Available from: http://www.iss.it/ccoaAccessed February 27, 2015
- SulisGEl HamadIFabianiMHIV/Migrants Study GroupClinical and epidemiological features of HIV/AIDS infection among migrants at first access to healthcare services as compared to Italian patients in Italy: a retrospective multicentre study, 2000–2010Infection20144285986724973981
- DiezMDiazAGarrigaCThe Hospital Survey Study Group C. A low-cost, sustainable, second generation system for surveillance of people living with HIV in Spain: 10-year trends in behavioural and clinical indicators, 2002 to 2011Euro Surveill20141920
- PellowskiJAKalichmanSCRecent advances (2011–2012) in technology-delivered interventions for people living with HIVCurr HIV/AIDS Rep2012932633422922945
- SeedatFHargreavesSFriedlandJSEngaging new migrants in infectious disease screening: a qualitative semi-structured interview study of UK migrant community health-care leadsPLoS One2014910e10826125330079
- MirzazadehAGrassoMJohnsonKAcceptability of Global Positioning System technology to survey injecting drug users’ movements and social interactions: a pilot study from San Francisco, USATechnol Health Care20142268970024990173
- MocroftALundgrenJDSabinMLCollaboration of Observational HIV Epidemiological Research Europe (COHERE) study in EuroCoordRisk factors and outcomes for late presentation for HIV-positive persons in Europe: results from the Collaboration of Observational HIV Epidemiological Research Europe Study (COHERE)PLoS Med2013109e100151024137103