Abstract
Introduction
Self-stigma plays a role in many areas of the patient’s life. Furthermore, it also discourages therapy. The aim of our study was to examine associations between self-stigma and adherence to treatment and discontinuation of medication in patients from various diagnostic groups.
Methods
This cross-sectional study involved outpatients attending the Department of Psychiatry, University Hospital Olomouc, Czech Republic. The level of self-stigma was measured with the Internalized Stigma of Mental Illness and adherence with the Drug Attitude Inventory. The patients also anonymously filled out a demographic questionnaire which included a question asking whether they had discontinued their medication in the past.
Results
We examined data from 332 patients from six basic diagnostic categories (substance abuse disorders, schizophrenia, bipolar disorders, depressive disorders, anxiety disorders, and personality disorders). The study showed a statistically significant negative correlation between self-stigma and adherence to treatment in all diagnostic groups. Self-stigma correlated positively and adherence negatively with the severity of disorders. Another important factor affecting both variables was partnership. Self-stigma positively correlated with doses of antidepressants and adherence with doses of anxiolytics. Self-stigma also negatively correlated with education, and positively with a number of hospitalizations and number of psychiatrists visited. Adherence was further positively correlated with age and age of onset of disorders. Regression analysis showed that self-stigma was an important factor negatively influencing adherence to treatment and significantly contributing to voluntary discontinuation of drugs. The level of self-stigma did not differ between diagnostic categories. Patients suffering from schizophrenia had the lowest adherence to treatment.
Conclusion
The study showed a significant correlation between self-stigma and adherence to treatment. High levels of self-stigma are associated with discontinuation of medications without a psychiatrist’s recommendation. This connection was present in all diagnostic groups.
Introduction
Stigma refers to a social phenomenon whereby the public has a negative view of individuals with attributes perceived by the general population as inferior, threatening, or having other negative connotations. An integral part of the process is unequal treatment of such individuals. The most important correlates of stigma include mental diseases.Citation1 Self-stigma, or internalized stigma, is a gradual process in which a person (eg, a psychiatric patient) is uncritically adopting negative societal prejudices about attributes discredited by others.Citation2 Five principal areas of internalized stigma are operationally defined by the Internalized Stigma of Mental Illness (ISMI) questionnaire, described in detail in the “Methods” section.
The lay public is only vaguely aware of the nature of mental disorders and tends to stigmatize psychiatric patients irrespective of the severity of their conditions. Having a psychiatric diagnosis is stressful for both patients and their families. Patients are concerned about the prejudices of those around them and often deny their disorders and delay seeking or starting adequate psychiatric care. Barney et al proved that the effort to avoid stigma is the most important obstacle to receiving help.Citation3
Patients are usually well aware of stereotypes that society holds about people receiving psychiatric care and are concerned about them. Anxiety about potential stigma increases in those who have a greater tendency toward self-stigma.Citation4 The consequences may be even more serious than in the case of stigmatization by others. An individual expecting rejection or condemnation by others tends to be socially withdrawn.Citation5 Outpatients who have adopted prejudices about psychiatric patients have less belief that their mental state will improve, are more depressed, and show more negative self-esteem.Citation6 Our previous studyCitation7 on patients with anxiety disorders, depressive, and personality disorders showed that individuals with higher levels of self-stigma preferred avoidance stress-coping strategies, such as a tendency to give up prematurely when solving a problem (behavioral resignation) or stopping substance abuse. Stigma itself may interfere with mental well-being when patients feel extremely nervous and constantly check the external signs of their nervousness (“so that others do not see me as a nutcase”). Our current study examined the levels of stigma and their relationship to treatment adherence and discontinuation of prescribed medications in psychiatric outpatients with various diagnoses.
Methods
Participation in the study was offered to all outpatients coming for check-ups at the Department of Psychiatry, University Hospital Olomouc between July 1 and September 30, 2013. Apart from attending regular outpatient check-ups, the patients were treated with standard medications in accordance with their diagnosis, current guidelines,Citation8 and good clinical practice.
