Abstract
Background and Goals
Psychotherapy is one of the most highly recommended and practiced approaches for the treatment of Generalized anxiety disorder (GAD). Commonly defined as excessive worry that is uncontrollable, GAD is one of the most prevalent psychiatric disorders. Anxiety is also one of the most common associated symptoms of migraine. Exposing migraineurs to narrow band green light (nbGL) reduces their anxiety and anxiety-like physiological symptoms such as throat tightness, shortness of breath, and palpitations. Here, we sought to determine whether the reduced anxiety described by our patients was secondary to the reduced headache or independent of it. The goal of the current study was therefore to determine whether exposure to nbGL can reduce anxiety in GAD patients who are not migraineurs.
Patients and Methods
Included in this open-label, proof-of-concept, prospective study were 13 patients diagnosed with moderate-to-severe GAD. We used the State-Trait Anxiety Inventory Questionnaire (Y-1) to compare anxiety level before and after each 45-minutes psychotherapy session conducted in white light (WL) (intensity = 100±5 candela/m2) vs nbGL (wavelength = 520±10nm (peak ± range), intensity = 10±5 candela/m2).
Results
Here, we show that psychotherapy sessions conducted under nbGL increase positive and decrease negative feelings significantly more than psychotherapy sessions conducted under regular room light (χ2 = 0.0001).
Conclusion
The findings provide initial evidence for the potential benefit of conducting psychotherapy sessions for patients suffering GAD under nbGL conditions. Given the absence of side effects or risks, we suggest that illuminating rooms used in psychotherapy with nbGL be considered an add-on to the treatment of GAD.
Introduction
Migraine is a debilitating neurological disorder characterized by recurrent headaches often accompanied by throbbing, nausea, photophobia, phonophobia and various other abnormal sensory, autonomic, affective (eg, anxiety, depression) and cognitive functions.Citation1 Affecting about 15% of the US populationCitation2,Citation3 and worldwide, migraine is the 6th most common disease and the 2nd leading cause of years lived with disability.Citation4 The high prevalence of migraine (3-4-fold higher in women than in men)Citation5 and the $36 billion it costs the US annually explain its profound socioeconomic burden.Citation6–9
Exacerbation of headache by light (photophobia) is experienced by 8/10 migraineurs with normal eyesightCitation10–12 and by visually impaired migraineurs.Citation13 Photophobia, although not as incapacitating as the headache, renders migraineurs dysfunctional as they are forced to quit their most fundamental daily tasks and seek the comfort of darkness. Because of the repetitiveness and frequency of the disease, migraineurs endure a significant hardship due to spending so much time in solitude during working hours or at times in which they must care for their family at home.Citation14 Historically, photophobia impact on migraine patients, although widely known, did not receive much attention. At one point, drugs could be approved for migraine pain without any demonstrated benefit on associated symptoms. Subsequently, the FDA decided that migraine was a complex neurological disorder and that acute migraine treatments needed to improve more than the pain. That led the FDA to adapt the 4 coprimary solution whereby acute migraine treatments had to statistically separate from placebo on pain, nausea, photophobia and phonophobia.
Studying the neural mechanisms of photophobia, we found that blue and red light exacerbate migraine headache more than amber and white light, whereas a specific narrow band of green light (nbGL; wavelength = 520±10 nm) eases rather than worsens headache intensity.Citation15 Attempting to understand these unexpected psychophysical findings, we used electroretinography to record the electrical signals the eyes send to the brain in response to each color of light, and the signals they generate in the cortex (using visual evoked potential), and reported that in migraineurs, white and narrow bands of blue, amber, and red lights generate significantly larger electrical signals in the eye and cortex than nbGL.Citation15 In parallel pre-clinical studies, we also described a novel retino-thalamo-cortical pathway that allows brain areas that process vision to “talk” to brain areas that mediate the classical pain of migraine as well as some of its most commonly associated cognitive (eg, clarity of thinking, memory and attention), affective (eg, anxiety, irritability) and sensory (eg, photophobia, phonophobia, osmophobia) symptoms.Citation16 A few years later, an independent group described long-lasting antinociceptive effects of nbGL in different animal models of pain.Citation17,Citation18
While studying the effects of colors on migraine patients, we took note of patients who found blue, red, and amber lights extremely unpleasant even when their headache intensity did not increase. After studying these patients more carefully, we reported that exposure to blue, red, amber, and white lights during migraine can be aversive as these colors of light increase anxiety level and trigger anxiety-like symptoms such as chest and throat tightness, shortness of breath, fast breathing, palpitations, dizziness, nausea, and lightheadedness by activating hypothalamic neurons that regulate pre-ganglionic sympathetic and parasympathetic neurons in the thoracic spinal cord and brainstem superior salivatory nucleus, respectively.Citation19 Unexpectedly, we found that exposure to nbGL replaced patients’ perception of anxiety with the perception of feeling calm, relaxed, and happy.Citation19
