Abstract
Introduction
Migraine and asthma are two frequent, disabling, chronic disorders with a major impact on patient well-being. The objectives of this study were to compare subjective well-being between patients with severe forms of migraine or asthma using a panel of PROs.
Methods
Adult patients were recruited during routine consultations with chest physicians or neurologists. Patients with severe migraine (reporting headaches on ≥8 days/month and having failed ≥2 prophylactic treatments) and patients with severe asthma (according to the 2017 GINA definition: requiring Step 4 or 5 treatment or presenting uncontrolled symptoms) were eligible. Each patient completed the EuroQol Questionnaire (EQ-5D-5L), the Work Productivity and Activity Impairment Questionnaire (WPAI) and the Hospital Anxiety and Depression scale (HAD). Patients with severe migraine the 6-item Headache Impact Test (HIT-6) and those with severe asthma completed the Asthma Control Test (ACT).
Results
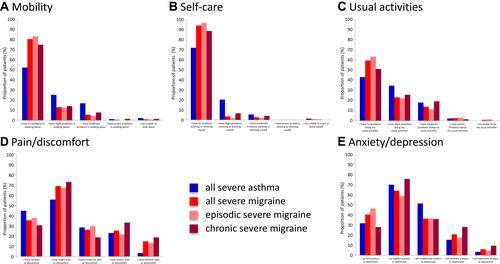
249 patients with severe migraine and 96 with severe asthma were enrolled. Mean EQ-5D-5L utility scores were significantly higher in the severe migraine group than in the severe asthma group (0.75±0.25 vs 0.68±0.26; p<0.01). Low EQ-5D-5L utility scores were associated with frequent (≥15 headache days/month) or disabling (HIT-6 score ≥60) headaches and with poor asthma control. Patients with severe migraine more frequently presented a HAD depression score ≥11 (23.0% in severe migraine; 7.5% in severe asthma; p<0.01), whereas those with severe asthma more frequently reported problems with mobility, self-care and usual activities. Absenteeism (percent worktime missed) was similar in both groups (severe migraine: 9.0%±19.1%; severe asthma: 13.8%±22.9%) but work impairment was higher in the severe migraine group (44.3% vs 28.4%; p<0.01).
Conclusion
Quality of life, work activity and psychological distress are all deteriorated in both severe migraine and severe asthma. Different aspects are affected in the two diseases: a greater impact on psychological aspects in severe migraine and a greater impact on physical aspects in severe asthma.
Introduction
Patient-reported outcome measures (PROMs) are designed to measure patient perceptions of their health and illness. These measures are important in routine clinical practice for gaining insight into how diseases affect general well-being and how these perceptions evolve over time. In clinical trials, they are important to measure the impact of treatments and disease management strategies on health perceptions. From a public health perspective, they are important in determining the burden of disease and for informing health policies and notably in prioritising the provision of health services.
Patient-reported outcome measures fall into two classes, generic measures and disease-specific measures. Generic PROMs, such as the Short-Form 36-item health profile (SF-36),Citation1 its shorter derivative the Short-Form 12-item health profile (SF-12),Citation2 the Sickness Impact Profile,Citation3 the Nottingham Health ProfileCitation4 and, more recently, the EuroQoL five dimension questionnaire (EQ-5D)Citation5 have been developed. These are useful for comparing health perceptions between different diseases. Specific PROMs are intended to determine health status in particular diseases and, as such, are designed to be highly sensitive to changes in functional domains that are specific for particular diseases (such as motor function in stroke patients). In common chronic diseases, such as migraineCitation6 and asthma,Citation7 large numbers of specific PROMs have been developed over the past three decades, spawning an abundant literature. For example, in migraine, the Migraine-Specific Quality of Life QuestionnaireCitation8 and 6-item Headache Impact Test (HIT-6)Citation9 are well established and validated. In asthma, the Asthma Quality-of-Life QuestionnaireCitation10 and the Asthma Control Test (ACT)Citation11 have been validated and used widely.