Study inclusion criteria
Included in the study were patients who met the following criteria: 1) willingness to fill out questionnaires; 2) age between 18 and 55 years; and 3) stabilized mental disorder (the patient is able to attend outpatient treatment). The exclusion criteria were as follows: 1) mental retardation; 2) organic mental disorder; and 3) acute condition requiring hospitalization or crisis intervention.
The diagnosis was made by an experienced physician in accordance with the ICD-10 criteriaCitation9 and confirmed by an independent examiner using the patient records.
Assessment instruments
ISMI
ISMICitation10 is a 29-item instrument with a 4-point scale that measures internalized stigma within five topic areas. These include alienation or the patient’s feelings of being less than a full member of society, stereotype endorsement or the degree to which the individual agrees with stereotypes about people with mental illness, perceived discrimination or the patient’s perception of the way other people treat him or her, social withdrawal, and the degree of stigma resistance. Given the absence of the Czech version, the instrument was translated by Dostálová and Dostál (unpublished material). Cronbach’s alpha for the entire translated scale was 0.9, with the individual subscales having higher internal consistency than the original subscales.Citation11 In the original English version, exploratory factor analysis identified five factors explaining 67% of the variance. The stereotype endorsement subscale was divided into two factors while stigma resistance did not have its own factor. This is consistent with the finding that stigma resistance is a conceptually distinct entity and factor analysis should, therefore, include only the four remaining subscales.Citation12 No norms are available for the method. In our institution, the internal consistency of the Czech translation was determined in 346 patients, with Cronbach’s alpha being 0.963 and split-half 0.905.Citation13
Drug Attitude Inventory
Drug Attitude Inventory 10 (DAI-10Citation14) is a questionnaire created to measure patients’ attitudes toward medications. The patient decides whether statements about drugs are true or false. The statements are concerned with drug effectiveness, necessity, and adherence. The instrument assesses the current attitudes toward medications, not whether the patients discontinued their medication in the past.
Clinical Global Impression
Clinical Global Impression (CGICitation15) is an instrument for overall assessment of the severity of psychopathology based on a comprehensive assessment of the patients’ condition by their physician. Its subjective version (CGI-S) is self-rated on a 7-point scale of severity, with each point characterized by a description.
Demographic questionnaire
Contains basic information, such as sex, age, employment status, marital status, pension income, education, age of illness onset, overall time of attending the outpatient center, number of hospitalizations, time elapsed since the last hospital stay, number of psychiatrists visited, current medication, and information about discontinued medication in the past (either on recommendation of a psychiatrist or by one’s own will).
Statistical evaluation
The results were processed with the statistical software Prism 3 (GraphPad Software Inc, La Jolla, CA, USA). Demographic data and mean total scores in the individual questionnaires and CGI scales were assessed using descriptive statistics to identify the mean, median, standard deviation, and the character of data distribution. The relationships between individual categories were assessed by correlation coefficients and linear regression. The relationships between alternative variables (sex, marital status, and discontinuation of medication) were assessed by the Fisher’s test. To test for differences among patient subgroups, one-way analysis of variance was used for parametric distribution of data and Kruskal–Wallis test for groups with nonparametrically distributed data. A 5% level of significance was adopted for all statistical tests.
Since individual factors determined by correlation statistics may interfere with one another, stepwise linear (ISMI and adherence) and logistic (discontinued medication in the past) regression methods were used to identify the most important factors. The model was created in two or three steps. The statistical analysis included the following variables: ISMI scores, adherence to treatment assessed by DAI-10, voluntary discontinuation of medication, diagnosis, age, age of illness onset, employment status, education, objective CGI (CGI-O), number of visited psychiatrists, use of antidepressants, anxiolytics, and antipsychotics.
The study was approved by the ethics committee of University Hospital Olomouc. The research was conducted in accordance with the latest version of the Helsinki Declaration and Guideline for Good Clinical Practice.Citation16 The participants gave informed written consent.
