Abstract
Purpose
Mindfulness-based cognitive therapy (MBCT) could be an intervention for improving subjective well-being among healthy individuals (HIs). However, MBCT studies for HIs to improve their subjective well-being are rare. The aim of this study was to report the feasibility, safety and effectiveness of MBCT for HIs in comparison with clinical samples.
Patients and Methods
We conducted a single-arm, pre-post comparison pilot study offering MBCT to both HIs and people with common mental disorders. Twenty-four participants in total were included in the study. Eight weekly two-hour sessions with six monthly boosters were offered to all participants. Assessment was carried out at baseline, week 4, 8, and during follow-up. The 5-item World Health Organization Well-Being Index (WHO-5) was the primary clinical outcome measure.
Results
The results showed the MBCT is sufficiently safe and would be more feasible in HIs compared to in clinical samples (attendance rate: 81.5% vs 61.3%, p=0.06). Although Satisfaction with Life Scale, the other scale of subjective well-being used, improved significantly at week 20 (p=0.01), no significant improvement was seen in WHO-5. The results of the sub-group analysis revealed WHO-5 improved significantly at week 8 and 32 among the subjects whose baseline scores began in the lower half.
Conclusion
MBCT is sufficiently safe and would be more feasible with HIs compared to the clinical samples. In designing randomized controlled trials, selecting HIs with lower subjective well-being would be reasonable to minimize the “ceiling effect” on outcomes.
Introduction
Numerous studies have endorsed Mindfulness Based Cognitive Therapy’s (MBCT’s) effectiveness on negative symptoms of clinical populations.Citation1–Citation3 The theoretical model indicates MBCT increases cognitive reappraisal and decreases expressive suppression strategies. This leads to a decrease in depressive and anxiety symptoms and to an increase in psychological well-being. However, whether such a mechanism would also work for healthy individuals (HIs) is not yet known. Subjective well-being for HIs is significant because previous studies revealed that better subjective well-being contributes to better health conditions, including higher quality of life, less stress,Citation5 and longer life expectancy.Citation6–Citation8 However, there is little research examining whether MBCT improves subjective well-being of HIs in the long term. Therefore, in anticipation of future Randomized Controlled Trials (RCTs), we decided to conduct a pilot study for HIs in parallel with clinical samples to assess feasibility, safety, and effectiveness of MBCT, and compare these results with those of clinical samples.
Materials and Methods
Design
The design of the study was a single-arm, pre-post comparison study. The participants consisted of HIs, and people with common mental disorders (CMDs). The same MBCT was offered to all participants in a mixed group.
Ethics Approval and Consent to Participate
The study was approved by the Institutional Review Board of the Keio University School of Medicine and was registered at the University Hospital Medical Information Network Clinical Trials Registry (registry ID: UMIN000022528, URL: https://upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000025928). The study was conducted and reported in conformance with the STROBE Statement.Citation9 This study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2008.
Procedure
The participants were recruited between May 2016 and February 2017 via the website of the Keio Center for Stress Research for HIs, and at Keio University Hospital for the people with CMDs. After an application from the candidates, one of the research investigators assessed their eligibility for the study. The separate inclusion/exclusion criteria were applied, respectively, as described in Participants section. The groups were not matched (eg age, gender, etc.). After providing written consent, all participants were offered an eight-week MBCT intervention, followed by six monthly follow-up sessions. Assessment was carried out at five time points: before the intervention (T1), at four weeks after the start of the program (T2), at the end of the program (week 8, T3), at three months and six months after completion of the intervention (T4 and T5).
Participants
HIs were included in the study if they (1) had no history of mental illness or had a history of mental illness that was followed by a recovery period of longer than 2 years, (2) had no severe physical illness hindering participation in the study, (3) were aged between 20 and 65, and (4) were able to submit written informed consent. Eligible participants were excluded if they were judged to have (1) difficulty in following up for eight months or (2) a history of previous mindfulness-based intervention (MBI). Patients were included in the comparison group, if they (1) met at least one of any diagnosis based on the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition Axis I Disorders including anxiety disorder (panic disorder with/without agoraphobia, social anxiety disorder, obsessive-compulsive disorder), adaptation disorder, or major depressive disorder (remitted for longer than 6 months); (2) were aged between 20 and 65 years; (3) submitted written informed consent. Candidate participants were excluded when they had (1) difficulty in following up for eight months; (2) a history of previous MBI; (3) severe physical disorders restricting participation in the study; (4) a history of substance use disorder, alcoholism, or antisocial personality disorder; (5) marked suicidal thoughts or self-injurious behavior; or (6) organic cerebral lesions.