Comparing findings between the many studies that have used generic PROMs to evaluate perceived health status in individual diseases is complicated by methodological differences between studies, such as the context of the study, the source population, how patients were selected and how the PROMs were administered. For this reason, studies which compare PROM scores between different diseases using an identical methodology are more informative. In spite of this, there are relatively few within-study comparisons that have been published. A landmark study published over twenty years agoCitation12 compared the health status of patients measured with the SF-36 between eleven diseases and demonstrated marked differences in overall health perceptions, as well as in the impact on the different health dimensions of the questionnaire. Since then, other studies have compared health perceptions between different diseases, for example multiple sclerosis and Parkinson’s disease,Citation13 epilepsy versus angina pectoris, rheumatoid arthritis, asthma and chronic obstructive pulmonary disease,Citation14 different dermatological diseasesCitation15 or diabetes and asthma.Citation16
The objectives of this study were to assess and compare quality of life (QoL), work performance and psychological distress using a panel of PROMs between two groups of patients with one of two frequent, disabling chronic diseases: severe migraine and severe asthma. The rationale behind the choice of these two diseases is related to the recent introduction of new prophylactic treatments for severe migraine.Citation17 However, there is currently no consensus definition for severe migraine and the indication for these new treatments is an ad hoc one. On the other hand, a consensus definition of severe asthma was introduced by the Global Initiative for Asthma (GINA) over twenty years ago,Citation18 and the most recent formulation of the conceptCitation19 is over a decade old. In addition, international practice guidelines have recommended severity-based treatment strategies since 2014.Citation20 For this reason, there is extensive information on the relationship between patient perceptions of the impact of asthma, documented with different PROs, and asthma severity as defined by GINA. It is therefore of interest to evaluate whether the ad hoc definition of severe migraine corresponds to a similar level of patient-perceived impact as the accepted consensus definition of severe asthma.
Methods
This study was performed in a sample of patients consulting a specialist (neurologists or chest physicians) for severe migraine or severe asthma in France between 24th April and 22nd June 2018.
Severity definitions
Severe migraine is defined as having at least 8 days of migraine headache per month and to have failed at least two prophylactic treatments. Severe asthma is defined according to the 2017 GINA guidelines as “asthma that is uncontrolled despite adherence with maximal optimized therapy and treatment of contributory factors, or that worsens when high dose treatment is decreased”.Citation21
Recruitment of Physicians
Physicians were identified by random selection from a listing of practicing neurologists and chest physicians in France. Potential participants were recruited by telephone and were administered a screening questionnaire to validate that they fulfilled the eligibility criteria for this study. Specialists working in either hospital or community practice were eligible. Physicians were eligible to participate if they spent ≥60% of their professional activity seeing patients, had at least three years of specialist experience. Physicians were required to have around fifty percent of their patients having severe migraine or asthma and consulting regularly. This requirement was set in order to optimise the chances of recruiting the required number of patients with severe disease in each diagnostic group during the two-month recruitment period of the study.
Neurologists were required to see at least twenty patients with migraine in a typical month, of whom ten should present with severe migraine (defined as having at least 8 days of migraine headache per month) and should have failed at least two prophylactic treatments. Five of these patients should have episodic migraine (defined as 8–14 days of migraine per month) and five have chronic migraine (defined as ≥15 days of migraine per month). Chest physicians were required to be specialists in the treatment of severe asthma and to see at least twenty patients with asthma in a typical month, of whom ten should present severe asthma.
Recruitment of Patients
Each participating physician was expected to invite the next ten patients consulting consecutively during the two-month recruitment period and fulfilling the eligibility criteria to participate in the study. Patients under eighteen years of age, patients presenting another chronic invalidating disease and patients participating in any clinical study were excluded.