As the number of migraine patients who choose to use the lamp that emits the nbGL (Allay Lamp) for alleviating their headache increases, the number of subjects reporting that nbGL also reduces their anxiety rises. Given that nbGL encompasses only a small fraction of the full human visible light spectrum (380–700 nm), it is considered less than minimal risk by IRBs. As such, we sought to determine if the use of this non-invasive, risk-free lamp to illuminate rooms in which people diagnosed with moderate-to-severe generalized anxiety disorder (GAD) undergo psychotherapy could improve within-session treatment outcome as determined by comparing anxiety levels before and immediately after sessions conducted in regular “white” room light vs nbGL. Our lead hypothesis was that nbGL ability to reduce anxiety is not unique to the anxiety that migraine patients feel during acute attack. Rather, that it is achieved through nbGL ability to foster calmness in GAD patients who are excessively worried and anxious about work, school, home, and social performancesCitation20 – possibly through the unique ability of this light to reduce cortical excitability, responsivity and sensitivity,Citation14 and hypothalamic activation of the sympathetic nervous system.Citation19
Design/Methods
The findings reported in this study were collected between April and December 2021 from moderate-to-severe GAD subjects undergoing in-person psychotherapy sessions at the Delray Center for Healing (a comprehensive mental health treatment clinic in Florida). Institutional Review Board (IRB) approval for the conduct of human subject research was obtained from the Ethics and Human Research Protection Program of Florida Health (Federal Wide Assurance # 00004682). The study was conducted according to Good Clinical Practice and the Declaration of Helsinki. ClinicalTrial.gov identifier: NCT04871087
Study Design
The overall goal of this prospective, open-label, proof-of-concept study was to evaluate effects of conducting psychotherapy sessions under regular room light (ie, white) vs nbGL on subjects undergoing repeated psychotherapy treatment sessions for the management of their anxiety. Patients of the Delray Center were presented with the option to participate in this study by their therapists. Those who signed the informed consent were instructed to mark the answers that best reflected their feelings on each of the 20 items in the State-Trait Anxiety Inventory Questionnaire (STAI Y-1) at the beginning and end of each 45-min therapy session with their regular psychotherapist. To complete the study, each participant had to attend a total of 8 sessions (). Of these, 2 sessions were conducted in regular (intensity reflecting from the walls and floor and reaching the patient’s eyes was measured at 100±5 candela/m2) white light (a standard mixture of the visible spectrum – wavelengths 380–750 nm), and 6 sessions were conducted in nbGL [wavelength: 520 ±10 nm (peak±range), intensity reflecting from the walls and floor and reaching the patient’s eyes was measured at 10±5 candela/m2, delivered by Allay Lamp, USA]. We chose this narrow band of green light as it allows 90% of the light to be distributed within a range that is least likely to activate the blue and red sensing retinal cones, and nearly maximally likely to activate the green sensing cones.
Intervention
Consistent with all our previous studies,Citation15,Citation19,Citation21,Citation22 the device emitting the nbGL (Allay Lamp) was the only source of light in the rooms in which the 45-min psychotherapy sessions were conducted. To illuminate the entire room, the lamp was placed on a high shelf and set at an intensity that allowed the therapist and the patient to see effortlessly during the session (measured at 10 ± 5 candela/m2).
Recruitment and Data Collection
Recruited to this study were men and women fulfilling diagnostic criteria for Generalized Anxiety Disorder (GAD) as defined in the DSM-5.Citation23 As part of the inclusion criteria, we required participants to be able to communicate in English and answer each of the 20 questions in the STAI Y-1 form, and be between the ages of 18–75. Since each patient provided answers before and after exposure to white light and nbGL, thus allowing us to conduct within-subject analysis, no exclusion criteria were implemented.
Data Analysis
In this within-subject (repeated measures) study design comparing the effects of conducting 2 psychotherapy sessions under white light (WL) and 6 sessions under nbGL, GAD patients provided self-evaluation using the State part of the State-Trait Anxiety Inventory questionnaire to choose one answer (out of 4 options) to 10 questions that reflect positive feelings and 10 questions that reflect negative feelings at the beginning and end of each psychotherapy session. The 4 options for each question were: (1) Not at all; (2) Somewhat; (3) Moderately so; (4) Very much so. The 10 positive-worded questions were: (1) I feel calm, (2) I feel secure, (3) I feel at ease, (4) I feel satisfied, (5) I feel comfortable, (6) I feel self-confident, (7) I am relaxed, (8) I feel content, (9) I feel steady, (10) I feel pleasant. The 10 negative-worded questions were: (1) I am tense, (2) I feel strained, (3) I feel upset, (4) I am presently worrying, (5) I feel frightened, (6) I feel nervous, (7) I am jittery, (8) I feel indecisive, (9) I am worried, (10) I feel confused.
