Abstract
Introduction
The outbreak of the COVID-19 has largely impacted individuals’ health and lifestyles. This study aimed to investigate people’s psychological well-being during the second phase of the COVID-19 pandemic.
Methods
We selected six indicators of psychological well-being: fear of COVID-19, loneliness, social interaction anxiety, generalized anxiety, PTSD, and depression. A sample of 231 Italian participants (56.3% women), with a mean age of 32.7 (SD=12.61), completed an online survey from February to March 2021, during the so called “second wave”. It included the Fear of COVID-19 Scale (FCV-19S), the UCLA Loneliness Scale- Version 3, the Generalized Anxiety Disorder 7-item Scale (GAD-7), the Patient Health Questionnaire-9 (PHQ-9), the Impact of Event Scale–Revised (IES-R), and the Social Interaction Anxiety Scale (SIAS).
Results
Apart from loneliness, women reported lower levels of psychological well-being than men. Fairly good associations between all the detected variables were found. Based on a mediation model evaluation (in which generalized anxiety was introduced as a mediator in the relationship between fear of COVID-19, PTSD, loneliness, social interaction anxiety, and depression), except for social interaction anxiety, total and partial mediation effects suggested that generalized anxiety played a crucial role in exacerbating depressive symptoms during the pandemic.
Conclusion
Our outcomes may expand the knowledge about the psychological well-being during the pandemic experience, with a focus on the mediating role of generalized anxiety.
Introduction
In December 2019, a new respiratory illness caused by a new Coronavirus (simply called COVID-19) was first identified in the city of Wuhan, China. The spread of the virus early became a global health problemCitation1 and the World Health OrganizationCitation2 declared a pandemic on March 12th, 2020. Even in Europe, first in Italy, the governments recurred to nationwide lockdown to slow down the virus transmission and reduce the pressure on the healthcare system for both physical and mental health (e.g., depression pandemic effects).Citation3,Citation4 Beyond the consequences on general health, the spread of the pandemic and the following restrictive measures had a great impact on the world economy and on all people’s daily life in all countriesCitation5–Citation9 as well as on developing countries.Citation10 As a result, social distancing – in association with personal risk (e.g., being female, above 44 years old, with many children, unemployed, etc.)Citation11 and protection factors (e.g., loneliness, mindfulness, and use of facemasks)Citation12,Citation13 – has more frequently caused negative psychological effects,Citation14–Citation16 such as fear of illness, fear of death, anxiety, depression, post-traumatic stress, and insomnia.Citation3,Citation5,Citation17–Citation19
Some scholars claimed that in Italy the prevalence of anxiety and depression doubled during the first lockdown and, in particular, depression symptoms increased from 33.6% (before the pandemic) to 38.9% (in the early stage of the pandemic).Citation20,Citation21 In addition, women – who also before the pandemic showed higher emotional expressivity, especially for negative emotions,Citation22 such as depressionCitation23 – were more exposed to the risks of negative psychological symptoms during pandemics, confirming their greater vulnerability than men.Citation10,Citation22,Citation24–Citation26
Some aspects of the COVID-19 disease, especially the high-speed contamination and the relatively high mortality,Citation27 have determined the fear of COVID-19.Citation28 Ahorsu et al.Citation29 highlighted that fear is a pandemic’s specific characteristic; with high levels of fear, people may not think/behave clearly and rationally regarding personal protective actions for the COVID-19.Citation30 Indeed, fear is an adaptive feeling which activates the needed energies to face danger, but only if it does not become excessive.Citation3 In these cases, according to an empirical tested model,Citation9 the physical symptoms ― mediated by the need for health information and perceived impact on pandemic ― can improve adverse mental health outcomes, such as anxiety and depression symptoms.Citation3,Citation31,Citation32
Loneliness and social isolation frequently co-occur with negative effects on psychological well-being.Citation33 As a generally accepted definition, «loneliness is defined as the subjective feeling of being alone, while social isolation describes an objective state of individuals’ social environments and interactional patterns».Citation35 Likewise, social anxiety and generalized anxiety disorder (GAD) frequently co-occur.Citation34,Citation36 Moreover, the lockdown restrictive measures – which invited people to stay at home and not to meet other people – had buffer effects on social anxiety and mental health,Citation37,Citation38 also increasing the levels of generalized anxiety disorderCitation37 and depression.Citation14,Citation40 Previous research documented a significant association between social interaction anxiety, depression, and anxiety.Citation39
In this climate of concern for one’s own health, post-traumatic stress disorder (PTSD) is a common experience, to the point of being considered as a widely shared experience during the pandemic.Citation40,Citation41 The core of PTSD’s symptoms – as described by the American Psychiatric Association (APA, 2013)Citation69 – are intrusion, negative alterations in mood and cognition, avoidance of trauma-related stimuli, and hyperarousal. Previous research showed a significant association between PTSD, anxiety, and depression, especially during the COVID-19 pandemic.Citation3,Citation26
Indeed, depression symptoms were a widespread experience during mass traumatic events, such as the COVID-19 pandemic,Citation42,Citation44 with no significant differences among countries.Citation45 Rodríguez-Hidalgo et alCitation3 showed that experiencing epidemic or natural disaster events may increase levels of long-term depression. They also reported depression as frequently linked to other negative feelings: stress predicted depression, depression and anxiety were frequently related to each other, and people with PTSD showed high levels of anxiety and depression.
Ultimately, during the first part of the pandemic experience (e.g., approximately from February to May 2020, when the governments introduced the restrictive measures for the first time) some researchCitation42 highlighted the risk for developing negative psychological responses to COVID-19 pandemic, which led to an increase of depressive symptoms. In fact, each of the selected indicators of psychological well-being showed strong associations with depression and generalized anxiety (e.g., fear of COVID-19,Citation3,Citation31,Citation32 loneliness,Citation39 PTSD,Citation3,Citation42 depression,Citation3 and social interaction anxietyCitation39). Based on previous studies,Citation46,Citation47 according to which anxiety disorders tended to temporally precede depression, we hypothesized a mediation model that could explain the direct and indirect influence of the selected indicators of psychological well-being on depression.