Results
Sample characteristics
The questionnaires were offered to a total of 1,162 patients attending our psychiatry department outpatient center. Included in the study were 332 (28.57%) patients who filled out at least two of the questionnaires. The sample comprised 171 females (51.5%). All four questionnaires were completed by 263 patients (28.6%). The reasons for not completing the questionnaires were varied; mostly lack of time, reluctance or self-proclaimed inability to fill out the questionnaires, or absence of corrective appliances (glasses). For sample characteristics, see .
Table 1 Sample characteristics
Antidepressants were used by 241 patients, antipsychotics by 117, anxiolytics by 74, and mood stabilizers or anti-convulsants by 36 patients. The mean daily doses were 36.54±22.95 mg (paroxetine index) for antidepressants, 13.49±35.77 mg (diazepam index) for anxiolytics, and 3.47±11.21 mg (risperidone index) for antipsychotics. A total of 124 patients (37.35%) admitted they had discontinued their medication previously. As for marital status, 131 patients (39.46%) were single, 128 (38.55%) were married, 62 (18.67%) were divorced, and eleven (3.31%) were widowed. A total of 140 patients (42.17%) had a positive family psychiatric history. The achieved education levels were as follows: primary (40; 12.05%), vocational (87; 26.20%); secondary (128; 38.55%); and tertiary (76; 22.89%). Patients were diagnosed according to ICD-10.Citation9 Fifty-eight patients were diagnosed with substance abuse, 62 with schizophrenia, 14 with bipolar disorder, 57 with depressive disorder, 120 with anxiety and neurotic disorders, and 21 patients with personality disorder.
Self-stigma, adherence, and discontinuation of medication in the entire sample: relation to demographic variables
Sex
The mean level of self-stigma assessed with ISMI was 61.08±14.54 for the entire sample. There was no statistically significant difference in self-stigma between males and females (). Similarly, there were no statistically significant differences in adherence to treatment and frequency of discontinuation of medication between the sexes ().
Table 2 Self-stigma, adherence, and discontinuation of medication in the entire sample in relation to sex, education, and partnership status
Education
The mean level of self-stigma tended to decrease with higher levels of education (). One-way analysis of variance showed statistically significant differences in self-stigma levels between subgroups with different education levels. However, Tukey’s post hoc test for multiple comparisons failed to show a statistically significant difference. Despite the fact that the mean current level of adherence increased with higher education, the statistical analysis showed no difference (). Moreover, there was no statistically significant difference in past discontinuation of medication with regard to education ().
Partnership status
Patients living without a partner had statistically significantly higher levels of self-stigma than those having partners (). Moreover, patients without a partner showed significantly lower adherence to treatment (). However, the two groups did not differ in the frequency of voluntary discontinuation of medication in the past ().
Age and age of illness onset
The levels of self-stigma expressed by the total ISMI scores did not significantly correlate with either age or age of disorder onset. By contrast, the levels of adherence to treatment were statistically significantly correlated with these variables (P<0.005). That is, the lower the patient’s age and age of illness onset, the lower the DAI-10 score and adherence to treatment.
Number of hospitalizations, time elapsed since the last hospital stay, and number of visited psychiatrists
The level of self-stigma as assessed with the ISMI did not significantly correlate with time elapsed since the last hospital stay. However, there was a statistically significant positive correlation between the number of previous hospitalizations (P<0.0001) as well as the number of outpatient psychiatrists visited in the past (P<0.0001). On the other hand, current adherence to treatment was not related to the number of hospital stays, time from the last hospital stay, or the number of psychiatrists visited in the past.
Higher numbers of visited psychiatrists increased the chance that patients voluntarily discontinued their medication by a factor of 1.174 (95% CI 1.004–1.327; P=0.044).
Medication
The levels of self-stigma expressed by the total ISMI scores were statistically significantly positively correlated with the doses of antidepressants (P<0.0001) but not anxiolytics or antipsychotics. Current adherence to treatment assessed with the DAI-10 questionnaire was statistically significantly correlated with doses of anxiolytics (P<0.05).
