?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Objective
Previous US-based economic models of noninvasive tests for diagnosis of Helicobacter pylori infection did not consider patient adherence or downstream costs of continuing infection. This analysis evaluated the long-term cost-effectiveness of the urea breath test (UBT), fecal antigen test (FAT), and serology for diagnosis of H. pylori infection after incorporating information regarding test adherence.
Materials and methods
A decision-analytic model incorporating adherence information evaluated the cost-effectiveness of the UBT, FAT, and serology for diagnosis of H. pylori infection. Positive test results led to first-line triple therapy; no further action was taken for nonadherence or negative results. Excess lifetime costs and reduced quality-adjusted life-years (QALYs) were estimated for patients with continuing H. pylori infection.
Results
In the base-case scenario with estimated adherence rates of 86%, 48%, and 86% for the UBT, monoclonal FAT, and serology, respectively, corresponding expected total costs were US$424.99, $466.41, and $404.98/patient. Test costs were higher for the UBT, but were fully or partially offset by higher excess lifetime costs for the monoclonal FAT and serology. The QALYs gained/patient with the UBT vs monoclonal FAT and serology were 0.86 and 0.27, respectively. The UBT was dominant vs the monoclonal FAT, leading to lower costs and higher QALYs; the UBT was cost-effective vs serology (incremental cost/QALY gained $74).
Conclusion
Based on a comprehensive modeled analysis that included consideration of patient test adherence and long-term consequences resulting from continuing H. pylori infection, the UBT provided the greatest economic value among noninvasive tests for diagnosis of H. pylori infection, because of high patient adherence and excellent test performance.
Introduction
Helicobacter pylori infection is a common chronic infection that is associated with upper gastrointestinal diseases, including chronic gastritis, peptic ulcers, and gastric cancer (GC).Citation1 The prevalence of H. pylori is estimated at ~30% in the adult US population, based on data from the National Health and Nutrition Examination Survey, with higher rates with increasing age.Citation2 Individuals infected with H. pylori have a 15% (vs 4% among noninfected individuals) risk of developing peptic ulcer disease (PUD), and are at tenfold-higher risk of gastric adenocarcinoma.Citation3,Citation4 A large majority (70%–90%) of patients with PUD are infected with H. pylori, and its eradication is an important component of treatment for preventing ulcer recurrence.Citation5
H. pylori infection in the stomach can be detected using invasive (ie, endoscopic) or noninvasive methods. Noninvasive methods have been developed to detect H. pylori antibodies in the blood (serology), H. pylori antigen in the feces (fecal antigen test [FAT]), and change in concentration of isotopically labeled carbon dioxide in exhaled breath samples as the result of hydrolysis of isotopically labeled urea by urease-containing H. pylori in the stomach (urea breath test [UBT]). The American College of Gastroenterology (ACG) and American Gastroenterological Association recommend noninvasive tests for H. pylori in dyspeptic patients aged <55 years who do not have alarm features, such as bleeding, early satiety, unexplained weight loss, progressive dysphagia, and family history of gastrointestinal cancer, and then treatment for those who test positive for the infection.Citation1,Citation6 Among noninvasive tests, both the ACG and American Gastroenterological Association recommend the UBT and FAT over serology, because both these tests detect active H. pylori infection, whereas serology is indicative of both current and previous exposures to H. pylori.
Several cost-effectiveness analyses comparing different test methods in the diagnosis of H. pylori infection have been published.Citation7–Citation11 These analyses typically indicated that the UBT and FAT were more cost-effective than serology when used individually to detect H. pylori infection (as opposed to when a test was used in tandem with another for confirmatory purposes). Some of these analyses also showed higher cost-effectiveness of the FAT over the UBT, because the FAT generally costs less than the UBT, while displaying high sensitivity, specificity, and positive and negative predictive values in diagnostic testing for H. pylori.Citation8,Citation11,Citation12 These analyses did not, however, include patient preference for type of test or patient compliance with/adherence to testing for H. pylori infection in their modeling. Several studies have shown low patient preference for or adherence to collecting stool samples for colorectal cancer screening and H. pylori testing.Citation13–Citation15 Patient-adherence rates in collecting stool samples ranged from 18% in colorectal cancer screening with the fecal occult blood test to 48% in posttreatment testing to confirm eradication of H. pylori infection.Citation13,Citation15
The objective of the present study was to create a robust US-based cost-effectiveness model that incorporates patient adherence to testing for infection to understand the differences (in terms of both health and economic outcomes) among noninvasive tests (UBT, FAT, and serology) for the diagnosis of H. pylori infection.