Intervention
The intervention used in the study was MBCT, developed by Segal et al.Citation10 The program consists of psychological education, meditation, yoga, and group discussion. Because MBCT was originally designed to target depression relapse prevention, we added minor modifications to the original program to focus on improving subjective well-being. The program contents and the parts modified are described in .
Table 1 Contents of the Program
As in the original MBCT, we ran eight weekly two-hour-long sessions. Monthly booster sessions were provided during a six-month follow-up period. Between the weekly sessions, the participants were assigned daily homework, such as meditation, yoga, or activity records. We did not assign any regular homework during the follow-up period. Instead, we asked participants to send short essays about their daily practice every two to three months to share their experiences among other participants. The program was mainly run by MS with more than five years’ experience of mindfulness practice, with assistance from AK and TK with three years and one year experience of mindfulness practice, respectively.
Outcomes
Feasibility and Safety
Feasibility and safety of the program was evaluated by the session attendance rate and incident rate of the critical adverse events during the program period.
Clinical Outcomes
The primary clinical outcome was subjective well-being, as measured by the 5-item World Health Organization Well-Being Index (WHO-5).Citation11 WHO-5 is one of the most widely used questionnaires for assessing affective aspects of subjective well-being. Scores on the scale range between 0 and 25. Higher scores indicate a higher level of affective well-being.
We also assessed 11 scalesCitation12–Citation25 as the secondary clinical outcomes as shown in and and Tables S1 and S2. Due to space restrictions, we only report the results of the WHO-5 (primary outcome), Satisfaction with Life Scale (SWLS), and Five Facet Mindfulness Questionnaire (FFMQ) in and . We extracted WHO-5 and FFMQ among the secondary outcomes because SWLS is the other aspect of the subjective well-being and FFMQ is a direct scale to assess mindfulness skills.
Table 2 Baseline Sociodemographic Characteristics and Diagnosis
Table 3 Attendance Frequency to the Sessions
Table 4 Outcomes Score at Each Assessment Point with Comparison to Baseline (Healthy Individuals)
Table 5 Outcomes Scores at Each Assessment Point with Comparison to Baseline (People with Common Mental Disorders)
Satisfaction with Life Scale (SWLS): The SWLS has 5 questions. The scale focuses on assessing one’s life satisfaction, which is cognitive aspect of subjective well-being. Scores on the scale range from 5 to 35.Citation12
Five Facet Mindfulness Questionnaire (FFMQ): The FFMQ is a scale to assess an individual’s mindfulness skills. It asks respondents to indicate their level of agreement with a series of 39 statements about their general tendency to be mindful during daily life experiences.Citation13 Scores are in the range between 39 and 195.
Details of the aforementioned outcomes and other secondary clinical outcomes appear in the supplementary files. (Clinical outcomes reported in the and , and 6, Clinical outcomes not reported in the –). All measures are self-report questionnaires and have been validated in the Japanese population.Citation26–Citation36
Table 6 Subgroup Analysis by Baseline Score (Mean (SD)) of WHO-5 Irrespective of Health Status at Each Assessment Point
Statistical Methods
Statistical data relevant to demographic and feasibility are presented descriptively. The change in mean scores at each scale between baseline and each observational point was analyzed with an intention-to-treat analysis and a mixed-effect model repeat measurement to deal with missing data in longitudinal clinical trials. With respect to the scales of the subjective well-being (ie, WHO-5 and SWLS), we treated each scale individually, rather than integrating them. All analyses were performed using the SPSS Version 24.Citation37
Results
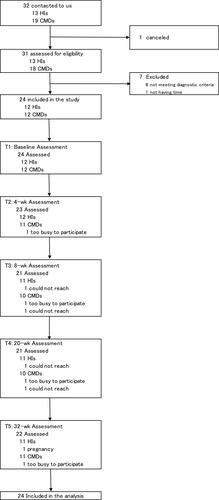
As shown in , 24 participants in total (12 HIs and 12 people with CMDs) were included in the study. We originally planned to recruit 30 participants. However, we conducted the study with 24 participants because we judged it was difficult to include all 30 participants by the end of the study period.