Linear regression analysis showed that the most important predictor of the total ISMI score was the use of antipsychotics. Patients taking antipsychotics had significantly higher total ISMI scores (P=0.007). In the case of current adherence levels, the use of antidepressants was identified as their predictor. In patients using antidepressants, the levels of current adherence increased (P=0.002). The use of antidepressants was associated with the chances of medication discontinuation by a factor of 0.416 (95% CI 0.242–0.715), P<0.005.
Self-stigma, adherence, and discontinuation of medication in the entire sample: relation to the questionnaires
The level of self-stigma as expressed by the total ISMI score was statistically significantly positively correlated with CGI-S and CGI-O scores and significantly negatively correlated with the current level of adherence (P<0.0001) (). In other words, the more self-stigmatized the patients were, the lower their current adherence to treatment and the more severe their condition.
Figure 1 Linear regression between total ISMI scores and adherence.
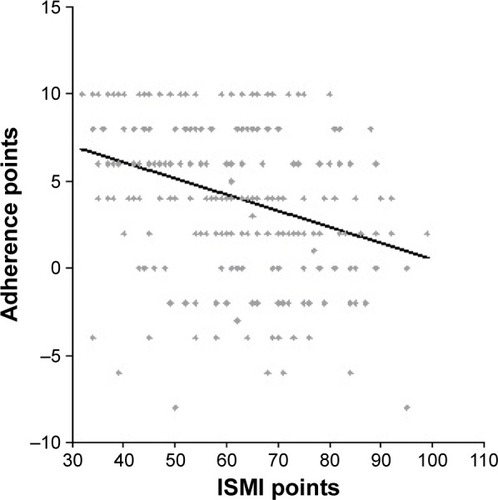
Linear regression analysis showed that the most important predictors of the total ISMI score were CGI-O and the current level of adherence. An increase in CGI-O was related to an increase in ISMI scores (P<0.0001). Conversely, increased current adherence predicted lower total ISMI scores (P<0.0001). Logistic regression analysis showed that an important parameter for predicting voluntary discontinuation of medication was the total ISMI score. Higher self-stigma levels increased the chances of voluntary discontinuation of medication by a factor of 1.09 (95% CI 1.0004–1.037; P<0.05).
Linear regression F=29.43, DFn, DFd=1.000, 256.0 P<0.0001.
When comparing the total ISMI scores in patients who had voluntarily discontinued their medication in the past (n=108; ISMI=63.62±14.55) and those who had not (n=169; ISMI=59.46±14.35), the difference in self-stigma levels was statistically significant; that is, patients who had voluntarily discontinued their medication showed higher self-stigma levels.
Self-stigma, adherence, and discontinuation of medication in individual diagnostic categories
There were no statistically significant differences in the mean ISMI scores between individual diagnostic categories ().
Table 3 ISMI scores for individual diagnostic categories
There were differences in the mean levels of current adherence between the diagnostic categories (). Statistical comparison of the levels of current adherence with the Kruskal–Wallis test showed that the differences were statistically highly significant. Post hoc analysis of differences between individual categories showed a statistically significant difference (P<0.001) in the mean adherence levels between schizophrenic patients and those with depressive disorder, with the adherence level being significantly higher in the latter subgroup.
Table 4 Levels of adherence in individual diagnostic categories
There were differences in the frequency of discontinuation of medication between the diagnostic categories. The highest and lowest percentages of those who voluntarily discontinued their medication were seen among bipolar and depressive patients, respectively. However, the differences were not statistically significant when all the categories were compared ().
Discussion
The study comprising 332 psychiatric outpatients with a wide spectrum of diagnoses assessed the relationship between self-stigma and current adherence to treatment, assessed with the DAI-10 questionnaire and self-reported voluntary discontinuation of medication in the past.
The present study showed that lower self-stigma levels were linked to better adherence. The finding is consistent with studies by other authors.Citation17–Citation19 This underlines the importance of interventions aimed at lowering the levels of self-stigma in patients.