Materials and methods
A decision-analytic model that incorporated patient adherence was developed from a US third-party payer perspective to evaluate the cost-effectiveness of the UBT, monoclonal and polyclonal FATs, and serology in the initial diagnosis of H. pylori infection (). The model considered only direct health care costs; indirect costs such as lost productivity due to treatment and other H. pylori-specific impairments were not included. According to US pharmacoeconomic modeling convention, patient copayments were not considered in the cost-effectiveness analysis. The study population consisted of patients aged 18–55 years (average age 35 years) with dyspeptic symptoms, but no gastrointestinal alarm features. In this population, noninvasive H. pylori-testing options are preferred to those requiring endoscopy, as recommended in the ACG guidelines.Citation1
Figure 1 Decision-tree model.
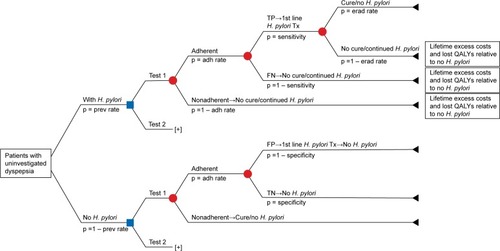
The decision-analytic model investigated the consequences of choosing between two tests. For each test, the model assumed that patients with positive test results (both true and false positives) received first-line triple therapy for the eradication of H. pylori infection. No further action was taken in the model for patients who were nonadherent to testing or who tested negative (both true and false negatives). Excess lifetime costs (LTCs) and reduced quality-adjusted life-years (QALYs) per patient – estimated with respect to patients without H. pylori infection – were applied to patients with continuing H. pylori infection due to nonadherence, false-negative test results, or treatment failure. The model assumed that true-positive patients respond to first-line treatment, and that no further action was taken for true-negative and false-positive patients without H. pylori infection.
Model input parameters included population characteristics, treatment attributes, and data for diseases related to H. pylori infection (). Input parameters for each diagnostic test included its sensitivity, specificity, cost, and rate of adherence to the test (). The sensitivities and specificities of the UBT, FAT, and serology represent mean values estimated from systematic reviews or meta-analyses evaluating these tests in pretreatment diagnosis of H. pylori.Citation12,Citation16,Citation17 The cost of each test was obtained from the 2014 Resource-Based Relative Value Scale using the Current Procedural Terminology codes indicated in . The adherence rates of the UBT and FAT (86% and 48%) were determined as the proportion of patients who completed these tests following H. pylori-eradication therapy.Citation13 Due to the lack of published literature on the adherence rate of serology, it was assumed to be the same as that of the UBT, as both require a follow-up visit. Both the monoclonal and polyclonal FATs were considered in the present model. Only information from analyses with the monoclonal FAT are however presented in this manuscript unless specified otherwise, because the monoclonal FAT has higher sensitivity and specificity than the polyclonal FAT (with all other attributes, including cost and adherence, being equal) and can thus be considered to be the better-performing test.
Table 1 Population characteristics, treatment attributes, and data for diseases related to Helicobacter pylori infection
Table 2 Test characteristics
Treatment-related inputs to the model included the cost and eradication rate of first-line triple therapy. The ACG recommends triple therapy with a standard-dose proton-pump inhibitor, amoxicillin 1,000 mg, and clarithromycin 500 mg twice daily for 14 days as first-line treatment of H. pylori infection.Citation1 The cost of this regimen with omeprazole 40 mg/day as the proton-pump inhibitor was determined to be US$205.85 based on average wholesale prices obtained from the Micromedex Red Book (Truven Health Analytics, Ann Arbor, MI, USA). The eradication rate for this 14-day triple-therapy regimen of 81% was obtained from a meta-analysis comparing different durations of therapy.Citation18
The H. pylori prevalence in the study population was estimated to be 37.4% based on a weighted average of prevalence rates reported for each racial/ethnic group in the 1999–2000 National Health and Nutrition Examination Survey.Citation19
Three H. pylori-related conditions were considered in the model: GC, PUD, and continuing dyspepsia. Estimates of the excess LTCs for patients with continuing H. pylori infection compared with patients without continuing infection were derived from parameters associated with each of these three conditions. For GC, these attributes included lifetime risk of developing GC with or without H. pylori infection, median survival with GC, expected LTCs of managing GC, and average time elapsed between diagnosis of H. pylori infection and diagnosis of GC. Similar parameters, combined with utility values for each H. pylori-related condition, were used to derive the reduced QALYs for patients with continuing H. pylori infection relative to patients without continuing infection.