To determine improvement per light condition, we averaged the scores that each question was given before the 2 sessions under white light, and after the 2 sessions under white light. A positive question that scored higher and a negative question that scored lower after the session (compared to before) were marked as improvement and received a score of 1. Next, we added the number of questions that improved in each patient based on responses to all positive and all negative questions (these numbers appear in each row in ). This process was repeated for the 6 sessions in which psychotherapy was conducted under nbGL conditions. The results obtained from each of the 13 participants who completed the 2 WL and 6 nbGL sessions were computed and the sums of all improved positive and negative items were compared using Chi square.
Table 1 A Summary of All 13 Patients’ Improved Responses to All 20 Questions Before and After the 2 Sessions in WL and 6 Sessions in the nbGL
To determine the predictive power of each item (and to make the process simpler and more user-friendly), we counted the number of times each question received a score of 1 (ie, reflecting improvement after the treatment session as compared to before) among all 13 participants and compared values obtained under white light vs nbGL. The questions in which the improvement was more than 50% under nbGL as compared to WL were considered the most predictive items and were, therefore, used in our final analysis.
The overall effectiveness of all psychotherapy sessions conducted under white and nbGL was analyzed using patients’ responses to 3 positive-worded and 4 negative-worded items (as explained above). Values were tested for normality, presented as median and interquartile range, and compared using the non-parametric Wilcoxon signed-rank test.
Data and Materials Availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Results
Database
Thirteen participants diagnosed with GAD provided data for this study at the beginning and end of 104 psychotherapy sessions. They were 18–62 y/o male (n = 7) and female (n = 6) subjects with >2 years history of disease. Each dataset consists of participants’ answers of 20 questions. A total of 4160 answers (2080 answers collected before treatment session and 2080 collected after treatment session) were analyzed. Of the 4160 questions/answers, 2080 were related to positively worded symptoms and 2080 to negatively worded symptoms.
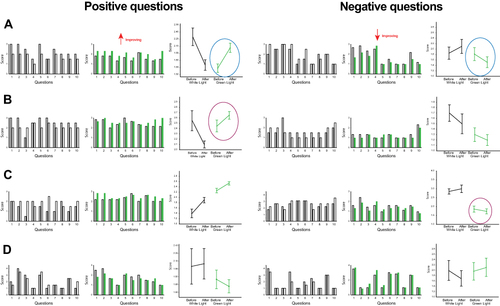
Analysis of participants’ responses to all 20 (questions) items: In 6 (46%) patients, improvement in psychotherapy sessions conducted under nbGL was shown by their answers to both the positive and negative questions (). In 5 (38%) patients, improvement under nbGL was shown by their answers to the positive but not negative questions, or vice-versa by their answers to the negative but not positive questions (). In 2 (15%) patients, responses to positive or negative questions reflected no improvement with the nbGL (). A summary of all 13 patients’ improved responses to all 20 questions before and after the 2 sessions in WL and 6 sessions in the nbGL is shown in . Under nbGL, patients reported increased positive feeling plus decreased negative feeling significantly more frequently than under WL (positively worded: WL = 35 vs nbGL = 71 times, χ2 = 0.000005, DF = 1; negatively worded: WL = 41 vs nbGL = 72 times, χ2 = 0.0001, DF = 1).
Figure 2 Analysis of participants’ responses to all 20 items in the State-Trait Anxiety Inventory (STAI Form Y-1). Histograms illustrate the score each item received before (gray bar) and after psychotherapy sessions conducted under white light (white bars) and narrow band green light (green bars). Answers to positively worded questions are shown on the left, and answers to negatively worded questions are shown on the right. Positively worded questions included: 1. I feel calm, 2. I feel secure, 3. I feel at ease, 4. I feel satisfied, 5. I feel comfortable, 6. I feel self-confident, 7. I am relaxed, 8. I feel content, 9. I feel steady, 10. I feel pleasant. Negatively worded questions included: 1. I am tense, 2. I feel strained, 3. I feel upset, 4. I am presently worrying over possible misfortunes, 5. I feel frightened, 6. I feel nervous, 7. I am jittery, 8. I feel indecisive, 9. I am worried, 10. I feel confused. Each question was scored as follows: 1 - not at all, 2 - somewhat, 3 - moderately so, 4 = very much so. Line plots illustrate mean ± SD of scores each subject provided for all 10 positively worded and all 10 negatively worded items before and after the 2 sessions in white light and 6 sessions in nbGL. (A) Example of a patient in which improvement in psychotherapy sessions conducted under nbGL was shown by the answers to both positive and negative questions (circled). (B) Example of a patient in which improvement under nbGL was shown by the answers to the positive (circled) but not negative questions. (C) Example of a patient in which improvement under nbGL was shown by the answers to the negative (circled) but not positive questions. (D) Example of a patient in which responses to positive or negative questions reflected no improvement under nbGL.
