Abstract
Psoriatic arthritis (PsA) is an inflammatory arthritis associated with psoriasis (PsO). The treatment of PsA can be challenging and includes non-steroidal anti-inflammatory drugs, synthetic disease modifying antirheumatic drugs, and biologicals. One novel oral compound that has been recently established for the treatment of PsO and PsA is apremilast, a small molecule PDE4 inhibitor. The inhibition of PDE4 results in increased intracellular cAMP levels and modulates the expression of inflammatory mediators critically involved in PsO and PsA pathogenesis like TNF, IL-12, IL-17, and IL-23. Apremilast received US Food and Drug Administration approval for the treatment of PsO and PsA in 2014 and received approval from the European Medicines Agency in early 2015. This article summarizes the pharmacology of apremilast, its efficacy and safety in clinical studies, and its potential position in modern PsO/PsA management.
Introduction
Psoriasis (PsO) is a chronic inflammatory disease of the skin and joints occurring in 3% of the populationCitation1,Citation2 and approximately 20% – 30% of patients diagnosed with PsO develop psoriatic arthritis (PsA).Citation3,Citation4 PsO is currently considered an autoimmune inflammatory disease, mainly caused by the interplay between the innate and the adaptive immune system. Predominant cells of the psoriatic inflammation are T-cells, antigen presenting cells like dendritic cells and neutrophilic granulocytes. Their mediators are responsible for the proliferative response by keratinocytes and vascular endothelial cells.Citation5,Citation6 There is increasing evidence that besides Th1 cells, Th17 cells, a subset of CD4+ T-cells that preferentially produce IL-17, are the key players in PsO pathogenesis.Citation7 IL-23 is an important cytokine that promotes the generation of pathogenic Th17 cell differentiation.Citation8 Upon activation, Th1 and Th17 cells produce inflammatory cytokines like IL-2, IFN-γ (Th1-cells), IL-17A, IL-17F, IL-21, IL-22 (Th17-cells), and TNF (Th1- and Th17- cells).Citation9–Citation11 Similar to PsO pathogenesis, Th17 cells have been found to play an important role in joint inflammation in PsA.Citation12
PsA is a separate clinical entity from rheumatoid arthritis. It is usually seronegative for rheumatoid factor, has a frequent involvement of distal joints, and has an asymmetric tendency. Moreover, PsA has a common spinal involvement and often goes along with enthesitis and dactylitis.Citation13 Patients affected with PsA show a reduced quality of life and demonstrate a reduced physical function, as measured in lower scores of the Medical Outcome Survey Short Form 36 (SF-36) and higher scores of the Health Assessment Questionnaire (HAQ).Citation14,Citation15
For the management of PsA patients it is important to adjust treatment according to the prevailing clinical pattern and to pay attention to both skin and joint manifestations. There are patients presenting with predominant skin involvement and mild arthritis, who are successfully treated for PsA with non-steroidal anti-inflammatory drug (NSAID) treatment. Yet, a substantial percentage of patients with PsA (20%) develop a severe, mutilating, and debilitating form of arthritis.Citation16,Citation17
Treatment of PsA has fundamentally changed over the last years through development of new synthetic and biological agents. Depending on PsA activity and severity, type of joint involvement and extra-articular manifestations, therapy usually starts with NSAIDs. When PsA shows high activity or when NSAIDs are inefficient, therapy is escalated to synthetic disease modifying antirheumatic drugs (DMARDs) with methotrexate being the most common agent. Second line therapy is used when DMARDs show lack of efficacy or show toxicities. The second line DMARDs are currently represented by biologicals with TNF antagonists being the most popular biological DMARD.Citation9,Citation18 The introduction of TNF-neutralizing fusion proteins and antibodies was a breakthrough in the treatment of PsA and PsO.