Objectives and Hypotheses
This study aimed to explore Italian general population’s psychological well-being during the COVID-19 pandemic. Based on literature findings, we studied the association between loneliness, fear of COVID-19, PTSD, social anxiety, and depression, also testing a mediation model.
Based on the literature findings reported above, we derived the following research hypotheses:
Hypothesis 1 (H1): We expect gender differences for loneliness, social anxiety, generalized anxiety, fear of COVID-19, PTSD, and depression, with women showing higher levels than men;
Hypothesis 2 (H2): We expect all the detected variables (loneliness, social anxiety, generalized anxiety, fear of COVID-19, PTSD, and depression) to be positively intercorrelated;
Hypothesis 3 (H3): We expect that generalized anxiety acts as a mediator in the relationship between fear of COVID-19, PTSD, loneliness, social interaction anxiety, and depression.
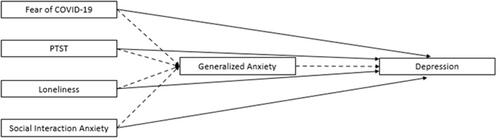
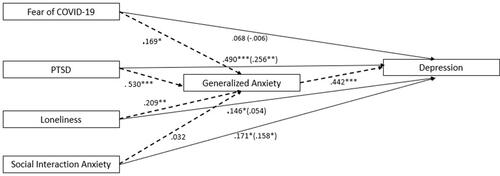
The hypothesized model is shown in .
Materials and Methods
Participants
Participants (N = 231) were all Italian people. They were fairly balanced across gender (56.3% women), aged from 18 to 69 (M = 32.7, SD = 12.61). Most of them (78.4%) declared neither to have contracted the virus nor to have had direct contacts with someone infected, 13.4% affirmed to have had close contacts with individuals affected by the virus, 6.1% stated to have been infected by the virus with mild symptoms, and 2.2% were individuals who have contracted the virus in a serious mode with hospital admission.
Measures
Fear of COVID-19
The Fear of COVID-19 Scale (FCV-19S)Citation29 is a 7-item Self-Report instrument (e.g., “I am most afraid of Coronavirus19”, “I am afraid of losing my life because of Coronavirus19”). It assesses the fear of COVID-19 with a five-point Likert scale from 1 (strongly disagree) to 5 (strongly agree), with a total score calculated by summing all items and ranging from 7 to 35. High scores indicate great fear of COVID-19. The internal consistency of the FCV-19S (Cronbach’s alpha) was 0.87.Citation29 In this study, we used the Italian version.Citation46 The Cronbach’s alpha for the present sample was 0.86.
Loneliness
The UCLA Loneliness Scale- Version3Citation48 was used to measure one’s own subjective feelings of loneliness as well as feelings of social isolation, in its Italian version.Citation49 It is a 20-item scale on a 4-point Likert scale from 1 (I never feel this way) to 4 (I often feel this way) (e.g., “I am unhappy doing so many things alone”, “I feel isolated from others”). This measure has high internal consistency (Cronbach’s alpha = 0.96)Citation48 and a test-retest correlation over two-month of 0.73. The Cronbach’s alpha for the present sample was 0.83.
Generalized Anxiety
Symptoms of generalized anxiety were measured by using the Generalized Anxiety Disorder 7-item Scale (GAD-7).Citation50 Participants indicated how often they experienced each symptom in the past 2 weeks on a four-point Likert scale from 0 (Not at all) to 3 (Nearly every day) (e.g., “Feeling nervous, anxious, or on edge”, “Trouble relaxing”). Higher scores are indicative of greater levels of anxiety. The GAD-7 has shown reliable and valid scores (Cronbach’s alpha = 0.83).Citation50 The Cronbach’s alpha for the present sample was 0.91.
Depression
Nine symptoms of depression were measured by using the Patient Health Questionnaire-9 (PHQ-9; e.g., “Little interest or pleasure in doing things”, “Trouble concentrating on things, such as reading the newspaper or watching television”).Citation51 It is a Self-Report scale which assesses the past two-week depressive symptoms on a 4-point Likert scale from 0 (Not at all) to 3 (Nearly every day). Higher scores represent problematic levels of depression (the total score ranges from 0 to 27). The Cronbach’s alpha value for the scale was 0.90.Citation51 In this study, we used the Italian version.Citation52 The Cronbach’s alpha for the present sample was 0.87.
Post-Traumatic Stress Disorder
The Impact of Event Scale–Revised (IES-R)Citation53 in its Italian versionCitation54 was used to evaluate the psychological traumatic impact of past epidemics (SARS, H1N1) during previous lockdown.Citation55 It was validated in various countriesCitation56–Citation60 during the COVID-19 pandemic and it was also widely used in Italian research on this topic.Citation61,Citation62 It assesses the intensity of 22 post-traumatic symptoms of intrusion, avoidance, and hyper-arousal on a Likert scale ranging from 0 (not at all) to 4 (extremely). It shows good test–retest reliability (r = 0.89–0.94) and internal consistency (Cronbach’s α) for each subscale (intrusion = 0.87–0.94, avoidance = 0.84–0.97, hyper-arousal = 0.79–0.91).Citation63 The IES-R consists of three PTSD dimensions: intrusion (e.g., “Any reminder brought back feelings about it”), agitation (e.g., “I felt irritable and angry”), and avoiding (e.g., “I avoided letting myself get upset when I thought about it or was reminded of it”). The Cronbach’s alpha for the present sample was 0.95 (intrusion = 0.90, avoidance = 0.88, hyper-arousal = 0.88).