Individual Questions Analysis
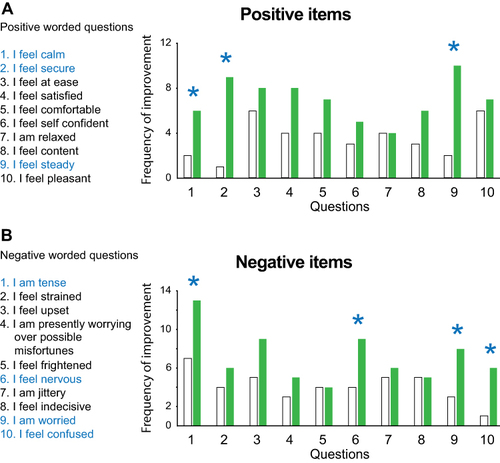
Analysis of the frequency of improved individual question (defined in Methods) under WL vs nbGL conditions identified 7 items (3 positively worded items = calm, secure, and steady; and 4 negatively worded items = tense, nervous, worried, and confused) where improvement under nbGL was >50% higher than under WL (). All other 13 items showed no difference or <50% difference in frequency of improvement under nbGL.
Figure 3 Item-by-item analysis: (A) Analysis of the frequency of positive items showing improvement under WL (white bars) as compared to nbGL (green bars) conditions. (B) Analysis of the frequency of negative items showing improvement under WL (white bars) as compared to nbGL (green bars) conditions. Asterisks depict items where improvement under nbGL was >50% higher than under WL.
Effectiveness of Psychotherapy Sessions Conducted Under nbGL vs WL
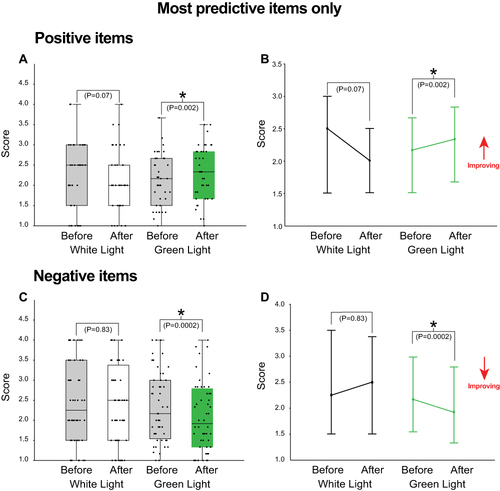
Analysis of the 3 most predictive positively worded items showed that psychotherapy sessions conducted under WL were less effective (before session: 2.5 [1.5–3.0] median [IQR] vs after session: 2.0 [1.5–2.5] p = 0.07 Wilcoxon) than sessions conducted under nbGL (before session: 2.1 [1.5–2.6] vs after session: 2.3 [1.6–2.8] p = 0.002 Wilcoxon) ( and ). Analysis of the 4 most predictive negatively worded items showed that psychotherapy session conducted under WL was less effective (before session: 2.2 [1.5–3.5] median [IQR] vs after session: 2.5 [1.5–3.3] p = 0.83 Wilcoxon) than sessions conducted under nbGL (before session: 2.1 [1.5–3.0] vs after session: 1.9 [1.3–2.7] p = 0.0002 Wilcoxon) ( and ).
Figure 4 Effectiveness of psychotherapy under nbGL vs WL. (A) Analysis of the 3 most predictive positively worded items. In the scatograms, each of the 39 dots represents the average of the scores given by each of the 13 patients to each item before and after exposure to white (average of 2 sessions) and nbGL (average of 6 sessions) lights. The Boxplots show median and IQR. (C) Analysis of the 4 most predictive negatively worded items. In the scatograms, each of the 52 dots represents the average of the scores given by each of the 13 patients to each item before and after exposure to white (average of 2 sessions) and nbGL (average of 6 sessions) lights. The Boxplots show median and IQR. (B and D) Line plots of median and IQR show direction of improvement. Asterisks depict significant difference p<0.05 Wilcoxon signed rank test.