Expected excess LTCs and reduced QALYs due to continuing H. pylori infection for each of the three H. pylori-related conditions were derived separately and then summed to obtain the total expected excess LTCs and reduced QALYs due to continuing H. pylori infection. The following equations describe the derivation of the excess LTCs due to continuing H. pylori infection (LTCHP):
(1) where Dysp is dyspepsia, and LTCi is excess LTCs for each H. pylori-related disease.
Excess LTCs for each of the three H. pylori-related diseases were in turn estimated as cost/patient of managing each disease multiplied by the excess risk associated with developing each disease due to continuing H. pylori infection:
(2) where Pi is risk associated with developing each disease, [w] is with H. pylori infection, [wo] is without H. pylori infection, and Ci is cost for each disease.
The cost/patient of managing PUD was estimated as the sum of the cost of PUD managed by medication (regardless of hospitalization) and the cost of a related hospitalization multiplied by its probability of occurrence:
(3) where CPUD is cost/patient of managing PUD, tPUD is duration of PUD (in years), CPUD[med] is cost/patient of managing PUD by medication (regardless of hospitalization), CPUD[hosp] is cost of related hospitalization, and pPUD[hosp] is its probability of occurrence.
The cost/patient of managing dyspepsia was estimated as the duration of dyspepsia (tDysp; in units of years) multiplied by the annual cost/patient of managing dyspepsia (CDysp[ann]). It was assumed that all patients with continuing H. pylori infection who do not develop PUD or GC develop dyspepsia:
(4)
(5) where CDysp is cost/patient of managing dyspepsia, tDysp is duration of dyspepsia (in years), and p is probability of occurrence.
Estimates of the reduced QALYs associated with continuing H. pylori infection were derived in a similar manner. As an illustration of the application of the aforementioned equations, the estimation of excess LTCs associated with PUD is described in a step-by-step manner in .
One-way and probabilistic sensitivity analyses were conducted to test the robustness of the cost-effectiveness results generated by the model to uncertainty in the input-parameter estimates. Input parameters for the one-way and probabilistic sensitivity analyses (eg, standard errors, ranges) were obtained from literature sources cited previously, if available, or were estimated based on assumptions of uncertainty around base-case parameter estimates (measures of uncertainty for model-input parameters are summarized in and ). For probabilistic sensitivity analyses, the beta-distribution was used for the sensitivities, specificities, and adherence rates of the tests, as well as all other probabilities used in the model. Gaussian distribution was used for all costs. Measures of uncertainty for excess LTC and reduced QALY estimates to be used in the one-way and probabilistic sensitivity analyses were estimated using a Monte Carlo simulation. The Monte Carlo simulation generated 3,000 values each for excess LTCs and reduced QALYs associated with continuing H. pylori infection, and the means and standard deviations of these parameters were estimated from the resulting simulated data sets. These descriptive statistics were then used to generate lower and upper bounds for the one-way sensitivity analyses. For the probabilistic sensitivity analyses, appropriate distributions were selected based on the resulting simulated data sets. Excess LTCs and reduced QALYs were estimated for patients aged 35 years, which was representative of the study population and is near the midpoint of the age range (18–55 years) considered in the study. The expected life years remaining for these representative patients were obtained from life tables (1999–2001) for the total US population when life expectancy at birth was 77 years.Citation20 The estimate of expected life years remaining was allowed to vary in the Monte Carlo simulations.