Patients with severe migraine were eligible if they had a physician-ascertained diagnosis, reported at least eight migraine days per month (MMD) and had failed at least two prophylactic treatments belonging to different therapeutic classes. Eligible patients were divided into episodic migraine (8–14 MMD) and chronic migraine (≥15 MMD) subgroups.
Patients with severe asthma were eligible if they had a physician-ascertained diagnosis of severe asthma according to the 2017 GINA guidelinesCitation21 and had not presented an exacerbation of asthma requiring a short course of oral corticosteroids in the previous month.
Data Collection
For each patient included, the physician completed a standardised medical questionnaire describing the demographic and clinical features of included patients, which enabled the eligibility criteria to be verified. Each patient enrolled completed an eight-page questionnaire including the five-level EQ-5D-5L,Citation5 the Work Productivity and Activity Impairment (WPAI) QuestionnaireCitation22 and the Hospital Anxiety and Depression (HAD) scale.Citation23 In addition, patients with migraine completed the HIT-6Citation9 and those with asthma the ACT.Citation11
The EQ-5D-5L assesses five aspects of QoL (mobility, self-care, usual activities, pain or discomfort and depression or anxiety) on five-point Likert scales. The profile of responses is converted into a linear, continuous utility measure ranging from −1 to 1. Since no valuation set for the EQ-5D-5L was available at the time the study was conducted, utility values for the EQ-5D-5L were derived from the existing EQ-5D-3L valuation set with the crosswalk method using a validated mapping function,Citation24 as recommended by NICE. In addition, a visual analogue scale (EQ-5D VAS) rates overall perception of QoL on a linear scale, yielding a score ranging from 0 (worst health the respondent can imagine) to 100 (best health the respondent can imagine).
The WPAI contains six items relating to health problems interfering with work or daily activities over the previous week: one yes/no question (are you currently employed [working for pay]?), three questions on the number of hours missed from work for different reasons and two questions on impact of health problems on work each rated on a ten-point ordinal scale. The WPAI yields four scores (absenteeism, presenteeism, work productivity loss and activity impairment), which can range from 0 (no impact on work/activities) to 100 (total incapacity). The HAD is a fourteen-item questionnaire assessing severity of symptoms of anxiety and depression, seven items relating to anxiety and seven to depression and each scored on a four-point Likert scale. Possible scores for each pathology dimension range from 0 to 21, with a higher score reflecting greater severity. A score over eight on either score corresponds to possible anxiety or depression and a score of ≥11 on either score corresponds to probable anxiety or depression.Citation25
The HIT-6 is a six-item questionnaire, which yields an impact score on a linear scale with minimum and maximum possible values of 36 and 78, respectively. On the basis of this score, subjects can be assigned to one of four impact grades (little or no impact, moderate impact, substantial impact and severe impact). The ACT is a questionnaire containing five items on symptoms or functioning in the previous four weeks, each rated on a five-point Likert scale. The total score can range from 5 (poor control of asthma) to 25 (complete control of asthma), with higher scores reflecting greater asthma control. An ACT score >19 indicates well-controlled asthma.
All questionnaires were used in their validated French translations.
Statistical Analysis
The target sample size was established a priori in order to obtain a precision of ≤10% (95% confidence intervals) for the different scores to be measured. In order to achieve this, 100 patients needed to be included in each patient group. For severe asthma, the recruitment target was set at 100 patients. For severe migraine, the recruitment target was set at 250 patients, in order to have 100 patients with chronic migraine, based on the distribution of migraine severity and frequency that has been described in France.Citation26
Regarding missing data, if none of the PRO questionnaires were completed in full, the patient was considered non-analysable. For the PRO questionnaires, if any of the items was not scored, the questionnaire was considered failed and was not analysed.