Social Interaction Anxiety
The Social Interaction Anxiety Scale (SIAS)Citation64 is a 19-item measure used to assess anxiety when engaging in social interactions (e.g., “It makes me uncomfortable to meet an acquaintance on the street”, “It’s hard for me to chat with other people”). Respondents were required to answer on a 5-point Likert-type scale, from 0 (not at all) to 4 (extremely); the total score reflects the severity of social interaction anxiety (Cronbach’s alpha = 0.86).Citation64 The Italian version of the SIAS was used in this study.Citation65 The Cronbach’s alpha for the present sample was 0.90.
Procedure
Participants completed an online survey through Google Forms, from February to March 2021, during the so called “second wave” of the COVID-19 pandemic. The survey was disseminated through social networks (e.g., Facebook, Instagram, and WhatsApp). After explaining the purposes of the study, participants who met our eligibility criteria (being Italian and older than 18) signed the informed consent. We avoided missing data using a mandatory response format in our google form. The online survey methodology was useful to overcome the problems of administration in-person during social distancing restrictions. However, it did not allow us to assess the response rate.
The study was conducted according to the 1964 Helsinki Declarations and its later amendments. The research project proposal was approved by the Internal Review Board of the psychological research of the UKE – University Kore Enna with the Code UKE-IRBPSY-03.21.01. The administration of the measures was carried out in compliance with the privacy guarantee regulations according to the Legislative Decree n. 196/2003, and the GDPR (EU Regulation n.2016/679). Data were collected individually for research purposes only and treated in an aggregated and anonymous form.
Data Analysis
After performing standard descriptive statistical analyses of data, a General Linear Model analysis was applied to test the gender differences in psychological well-being during the second wave of COVID-19 pandemic (H1). We also tested the associations between all the observed variables (e.g., fear of COVID-19, PTSD, loneliness, social interaction anxiety, generalized anxiety, and depression), using Pearson’s correlations (H2).
To test H3, a mediation model was performed using jamovi (version 1.2) GLM package (JAMM module). The model investigated the direct and indirect effects (mediated by generalized anxiety) of fear of COVID-19, PTSD, loneliness, and social interaction anxiety on depression. Multivariate distribution was first checked to verify whether the assumption of multivariate normality was met. By comparing Mardia’s coefficient (60.11) with the critical value associated with six-degrees-of-freedom (48), there was clear evidence that our data violated the assumption of multivariate normality. Bootstrapping is a non-parametric resampling procedure, recognized as a powerful and rigorous method for mediation analysisCitation67 and the best suited procedure to be applied when data are not normally distributed. Therefore, in this study, the bootstrapping procedure (percentiles) was applied to test the mediation hypothesis using 1000 bootstrap samples and 95% confidence intervals. Finally, in order to verify whether the tested mediation model was invariant across gender, the mediation analysis was also performed separately for men and women.
Results
General Linear Model: Does Gender Lead to Differences in Psychological Well-Being?
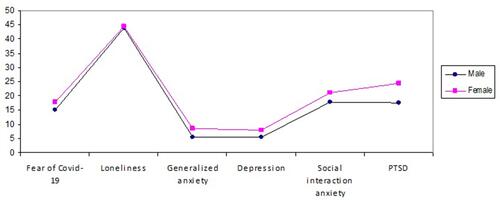
A General Linear Model analysis was applied to verify the hypothesized effect between gender and fear of COVID-19, loneliness, social interaction anxiety, generalized anxiety, PTSD, and depression (see and for descriptive statistics). Univariate tests of between-subjects effects with gender as a between-participants variable were conducted as follow up tests to determine whether levels of psychological well-being differed across the two groups (males vs females).
Table 1 Descriptive Statistics of All the Study Variables
Table 2 Descriptive Statistics of All the Study Variables Disaggregated by Gender
Overall, results showed that gender significantly affected psychological wellness, Wilks’ Ʌ = 0.894, F (6, 215) = 4.242, p<0.001, partial η2 = 0.106. Tests of between-subjects effects showed that women scored significantly higher on fear of COVID-19, F(1, 220) = 12.938, p<0.001, partial η2 = 0.056, generalized anxiety, F(1, 220) = 20.115, p<0.001, partial η2 = 0.084, depression, F(1, 220) = 10.475, p<0.001, partial η2 = 0.045, social interaction anxiety, F(1, 220) = 5.113, p<0.05, partial η2 = 0.023, and PTSD, F(1, 220) = 9.659, p<0.01, partial η2 = 0.042, than men. Only loneliness did not show statistically significant results in relationship with gender, F(1, 220) = 0.372, p = 0.543, partial η2 = 0.002. presents means of the psychological well-being variables for the two gender groups.
Correlations Between the Selected Indicators of Psychological Well-Being
We also explored the associations between all the detected variables. We considered fear of COVID-19, loneliness, social interaction anxiety, generalized anxiety, PTSD, and depression as indicators of psychological well-being during the COVID-19 pandemic. Our results showed statistically significant correlations between all of them (mostly p<0.001; only the association between fear of COVID-19 and loneliness was p<0.01) (see ). Moreover, we performed a correlational analysis between all the study variables disaggregated by gender (see ). For both groups, the relationships between the study variables were statistically significant, except for the association between loneliness and PTSD with fear of COVID-19 in men.