Results
In the base-case scenario, wherein the estimated patient-adherence rates were 86%, 48%, and 86% for the UBT, monoclonal FAT, and serology, respectively, the corresponding expected total costs/patient were estimated to be $424.99, $466.41, and $404.98 (). The polyclonal FAT was also evaluated in the model, showing a total cost of $483.25/patient, which was similar to that for the monoclonal FAT. (Hereafter, results for the FAT refer to those obtained with the monoclonal FAT.) Despite the higher testing costs of the UBT vs the FAT, the total cost associated with the UBT was less than that with the FAT, reflecting the substantially higher excess LTCs (associated with the FAT) of managing continuing dyspepsia, PUD, and GC in patients with continuing H. pylori infection. Moreover, the cost per accurately diagnosed case of H. pylori infection was approximately twice as high for the FAT vs the UBT. The estimated QALYs gained/patient with the UBT vs the FAT and serology were 0.86 and 0.27, respectively. The reduced QALYs due to continuing H. pylori infection were estimated to be 0.78, 1.63, and 1.05 for the UBT, FAT, and serology, respectively.
Table 3 Base-case economic and health outcomes
The UBT was cost-effective when compared with the FAT and serology as a diagnostic test for the detection of H. pylori infection. Furthermore, the UBT achieved a decrease in total costs, as well as an increase in QALYs, compared with the FAT (). The estimated incremental cost/QALY gained (ie, incremental cost-effectiveness ratio [ICER]) was negative for the UBT vs FAT comparison, indicating that the UBT was dominant (cost-saving while also improving health outcomes). In comparison with serology, there was a modest increase of ~5% in total cost and a ~26% increase in QALYs for the UBT. The ICER for the UBT vs serology comparison was $74.20/QALY gained. Further, the UBT had the lowest cost per correct diagnosis among the three noninvasive tests evaluated. The primary driver of the cost-effectiveness of the UBT was its higher adherence rate vs the FAT, and its higher sensitivity and specificity vs serology.
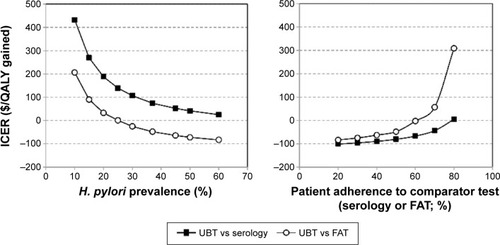
The effects of patient-adherence rates and H. pylori prevalence on the cost-effectiveness of the UBT vs FAT and serology were assessed in one-way sensitivity analyses (). The UBT was cost-saving vs the FAT across patient-adherence rates with the FAT of 20%–62%; the UBT remained cost-effective vs the FAT when the adherence rate with the FAT was between 63% and 87%. The FAT became more cost-effective than the UBT when the patient-adherence rate with the FAT exceeded ~87.4%. The UBT remained cost-effective even with H. pylori prevalence <25%. The UBT was cost-saving vs serology at patient-adherence rates with serology of 20%–70% and cost-effective across H. pylori prevalence rates of 10%–60%.
Figure 2 Effect of adherence and prevalence.
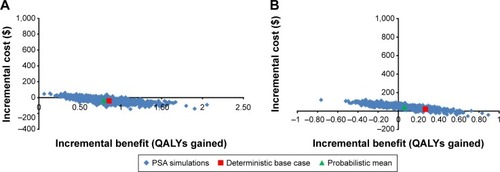
Probabilistic sensitivity analyses indicated that under uncertainty in the input parameters, the probabilities of the UBT being cost-effective compared with the FAT and serology were 1.00 and 0.58, respectively, at a willingness-to-pay threshold of $50,000/QALY gained (). Therefore, the cost-effectiveness outcomes of the UBT vs FAT did not change under uncertainty in the model parameters, whereas the cost-effectiveness outcomes of the UBT vs serology was able to change.