Participants’ Characteristics
The baseline socio-demographic characteristics are presented in . In brief, the mean age (SD) of the participants was 45.1 years (SD 9.5), 66.7% were female, all were employed, and 66.7% were married in HIs. The participants in CMDs also showed similarity to the HIs except diagnoses of CMDs (five had anxiety disorder, while four and three participants had adaptive disorder and major depressive disorder (currently remitted), respectively).
Feasibility and Safety
The mean number of sessions attended in HIs was 7.3 out of 8 compared to 5.9 in CMDs (p= 0.11) during the weekly sessions, and 4.2 out of 6, while 2.7 in CMDs (p=0.09) during the follow-up period (). Serious adverse events were not observed in this study.
Clinical Outcomes
Healthy Individuals
The results of the clinical outcomes in HIs are shown in and S1. No statistically significant improvement was observed in the primary outcome: WHO-5. However, scores on the SWLS showed significant improvements at week 20. On the FFMQ, one subscale (nonjudgement) score showed a significant improvement at week 4 and 8. Among other secondary outcomes, subscales of Self Compassion Scales (SCS) and Multidimensional Assessment of Interoceptive Awareness (MAIA) improved significantly at week 20 and 32 (Table S1).
Common Mental Disorders
For the participants with CMDs, WHO-5 showed a significant improvement at week 32. All secondary clinical outcomes, except Connor Davidson Resilience Scale, Perceived Stress Scale, Health and Work Performance Questionnaire (relative presenteeism) and some subscales of SCS and MAIA showed significant improvements during the observational period ( and S2).
Subgroup Analysis
We conducted a subgroup analysis by dividing all samples into two subgroups irrespective of health status: the upper and the lower half of the baseline scores of WHO-5. The results revealed that WHO-5 improved significantly at week 8 and 32 among the subjects whose baseline score started in the lower half ().
Discussion
To the best of our knowledge, this is the first study to evaluate the safety, feasibility and effectiveness of MBCT for improving the subjective well-being of HIs in long term in comparison with clinical samples. With respect to the program’s safety and feasibility, no serious adverse events were observed. The mean attendance rate was higher in HIs compared to that in patients with CMDs (). Better health condition might have contributed to higher attendance rate. Considering the fact that the attendance rate of healthy individuals in the study is equivalent enough to the results of previous studies (between 46% and 97%),Citation38 the MBCT for HIs is sufficiently safe and feasible, and is possibly more acceptable compared to the patients with CMDs.
Concerning the subjective well-being among HIs, a statistically significant improvement was detected in SWLS at week 20, following the improvement of one of the FFMQ subscale (nonjudgement) at week 4 and 8. In contrast, no improvement was seen in the primary outcome: WHO-5. Garland et al suggested a mindfulness-to-meaning theory explaining how mindfulness improves peoples’ well-being.Citation39 This theory indicates that mindfulness practice improves metacognitive capacity for experience through amelioration of mindfulness skills, resulting in a positive reappraisal of the experience and an increase in positive affect. According to the theory, the order of improvement should be mindfulness skill (FFMQ), followed by the cognitive aspect (SWLS), and the affective aspects (WHO-5) of well-being. This might explain why FFMQ and SWLS improved within the study period, but WHO-5 did not show any significant improvement.
In the people with CMDs, both WHO-5 and SWLS improved significantly at week 32. We judged that this discrepancy possibly occurred due to the following two reasons. The first is the lack of statistical power due to the very limited sample size. The other reason is the “ceiling effect”. As shown in and , the baseline scores of any scales were significantly better in HIs. As the results of the subgroup analysis in show, WHO-5 improved significantly at week 8 and 32 if we focused on the subjects whose baseline scores were in the lower half. Considering these facts, in developing a design of RCTs, selecting individuals with lower subjective well-being would be reasonable to minimize the “ceiling effect”.