Discussion
Psychotherapy is one of the most highly recommended and practiced approaches for the treatment of GAD.Citation24 It is most commonly practiced at regular (white) room light. In this open-label, proof-of-concept, prospective study, we show that psychotherapy sessions conducted under a specific narrow band of green light improves treatment outcome as judged by changes in level of anxiety after, as compared to before a 45-min treatment session by licensed therapists. Given the non-invasive nature of nbGL, its affordability, and the absence of adverse events, we suggest that illuminating rooms used in psychotherapy with nbGL be considered an affordable add-on to the treatment of GAD. The nature of this study, the small number of participants, and the findings justify carrying out a large-scale, double-blind, randomized controlled trial.
Generalized anxiety disorder, commonly defined as excessive worry that is uncontrollable, is one of the most prevalent psychiatric disorders.Citation25,Citation26 It affects more women than men,Citation27 mostly those younger than 50 y/o, and it carries with it a high burden of illness.Citation28,Citation29 Pathophysiologically, it is thought to be maintained by cognitive biases toward events/stimuli that are potentially threatening or worrisome and the development of overly cautious behavior aimed at avoiding autonomic arousal,Citation30,Citation31 somatic anxiety symptoms such as palpitations, dizziness, nausea, and muscle tension, and psychological symptoms such as nervousness, insomnia, and constant worry.Citation32 To date, most experts advocate psychotherapy, pharmacotherapy, or both, for the treatment of anxiety and its somatic and psychological symptoms. While the proven efficacy of anxiolytic drugs such as the benzodiazepines define a gold standard for pharmacotherapy, risky side effects, development of dependence and the introduction of withdrawal syndrome have led patients and health-care providers to seek alternative, less harmful treatment approaches. According to the European Study of the Epidemiology of Mental Disorders (ESEMeD), psychotherapy is one of the more commonly used alternative and/or complementary approaches to the treatment of GAD.Citation27,Citation33,Citation34 In spite of being highly recommended by the World Health Organization trials portal, the use of psychotherapy is challenged by methodological issues used to estimate magnitude of effect (as the use of placebo is difficult to establish), and by high rates of patient-initiated premature termination.Citation35–39 One of the many recognized causes of patient-initiated premature termination of psychotherapyCitation35 is loss of motivation,Citation40 possibly due to lack of immediate benefit (ie, potential to decrease anxiety level within a single psychotherapy session) to the patient. The current study raises the possibility that motivation to continue with psychotherapy may be enhanced by conducting sessions under conditions of nbGL illumination as it increases patients’ perception of within-session benefit of reduced level of anxiety (ie, immediate reward).
The discovery that low-intensity nbGL reduces anxiety is relatively new.Citation18,Citation19,Citation41 It originated in a series of studies that initially attempted to understand how light exacerbates migraine headache. These studies have led to the discovery of 3 novel neural pathways by which color/light can alter sensory, physiological, cognitive, and emotional states. The first, called the retino-thalamo-cortical pathway, allows nbGL to reduce the perception of pain and headache, abnormal sensitivity to light, and, surprisingly, transient impairment in cognitive functions such as clarity of thinking, memory and attentionCitation13,Citation15,Citation16 - symptoms commonly described during migraine.Citation1 The second, called the retino-hypothalamic-sympathetic pathway, allows nbGL to reduce somatic anxiety symptoms such as chest and throat tightness, shortness of breath, fast breathing, and palpitations by activating hypothalamic neurons that regulate sympathetic outflow,Citation19 and the third, called the retino-hypothalamic-parasympathetic pathway, allows nbGL to reduce the perception of dizziness, nausea, and lightheadedness by activating different classes of hypothalamic neurons that regulate parasympathetic outflow.Citation19 While the exact mechanism by which nbGL reduces overall brain excitability is not fully understood, human electrophysiological studies show that compared to red and blue lights, nbGL generates significantly smaller electrical signals in the retina (measured by electroretinography recording) and cortex (measured by recording visual evoked potentials). Thus, it is reasonable to propose that the anxiolytic effects of nbGL may be achieved by its ability to (a) reduce neuronal excitability and responsivity in cortical (eg, prefrontal cortex) and subcortical (eg, amygdala) areas involved in the pathophysiology of GAD,Citation42–46 (b) alter autonomic responses to negative emotions such as stress, fear, and anxiety,Citation47 and (c) stimulate hypothalamic neurons that release chemicals such as oxytocin, dopamine, and GABA.Citation19,Citation48
Conclusions
The findings provide initial evidence for the potential benefit of conducting psychotherapy sessions with patients suffering GAD under dim nbGL conditions. The lamp that emits this specific band of green light (the Allay Lamp) is affordable, non-invasive, and risk-free. Future randomized controlled trials are needed to evaluate the use of this nbGL as an add-on tool to increase patients’ perception that each psychotherapy session reduces their anxiety. If successful, such confirmation can reduce patient-initiated premature termination due to lack of immediate gratification – a common expectation since the ubiquitous embrace of the internet.