Discussion
The present study is the first cost-effectiveness analysis of noninvasive testing of H. pylori infection to incorporate patient-adherence information, as well as downstream costs and health outcomes (as measured by reduced QALYs) of continuing H. pylori infection, from a US perspective. Downstream costs and health outcomes were included in this analysis based on two reasons: first, the cost of testing and treating H. pylori infection (in the vicinity of hundreds of dollars) is substantially less than that of managing potential H. pylori-related long-term complications, such as peptic ulcers and GC (both of which could incur substantial management costs, including hospitalization); and second, the cost of testing and treating H. pylori infection may not be incurred again for a majority of patients, because recurrence of H. pylori in the US is <2.5%/year after successful eradication therapy.Citation21
The incorporation of patient adherence into the model is clinically important. Patients with continuing H. pylori infection due to nonadherence to the test-and-treat order by the physician will be at an increased risk of developing more severe and costly complications, such as peptic ulcers and GC. Previous studies have described patient preference for or adherence to tests based on different sample matrices. For example, it is established that the fecal occult blood test is an effective screening method for early detection of colorectal cancer.Citation22 Low patient adherence to completing the stool-sample collection, however, is also well recognized.Citation23 In an Israeli study of 2,000 men and women, only 18% of the participants sent stool samples to the testing laboratory.Citation15 Two published studies specific to H. pylori testing were identified. In a posteradication study of 29 patients with H. pylori infection, 25 (86%) returned for the UBT, but only 14 (48%) returned with a stool sample for the FAT.Citation13 Moreover, in a survey of attitudes toward H. pylori testing when serology was not available for initial diagnosis, 58% of patients preferred the UBT compared with 34% opting for the FAT.Citation14 These studies suggest that the difference in patient preference/adherence between noninvasive tests is not insignificant in routine clinical practice. Such information should thus be incorporated into pharmacoeconomic analyses involving different tests.
Decision-tree and Markov models have been used in some studies to evaluate the cost-effectiveness of H. pylori testing.Citation7–Citation11 Those studies considered similar populations (patients aged <50 or <55 years who presented with symptoms of dyspepsia, but no alarm features), and used sensitivity and specificity data, together with testing costs, as input parameters to the economic models. These studies differed, however, in whether the analyses were restricted to H. pylori testing aloneCitation8,Citation10,Citation11 or whether test and treat also was considered in the model.Citation7,Citation9 Holmes et alCitation9 concluded that the available endoscopic tests had similar costs and levels of effectiveness, whereas Elwyn et alCitation8 determined that the FAT was associated with the lowest cost and yielded a slightly higher number of true-positive test results than did the UBT. Masucci et alCitation10 evaluated the UBT as a diagnostic test and confirmatory test in a two-step strategy for positive serologic findings. The two-step strategy was costlier, but resulted in fewer false positives than did serology alone; however, it was less costly and more effective than the UBT alone. All these models used such outcomes as cost per misdiagnosis (eg, false positive and false negative), cost per correct diagnosis, appropriateness of eradication therapy given a patient’s active infection status, and cost per symptom-free year; however, none of these models incorporated long-term outcomes, such as excess LTCs and reduced QALYs associated with continuing H. pylori infection. Patient adherence was not incorporated in the models either.
The present analysis addressed the aforementioned limitations of previous studies, and demonstrated that the UBT provided the greatest economic value among the tests considered for diagnosis of H. pylori infection after adjusting for patient-adherence rates. The UBT was dominant over the FAT, increasing QALYs and reducing total costs. Moreover, the UBT substantially increased QALYs at a modest increase in cost compared with serology, and was found to be cost-effective when compared against an ICER threshold of $50,000/QALY gained. This threshold value was recently suggested to be a conservative estimate for the cost-effectiveness threshold.Citation24
Patient adherence and test performance were important determinants of the cost-effectiveness of detection and management of H. pylori infection. One-way sensitivity analysis showed that the UBT was cost-effective compared with the FAT, except when adherence to the FAT was greater than to the UBT; the UBT was cost-saving compared with serology when adherence to the UBT was the same or higher than to serology.
The prevalence of H. pylori affects the cost-effectiveness of noninvasive H. pylori tests. In the decision model by Vakil et al,Citation11 the most cost-effective strategies were as follows: at low H. pylori prevalence (30%), the FAT, followed by confirmatory testing with the UBT of positives; at intermediate prevalence (60%), the UBT, followed by the rapid urease test for negatives; and at high prevalence (90%), the UBT, followed by the rapid urease test for negatives and further confirmation with histology. In the present model, which incorporated patient adherence and used a long-term outcome, H. pylori prevalence affected ICER magnitude, but did not change the overall conclusions regarding cost-effectiveness ().
These results should be interpreted with caution, due to the assumptions in the model structure, patient populations, and input parameters used to populate the model. The primary limitation of the model results from the assumptions in parameters for which data were not available from the literature or for which only limited data were available. Although the assumptions regarding parameter estimates were confirmed as realistic by an expert clinician, it would be appropriate to update parameter estimates as additional information in the literature becomes available. The adherence rate with serology is unknown, but is of particular interest, since adherence is a significant driver of the cost-effectiveness of the UBT compared with both serology and the FATs.