Limitations
The study had some limitations. The sample size was too small to detect clinically significant difference. Another limitation was that the basic characteristics of the samples in each group were not matched. Furthermore, the study was performed with a pre-post comparison design. Therefore, a well-designed RCT with larger sample sizes is warranted in the next research stage.
Conclusions
MBCT is sufficiently safe and would be more feasible in HIs compared to in the clinical samples. In designing RCTs, selecting HIs with lower subjective well-being would be reasonable to minimize the “ceiling effect”.
Abbreviations
CMDs, people with Common Mental Disorders; FFMQ, Five Facet Mindfulness Questionnaire; His, Healthy Individuals; MBCT, Mindfulness-Based Cognitive Therapy; RCTs, Randomized Controlled Trials; SCS, Self Compassion Scales; SD, Standard Deviation; SE, Standard Error; SWLS, Satisfaction with Life Scale; WHO-5, the 5-item World Health Organization Well-Being Index.
Date Availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
This study was approved by the ethical committee at Keio University School of Medicine (reference: 20160009). All participants submitted written informed consent. The identification number of the clinical trial registry system at the University Hospital Medical Information Network was UMIN000022528. This study was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2008.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Acknowledgments
The authors would like to thank Ms. Miyu Takahashi and Ms. Ayaka Inaba for their remarkable assistance in developing the dataset.
Disclosure
The authors declare that they have no competing interests.
Additional information
Funding
References
- Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68(4):615–623. doi:10.1037/0022-006X.68.4.615
- Kuyken W, Byford S, Taylor RS, et al. Mindfulness-based cognitive therapy to prevent relapse in recurrent depression. J Consult Clin Psychol. 2008;76(6):966–978. doi:10.1037/a0013786
- Ninomiya A, Sado M, Park S, et al. Effectiveness of mindfulness-based cognitive therapy in patients with anxiety disorders in secondary-care settings: a randomized controlled trial. Psychiatry Clin Neurosci. 2020;74(2):132–139. doi:10.1111/pcn.12960
- Shapero BG, Greenberg J, Pedrelli P, Desbordes G, Lazar SW. Mindfulness-based cognitive therapy. In: The Massachusetts General Hospital Guide to Depression. Springer; 2019:167–177.
- Diener E, Pressman SD, Hunter J, Delgadillo-Chase D. If, why, and when subjective well-being influences health, and future needed research. Appl Psychol Health Well Being. 2017;9(2):133–167. doi:10.1111/aphw.12090
- Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. 2015;385(9968):640–648. doi:10.1016/S0140-6736(13)61489-0
- Howell RT, Kern ML, Lyubomirsky S. Health benefits: meta-analytically determining the impact of well-being on objective health outcomes. Health Psychol Rev. 2007;1(1):83–136. doi:10.1080/17437190701492486
- Diener E, Chan M. Happy people live longer: subjective well‐being contributes to health and longevity. Appl Psychol Health Well-Being. 2011;3(3):1–43. doi:10.1111/j.1758-0854.2010.01045.x
- Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18(6):805–835. doi:10.1097/EDE.0b013e3181577511
- Segal Z, Williams JM, Teasdale J. Mindfulness-Based Cognitive Therapy for Depression. A New Approach to Preventing Relapse. Guilford Publications; 2002.
- World Health Organizaiton. Regional Office for Europe, Psychiatric Research Unit. Mastering depression in primary care. Frederiksborg General Hospital. 1998.
- Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49(1):71–75. doi:10.1207/s15327752jpa4901_13
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi:10.1177/1073191105283504
- Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54(5):573–583. doi:10.1016/S0006-3223(02)01866-8
- Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092
- Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. doi:10.1002/da.10113
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. doi:10.2307/2136404
- Cohen S. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, Spacapan S, Oskamp S, editors. The Social Psychology of Health. Sage Publications, Inc; 1988:31–67.
- Neff K. The development and validation of a scale to measure self-compassion. Self Identity. 2010;2(3):223–250. doi:10.1080/15298860309027
- Rosenberg M. Society and the Adolescent Self-Image. Princeton University Press; 1965.