Caveats: (a) As with all small, prospective, open-label, proof-of-concept studies, the findings must be interpreted with caution as only an appropriately powered, multi-center, randomized controlled trial can provide the strength of evidence needed to recommend the use of this intervention. (b) Whereas the intensity of the regular (white) room light was 100 candela/m2, the intensity of the nbGL was 10±5 candela/m2. This difference raises the possibility that the improved outcome seen during the session conducted under nbGL (as compared to regular room light) may be attributed to the intensity of the light rather than the color. Our previous studiesCitation15,Citation19 refute this possibility. By showing that white light is aversive to the extent that it exacerbates the headache at intensities as low as 1, 5, and 20 candela/m2 (eg, see and in reference 6), while nbGL alleviates the headache and its aversive aspects at low (1 and 5 candela/m2), medium (20 candela/m2) and high (50 candela/m2) intensities, we concluded that the therapeutic effects of nbGL are achieved due to its ability to activate retinal cones that are most sensitive to wavelengths of the green light and least sensitive to retinal cones that detect wavelengths of the red and blue lights (ie, the color effect), rather than the intensity on the these lights. (7) Given that symptoms such as fatigued, difficulty concentrating, irritability, muscle tension, and sleep disturbance are common in both migraine and GAD, and that excessive worry about when the next attack will commence can give rise to anxiety in those experiencing frequent migraine attacks, electrophysiological and neuroimaging studies that focus on nbGL effects on brain areas involved in anxiety and migraine, anxiety but not migraine and migraine but not anxiety are needed to determine whether the mechanism by which nbGL reduce anxiety differ when patients experience GAD but no headache or headache and anxiety.
Disclosure
Dr Sait Ashina reports personal fees from Abbvie/Allergan, Eli Lilly and Company, Novartis, Amgen, Satsuma, Impel NeuroPharma, Biohaven, Percept, and Theranica, outside the submitted work. Rami Burstein reports the following conflicts within the past 12 months: Research Support: National Institutes of Health, AbbVie/Allergan, Eli Lilly, Teva. Consulting: Alder, Allergan/AbbVie, Amgen/Novartis, Biohaven, Dr. Reddy Lab, Eli Lilly, Ipsen, Neurolief, Percept, Revance, Teva, Theranica. Options: Theranica, Percept, Allay. Patents: 9061025: Methods for selecting headache patients responsive to botulinum toxin therapy, 11732265.1: Method and compositions for the treatment of migraine headaches, endothelial dysfunction and muscle tenderness with statin and vitamin D, US 10,766,952 B2: Methods for selecting a headache patient responsive to treatment with an anti-CGRP antibody and for reducing headache frequency in the selected patients comprising administering an anti-CGRP antibody, 10806890: Method and apparatus for managing photophobia and migraine photophobia, US2021-0015908: Methods for treating and for inhibiting progression of seizures, WO21007165: Methods for treating and for inhibiting progression of seizures, US2021-0128724: CGRP antagonists and clostridial derivatives for the treatment of cortical spreading depression associated disorders, WO21005497: CGRP antagonists and clostridial derivatives for the treatment of cortical spreading depression associated disorders. All other authors have no relevant financial or non-financial interests to disclose for this work.
Acknowledgments
Lamps emitting the narrow band green light were provided by Allay. No other support was provided for this study. We thank Lacey Burkett, Skyler Rosen, Erica Sanes, and Cara Harbaugh for their role in conducting the psychotherapy sessions at the different light conditions.
References
- Olesen J, Goadsby P, Ramadan NM, Tfelt-Hansen P, Welch KMA. The Headaches. Third ed. Philadelphia: Lippincott Williams & Wilkins; 2006.
- Burch R, Rizzoli P, Loder E. The prevalence and impact of migraine and severe headache in the United States: figures and trends from government health studies. Headache. 2018;58(4):496–505. doi:10.1111/head.13281
- Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68(5):343–349. doi:10.1212/01.wnl.0000252808.97649.21
- Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1211–1259.
- Stewart WF, Wood C, Reed ML, Roy J, Lipton RB, Group AA. Cumulative lifetime migraine incidence in women and men. Cephalalgia. 2008;28(11):1170–1178. doi:10.1111/j.1468-2982.2008.01666.x
- Goldberg LD. The cost of migraine and its treatment. Am J Manag Care. 2005;11(2 Suppl):S62–67.