Conclusion
The economic analysis conducted with this model (from the perspective of a US third-party payer) suggests that the UBT is a cost-effective alternative to other noninvasive tests, including the polyclonal and monoclonal FATs and serology. The principal drivers of the cost-effectiveness of the UBT were its higher adherence rate vs the FAT and its better performance (ie, increased sensitivity and specificity) vs serology. Notably, the higher cost of the UBT within the range of current reimbursement schemes was not a factor in the outcome of this cost-effectiveness analysis. Therefore, the UBT provided the greatest economic value among these noninvasive tests for diagnosis of H. pylori infection.
Acknowledgments
This research was fully funded by Otsuka America Pharmaceutical Inc. Editorial assistance was provided by Catherine Fontana, Geoff Marx, and Barry M Weichman, PhD of BioScience Communications, New York, and was funded by Otsuka. The abstract of this manuscript was presented as a poster presentation at the 79th annual scientific meeting of American College of Gastroenterology, in 2014. The poster abstract was published in The American Journal of Gastroenterology; 2014;109(2):s661. http://www.nature.com/ajg/journal/v109/n2s/pdf/ajg2014280a.pdf.
Supplementary material
Table S1 Estimation of excess lifetime costs associated with peptic ulcer disease
Disclosure
SHB is a former employee of Otsuka. AWM, VR, and DM are employees of RTI, which was contracted by Otsuka to conduct this study. TW is an employee of Otsuka. The authors report no other conflicts of interest in this work.
References
- CheyWDWongBCAmerican College of Gastroenterology guideline on the management of Helicobacter pylori infectionAm J Gastroenterol20071021808182517608775
- GradYHLipsitchMAielloAESecular trends in Helicobacter pylori seroprevalence in adults in the United States: evidence for sustained race/ethnic disparitiesAm J Epidemiol2012175545922085628
- KustersJGvan VlietAHKuipersEJPathogenesis of Helicobacter pylori infectionClin Microbiol Rev20061944949016847081
- PetersonWLFendrickMCaveDRPeuraDAGarabedian-RuffaloSMLaineLHelicobacter pylori-related disease: guidelines for testing and treatmentArch Intern Med20001601285129110809031
- YuanYPadolITHuntRHPeptic ulcer disease todayNat Clin Pract Gastroenterol Hepatol20063808916456574
- TalleyNJAmerican Gastroenterological Association medical position statement: evaluation of dyspepsiaGastroenterology20051291753175516285970
- CheyWDFendrickAMNoninvasive Helicobacter pylori testing for the “test-and-treat” strategy: a decision analysis to assess the effect of past infection on test choiceArch Intern Med20011612129213211570943
- ElwynGTaubertMDaviesSBrownGAllisonMPhillipsCWhich test is best for Helicobacter pylori? A cost-effectiveness model using decision analysisBr J Gen Pract20075740140317504592
- HolmesKPFangJCJacksonBRCost-effectiveness of six strategies for Helicobacter pylori diagnosis and management in uninvestigated dyspepsia assuming a high resource intensity practice patternBMC Health Serv Res20101034421176158
- MasucciLBlackhouseGGoereeRCost-effectiveness of the carbon-13 urea breath test for the detection of Helicobacter pylori: an economic analysisOnt Health Technol Assess Ser201313128
- VakilNRhewDSollAOfmanJJThe cost-effectiveness of diagnostic testing strategies for Helicobacter pyloriAm J Gastroenterol2000951691169810925969
- GisbertJPPajaresJMStool antigen test for the diagnosis of Helicobacter pylori infection: a systematic reviewHelicobacter2004934736815270750
- CullenKPBroderickBMJayaramJFlynnBO’ConnorHJEvaluation of the Helicobacter pylori stool antigen (HpSA) test in routine clinical practice – is it patient-friendly?Ir Med J20029530530612537325
- McNultyCAWhitingJWPatients’ attitudes to Helicobacter pylori breath and stool antigen tests compared to blood serologyJ Infect200755192217276512