Despite the vast advancement in PsA therapy over the past 15 years, there is still need for further improvement. Biological DMARDs have to be administered intravenously or subcutaneously and are very cost intensive for patients and the health system. Moreover, immunosuppressive biologicals show increased risks for infections and certain malignancies. Therefore, recent developments focus on oral DMARDs, which selectively silence inflammatory immune responses with acceptable safety profiles.Citation9,Citation19 One of these novel chemical compounds is apremilast, which has been recently approved by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) as second line treatment for PsA and PsO.
Apremilast – mode of action
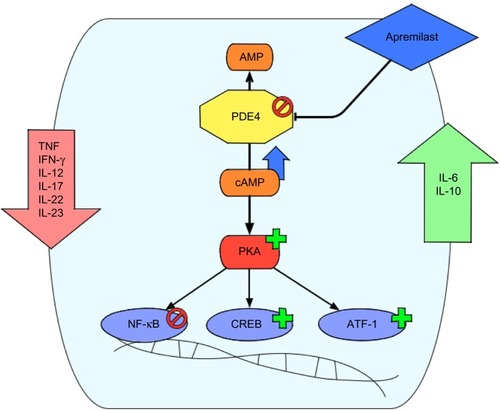
Apremilast – (S)-N-{2-[1-(3-ethoxy-4-methoxyphenyl)-2-(methylsulfonyl)ethyl-1,3-dioxo-2,3-dihydro-1H-isoindol-4-yl}acetamide – is an orally available small molecule inhibitor of PDE4.Citation20 Inhibition of PDE4 leads to reduced production of pro-inflammatory mediators like TNF, IFN-γ, IL-12/23p40, IL-23p19, IL-17A, and IL-22. On the other hand, apremilast has been reported to increase the production of IL-6 and IL-10.Citation20 This is of interest, since IL-10 is a cytokine with potent anti-inflammatory properties, while IL-6 is a cytokine with pro- and anti-inflammatory features.Citation21,Citation22
Mechanistically, PDEs degrade intracellular cAMP levels by enzymatic hydrolysis. The cyclic nucleotide cAMP is an important intracellular secondary messenger. Extracellular inflammatory signals like chemokines, leukotrienes, and PGs bind to GPCRs, leading to activation of AC, which increases the production of cAMP.Citation23 The secondary messenger cAMP then interacts with and activates effector proteins like PKA. On the one hand this kinase results in phosphorylation and activation of transcription factors like CREB and ATF-1. On the other hand PKA activation leads to inhibition of other transcription factors like NF-κB.Citation24,Citation25 In this way cAMP is involved in immune homeostasis by increasing inflammatory signals when cAMP levels are low and by reducing inflammatory signaling when cAMP levels are high ().
Figure 1 Mode of action of apremilast.
There are eleven individual families of PDEs described in mammalian species (PDE1–PDE11) with different selectivity to cAMP/cGMP hydrolyzation and distinct predominant cellular localization.Citation26 PDE4 is specific for cAMP hydrolyzation and is the major PDE isoenzyme found in immune cells like monocytes, T-cells, and neutrophils.Citation27 Apremilast is a selective inhibitor of PDE4, with significant inhibition observed only for the PDE4 isoenzymes encoded by four genes (PDE4A, PDE4B, PDE4C, and PDE4D). In a recent study, apremilast (10 μM) showed an average of approximately 95% inhibition of the PDE4 enzymes in vitro. There was no significant inhibition measured on other members of the PDE family.Citation28 Originally, apremilast was developed as a thalidomide analog as both drugs have the phthalimide ring in common.Citation29 Despite this relatedness, apremilast shows no binding to CRBN, the primary molecular target of thalidomide teratogenicity, as this binding is mediated through the glutarimide ring of thalidomide and apremilast does not contain a glutarimide ring.Citation28,Citation30
Apremilast treatment has been reported to elevate intracellular cAMP levels in human peripheral blood mononuclear cells (PBMCs) in response to PGE2.Citation28 In vitro, treatment of PBMCs with apremilast inhibits LPS-induced TNF production and reduces CpG ODN-stimulated IFN-α production.Citation28 Further, the production of cytokines like IL-2, IL-5, IL-10, IL-13, Il-17, TNF, GM-CSF, and IFN-γ by anti-CD3-stimulated T-cells was inhibited by apremilast.Citation28 In contrast, the presence of apremilast significantly enhanced IL-10 and IL-6 production from LPS-stimulated PBMCs.Citation20 The different regulation of IL-10 in T-cells compared to PBMCs by apremilast could be explained by the presence of antigen presenting cells when studying cytokine production in PBMCs. In an antigen-specific transgenic T- and B-cell clonal expansion mouse model, apremilast had no effect on the clonal expansion of T- or B-cells and had no effect on antibody responses.Citation28