- Hawkins K, Wang S, Rupnow M. Direct cost burden among insured US employees with migraine. Headache. 2008;48(4):553–563. doi:10.1111/j.1526-4610.2007.00990.x
- Hawkins K, Wang S, Rupnow MF. Indirect cost burden of migraine in the United States. J Occup Environ Med. 2007;49(4):368–374. doi:10.1097/JOM.0b013e31803b9510
- Bonafede M, Sapra S, Shah N, Tepper S, Cappell K, Desai P. Direct and indirect healthcare resource utilization and costs among migraine patients in the United States. Headache. 2018;58(5):700–714. doi:10.1111/head.13275
- Liveing E. On Megrim, Sick Headache. Nijmegen: Arts & Boeve Publishers; 1873.
- Selby G, Lance JW. Observations on 500 cases of migraine and allied vascular headache. J Neurol Neurosurg Psychiat. 1960;23:23–32. doi:10.1136/jnnp.23.1.23
- Drummond PD. A quantitative assessment of photophobia in migraine and tension headache. Headache. 1986;26(9):465–469. doi:10.1111/j.1526-4610.1986.hed2609465.x
- Noseda R, Kainz V, Jakubowski M, et al. A neural mechanism for exacerbation of headache by light. Nat Neurosci. 2010;13(2):239–245. doi:10.1038/nn.2475
- Burstein R, Noseda R, Fulton AB. Neurobiology of Photophobia. J Neuroophthalmol. 2019;39(1):94–102. doi:10.1097/WNO.0000000000000766
- Noseda R, Bernstein CA, Nir RR, et al. Migraine photophobia originating in cone-driven retinal pathways. Brain. 2016;139(139):1971–1986. doi:10.1093/brain/aww119
- Noseda R, Jakubowski M, Kainz V, Borsook D, Burstein R. Cortical projections of functionally identified thalamic trigeminovascular neurons: implications for migraine headache and its associated symptoms. J Neurosci. 2011;31(40):14204–14217. doi:10.1523/JNEUROSCI.3285-11.2011
- Ibrahim MM, Patwardhan A, Gilbraith KB, et al. Long-lasting antinociceptive effects of green light in acute and chronic pain in rats. Pain. 2017;158(2):347–360. doi:10.1097/j.pain.0000000000000767
- Martin LF, Patwardhan AM, Jain SV, et al. Evaluation of green light exposure on headache frequency and quality of life in migraine patients: a preliminary one-way cross-over clinical trial. Cephalalgia. 2021;41(2):135–147. doi:10.1177/0333102420956711
- Noseda R, Lee AJ, Nir RR, et al. Neural mechanism for hypothalamic-mediated autonomic responses to light during migraine. Proc Natl Acad Sci U S A. 2017;114(28):E5683–E5692. doi:10.1073/pnas.1708361114
- Patriquin MA, Mathew SJ. The neurobiological mechanisms of generalized anxiety disorder and chronic stress. Chronic Stress. 2017;1. doi:10.1177/2470547017703993
- Nir RR, Lee AJ, Huntington S, et al. Color-selective photophobia in ictal vs interictal migraineurs and in healthy controls. Pain. 2018;159(10):2030–2034. doi:10.1097/j.pain.0000000000001303
- Bernstein CA, Nir RR, Noseda R, et al. The migraine eye: distinct rod-driven retinal pathways’ response to dim light challenges the visual cortex hyperexcitability theory. Pain. 2019;160(3):569–578. doi:10.1097/j.pain.0000000000001434
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Vol. 5. Washington DC: American Psychiatric Association; 2013.
- Bandelow B, Michaelis S, Wedekind D. Treatment of anxiety disorders. Dialogues Clin Neurosci. 2017;19(2):93–107. doi:10.31887/DCNS.2017.19.2/bbandelow
- Kessler RC, Ruscio AM, Shear K, Wittchen HU. Epidemiology of anxiety disorders. Curr Top Behav Neurosci. 2010;2:21–35.