Those patients who admitted that they had voluntarily discontinued their medication in the past showed significantly higher self-stigma levels than those who had not (or did not admit that they had). The finding is consistent with the results of a study showing that depressive patients perceiving more stigma tended to discontinue or interrupt their treatment.Citation20–Citation23
Regression analysis showed that the level of self-stigma was associated with both current adherence to treatment and discontinuation of medication in the past without psychiatrists’ recommendations; the other factors were suppressed by the analysis. Thus, it may be assumed that the level of self-stigma may considerably influence the patient’s therapy and should be noted not only by psychotherapists but also by all psychiatrists prescribing drugs to their patients.
Factors influencing adherence to treatment have been investigated mainly in patients with physical illnesses.Citation24 The only mental disorder factor shown to affect adherence to treatment was the level of depression.Citation25 The present study showed no differences concerning the relationship between current adherence and demographic data with respect to sex. Findings regarding the effect of sex have been inconsistent. Better adherence to treatment in females has only been shown in one study.Citation26
Despite the fact that patients with tertiary education had the highest mean scores of adherence in the present study, the differences between the subgroups were not statistically significant. This finding is in contrast with both our hypotheses and other studies.Citation27,Citation28 The discrepancy may be explained by the smaller proportion of patients with primary education.
Additionally, the level of current adherence to treatment was correlated with patients’ age, with older patients showing better adherence. The level of adherence tended to increase with the later onset of diseases and higher doses of anxiolytics; however, there was a negative association with both subjective and objective clinical impression. Living with a partner was associated with better adherence in HIV patients.Citation29 Patients living without a partner had significantly lower adherence to treatment than those having a partner, which is consistent with other studies.Citation30 Thus, lower adherence may be expected in younger patients, living without a partner, with early-onset diseases, and generally more severe conditions; once again, the direction of causality is difficult to ascertain from the data. Unlike self-stigma, patients in various diagnostic categories may have different levels of adherence to treatment. The present study showed that patients diagnosed with schizophrenia had lower current adherence than those with depressive disorder. Although adherence has been investigated in patients with both depressionCitation31,Citation32 and schizophrenia,Citation33,Citation34 none of the studies used the DAI-10 questionnaire. The association was not found in the other diagnostic categories; however, the subgroups of patients with bipolar disorder and personality disorder were not large enough to confirm the relationship.
When assessing current adherence to treatment with regard to various groups of drugs, an association was found between adherence and doses of anxiolytics. Adherence to various groups of drugs was studied by Bulloch and Patten.Citation35 Nonadherence ranged from 34.6% for antipsychotics to 45.9% for antidepressants. For anxiolytics, nonadherence was 38.1%. The discrepancy between the studies may be explained by the fact that Bulloch and PattenCitation35 used a mail survey to ask patients if they had failed to take their pills and why, whereas the present study used the DAI-10 questionnaire to evaluate adherence. There was also a major difference in the percentages of anxiolytic users. Anxiolytics were prescribed to 1.1% of subjects in the study by Bulloch and PattenCitation35 but to as many as 22.3% of patients in the present study.
There was no difference in discontinuation of medication in the past between the sexes, which is consistent with Bulloch and Patten.Citation35 Bulloch and PattenCitation35 admitted voluntary discontinuation of medication in the past was not significantly different when comparing patients living with and without a partner or those with various levels of education. The present study also failed to show that voluntary discontinuation of medication in the past was influenced by the diagnostic category. No studies directly comparing the likelihood of discontinuation of medication in patients of various diagnostic categories have been found in the available databases. However, it may be speculated that the negative finding may be mainly due to the small number of patients. Another question is how valid such self-reported data are.
The study analyzed whether self-stigma was dependent on demographic data. The findings suggest that sex played no role in perceiving oneself as ill. The findings are inconsistent with those reported by some other authors. A study by Brohan et alCitation36 investigating 1,229 patients with schizophrenia in 14 European countries showed higher levels of self-stigma in females. Similarly, Girma et alCitation37 reported significantly higher self-stigma levels assessed with the ISMI in females than in males. However, there is a study that failed to confirm the relationship between sex and age.Citation38 This may be due to the fact that the studies were carried out in different years, different countries with various sociocultural background, and different groups of patients. Another explanation may be that various scales were used for assessing the levels of self-stigma.