PDE4 inhibition has also been tested in preclinical models of PsO and PsA. In vivo studies using a PsO mouse model showed significant reduced epidermal thickness, reduced proliferation index, and recovery of psoriasiform histological features upon apremilast treatment.Citation20 In a murine model of arthritis apremilast treatment blocked synovial inflammation, cartilage damage, and bone erosion.Citation31
Efficacy of apremilast
Clinical efficacy of apremilast in PsA was studied in four randomized, placebo-controlled trials with open-label extension periods.Citation32 This extensive Phase III clinical trial program is called the Psoriatic Arthritis Longterm Assessment of Clinical Efficacy (PALACE).Citation32 For clinical efficacy assessment of apremilast in plaque-type PsO two randomized, placebo-controlled Phase III clinical studies with open-label extensions have been performed, ESTEEM 1 and ESTEEM 2.Citation33
Recently, the first results of a Phase III clinical trial comparing apremilast to placebo and etanercept called the LIBERATE trial were presented at the 73rd Annual Meeting of the American Academy of Dermatology.Citation34
Efficacy of apremilast in PsA
Efficacy data of apremilast in PsA are available from the PALACE 1, PALACE 2, and PALACE 3 studies. Those trials had a similar design and enrolled patients with active PsA defined by ≥3 swollen joints and ≥3 tender joints despite prior or current treatment with DMARDs (small-molecule and/or biologic). Different to PALACE 1 and PALACE 2, the PALACE 3 trial studied the efficacy of apremilast in patients with active PsA who had at least one psoriatic lesion with a body surface area (BSA) ≥3%.Citation32,Citation35,Citation36 Overall there have been 1,493 patients randomized and treated either with placebo or apremilast 20 mg twice daily (BID) or 30 mg BID.Citation33 Apremilast was either given as a monotherapy (34.8%) or in combination with stable doses of non-biological DMARDs (65.2%). Methotrexate (≤25 mg per week) was the most common co-medication of patients (54.5%).Citation33 Primary efficacy endpoint was the proportion of patients meeting 20% improvement in modified American College of Rheumatology response criteria (ACR20) at week 16. Additional efficacy outcome measures included symptoms of PsA, physical function, enthesitis, dactylitis, and PsO.Citation32 At week 16, significantly more patients receiving apremilast 20 mg BID (30.4%) or 30 mg BID (38.1%) achieved an ACR20 response compared to placebo treatment (19.0%) in the PALACE 1 trial.Citation32 The pooled data of PALACE 1–3 trials after 16 weeks of treatment with apremilast 30 mg BID showed a significantly higher ACR20 response (37.0%) compared to placebo (18.8%).Citation33 Patients with baseline enthesitis had a significantly higher change from the Maastricht Ankylosing Spondylitis Enthesitis Score when treated with apremilast 30 mg BID versus placebo. In patients with dactylitis, the mean change from baseline in dactylitis severity score was higher with apremilast versus placebo but did not reach statistical significance at week 24.Citation32 After 24 weeks of treatment, the placebo-controlled phase ended and the remaining placebo patients were re-randomized to either apremilast 20 mg BID or apremilast 30 mg BID.Citation32 The ACR20 response could be sustained among the patients who continued receiving treatment with apremilast through week 52. At week 52, 63.0% of patients who received apremilast 20 mg BID and 54.6% who received 30 mg BID achieved an ACR20 response ().Citation37
Table 1 Efficacy of apremilast treatment
Efficacy of apremilast in PsO