Table 3 Intercorrelations Between the Study Variables
Table 4 Intercorrelations Between the Study Variables Disaggregated by Gender
Mediation Analysis
displays the results of the proposed mediation model considering the whole sample. The total and direct effect of fear of COVID-19 on depression did not show significant results (β=0.097, p=0.065, 95% CI [−0.006, 0.183] and β=−.009, p=0.854, 95% CI [−0.096, 0.089], respectively). With the introduction of generalized anxiety as a mediator, the indirect effect was significant (β=0.106, p=0.002, 95% CI [0.044, 0.162]), providing evidence of a fully mediated effect. PTSD had a significant direct relationship on depression (β=0.216, p=0.032, 95% CI [0.001, 0.126]) and the magnitude of its effect increased when generalized anxiety was included as a mediator (β=0.231, p<0.001, 95% CI [0.043, 0.114]). Generalized anxiety accounted for the 51.361% of the total effect of PTSD on depression (β=0.447, p<0.001, 95% CI [0.102, 0.181]). The association between loneliness and depression was also partially mediated by generalized anxiety, which explained the 52.469% of the total effect (β=0.210, p<0.001, 95% CI [0.68, 0.210]). As a matter of fact, it showed a significant direct (β=0.099, p=0.038, 95% CI [0.001, 0.124]) and indirect effect (β=0.110, p=0.005, 95% CI [0.029, 0.130]) on depression. Lastly, social interaction anxiety showed a significant direct effect on depression (β=0.142, p=0.040, 95% CI [0.002, 0.133]), whereas generalized anxiety did not act as a mediator (β=0.011, p=0.762, 95% CI [−0.031, 0.040]).
Table 5 Total, Direct, and Indirect Effects of the Hypothesized Mediation Model (Whole Sample)
In addition, to test whether the proposed mediation model was invariant across gender, the associations among the selected variables were analysed separately for men and women.
Regarding men, we found that general anxiety fully mediated the relationship between fear of COVID-19 and depression (β=0.096, p=0.027, 95% CI [0.011, 0.197]); both loneliness and PTSD directly affected depression (β=0.175, p=0.022, 95% CI [0.169, 0.217] and β=0.193, p=0.036, 95% CI [0.004, 0.122], respectively), and the magnitude of their associations increased when generalized anxiety was introduced as a mediator (β=0.154, p=0.003, 95% CI [0.036, 0.170] and β=0.191, p=0.002, 95% CI [0.023, 0.102]). Lastly, social interaction anxiety was neither directly nor indirectly associated with depression (β=0.106, p=0.275, 95% CI [−0.039, 0.140] and β=0.011, p=0.847, 95% CI [−0.049, 0.060]).
As far as it concerns the mediation model tested for women, a fully mediation was evaluated in the association between fear of COVID-19 and depression (β=0.075, p=0.027, 95% CI [0.007, 0.119]) and between loneliness and depression (β=0.092, p=0.009, 95% CI [0.015, 0.102]); PTSD directly affected depression (β=0.256, p=0.004, 95% CI [0.026, 0.132]) and by introducing general anxiety as a mediator, a stronger significant association was estimated (β=0.234, p <0.001, 95% CI [0.038, 0.107]); social interaction reported a statistical direct effect on depression (β=0.158, p=0.035, 95% CI [0.004, 0.141]), whereas generalized anxiety did not function as a mediator (β=0.014, p=0.685, 95% CI [0.038, 0.107]). A more detailed description of the total, direct, and indirect effects of the selected variables on depression for men and for women are shown in and , respectively. The measurement models for the whole sample, men, and women are depicted in –, respectively; only significant paths are reported.
Table 6 Total, Direct, and Indirect Effects of the Hypothesized Mediation Model (Men)
Table 7 Total, Direct, and Indirect Effects of the Hypothesized Mediation Model (Women)
Figure 3 Measurement model testing the relationship between fear of COVID-19, PTSD, loneliness, and social interaction anxiety through generalized anxiety (whole sample).
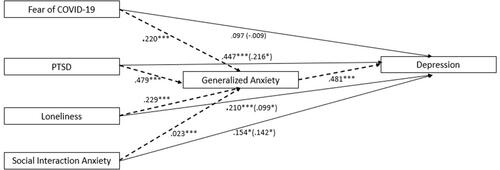
Figure 4 Measurement model testing the relationship between fear of COVID-19, PTSD, loneliness, and social interaction anxiety through generalized anxiety (men).
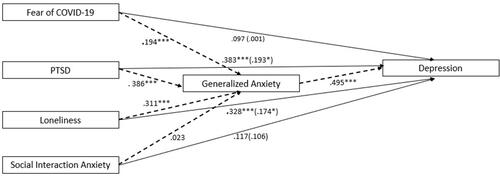
Figure 5 Measurement model testing the relationship between fear of COVID-19, PTSD, loneliness, and social interaction anxiety through generalized anxiety (women).
Discussion
In December 2019, the new COVID-19 was first identified in China and then spread throughout the world. As a problematic and alarming perspective, Brooks et alCitation43 have recently highlighted that periods of isolation, even less than 10 days, may improve the psychiatric symptoms, also with long-term effects. Besides, many people did not have access to mental health services – although they were increased during the pandemicCitation55 – and consequently resorted to self-care, self-medication, and self-help,Citation28 especially for psychiatric patients.Citation66 This study aimed to investigate people’s psychological well-being (i.e., fear of COVID-19, loneliness, social interaction anxiety, generalized anxiety, PTSD, and depression) during the “second wave” of the COVID-19 pandemic.