The presentation of the data is purely descriptive and no a priori hypotheses were tested. Continuous data are presented as mean values ± standard deviations (SD) or median values. Categorical variables are presented as frequency counts with percentages. Categorical and continuous variables were compared between groups using the χ2 test and Student’s t-test respectively. For the comparison between the distribution of response levels of the EQ-5D, the highest levels (4 and 5 or 3, 4 and 5) were combined when necessary to avoid empty cells or cells containing only one subject. All statistical analyses were performed using Quantum software version 5.8 (IBM, Armonk, United States).
Ethical Considerations
The survey was conducted in accordance with the ESOMAR International Code on Market and Social Practice, the EphMRA Code of Conduct, relevant current French and European legislation, and Good Epidemiological Practice guidelines. Since the patients’ identity did not appear on the study questionnaires and patient management was not affected by participation in the study, submission to an Institutional Review Board for ethical approval was not required. The physicians were required to give a letter of information to their patients who in turn were asked to provide oral consent to their physician before being able to take part in the survey. The letter of information included a summary of the recommendations of the French Data Protection Authority (Commission Nationale de l’Informatique et des Libertes; CNIL) on the protection of personal data and the processing of the data from the survey. Using a dedicated hotline, patients also had access to all data concerning them as well as the right to correct or delete such data, in conjunction with Kantar Health. To guarantee complete confidentiality, data collection, processing and analysis were centralised by Kantar Health.
Results
Participants
Nineteen neurologists (thirteen hospital-based and six community-based) and ten chest physicians (nine hospital-based and one community-based) participated in the study. These physicians recruited 250 patients with severe migraine and 100 with severe asthma. Data for one patient with severe migraine and four with severe asthma were not analysed as none of the PRO questionnaires were completed. The sociodemographic characteristics of the remaining analysable patients (249 with severe migraine and 96 with severe asthma) are presented in . For both disease groups, the mean age was similar, around 42 years, whereas women were more represented in the severe migraine group than in the severe asthma group (p <0.001). Mean BMI was somewhat lower (p <0.01) in the severe migraine group compared to the severe asthma group. No significant difference in any of these variables was observed between the patients with episodic migraine or with chronic migraine. Around half of the patients with severe asthma were registered for long-term disability status qualifying them for full health insurance coverage, whereas this was only the case for less than ten percent of patients with migraine. In both diseases, the mean time since diagnosis was around twenty years. The mean HIT-6 impact score in patients with severe migraine was 63.7, being higher in the patients with chronic migraine compared to episodic migraine. The mean ACT score in the severe asthma group was 14.5, being higher in controlled than in uncontrolled patients. The number of days in the previous month that patients took sick leave was lower in the severe migraine group than in the severe asthma group (p <0.05).
Table 1 Sociodemographic and Clinical Characteristics of the Study Population
Quality of Life
According to the EQ-5D-5L utility measures, mean scores were significantly higher in the severe migraine group than in the severe asthma group (p <0.01; ). Within the severe asthma group, the mean EQ-5D-5L utility score was higher in the patients with well- or partly controlled asthma than in those with uncontrolled asthma (0.83 ± 0.22 versus 0.59 ± 0.25; p <0.01). Within in the severe migraine group, mean scores were higher in patients with episodic migraine than in those with chronic migraine (p <0.01; ) and lower in those with a severe impact (HIT-6 score ≥ 60: 0.72 ± 0.26) compared to those with a HIT-6 score <60 (0.86 ± 0.16; p <0.01).
Table 2 Summary of Patient-Reported Outcomes
With regard to the EQ-5D VAS score, similar patterns were observed between the different patient groups, although the difference between the severe migraine and the severe asthma group was no longer significant (). The patterns of response to the different items of the EQ-5D-5L differed between the severe asthma and severe migraine groups (), with the former reporting more frequent problems with mobility (p <0.001), self-care (p <0.001) and, marginally, for usual activities (p = 0.046), and patients with severe migraine marginally reporting more frequent pain/discomfort (p = 0.035) and anxiety/depression (p = 0.05). The only difference in the distribution of ED-5Q response modalities between the chronic and episodic migraine groups was observed for the anxiety/depression dimension (p = 0.014).