The present study showed a statistically significant relationship between the level of self-stigma and the level of education. This association was found by numerous studies carried out in other populations. Ustündağ and KesebirCitation39 used the ISMI in Turkish bipolar patients to find that self-stigma was more frequent in those with low socioeconomic status, low education level, rural residence, lack of work, and more children. Girma et alCitation37 found an inverse correlation between the level of education and the level of self-stigma assessed with the ISMI in 422 patients with severe mental illness in Ethiopia, and Temilola et alCitation40 in 256 patients in Nigeria. Similarly, Werner et alCitation41 found lower levels of self-stigma assessed with the ISMI in geriatric depressive patients in Israel with higher education than in those with lower education levels. This finding was confirmed in a study by Lv et alCitation42 on the association between self-stigma and the level of education in Chinese patients with schizophrenia. Given the fact that a review and meta-analysis of 127 articles on stigma and self-stigma, mostly in developed countries,Citation5 failed to show a significant relationship between demographic factors and self-stigma, the inconsistency between the above studies and the present results may be explained by cultural differences.
Patients living without partners showed significantly higher levels of self-stigma than those having partners. It may be assumed that individuals who stigmatize themselves are less likely to build or maintain a relationship or vice versa, that is, people who are alone tend to stigmatize themselves. We consider the latter to be more likely. For humans, it is natural to live in a partnership. Inability to find a partner or to maintain a relationship, unrequited love, or feelings of loneliness may be interpreted by patients as the price they pay for their illness and may contribute to self-stigma. To the best of our knowledge, no study on the link between psychiatric patients’ self-stigma and partnership is available in the databases.
It also seems that the more exposed the patients are to hospitals or health facilities, the more they stigmatize themselves. We speculate that the explanation lies in the deeply rooted term “madhouse” for a psychiatric hospital and the general stereotype that psychiatric patients are hospitalized mainly because they are aggressive. Another explanation for the association between the level of self-stigma and number of hospitalizations may be that more self-stigmatized patients have more severe illnesses and thus need more frequent hospital stays. Once again, this statement could not be confirmed by available studies. Longitudinal prospective studies will be required to test this and similar hypotheses.
The level of self-stigma has also been shown to be associated with the severity of illness evaluated both objectively by psychiatrists and subjectively by the patients themselves. A similar link between the severity of a psychopathology and level of self-stigma was reported in the review and meta-analysis of 127 articles by Livingston and Boyd.Citation5 From our data, it is unclear whether the severity of illness leads to a higher level of self-stigma or whether the higher level of self-stigma contributes to the perceived severity of illness. The level of self-stigma is also associated with the number of outpatient psychiatrists visited in the past. Perhaps patients with higher self-stigma levels responding more poorly to treatment perceive their illness subjectively as more severe and thus understandably seek help from more psychiatrists. The fact that self-stigma levels are negatively associated with antidepressant doses may be linked to a better control of depressive experience. This assumption, which cannot be confirmed based on our data as the level of depression was not specifically evaluated, may be a subject of further investigation.
Despite the existence of studies of patients with schizophrenia on the association between medication and self-stigma levels,Citation43–Citation45 specific differences between individual groups of drugs have not been investigated.
Limitations of the study
One of the study’s limitations is the fact that most data were obtained using self-reported questionnaires. Thus, with the exception of demographic data, objective CGI scores, and medication doses, the data could be modified by various motivations of the patients. Moreover, some patients filled in only certain parts of the questionnaires. The most important limitation of the study is the insufficient number of participants in the subgroups of bipolar and personality disorders.