According to our initial hypothesis (H1) and previous research,Citation15,Citation24,Citation26–Citation28 our findings demonstrated that women had lower levels of psychological well-being in all the selected indicators, except for loneliness. As a viable interpretation, all people (both men and women) were affected by the same restrictive measures. In case of illness or contact with someone infected, the governments have indicated social isolation to better control the spread of the pandemic. Nevertheless, as demonstrated by previous studies, women had higher emotional expressivity than men, particularly for negative emotions;Citation19 for this reason, women might more likely recognize and declare their negative emotional experiences in self-report assessment. Additionally, some studiesCitation71,Citation72 highlighted that women experienced more psychological difficulties than men due to the schools’ closures, resulting in higher domestic workload and less time for rest during COVID-19 period. The gender inequity could also be accentuated by a disproportion in responsibility for domestic duties, especially for childcare and eldercare, but also by the increase in domestic violence by the partner and a greater loss of women’s jobs.Citation72,Citation73 Based on these findings, on a practical level, it should be crucial to produce awareness-raising campaigns to generate awareness and prevent inequity.
We also examined the relationship between all the study variables. According to our initial hypothesis (H2) and previous research,Citation3,Citation5,Citation16,Citation18,Citation32,Citation37–Citation39,Citation68 our results showed a fairly good positive correlation between all of them. We also performed a correlation analysis disaggregated by gender to test whether the detected variables reported similar patterns of correlations. Except for the absence of correlation between loneliness and fear of COVID-19 and between PTSD and fear of COVID-19 (for men), all the relationships were positive and significant.
As a practical interpretation, the increase in infections, the incidence of severe symptoms, and the daily bulletin of deathsCitation29 may increase psychological symptoms such as fear, loneliness, social anxiety, generalized anxiety, depression, and PTSD in reciprocal escalation. Against this background, the psychological symptoms could be very heavy even in the long term. As such, further studies should deepen any other indicator of psychological well-being connected with restrictive measures to contain psychological problems during and after the COVID-19 pandemic.
Lastly, we proposed a mediation model to explain the relationships among the detected variables (see ). Our findings supported our initial hypothesis (H3) and were consistent with many studies related to the pandemic experience.Citation3,Citation5,Citation14,Citation16–Citation18,Citation28,Citation32,Citation37–Citation40,Citation67 We found a fully mediated effect of generalized anxiety when considering the association between fear of COVID-19 and depression, but not a direct effect. Based on our results and previous research,Citation3,Citation32 the fear of COVID-19 alone is not enough to determine the depression symptoms. Experiencing lockdown and anxiety toward any forms of possible contamination could exacerbate fear of COVID-19 and consequently generalized anxiety. As a viable interpretation, this state of fear and anxiety together could result in depressive symptoms; these last could be secondary symptoms after the negative emotions. We also found a significant direct effect of PTSD on depression, and this association had a greater magnitude effect when we introduced generalized anxiety as a mediator. PTSD appears after traumatic experiences (e.g., actual or threatened death), such as pandemic COVID-19,Citation41 and it is characterized by typical symptoms including negative emotions.Citation70 As a possible explanation, the specific characteristics of the COVID-19 pandemic – especially the worry about contagion, which causes fear for one’s own and others’ health – could lead to depressive feelings of helplessness.Citation3,Citation28 Generalized anxiety could intensify this relationship through constant perception, and excessive tension may be exacerbated by personal characteristics.Citation33 Moreover, our results highlighted that the association between loneliness and depression had a direct effect, but it was partially mediated by generalized anxiety. Our findings were in line with previous studiesCitation68,Citation70 that showed a strong predictive association of loneliness on depression. In view of the foregoing, isolation imposed by legislative measures could be extremely unbearable. Thus, the introduction of generalized anxiety as a mediator could distance people from other people and places, by increasing frustration, low mood, and asthenia.
Lastly, social interaction anxiety had a direct effect on depression without mediation of generalized anxiety. As a possible interpretation, social interaction anxiety could play a role specifically connected to the COVID-19 pandemic. Indeed, the contagion occurs through direct contact with an infectious person (governments suggest staying at one meter away from each other).Citation40 In such conditions, social interaction anxiety would be enough to cause unhappiness and sadness, without the occurrence of generalized anxiety as a mediator.
When inspecting the hypothesized mediation model separately for men and women, no substantial differences were estimated, providing additional support to the role of general anxiety in modulating the relationship between the set of observed psychological variables and depressive symptoms. It means that, regardless of gender, general anxiety may fully or partly explain the development of depressive symptoms during the pandemic. From this perspective, it is likely that these ongoing conditions (e.g., uncertainty, unpredictability, continuous changes) may primarily increase general anxiety in individuals, who constantly receive several – and somewhat contradictory – information about the COVID-19 and its transmissibility. From this point of view, as stated by previous research,Citation74 improving public awareness of the COVID-19, through the diffusion of clear, timely, and complete messages, might prevent the spread of anxious symptoms. Accordingly, it would be desirable that governments and public policies would pay attention to the communication strategies during a global health crisis. Likewise, specific programs should be implemented to improve people’s skill in handling their own anxious symptoms arising in similar circumstances. Our findings are in line with previous studiesCitation75 that confirmed the presence of clinically significant symptoms even after the early stages of the pandemic. Further research should enhance a longitudinal approach and it should also pay attention to the vaccines’ implications on anxiety and depression in Italian population: the acceptance to the COVID-19 vaccines could be different for general and psychiatric population.Citation76
In conclusion, fear of COVID-19, PTSD, loneliness, and social interaction anxiety had an impact on depression, and generalized anxiety was a significant mediator in these relationships. The pandemic experience (eg, social distancing, isolation, increased contagion) seemed very debilitating for people’s mental health. Further research should deepen further mental health indicators to better handle psychological disturbances also in long-term.
Limitation
Our study has some critical limitations that require further investigation. First, we used an online survey procedure for collecting data. Therefore, it was not possible to check whether the testing conditions were optimal, but restrictive measures did not allow any other option. Also, we could not obtain balanced categories referring to the different risks of contagion, thus preventing additional related analyses. Further, we did not calculate the minimum required sample size for conducting our analyses prior to data collection. Moreover, the sample size is small relative to the number of variables included in the mediation model. Future research should replicate it with a larger sample. Lastly, the cross-sectional nature of the data did not help us to determine cause and effect associations. As a matter of fact, the applied data analyses could not address the temporal relationships among the measured variables for the identification of potential causal factors.