Data on the efficacy of apremilast on PsO were collected in trials for PsA and in PsO trials. The PALACE studies showed a reduction of the baseline Psoriasis Area and Severity Index (PASI) in patients with PsO affecting ≥3% of the BSA by at least 50% (PASI-50) in a significantly higher proportion of patients receiving apremilast 20 mg BID (33.8%) or apremilast 30 mg BID (50.6%) compared to placebo (18.5%) after 24 weeks.Citation32 In the ESTEEM 1 and ESTEEM 2 trials, 1,257 patients with moderate to severe plaque PsO defined by a PASI score ≥12, a BSA ≥10%, and a static physician global assessment (sPGA) ≥3, who were candidates for systemic or phototherapy were included.Citation33 Patients were treated with either apremilast 30 mg BID or placebo (2:1) for 16 weeks, from week 16 to week 32 every patient received apremilast 30 mg BID followed by a randomized reset phase from week 32 to week 52, depending on primary PASI response. The primary efficacy endpoint was a PASI-75 response after 16 weeks, the secondary efficacy endpoint was the proportion of patients reaching an sPGA of 0 (clear) or 1 (almost clear) after 16 weeks.
Patients included in this trial had a mean PASI score of 19.07, 70% had an sPGA score of 3 (moderate) and 29.8% had an sPGA score of 4 (severe). Eighteen percent of patients in the ESTEEM 1 and ESTEEM 2 trial also suffered from PsA.Citation33 After 16 weeks of treatment with apremilast 30 mg BID, 33.1% of patients in the ESTEEM 1 trial had a PASI-score improvement of 75% compared to baseline (5.3% with placebo treatment). In the ESTEEM 2 trial, 28.8% of patients reached a PASI-75 response after 16 weeks compared to 5.8% following placebo treatment. An sPGA score of clear or almost clear was reached by 21.7% of patients in the ESTEEM 1 trial (3.9% with placebo) and by 20.4% of patients in the ESTEEM 2 trial (4.4% with placebo). Seventy-nine out of 835 patients (9.5%) treated with apremilast 30 mg BID in both trials had a 90% improvement in PASI score (PASI-90) after 16 weeks ().Citation33
Beside PASI and sPGA response, patients treated with apremilast in the ESTEEM 1 and ESTEEM 2 trial had an improvement in nail PsO, scalp PsO, and pruritus.Citation33
In the LIBERATE (EvaLuatIon from a PlaceBo-controllEd Study of ORal ApremilasT and Etanercept in Plaque Psoriasis) Phase IIIb clinical trial to measure the efficacy and safety of apremilast, etanercept, and placebo in patients with moderate to severe plaque PsO, 250 subjects who had no prior exposure to biological agents were randomized 1:1:1 to receive either apremilast 30 mg BID, etanercept 50 mg subcutaneously once weekly or placebo for 16 weeks. After week 16 all patients received apremilast 30 mg BID through week 104.Citation34 The primary endpoint was to evaluate efficacy and safety of apremilast 30 mg BID compared to placebo at week 16. The study was not designed to directly compare apremilast to etanercept treatment.Citation34
After 16 weeks, 33 out of 83 (40%) patients receiving apremilast 30 mg BID showed a PASI-75 response, compared to ten out of 84 (12%) patients receiving placebo treatment and 40 out of 84 (48%) patients receiving etanercept 50 mg subcutaneously once weekly.Citation34
Safety and tolerability of PDE4 inhibition
In a pooled analysis, 1,493 patients receiving either placebo (n=495), apremilast 20 mg BID (n=501) or apremilast 30 mg BID (n=497) in the PALACE 1, 2, and 3 clinical trials were included in a safety population to assess safety and tolerability of apremilast treatment.Citation38 After 24 weeks, all patients receiving placebo were re-randomized to either 20 mg BID or 30 mg BID apremilast. The apremilast exposure in this pooled analysis included 720 patients exposed to apremilast 20 mg BID (766.4 patient years) and 721 patients exposed to apremilast 30 mg BID (769.0 patient years).Citation38 The most common adverse events (AEs) in these studies were diarrhea (14.3%), nausea (12.6%), urinary tract infections (10.3%), headache (10.1%), and nasopharyngitis (7.4%) ().Citation33 In the PALACE 