Work Performance and Impairment
The level of absenteeism (time off work due to health problems) in the last week was similar in patients with severe migraine (9.0% ± 19.1) and in those with severe asthma (13.8% ± 22.9). In contrast, presenteeism (time at work when performance was impaired by health problems), work productivity loss and overall activity impairment were all significantly higher in patients with severe migraine than in those with severe asthma ().
Psychological Distress
In both patients with severe migraine and those with severe asthma, mean anxiety scores were relatively high (>8; ) and around 30% in both groups had scores considered indicative of clinical anxiety (≥11). No difference was observed in mean anxiety scores between these two groups, although the categorical distribution was marginally different (p = 0.04), suggesting more frequent anxiety in patients with migraine. The mean anxiety score was significantly higher in patients with chronic severe migraine than in those with episodic severe migraine but the categorical score distribution did not differ significantly according to headache frequency.
For the depression measure, mean scores were lower than the mean anxiety scores, but were significantly higher (p <0.01) in patients with severe migraine (6.9) than in those with severe asthma. The categorical distribution also differed significantly between the two groups (p <0.001), with the proportion of patients with scores consistent with clinical depression being higher in patients with severe migraine (23.0% versus 7.5% in severe asthma). Within the severe migraine group, mean depression scores and the proportion of patients with scores ≥11 were significantly higher in patients with chronic headaches compared to those with episodic headaches (p <0.01 in both cases).
Discussion
This study of PROMs in patients with severe migraine and severe asthma has shown that both these conditions are associated with deteriorations in quality of life, although the pattern of deterioration differs between the two. Mean EQ-5D utility scores were 0.68 in severe asthma and 0.75 in severe migraine, compared to 0.89 in the French general population.Citation27 The minimally important clinical difference for the EQ-5D-5L has been estimated to be in the range of 0.04–0.07.Citation28
In the severe migraine group, mean EQ-5D utility scores were significantly lower (worse QoL) in patients with chronic rather than episodic migraine and in the former group, the mean EQ-5D utility score was 0.70, close to the score in patients with severe asthma. Similarly, scores were lower in patients reporting a severe impact with the HIT-6. The difference in mean EQ-5D scores between chronic and episodic migraine was 0.07, the minimally important clinical difference on this measure.Citation28 Similarly, in the severe asthma group, mean scores were significantly lower in patients with uncontrolled asthma than in those with well- or partly controlled severe disease, the difference again being larger than the minimally important difference, consistent with other studies.Citation29 The relationships observed between headache frequency and impact or asthma control, on the one hand, and QoL on the other are consistent with those reported in other studies in these diseasesCitation29–Citation34 and provide further support for the internal validity of these PROMs for evaluating patients with severe migraine or severe asthma.
In the case of severe migraine, the mobility, self-care and usual activity items of the EQ-5D were less impacted than in severe asthma, whereas the converse was true for the pain/discomfort item. Using the HAD, which measures psychological distress, mean scores on the depression item were significantly higher in severe migraine than in severe asthma, and 23% of subjects with severe migraine had scores consistent with clinically relevant depression compared to 7% of the subjects with severe asthma. In contrast, scores on the anxiety dimension of the HAD were similar in the two groups.
With regard to work performance measured with the WPAI, absenteeism over the past week was relatively low in both severe migraine (9.0%) and severe asthma (13.8%). In contrast, presenteeism, work productivity loss and impact impairment all affected around one-half of potential work/activity time in severe migraine and around one-third of this time in severe asthma. This impact was consistently higher in chronic than in episodic migraine. It should be noted that the definition of severe migraine required patients to experience on average eight headaches a week (fifteen headaches a week for chronic migraine) and that the diagnostic criteria for migraine specify that migraine headaches may last from 4 to 72 hrs and are aggravated by or cause avoidance of routine physical activity.Citation35 For this reason, it is to be expected that the amount of time when activities are impaired by migraine headaches will be high.