- OreLHagoelLLaviIRennertGScreening with faecal occult blood test (FOBT) for colorectal cancer: assessment of two methods that attempt to improve complianceEur J Cancer Prev20011025125611432712
- GisbertJPPajaresJM13C-urea breath test in the diagnosis of Helicobacter pylori infection – a critical reviewAliment Pharmacol Ther2004201001101715569102
- LoyCTIrwigLMKatelarisPHTalleyNJDo commercial serological kits for Helicobacter pylori infection differ in accuracy? A meta-analysisAm J Gastroenterol199691113811448651160
- CalvetXGarcíaNLópezTGisbertJPGenéERoqueMA meta-analysis of short versus long therapy with a proton pump inhibitor, clarithromycin and either metronidazole or amoxycillin for treating Helicobacter pylori infectionAliment Pharmacol Ther20001460360910792124
- CardenasVMMullaZDOrtizMGrahamDYIron deficiency and Helicobacter pylori infection in the United StatesAm J Epidemiol200616312713416306309
- AriasECurtinLRWeiRAndersonRNU.S. decennial life tables for 1999–2001, United States life tablesNatl Vital Stat Rep200857136
- NivYHazaziRHelicobacter pylori recurrence in developed and developing countries: meta-analysis of 13C-urea breath test follow-up after eradicationHelicobacter200813566118205667
- StracciFZorziMGrazziniGColorectal cancer screening: tests, strategies, and perspectivesFront Public Health2014221025386553
- GhanouniASmithSGHalliganSPublic preferences for colorectal cancer screening tests: a review of conjoint analysis studiesExpert Rev Med Devices20131048949923895076
- NeumannPJCohenJTWeinsteinMCUpdating cost-effectiveness – the curious resilience of the $50,000-per-QALY thresholdN Engl J Med201437179679725162885
- OptumInsightThe Essential RBRVS 2014: A Comprehensive Listing of RBRVS Values for CPT and HCPCS CodesEden Prairie (MN)OptumInsight2014
- Truven Health AnalyticsRed Book2014 Available from: http://micromedex.com/redbookAccessed December 13, 2015
- KuipersEJReview article: exploring the link between Helicobacter pylori and gastric cancerAliment Pharmacol Ther199913Suppl 131110209681
- LaineLEstradaRTrujilloMKniggeKFennertyMBEffect of proton-pump inhibitor therapy on diagnostic testing for Helicobacter pyloriAnn Intern Med19981295475509758575
- DaviesRCrabbeDRoderickPGoddardJRRafteryJPatelPA simulation to evaluate screening for Helicobacter pylori infection in the prevention of peptic ulcers and gastric cancersHealth Care Manag Sci2002524925812437272
- AsakaMSepulvedaARSugiyamaTGrahamDYGastric cancerMobleyHLMendzGLHazellSLHelicobacter pylori: Physiology and GeneticsWashingtonAmerican Society for Microbiology Press2001
- ChibaNvan ZantenSJSinclairPFergusonRAEscobedoSGraceETreating Helicobacter pylori infection in primary care patients with uninvestigated dyspepsia: the Canadian adult dyspepsia empiric treatment-Helicobacter pylori positive (CADET-Hp) randomised controlled trialBMJ20023241012101611976244
- YehJMHurCKuntzKMEzzatiMGoldieSJCost-effectiveness of treatment and endoscopic surveillance of precancerous lesions to prevent gastric cancerCancer20101162941295320564399
- HowardKLordSJSpeerAGibsonRNPadburyRKearneyBValue of magnetic resonance cholangiopancreatography in the diagnosis of biliary abnormalities in postcholecystectomy patients: a probabilistic cost-effectiveness analysis of diagnostic strategiesInt J Technol Assess Health Care20062210911816673687
- ErstadBLCost-effectiveness of proton pump inhibitor therapy for acute peptic ulcer-related bleedingCrit Care Med2004321277128315187506
- YouJHTsuiKKWongRSChangGCost-effectiveness of dabigatran versus genotype-guided management of warfarin therapy for stroke prevention in patients with atrial fibrillationPLoS One20127e3964022745801
- YabroffKRLamontEBMariottoACost of care for elderly cancer patients in the United StatesJ Natl Cancer Inst200810063064118445825
- SlawskyKCyrPLOlchanskiNHowdenCWCost-effectiveness of diagnostic strategies for H. pylori infection in a high prevalence populationGastroenterology2011140Suppl 1S203