1 clinical trial, most AEs occurred during the first 24 weeks of treatment, with most AEs (over 90%) being mild to moderate in severity and discontinuation rates because of AEs were under 10%.Citation37 Diarrhea and nausea occurred most often during the first 2 weeks of treatment and usually resolved within 4 weeks despite continued treatment and without medical intervention.Citation37 From week 0 to 52, 6.1% of patients in both treatment arms (apremilast 20 mg BID and apremilast 30 mg BID) reported severe AEs (SAEs) while 3.6% of patients treated with placebo reported an SAE from week 0 to 24. With the exception of myocardial infarction, which was reported in two patients receiving apremilast 20 mg BID, no individual SAE was reported more than once per treatment group.Citation37
Table 2 Safety and tolerability of apremilast treatment – most common adverse events
During the 52-week period there were no cases of lymphoma, de novo tuberculosis or tuberculosis reactivations reported, while there has been one squamous cell carcinoma of the skin identified in this period.Citation37 One death occurred in the placebo-controlled phase in a 52-year old woman receiving apremilast 20 mg BID and methotrexate due to multi-organ failure secondary to pre-existing vitamin B12 deficiency and was not considered to be study drug related by the investigator.Citation37
There were no clinically meaningful effects on laboratory measurements detected during the first 52 weeks of the trial with no marked abnormalities in leukocytes, neutrophils, or platelets and only in one or two patients have there been marked increases in ALT (n=2) or creatinine (n=1), or marked decreases in hemoglobin (n=2).Citation37,Citation38
Preclinical trials showed that PDE4B deficient mice were leaner, had lower fat pad weights, smaller adipocytes, and decreased serum leptin levels compared to wild type mice.Citation39 In the PALACE 1 trial, weight decrease was reported as an AE in 1.6% of patients receiving apremilast 20 mg BID and 2.0% of patients receiving apremilast 30 mg BID during the apremilast exposure period.Citation40 Weight loss, that was not considered an AE, was observed in a larger proportion of patients, as after 52 weeks weight loss greater than 5% was observed in 15.8% of patients receiving apremilast 20 mg BID and in 17.2% of patients receiving apremilast 30 mg BID. Patients treated with apremilast 30 mg BID had a mean weight loss of –1.79 kg after 52 weeks (0.91 kg with apremilast 20 mg BID treatment).Citation37 There was no association between weight loss and gastrointestinal AEs such as diarrhea or nausea and vomiting.Citation40
Besides anti-inflammatory effects, PDE4 inhibitors are known to mediate behavioral changes in the animal model.Citation28 In the conscious ferret model, mild behavioral changes like flattened posture, lip licking, and backward walking were observed at doses under 10 mg/kg apremilast. Higher doses led to marked emesis along with pronounced behavioral changes in these animals.Citation28 During the placebo-controlled phase of the clinical trials, 1.2% (14/1,184) of patients treated with apremilast compared to 0.5% (2/418) of patients treated with placebo reported depressive mood or depression. None of these depressions was classified as severe or led to discontinuation of the study.Citation33
Patient focused perspectives
PsO and PsA go along with severe disease-related limitations in quality of life. PsO patients indicated itching, scales, and flaking as most bothersome, while joint pain was reported by 89% of patients with PsA.Citation41 Patients with more than four affected joints answered “much difficulty” or “unable to do” for many daily life tasks like bending down to pick up clothing from the floor (26%), walking outdoors on flat ground (18%), dressing themselves (15%), getting in and out of bed or the car (15%), washing and drying their body (12%), turning faucets on and off (8%), and lifting a full cup or glass to their mouth (7%).Citation41