The PROM scores observed in this study are generally consistent with those observed in previous studies of asthmaCitation16,Citation29,Citation36 and migraineCitation32,Citation37,Citation38 in France. However, since the present sample consists of patients with severe disease only, absolute EQ-5D scores were lower, and WPAI and HID scores higher, than in studies evaluating patients with asthma or migraine of undifferentiated severity.
It is important to note that the differences observed in PROM scores between severe migraine and severe asthma are subject to a risk of confounding due to other variables that may be distributed differently between the two patient groups and which may influence the quality of life or other constructs evaluated. Possible such confounding factors include age, gender and disease severity. Mean age was close between the two disease groups. The proportion of female patients was, as expected, higher in the severe migraine group than in the severe asthma group. However, women tend to rate their quality of life lower than do men,Citation27 and confounding by gender would thus tend to bias the findings towards worse quality of life in severe migraine, the reverse of what was actually found. The presence of other confounding factors cannot be excluded.
The strengths of this study include the relatively large number of patients included, the range of PROMS used and the limited amount of missing data. In addition, patients were enrolled by specialists experienced in migraine or asthma, who confirmed the diagnosis and ascertained disease severity. The principal limitation was that the samples of severe migraine and severe asthma patients were not matched and that, for this reason, potential confounding factors cannot be excluded. In addition, no control group was included and absolute disutilities associated with severe migraine and severe asthma cannot be determined.
With regard to severity, the definition of severe asthma was based on the GINA definition whereas that used for severe migraine was an ad hoc one and thus somewhat arbitrary. It is thus possible that other definitions of severe migraine would have yielded different findings, and this would be of interest to explore in future studies, notably to evaluate whether the impact of migraine is primarily driven by headache intensity or headache frequency, or both. In this respect, it has recently been proposed that the definition of chronic migraine be broadened from ≥15 headache days with at least eight MMD to only ≥8 MMD.Citation39 The motivations for this proposal were first that patients with ≥15 headache days per month and those with ≥8 but <15 headache days are essentially the same and secondly that the burden of disease is high in both groups. These were the two severe migraine groups evaluated in the present study. Our findings study partially support the proposal as no differences between the two groups were found in terms of demographic characteristics, symptom presentation, sick leave or physician consultations. On the other hand, EQ-5D quality of life scores, WPAI work impairment scores and HAD psychological distress scores all indicated more impact of migraine in the patients with ≥15 MMD compared to those with ≥18 but <15 MMD. It would be interesting to evaluate whether disease impact, measured with such scales, varies linearly with headache frequency or whether there is a clear inflection point which could be used to define chronic or severe migraine.
In conclusion, quality of life, work activity and psychological distress are all deteriorated both in severe migraine, notably in chronic disease, and in severe asthma, but different aspects are affected in the two diseases. The different PROMs used in this study provide consistent information on the impact of these diseases on the patient.
Data Sharing Statement
The data are hosted by a third party (Kantar Health). Access to the data will require special permission. Reasonable requests can be made to the corresponding author, who will transfer the request to the database manager.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Dr Christian Lucas reports personal fees from Novartis, during the conduct of the study; personal fees from Lilly, personal fees from Amgen, personal fees from Ethypharm, grants and personal fees from Sanofi, personal fees from Teva, personal fees from Grunenthal, personal fees from Biogen, and personal fees from Boston Scientific, outside the submitted work. Prof. Dr. Gilles Garcia reports personal fees from Novartis, during the conduct of the study; personal fees from GSK, AstraZeneca, Roche, Sanofi, and MSD, outside the submitted work. Mrs Samia Aly is an employee of Novartis. Mrs Chantal Touboul, Mrs Rahma Sellami and Mr Xavier Guillaume are employees of Kantar Health. Mrs Chantal Touboul and Mr Xavier Guillaume report personal fees from Novartis, during the conduct of the study. The authors report no other conflicts of interest in this work.