- Bornemann B, Herbert BM, Mehling WE, Singer T. Differential changes in self-reported aspects of interoceptive awareness through 3 months of contemplative training. Front Psychol. 2015;5:1504. doi:10.3389/fpsyg.2014.01504
- Mehling WE, Acree M, Stewart A, Silas J, Jones A. The Multidimensional Assessment of Interoceptive Awareness, version 2 (MAIA-2). PLoS One. 2018;13(12):e0208034. doi:10.1371/journal.pone.0208034
- Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–1736. doi:10.1007/s11136-011-9903-x
- Kessler RC, Barber C, Beck A, et al. The World Health Organization Health and Work Performance Questionnaire (HPQ). J Occup Environ Med. 2003;45(2):156–174. doi:10.1097/01.jom.0000052967.43131.51
- Suzuki T, Miyaki K, Sasaki Y, et al. Optimal cutoff values of WHO-HPQ presenteeism scores by ROC analysis for preventing mental sickness absence in Japanese prospective cohort. PLoS One. 2014;9(10):e111191. doi:10.1371/journal.pone.0111191
- Awata S, Bech P, Koizumi Y, et al. Validity and utility of the Japanese version of the WHO-five well-being index in the context of detecting suicidal ideation in elderly community residents. Int Psychogeriatr. 2007;19(1):77–88. doi:10.1017/S1041610206004212
- Kadono T. Development and validation of the Japanese version of the satisfaction with life scale. Jpn Assoc J Educ Psychol. 1994;36:192. doi:10.20587/pamjaep.36.0_192
- Sugiura Y, Sato A, Ito Y, Murakami H. Development and validation of the Japanese version of the five facet mindfulness questionnaire. Mindfulness. 2012;3(2):85–94. doi:10.1007/s12671-011-0082-1
- Mimura C, Griffiths P. A Japanese version of the perceived stress scale: cross-cultural translation and equivalence assessment. BMC Psychiatry. 2008;8(1):85. doi:10.1186/1471-244X-8-85
- Arimitsu K. [Development and validation of the Japanese version of the Self-Compassion Scale]. Shinrigaku Kenkyu. 2014;85(1):50–59. doi:10.4992/jjpsy.85.50. [ Japanese]
- Mimura C, Griffiths P. A Japanese version of the Rosenberg self-esteem scale: translation and equivalence assessment. J Psychosom Res. 2007;62(5):589–594. doi:10.1016/j.jpsychores.2006.11.004
- Shoji M, Mehling WE, Hautzinger M, Herbert BM. Investigating multidimensional interoceptive awareness in a Japanese population: validation of the Japanese MAIA-J. Front Psychol. 2018;9:1855. doi:10.3389/fpsyg.2018.01855
- Tsuchiya A, Ikeda S, Ikegami N, et al. Estimating an EQ-5D population value set: the case of Japan. Health Econ. 2002;11(4):341–353. doi:10.1002/hec.673
- Fujisawa D, Nakagawa A, Tajima M, et al. Cross-cultural adaptation of the quick inventory of depressive symptomatology, self-report (QIDS-SR). Jpn J Stress Sci. 2010;25(1):43–52.
- Muramatsu K, Miyaoka H, Ueshima K, et al. Validation and utility of a Japanese version of the GAD-7. Jpn J Psychosom Med. 2010;50(6):592.
- Ito M, Nakajima S, Shirai A, Kim Y Cross-cultural validity of the ConnorDavidson Scale: data from Japanese population. presented at: Poster presented at 25th Annual Meeting, International Society of Traumatic Stress Studies (ISTSS). Atlanta, GA; November 2009.
- SPSS Statistics ver. 24; IBM, New York; 2016.
- de Vibe M, Bjørndal A, Fattah S, Dyrdal GM, Halland E, Tanner-Smith EE. Mindfulness-based stress reduction (MBSR) for improving health, quality of life and social functioning in adults: a systematic review and meta-analysis. Campbell Syst Rev. 2017;8(1):1–127. doi:10.4073/csr.2012.3
- Garland EL, Farb NA, Goldin PR, Fredrickson BL. Mindfulness broadens awareness and builds eudaimonic meaning: a process model of mindful positive emotion regulation. Psychol Inq. 2015;26(4):293–314. doi:10.1080/1047840x.2015.1064294