In the PALACE 1 clinical trial, at week 16, apremilast treatment was associated with significantly greater reductions (improvements) in the HAQ-Disability Index (HAQ-DI) compared with placebo.Citation32 The HAQ-DI scores were maintained over 52 weeks with mean reductions in HAQ-DI score of −0.37 with apremilast 20 mg BID and −0.32 with apremilast 30 mg BID.Citation37 A significant improvement was also measured in physical functions by the 36-Item Short-Form Health Survey v2 Physical Function domain, in health-related quality of life (SF-36v physical component summary and Functional Assessment of Chronic Illness Therapy-Fatigue) and in patient assessment of pain.Citation33,Citation37
With pruritus being one of the major problems of PsO, apremilast treatment led to a reduction of −31.5 points (ESTEEM 1) and −33.5 points (ESTEEM 2) in the visual analog scale after 16 weeks compared to an improvement of −7.3 points (ESTEEM 1) and −12.2 points (ESTEEM 2) in the visual analog scale when treated with placebo.Citation33
In the Dermatology Life Quality Index score where 0 is the best and 30 is the worst value of daily life quality, apremilast treatment of 30 mg BID showed a mean improvement of −6.6 points (ESTEEM 1) and −6.7 points (ESTEEM 2) compared to −2.1 points (ESTEEM 1) and −2.8 points (ESTEEM 2) upon placebo treatment. These improvements could be maintained until week 52.Citation33
There were also statistically significant improvements seen in the 36-Item Short-Form Health Survey v2 mental component score and in “Work Limitations Questionnaire (WLQ-25) Index” upon apremilast treatment compared to placebo.Citation33
Apremilast’s position in PsO therapy
Apremilast is an orally available PDE4 inhibitor with good efficacy in PsA and PsO. The safety profile of apremilast within a treatment period of 52 weeks seems to be favorable with no increased rates of laboratory abnormalities, severe infections or malignancies. Rare AEs reported in some of the patients are weight loss and depression.Citation33 These side effects seem to be compound-specific. Weight loss should be closely monitored in patients treated with apremilast, underweight patients should only be treated with caution. However, weight loss may be a beneficial side effect in selected patients with adiposity, which is a strong risk factor for incident PsO and obesity-related disorders like diabetes mellitus type 2, hyperlipidemia, hypertension, and ischemic heart disease.Citation42 However, for a concluding statement on apremilast safety profile additional data from long-term extension phases of clinical trials, Phase IV studies, and registry data are needed. The manufacturer does not recommend performing pre-examinations for tuberculosis, or laboratory monitoring during therapy with apremilast.Citation33 However, it is up to the dermatologist and the rheumatologist to evaluate the need for laboratory testing. Current therapy guidelines recommend PsA treatment with NSAIDs, followed by methotrexate treatment or other orally available DMARDs like leflunomide or sulfasalazine when clinical progression is observed. If these DMARDs are contraindicated, show toxicity or lack of efficacy, second line therapy with biological agents like etanercept or other TNF-blocking drugs, with or without DMARD co-medication is indicated.Citation18 In patients with PsA, apremilast could find its place early in the treatment ladder due to its favorable safety profile and its clinical response to signs and symptoms of PsA.
Compared to biological agents, apremilast seems not to increase the risk of infections and malignancies and has the advantage of an oral route of application, but head to head studies are helpful to evaluate its clinical efficacy in PsA. Moreover, efficacy and safety trials of combination therapies of apremilast and biological DMARDs are needed, since this approach may be of benefit in difficult to treat patients or in patients with AEs or contraindications to methotrexate.