Additional information
Funding
References
- Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. doi:10.1097/00005650-199206000-00002
- Ware JE, Kosinski M, Keller SD. 12-item short-form health survey. Construction of scales and preliminary tests of reliability and validity. Med Care. 1995;34:220–233. doi:10.1097/00005650-199603000-00003
- Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: development and final revision of a health status measure. Med Care. 1981;19(8):787–805. doi:10.1097/00005650-198108000-00001
- Hunt SM, McEwen J, McKenna SP. Measuring health status: a new tool for clinicians and epidemiologists. J R Coll Gen Pract. 1985;35(273):185–188.
- Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–1736. doi:10.1007/s11136-011-9903-x
- Haywood KL, Mars TS, Potter R, Patel S, Matharu M, Underwood M. Assessing the impact of headaches and the outcomes of treatment: a systematic review of patient-reported outcome measures (PROMs). Cephalalgia. 2018;38(7):1374–1386. doi:10.1177/0333102417731348
- Worth A, Hammersley V, Knibb R, et al. Patient-reported outcome measures for asthma: a systematic review. NPJ Prim Care Respir Med. 2014;24:14020. doi:10.1038/npjpcrm.2014.20
- Martin BC, Pathak DS, Sharfman MI, et al. Validity and reliability of the migraine-specific quality of life questionnaire (MSQ Version 2.1). Headache. 2000;40(3):204–215. doi:10.1046/j.1526-4610.2000.00030.x
- Kosinski M, Bayliss MS, Bjorner JB, et al. A six-item short-form survey for measuring headache impact: the HIT-6. Qual Life Res. 2003;12(8):963–974. doi:10.1023/A:1026119331193
- Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax. 1992;47(2):76–83. doi:10.1136/thx.47.2.76
- Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113(1):59–65. doi:10.1016/j.jaci.2003.09.008
- Lyons RA, Lo SV, Littlepage BN. Comparative health status of patients with 11 common illnesses in Wales. J Epidemiol Community Health. 1994;48(4):388–390. doi:10.1136/jech.48.4.388
- Riazi A, Hobart JC, Lamping DL, et al. Using the SF-36 measure to compare the health impact of multiple sclerosis and Parkinson’s disease with normal population health profiles. J Neurol Neurosurg Psychiatry. 2003;74(6):710–714. doi:10.1136/jnnp.74.6.710
- Stavem K, Lossius MI, Kvien TK, Guldvog B. The health-related quality of life of patients with epilepsy compared with angina pectoris, rheumatoid arthritis, asthma and chronic obstructive pulmonary disease. Qual Life Res. 2000;9(7):865–871. doi:10.1023/A:1008993821253
- Balieva F, Kupfer J, Lien L, et al. The burden of common skin diseases assessed with the EQ5D: a European multicentre study in 13 countries. Br J Dermatol. 2017;176(5):1170–1178. doi:10.1111/bjd.15280
- Demoly P, Annunziata K, Gubba E, Adamek L. Repeated cross-sectional survey of patient-reported asthma control in Europe in the past 5 years. Eur Respir Rev. 2012;21(123):66–74. doi:10.1183/09059180.00008111
- Tso AR, Goadsby PJ. Anti-CGRP monoclonal antibodies: the next era of migraine prevention? Curr Treat Options Neurol. 2017;19(8):27. doi:10.1007/s11940-017-0463-4
- Global Initiative for Asthma. Asthma Management and Prevention. Bethesda (USA): National Institutes of Health; 1995.
- Global Initiative for Asthma. Global strategy for asthma management and prevention. 2006. Available from: http://www.ginashtma.org. Accessed December 17, 2020.