Conclusion
Despite the limitations, our outcomes may expand the knowledge about the psychological well-being during the pandemic experience, with a focus on the specific role of generalized anxiety, thus guiding future research and clinical practice toward a better understanding of the psychological processes involved in similar circumstances. On a theoretical level, our findings, and especially those related to the role of generalized anxiety in modulating depressive symptoms, may offer a deeper knowledge of the psychological mechanisms implicated when people experience negative events, also providing the basis for a longitudinal understanding of psychological well-being during potentially different COVID-19 “waves”. On a practical level, understanding how people react to a stressful event such a pandemic could facilitate clinical work on mental health also to prevent eventual long-term symptoms. The online psychotherapy, such as the cognitive behavior therapy, could offer an online setting to help individuals to counteract the pandemic psychological effects, by respecting the restrictive measures and social-distancing.Citation77–Citation79
Disclosure
The authors declared no potential conflicts of interest concerning to the research, authorship, and/or publication of this article.
References
- Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi:10.1016/S0140-6736(20)30185-9
- World Health Organization. WHO director-generals opening remarks at the mission briefing on COVID-19; 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-mission-briefing-on-covid-19—12-march-2020. Accessed March 7, 2022.
- Rodríguez-Hidalgo AJ, Pantaleón Y, Dios I, Falla D. Fear of COVID-19, stress, and anxiety in university undergraduate students: a predictive model for depression. Front Psychol. 2020;11:591797. doi:10.3389/fpsyg.2020.591797
- Lee Y, Lui LMW, Chen-Li D, et al. Government response moderates the mental health impact of COVID-19: a systematic review and meta-analysis of depression outcomes across countries. J Affect Disord. 2021;290:364–377. doi:10.1016/j.jad.2021.04.050
- Di Crosta A, Palumbo R, Marchetti D, et al. Individual differences, economic stability, and fear of contagion as risk factors for PTSD symptoms in the COVID-19 emergency. Front Psychol. 2020;11:567367. doi:10.3389/fpsyg.2020.567367
- Gollwitzer M, Platzer C, Zwarg C, Göritz AS. Public acceptance of Covid-19 lockdown scenarios. Int J Psychol. 2021;56(4):551–565. doi:10.1002/ijop.12721
- Racine S, Miller A, Mehak A, Trolio V. Examining risk and protective factors for psychological health during the COVID-19 pandemic. Anxiety Stress Coping. 2021;1–17. doi:10.1080/10615806.2021.1958789
- Xiong J, Lipsitz O, Nasri F, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi:10.1016/j.jad.2020.08.001
- Wang C, Chudzicka-Czupała A, Tee ML, et al. A chain mediation model on COVID-19 symptoms and mental health outcomes in Americans, Asians and Europeans. Sci Rep. 2021;11(1):6481. doi:10.1038/s41598-021-85943-7
- Wang C, Tee M, Roy AE, et al. The impact of COVID-19 pandemic on physical and mental health of Asians: a study of seven middle-income countries in Asia. PLoS One. 2021;16(2):e0246824. doi:10.1371/journal.pone.0246824
- Le XTT, Dang AK, Toweh J, et al. Evaluating the psychological impacts related to COVID-19 of Vietnamese people under the first nationwide partial lockdown in Vietnam. Front Psychiatry. 2020;11:824. doi:10.3389/fpsyt.2020.00824
- Gill PK, Du C, Khan F, Karimi N, Sabharwal K, Agarwal M. The psychological effects of COVID-19 spread in young Canadian adults. Int J Soc Psychiatr. 2021. doi:10.1177/0020764020988878
- Wang C, Chudzicka-Czupała A, Grabowski D, et al. The association between physical and mental health and face mask use during the COVID-19 pandemic: a comparison of two countries with different views and practices. Front Psychiatry. 2020;11:569981. doi:10.3389/fpsyt.2020.569981
- Pietrabissa G, Simpson SG. Psychological consequences of social isolation during COVID-19 outbreak. Front Psychol. 2020;11:2201. doi:10.3389/fpsyg.2020.02201
- Obschonka M, Gewirtz AH, Zhu L. Psychological implications of the COVID-19 pandemic around the world: introduction to the special issue. Int J Psychol. 2021;56(4):493–497. doi:10.1002/ijop.12793
- Özdin S, Bayrak özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int J Soc Psychiatry. 2020;66(5):504–511. doi:10.1177/0020764020927051
- Mohammadpour M, Ghorbani V, Khoramnia S, Ahmadi SM, Ghvami M, Maleki M. Anxiety, self-compassion, gender differences and COVID-19: predicting self-care behaviors and fear of COVID-19 based on anxiety and self-compassion with an emphasis on gender differences. Iran J Psychiatry. 2020;15(3):213–219. doi:10.18502/ijps.v15i3.3813
- Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry. 2020;66(4):317–320. doi:10.1177/0020764020915212
- Deng Y, Chang L, Yang M, Huo M, Zhou R. Gender differences in emotional response: inconsistency between experience and expressivity. PLoS One. 2016;11(6):e0158666. doi:10.1371/journal.pone.0158666
- Amerio A, Lugo A, Stival C, et al. COVID-19 lockdown impact on mental health in a large representative sample of Italian adults. J Affect Disord. 2021;292:398–404. doi:10.1016/j.jad.2021.05.117
- Medda E, Toccaceli V, Gigantesco A, Picardi A, Fagnani C, Stazi MA. The COVID-19 pandemic in Italy: depressive symptoms immediately before and after the first lockdown. J Affect Disord. 2022;298(PtA):202–208. doi:10.1016/j.jad.2021.10.129