Conclusion
The study results suggest that the level of self-stigma may be a very important factor associated with low adherence to treatment and discontinuation of medication in patients with mental diseases irrespective of the diagnostic category. Of particular interest is also the finding that there were no differences in the level of self-stigma among the diagnostic categories. This is in contrast with expectations of many specialists who expect a higher level of self-stigmatization in patients suffering from severe mental illnesses (schizophrenia, bipolar disorder). If the results are confirmed by future studies, adherence may be increased by applying promising strategies to reduce self-stigma. These strategies may be implemented through systematic psychoeducation of patients or in the course of psychotherapy.
Disclosure
The authors report no conflicts of interest in this work.
References
- LinkBGPhelanJCBresnahanMStueveAPescosolidoBAPublic conceptions of mental illness: Labels, causes, dangerousness, and social distanceAm J Public Health19998991328133310474548
- CorriganPWRafaczJRüschNExamining a progressive model of self-stigma and its impact on people with serious mental illnessPsychiatry Res2011189333934321715017
- BarneyLJGriffithsKMChristensenHJormAFExploring the nature of stigmatising beliefs about depression and help-seeking: implications for reducing stigmaBMC Public Health200996119228435
- RüschNAngermeyerMCCorriganPWMental illness stigma: concepts, consequences, and initiatives to reduce stigmaEur Psychiatry200520852953916171984
- LivingstonJDBoydJECorrelates and consequences of internalized stigma for people living with mental illness: a systematic review and meta-analysisSoc Sci Med2010712150216121051128
- RitsherJBPhelanJCInternalized stigma predicts erosion of morale among psychiatric outpatientsPsychiatry Res2004129325726515661319
- OciskováMPraškoJLátalováKInternalizované stigma a efektivita farmakoterapie a psychoterapie u úzkostných poruch a poruch neurotického spektra. [Internalized stigma and efficacy of pharmacotherapy and psychotherapy in anxiety disorders and neurotic spectrum disorders]Česká a Slovenská Psychiatrie2014b1103133143
- RabochJUhlikováPHellerováPAndersMŠustaMPsychiatrie: Doporučené postupy v psychiatrické péče. [Psychiatry: Treatment guidelines] Psychiatrická společnost]ČLS JEP
- World Health Organization (WHO)ICD-10: The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic GuidelinesGenevaWord Health Organization1992
- BoydJEAdlerEPOtilingamPGPetersTInternalized Stigma of Mental Illness (ISMI) scale: A multinational reviewCompr Psychiatry201455122123124060237
- RitsherJBOtilingamPOGrajalesMInternalized stigma of mental illness: psychometric properties of a new measurePsychiatry Res2003121314914572622
- LysakerPHRoeDYanosPTToward understanding the insight paradox: Internalized stigma moderates the association between insight and social functioning, hope, and self-esteem among people with schizophrenia spectrum disordersSchizophr Bull200733119219916894025
- OciskovaMPraskoJDostalovaLSelf-stigma in psychiatric patients – standardization of the ISMI scaleNeuro Endocrinol Lett201435762463225617887
- HoganTPAwadAGEastwoodRA self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validityPsychol Med19831311771836133297
- GuyWECDEU Assessment Manual for PsychopharmacologyRockville, MDU.S. DHEW1976
- EMEA2002 Available from: http://www.ema.europa.eu/pdfs/human/ich/013595en.pdfAccessed March 20, 2009
- TsangHWFungKMChungRCSelf-stigma and stages of change as predictors of treatment adherence of individuals with schizophreniaPsychiatry Res20101801101520493552
- FungKMTsangHWChanFSelf-stigma, stages of change and psychosocial treatment adherence among Chinese people with schizophrenia: a path analysisSoc Psychiatry Psychiatr Epidemiol201045556156819649752
- LyimoRAStutterheimSEHospersHJde GleeTvan der VenAde BruinMStigma, disclosure, coping, and medication adherence among people living with HIV/AIDS in Northern TanzaniaAIDS Patient Care STDS20142829810524517541