- Chung KF, Wenzel SE, Brozek JL, et al. International ERS/ATS guidelines on definition, evaluation and treatment of severe asthma. Eur Respir J. 2014;43(2):343–373. doi:10.1183/09031936.00202013
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2017. Available from: http://www.ginasthma. Accessed December 17, 2020.
- Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics. 1993;4(5):353–365. doi:10.2165/00019053-199304050-00006
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi:10.1111/acp.1983.67.issue-6
- van Hout B, Janssen MF, Feng YS, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15(5):708–715. doi:10.1016/j.jval.2012.02.008
- Snaith RP. The hospital anxiety and depression scale. Health Qual Life Outcomes. 2003;1:29. doi:10.1186/1477-7525-1-29
- Henry P, Auray JP, Gaudin AF, et al. Prevalence and clinical characteristics of migraine in France. Neurology. 2002;59(2):232–237. doi:10.1212/WNL.59.2.232
- Szende A, Janssen B, Cabasés J. Self-Reported Population Health: An International Perspective Based on EQ-5D. Berlin: Springer Open; 2018.
- McClure NS, Sayah FA, Xie F, Luo N, Johnson JA. Instrument-defined estimates of the minimally important difference for EQ-5D-5L index scores. Value Health. 2017;20(4):644–650. doi:10.1016/j.jval.2016.11.015
- Hernandez G, Garin O, Dima AL, et al. EuroQol (EQ-5D-5L) validity in assessing the quality of life in adults with asthma: cross-sectional study. J Med Internet Res. 2019;21(1):e10178. doi:10.2196/10178
- Guilbert TW, Garris C, Jhingran P, et al. Asthma that is not well-controlled is associated with increased healthcare utilization and decreased quality of life. J Asthma. 2011;48(2):126–132. doi:10.3109/02770903.2010.535879
- Mungan D, Aydin O, Mahboub B, et al. Burden of disease associated with asthma among the adult general population of five Middle Eastern countries: results of the SNAPSHOT program. Respir Med. 2018;139:55–64. doi:10.1016/j.rmed.2018.03.030
- Vo P, Fang J, Bilitou A, Laflamme AK, Gupta S. Patients’ perspective on the burden of migraine in Europe: a cross-sectional analysis of survey data in France, Germany, Italy, Spain, and the United Kingdom. J Headache Pain. 2018;19(1):82. doi:10.1186/s10194-018-0907-6
- Doz M, Chouaid C, Com-Ruelle L, et al. The association between asthma control, health care costs, and quality of life in France and Spain. BMC Pulm Med. 2013;13:15. doi:10.1186/1471-2466-13-15
- Blumenfeld AM, Varon SF, Wilcox TK, et al. Disability, HRQoL and resource use among chronic and episodic migraineurs: results from the International Burden of Migraine Study (IBMS). Cephalalgia. 2011;31(3):301–315. doi:10.1177/0333102410381145
- Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808. doi:10.1177/0333102413485658
- Hennegrave F, Le Rouzic O, Fry S, Behal H, Chenivesse C, Wallaert B. Factors associated with daily life physical activity in patients with asthma. Health Sci Reports. 2018;1(10):e84. doi:10.1002/hsr2.v1.10
- Lucas C, Lanteri-Minet M, Massiou H, et al. The GRIM2005 study of migraine consultation in France II. Psychological factors associated with treatment response to acute headache therapy and satisfaction in migraine. Cephalalgia. 2007;27(12):1398–1407. doi:10.1111/j.1468-2982.2007.01446.x
- Lucas C, Geraud G, Valade D, Chautard MH, Lanteri-Minet M. Recognition and therapeutic management of migraine in 2004, in France: results of FRAMIG 3, a French nationwide population-based survey. Headache. 2006;46(5):715–725. doi:10.1111/j.1526-4610.2006.00430.x
- Chalmer MA, Hansen TF, Lebedeva ER, Dodick DW, Lipton RB, Olesen J. Proposed new diagnostic criteria for chronic migraine. Cephalalgia. 2019;333102419877171.