With approximately one out of three patients reaching a PASI-75 response and one out of ten (9.5%) reaching a PASI-90 response after 16 weeks of treatment, apremilast will probably stay a second line drug for PsA patients with major skin involvement. With newly introduced biological agents like secukinumab, an IL-17A antibody, approximately 70%–75% of patients achieve a PASI-90 response after 16 weeks of treatment.Citation43 Other second generation biologicals targeting the Th17 axis like antibodies neutralizing IL-23p19 are under clinical investigation.
Taken together, apremilast is a modern anti-psoriatic oral compound with a favorable safety profile, which primarily will be used in patients with PsO and PsA who do not respond adequately to methotrexate or other oral anti-psoriatics.
Disclosure
Stephan Forchhammer has been an investigator for Almirall, Biogen Idec, Celgene, Delenex Therapeutics, Eli Lilly and Company, Galderma SA, Janssen-Cilag, MSD Sharp and Dohme, Novartis Pharmaceuticals, and Pfizer. Kamran Ghoreschi has been a consultant, lecturer or investigator for Abbvie, Almirall, Biogen Idec, Celgene, Delenex Therapeutics, Eli Lilly and Company, Galderma SA, Janssen-Cilag, MSD Sharp and Dohme, Novartis Pharmaceuticals, Pfizer, and the Schering-Plough Research Institute and received research grants from Fumapharm AG (now Biogen Idec) and Pfizer.
References
- KurdSKGelfandJMThe prevalence of previously diagnosed and undiagnosed psoriasis in US adults: results from NHANES 2003–2004J Am Acad Dermatol200960221822419022533
- ParisiRSymmonsDPGriffithsCEAshcroftDMIdentification and Management of Psoriasis and Associated ComorbidiTy (IMPACT) project teamGlobal epidemiology of psoriasis: a systematic review of incidence and prevalenceJ Invest Dermatol2013133237738523014338
- GladmanDDPsoriatic arthritis from Wright’s era until todayJ Rheumatol Suppl2009834819661526
- ReichKKrügerKMössnerRAugustinMEpidemiology and clinical pattern of psoriatic arthritis in Germany: a prospective interdisciplinary epidemiological study of 1511 patients with plaque-type psoriasisBr J Dermatol200916051040104719210498
- BoehnckeWHSchönMPPsoriasisLancet Epub2015526
- GhoreschiKWeigertCRöckenMImmunopathogenesis and role of T cells in psoriasisClin Dermatol200725657458018021895
- GhoreschiKLaurenceAYangXHiraharaKO’SheaJJT helper 17 cell heterogeneity and pathogenicity in autoimmune diseaseTrends Immunol201132939540121782512
- GhoreschiKLaurenceAYangXGeneration of pathogenic T(H)17 cells in the absence of TGF-b signallingNature2010467731896797120962846
- BelgeKBrückJGhoreschiKAdvances in treating psoriasisF1000Prime Rep20146424592316
- BaliwagJBarnesDHJohnstonACytokines in psoriasisCytokine201573234235025585875
- NestleFOKaplanDHBarkerJPsoriasisN Engl J Med2009361549650919641206
- LeipeJGrunkeMDechantCRole of Th17 cells in human autoimmune arthritisArthritis Rheum201062102876288520583102
- GladmanDDClinical aspects of the spondyloarthropathiesAm J Med Sci199831642342389766484
- HustedJAGladmanDDFarewellVTCookRJHealth-related quality of life of patients with psoriatic arthritis: a comparison with patients with rheumatoid arthritisArthritis Rheum200145215115811324779
- HustedJATomBDFarewellVTSchentagCTGladmanDDA longitudinal study of the effect of disease activity and clinical damage on physical function over the course of psoriatic arthritis: Does the effect change over time?Arthritis Rheum200756384084917328058