- SireyJABruceMLAlexopoulosGSPerceived stigma as a predictor of treatment discontinuation in young and older outpatients with depressionAm J Psychiatry200115847948111229992
- SireyJABruceMLAlexopoulosGSPerlickDAFriedmanSJMeyersBSStigma as a barrier to recovery: Perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherencePsychiatr Serv200152121615162011726752
- SireyJABruceMLAlexopoulosGSPerceived stigma as a predictor of treatment discontinuation in young and older outpatients with depressionAm J Psychiatry2001158347948111229992
- SireyJABruceMLAlexopoulosGSThe treatment initiation program: an intervention to improve depression outcomes in older adultsAm J Psychiatry2005162118418615625220
- DiMatteoMRVariations in patients’ adherence to medical recommendations: a quantitative review of 50 years of researchMed Care200442320020915076819
- DiMatteoRMLepperHSCroghanTWDepression is a risk factor for noncompliance with medical treatmentArch Intern Med20001602101210710904452
- BlouinAPerezEMinolettiACompliance to referrals from the psychiatric emergency roomCan J Psychiatry1985301031063995453
- KalichmanSCRamachandranBCatzSAdherence to combination antiretroviral therapies in HIV patients of low health literacyJ Gen Intern Med199914526727310337035
- LastCGThaseMEHersenMBellackASHimmelhochJMPatterns of attrition for psychosocial and pharmacologic treatments of depressionJ Clin Psychiatry1984463613664030699
- PowerRKoopmanCVolkJSocial support, substance use, and denial in relationship to antiretroviral treatment adherence among HIV-infected personsAIDS Patient Care2003175245252
- MatasMStaleyDGriffinWA profile of the noncompliant patient: a thirty-month review of outpatient psychiatry referralsGen Hosp Psychiatry1992141241301592248
- MelfiCAChawlaAJCroghanTWHannaMPKennedySSredlKThe effects of adherence to antidepressant treatment guidelines on relapse and recurrence of depressionArch Gen Psychiatry19985512112811329862557
- LingamRScottJTreatment non-adherence in affective disordersActa Psychiatr Scand2002105316417211939969
- BabikerIENoncompliance in schizophreniaPsychiatr Dev198643293372883650
- GilmerTPDolderCRLacroJPAdherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophreniaAm J Psychiatry200416169269915056516
- BullochAGMPattenSBNon-adherence with psychotropic medications in the general populationSoc Psychiatry Psychiatr Epidemiol2010451475619347238
- BrohanEElgieRSartoriusNThornicroftGSelf-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: The GAMIAN-Europe studySchizophrenia Res20101221–3232238
- GirmaETesfayeMFroeschlGMöller-LeimkühlerAMDehningSMüllerNFacility based cross-sectional study of self stigma among people with mental illness: towards patient empowerment approachInt J Ment Health Syst2013712124004512
- YenCFChenCCLeeYTangTCYenJYKoCHSelf-stigma and its correlates among outpatients with depressive disordersPsychiatr Serv200556559960115872170
- UstündağMFKesebirSInternalized stigmatization in bipolar patients: relationship with clinical properties, quality of life and treatment complianceTurk Psikiyatri Derg201324423123924310089
- TemilolaMJAdegokeAOOlaoluATAdegboyegaOOlaideAKSelf-stigma, quality of life and schizophrenia: An outpatient clinic survey in NigeriaInt J Soc Psychiatry201460437738623828766
- WernerPStein-ShvachmanIHeinikJPerceptions of self-stigma and its correlates among older adults with depression: A preliminary studyInt Psychogeriatr20092161180118919586565
- LvYWolfAWangXExperienced stigma and self-stigma in Chinese patients with schizophreniaGen Hosp Psychiatry2013351838822925273
- FungKMTTsangHWHCorriganPWSelf-stigma of people with schizophrenia as predictor of their adherence to psychosocial treatmentPsychiatr Rehabil J200832485495
- TsangHWFungKMChungRCSelf-stigma and stages of change as predictors of treatment adherence of individuals with schizophreniaPsychiatry Res20101801101520493552
- KrankeDAFloerschJKrankeBOMunsonMRA qualitative investigation of self-stigma among adolescents taking psychiatric medicationPsychiatr Serv201162889389921807828