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi:10.1001/archpsyc.62.6.593
- Bandelow B, Michaelis S. Epidemiology of anxiety disorders in the 21st century. Dialogues Clin Neurosci. 2015;17(3):327–335. doi:10.31887/DCNS.2015.17.3/bbandelow
- Chisholm D, Sweeny K, Sheehan P, et al. Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry. 2016;3(5):415–424. doi:10.1016/S2215-0366(16)30024-4
- Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. 2011;21(9):655–679. doi:10.1016/j.euroneuro.2011.07.018
- Otte C. Cognitive behavioral therapy in anxiety disorders: current state of the evidence. Dialogues Clin Neurosci. 2011;13(4):413–421. doi:10.31887/DCNS.2011.13.4/cotte
- Arch JJ, Craske MG. First-line treatment: a critical appraisal of cognitive behavioral therapy developments and alternatives. Psychiatr Clin North Am. 2009;32(3):525–547. doi:10.1016/j.psc.2009.05.001
- ICD-10. Classifcation of mental and behvioural disorders: clinical descriptions and diagnostic guidelines. In: “Blue Book” Clinical Descriptions and Diagnostic Guidelines. Geneva, Swotzerland: Worlde Health Organization; 1991.
- Alonso J, Lepine JP; Committee ESMS. Overview of key data from the European Study of the Epidemiology of Mental Disorders (ESEMeD). J Clin Psychiatry. 2007;68(Suppl 2):3–9.
- Nutt DJ, Kessler RC, Alonso J, et al. Consensus statement on the benefit to the community of ESEMeD (European Study of the Epidemiology of Mental Disorders) survey data on depression and anxiety. J Clin Psychiatry. 2007;68(Suppl 2):42–48.
- Ogrodniczuk JS, Joyce AS, Piper WE. Strategies for reducing patient-initiated premature termination of psychotherapy. Harv Rev Psychiatry. 2005;13(2):57–70. doi:10.1080/10673220590956429
- Swift JK, Greenberg RP. Premature discontinuation in adult psychotherapy: a meta-analysis. J Consult Clin Psychol. 2012;80(4):547–559. doi:10.1037/a0028226
- Owen J, Imel Z, Adelson J, Rodolfa E. ‘No-show’: therapist racial/ethnic disparities in client unilateral termination. J Couns Psychol. 2012;59(2):314–320. doi:10.1037/a0027091
- Krishnamurthy P, Khare A, Klenck SC, Norton PJ. Survival modeling of discontinuation from psychotherapy: a consumer decision-making perspective. J Clin Psychol. 2015;71(3):199–207. doi:10.1002/jclp.22122
- Wetherell JL, Unutzer J. Adherence to treatment for geriatric depression and anxiety. CNS Spectr. 2003;8(12 Suppl 3):48–59. doi:10.1017/S1092852900008270
- Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. doi:10.1016/S0140-6736(12)61689-4
- Martin L, Porreca F, Mata EI, et al. Green light exposure improves pain and quality of life in fibromyalgia patients: a preliminary one-way crossover clinical trial. Pain Med. 2021;22(1):118–130. doi:10.1093/pm/pnaa329
- Diekhof EK, Geier K, Falkai P, Gruber O. Fear is only as deep as the mind allows: a coordinate-based meta-analysis of neuroimaging studies on the regulation of negative affect. NeuroImage. 2011;58(1):275–285. doi:10.1016/j.neuroimage.2011.05.073
- Roy AK, Fudge JL, Kelly C, et al. Intrinsic functional connectivity of amygdala-based networks in adolescent generalized anxiety disorder. J Am Acad Child Adolesc Psychiatry. 2013;52(3):290–299 e292. doi:10.1016/j.jaac.2012.12.010
- Monk CS, Telzer EH, Mogg K, et al. Amygdala and ventrolateral prefrontal cortex activation to masked angry faces in children and adolescents with generalized anxiety disorder. Arch Gen Psychiatry. 2008;65(5):568–576. doi:10.1001/archpsyc.65.5.568
- Etkin A, Prater KE, Schatzberg AF, Menon V, Greicius MD. Disrupted amygdalar subregion functional connectivity and evidence of a compensatory network in generalized anxiety disorder. Arch Gen Psychiatry. 2009;66(12):1361–1372. doi:10.1001/archgenpsychiatry.2009.104
- Etkin A, Wager TD. Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry. 2007;164(10):1476–1488. doi:10.1176/appi.ajp.2007.07030504
- Teed AR, Feinstein JS, Puhl M, et al. Association of generalized anxiety disorder with autonomic hypersensitivity and blunted ventromedial prefrontal cortex activity during peripheral adrenergic stimulation: a randomized clinical trial. JAMA Psychiatry. 2022;79(4):323–332. doi:10.1001/jamapsychiatry.2021.4225
- Noseda R, Kainz V, Borsook D, Burstein R. Neurochemical pathways that converge on thalamic trigeminovascular neurons: potential substrate for modulation of migraine by sleep, food intake, stress and anxiety. PLoS One. 2014;9(8):e103929. doi:10.1371/journal.pone.0103929