- Broche-Pérez Y, Fernández-Fleites Z, Jiménez-Puig E, Fernández-Castillo E, Rodríguez-Martin BC. Gender and fear of COVID-19 in a Cuban population sample. Int J Ment Health Addict. 2020;1–9. doi:10.1007/s11469-020-00343-8
- Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. 2018;8(1):2861. doi:10.1038/s41598-018-21243-x
- Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. doi:10.1016/j.psychres.2020.112921
- Shevlin M, McBride O, Murphy J, et al. Anxiety, depression, traumatic stress and COVID-19-related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open. 2020;6(6):e125. doi:10.1192/bjo.2020.109
- Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–542. doi:10.1016/j.bbi.2020.05.048
- Seyed Hashemi SG, Hosseinnezhad S, Dini S, Griffiths MD, Lin CY, Pakpour AH. The mediating effect of the cyberchondria and anxiety sensitivity in the association between problematic internet use, metacognition beliefs, and fear of COVID-19 among Iranian online population. Heliyon. 2020;6(10):e05135. doi:10.1016/j.heliyon.2020.e0513510.1016/j.heliyon.2020.e05135
- Yıldırım M, Akgül Ö, Geçer E. The effect of COVID-19 anxiety on general health: the role of COVID-19 coping. Int J Ment Health Ad. 2021;1–12. doi:10.1007/s11469-020-00429-3
- Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Ad. 2020;1–9. doi:10.1007/s11469-020-00270-8
- Arora T, Grey I. Health behaviour changes during COVID-19 and the potential consequences: a mini-review. J Health Psychol. 2020;25(9):1155–1163. doi:10.1177/1359105320937053
- Sakib N, Akter T, Zohra F, Bhuiyan AI, Mamun MA, Griffiths MD. Fear of COVID-19 and depression: a comparative study among the general population and healthcare professionals during COVID-19 pandemic crisis in Bangladesh. Int J Ment Health Ad. 2021;1–17. doi:10.1007/s11469-020-00477-9
- Schweda A, Weismüller B, Bäuerle A, et al. Phenotyping mental health: age, community size, and depression differently modulate COVID-19-related fear and generalized anxiety. Compr Psychiatry. 2021;104:152218. doi:10.1016/j.comppsych.2020.152218
- Park C, Majeed A, Gill H, et al. The effect of loneliness on distinct health outcomes: a comprehensive review and meta-analysis. Psychiatry Res. 2020;294:113514. doi:10.1016/j.psychres.2020.113514
- Hwang TJ, Rabheru K, Peisah C, Reichman W, Ikeda M. Loneliness and social isolation during the COVID-19 pandemic. Int Psychogeriatr. 2020;32(10):1217–1220. doi:10.1017/S1041610220000988
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication [published correction appears in Arch Gen Psychiatry. Arch Gen Psychiatry. 2005;62(6):617–627. doi:10.1001/archpsyc.62.6.617
- Hendriksen PA, Kiani P, Garssen J, Bruce G, Verster JC. Living alone or together during lockdown: association with mood, immune fitness and experiencing COVID-19 symptoms. Psychol Res Behav Manag. 2021;14:1947–1957. doi:10.2147/PRBM.S332853
- Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16(1):57. doi:10.1186/s12992-020-00589-w
- Robb CE, de Jager CA, Ahmadi-Abhari S, et al. Associations of social isolation with anxiety and depression during the early COVID-19 pandemic: a survey of older adults in London, UK. Front Psychiatry. 2020;11:591120. doi:10.3389/fpsyt.2020.591120
- Hughes AA, Heimberg RG, Coles ME, Gibb BE, Liebowitz MR, Schneier FR. Relations of the factors of the tripartite model of anxiety and depression to types of social anxiety. Behav Res Ther. 2006;44(11):1629–1641. doi:10.1016/j.brat.2005.10.015
- Liang L, Gao T, Ren H, et al. Post-traumatic stress disorder and psychological distress in Chinese youths following the COVID-19 emergency. J Health Psychol. 2020;25(9):1164–1175. doi:10.1177/1359105320937057
- Salmanian M, Salehi M, Hooshyari Z. Global prevalence of Posttraumatic Stress Disorder (PTSD) during and after coronavirus pandemic: a study protocol for a systematic review and meta-analysis. Iran J Psychiatry. 2020;15(3):252–255. doi:10.18502/ijps.v15i3.3819
- Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9):e2019686. doi:10.1001/jamanetworkopen.2020.19686
- Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi:10.1016/S0140-6736(20)30460-8
- Ustun G. Determining depression and related factors in a society affected by COVID-19 pandemic. Int J Soc Psychiatr. 2020. doi:10.1177/0020764020938807
- Al Omari O, Al Sabei S, Al Rawajfah O, et al. Prevalence and predictors of depression, anxiety, and stress among youth at the time of COVID-19: an Online Cross-Sectional Multicountry Study. Depress Res Treat. 2020;2020:8887727. doi:10.1155/2020/8887727
- Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. J Child Psychol Psychiatry. 2005;46(11):1200–1210. doi:10.1111/j.1469-7610.2005.00422.x
- Starr LR, Davila J. Temporal patterns of anxious and depressed mood in generalized anxiety disorder: a daily diary study. Behav Res Ther. 2012;50(2):131–141. doi:10.1016/j.brat.2011.11.005
- Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66(1):20–40. doi:10.1207/s15327752jpa6601_2
- Boffo M, Mannarini S, Munari C. Exploratory structure equation modeling of the UCLA loneliness scale: a contribution to the Italian adaptation. TPM Test Psychom Methodol Appl Psychol. 2012;19(4). doi:10.4473/TPM19.4.7
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arc Intern Med. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. primary care evaluation of mental disorders. patient health questionnaire. JAMA. 1999;282(18):1737–1744. doi:10.1001/jama.282.18.1737
- Mazzotti E, Fassone G, Picardi A, et al. II Patient Health Questionnaire (PHQ) per lo screening dei disturbi psichiatrici: uno studio di validazione nei confronti della Intervista Clinica Strutturata per il DSM-IV asse I (SCID-I). Italian J Psychopathol. 2003;9(3):235–242.
- Christianson S, Marren J. The Impact of Event Scale - Revised (IES-R). Medsurg Nurs. 2012;21(5):321–322.
- Craparo G, Faraci P, Rotondo G, Gori A. The impact of event scale - revised: psychometric properties of the Italian version in a sample of flood victims. Neuropsychiatr Dis Treat. 2013;9:1427–1432. doi:10.2147/NDT.S51793
- Liu X, Kakade M, Fuller CJ, et al. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry. 2012;53(1):15–23. doi:10.1016/j.comppsych.2011.02.003
- Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020. doi:10.3390/ijerph17051729
- Wang C, López-Núñez MI, Pan R, et al. The Impact of the COVID-19 pandemic on physical and mental health in China and Spain: cross-sectional Study. JMIR Form Res. 2021;5(5):e27818. doi:10.2196/27818
- Wang C, Tripp C, Sears SF, et al. The impact of the COVID-19 pandemic on physical and mental health in the two largest economies in the world: a comparison between the United States and China. J Behav Med. 2021;44(6):741–759. doi:10.1007/s10865-021-00237-7
- Wang C, Fardin MA, Shirazi M, et al. Mental health of the general population during the 2019 coronavirus disease (COVID-19) pandemic: a tale of two developing countries. Psychiatry International. 2021;2(1):71–84. doi:10.3390/psychiatryint2010006
- Tee ML, Tee CA, Anlacan JP, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. 2020;277:379–391. doi:10.1016/j.jad.2020.08.043
- Davico C, Ghiggia A, Marcotulli D, Ricci F, Amianto F, Vitiello B. Psychological impact of the COVID-19 pandemic on adults and their children in Italy. Front Psychiatry. 2021;12(12):572997. doi:10.3389/fpsyt.2021.572997
- Caliandro M, Fabiana G, Surgo A, et al. Impact on mental health of the COVID-19 pandemic in a radiation oncology department. Radiol med. 2022;127:220–224. doi:10.1007/s11547-021-01440-x
- Matias T, Dominski FH, Marks DF. Human needs in COVID-19 isolation. J Health Psychol. 2020;25(7):871–882. doi:10.1177/1359105320925149
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behav Res Ther. 1998;36(4):455–470. doi:10.1016/s0005-7967(97)10031-6
- Sica C, Musoni I, Bisi B, Lolli V, Sighinolfi C. Social phobia scale e social interaction anxiety scale: traduzione e adattamento italiano. Bollettino Di Psicologia Applicata. 2007;252:59.
- Hao F, Tan W, Jiang L, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020;87:100–106. doi:10.1016/j.bbi.2020.04.069
- Carrión GC, Nitzl C, Roldán JL. Mediation analyses in partial least squares structural equation modeling: guidelines and empirical examples. In: Partial Least Squares Path Modelling. Cham: Springer; 2017:173–195.
- Stickley A, Matsubayashi T, Ueda M. Loneliness and COVID-19 preventive behaviours among Japanese adults. J Public Health (Oxf). 2021;43(1):53–60. doi:10.1093/pubmed/fdaa151
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorder. 5th ed. 2013. doi:10.1176/appi.books.9780890425596
- Erzen E, Çikrikci Ö. The effect of loneliness on depression: a meta-analysis. Int J Soc Psychiatr. 2018;64(5):427–435. doi:10.1177/0020764018776349
- Bhaskar S, Rastogi A, Menon KV, Kunheri B, Balakrishnan S, Howick J. Call for action to address equity and justice divide during COVID-19. Front Psychiatry. 2020;11:559905. doi:10.3389/fpsyt.2020.559905
- Burki T. The indirect impact of COVID-19 on women. Lancet Infect Dis. 2020;20(8):904–905. doi:10.1016/S1473-3099(20)30568-5
- Almeida M, Shrestha AD, Stojanac D, Miller LJ. The impact of the COVID-19 pandemic on women’s mental health. Arch Womens Ment Health. 2020;23(6):741–748. doi:10.1007/s00737-020-01092-2
- Liu Y, Li P, Lv Y, et al. Public awareness and anxiety during COVID-19 epidemic in China: a cross-sectional study. Compr. Psychiatry. 2021;107:152235. doi:10.1016/j.comppsych.2021.152235
- Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40–48. doi:10.1016/j.bbi.2020.04.028
- Hao F, Wang B, Tan W, et al. Attitudes toward COVID-19 vaccination and willingness to pay: comparison of people with and without mental disorders in China. BJPsych Open. 2021;7(5):e146. doi:10.1192/bjo.2021.979
- Ho CS, Chee CY, Ho RC. Mental health strategies to combat the psychological impact of coronavirus disease 2019 (COVID-19) beyond paranoia and panic. Ann Acad Med Singap. 2020;49(3):155–160. doi:10.47102/annals-acadmedsg.202043
- Zhang MW, Ho RC. Moodle: the cost effective solution for internet cognitive behavioral therapy (I-CBT) interventions. Technol Health Care. 2017;25(1):163–165. doi:10.3233/THC-161261
- Soh HL, Ho RC, Ho CS, Tam WW. Efficacy of digital cognitive behavioural therapy for insomnia: a meta-analysis of randomised controlled trials. Sleep Med. 2020;75:315–325. PMID: 32950013. doi:10.1016/j.sleep.2020.08.020