- GladmanDDShuckettRRussellMLThorneJCSchachterRKPsoriatic arthritis (PSA) – an analysis of 220 patientsQ J Med1987622381271413659255
- HuynhDKavanaughAPsoriatic arthritis: current therapy and future approachesRheumatology (Oxford)2015541202825125588
- GossecLSmolenJSGaujoux-VialaCEuropean League Against Rheumatism recommendations for the management of psoriatic arthritis with pharmacological therapies. European League Against RheumatismAnn Rheum Dis201271141221953336
- GhoreschiKGadinaMJakpot! New small molecules in autoimmune and inflammatory diseasesExp Dermatol2014231711
- SchaferPHPartonAGandhiAKApremilast, a cAMP phosphodiesterase-4 inhibitor, demonstrates anti-inflammatory activity in vitro and in a model of psoriasisBr J Pharmacol2010159484285520050849
- de Waal MalefytRAbramsJBennettBFigdorCGde VriesJEInterleukin 10(IL-10) inhibits cytokine synthesis by human monocytes: an autoregulatory role of IL-10 produced by monocytesJ Exp Med19911745120912201940799
- TilgHTrehuEAtkinsMBDinarelloCAMierJWInterleukin-6 (IL-6) as an anti-inflammatory cytokine: induction of circulating IL-1 receptor antagonist and soluble tumor necrosis factor receptor p55Blood19948311131188274730
- SerezaniCHBallingerMNAronoffDMPeters-GoldenMCyclic AMP: master regulator of innate immune cell functionAm J Respir Cell Mol Biol200839212713218323530
- ZambonACZhangLMinovitskySGene expression patterns define key transcriptional events in cell-cycle regulation by cAMP and protein kinase AProc Natl Acad Sci U S A2005102248561856615939874
- OllivierVParryGCCobbRRde ProstDMackmanNElevated cyclic AMP inhibits NF-kappaB-mediated transcription in human monocytic cells and endothelial cellsJ Biol Chem19962713420828208358702838
- FrancisSHBlountMACorbinJDMammalian cyclic nucleotide phosphodiesterases: molecular mechanisms and physiological functionsPhysiol Rev201191265169021527734
- HouslayMDSchaferPZhangKYKeynote review: phosphodiesterase-4 as a therapeutic targetDrug Discov Today200510221503151916257373
- SchaferPHPartonACaponeLApremilast is a selective PDE4 inhibitor with regulatory effects on innate immunityCell Signal20142692016202924882690
- MolostvovGMorrisARosePBasuSMullerGThe effects of selective cytokine inhibitory drugs (CC-10004 and CC-1088) on VEGF and IL-6 expression and apoptosis in myeloma and endothelial cell co-culturesBr J Haematol2004124336637514717786
- ItoTAndoHSuzukiTIdentification of a primary target of thalidomide teratogenicityScience201032759711345135020223979
- McCannFEPalfreemanACAndrewsMApremilast, a novel PDE4 inhibitor, inhibits spontaneous production of tumour necrosis factor-alpha from human rheumatoid synovial cells and ameliorates experimental arthritisArthritis Res Ther2010123R10720525198
- KavanaughAMeasePJGomez-ReinoJJTreatment of psoriatic arthritis in a phase 3 randomised, placebo-controlled trial with apremilast, an oral phosphodiesterase 4 inhibitorAnn Rheum Dis20147361020102624595547
- Otezla® (apremilast) tablets for oral use [prescribing information]Summit, NJCelgene Corporation2014 Available from http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003746/WC500182627.pdfAccessed August 26, 2015
- Celgene.com [homepage on the Internet]Positive Results from Phase III Study Evaluating Oral OTEZLA® (Apremilast) or Injectable Etanercept versus Placebo in Patients with Moderate to Severe Plaque Psoriasis Presented at AADCelgene Corporation2015 [updated Mar 20, 2015; cited May 17, 2015]. Available from: http://ir.celgene.com/releasedetail.cfm?releaseid=902701Accessed May 17, 2015
- CutoloMMyersonGEFleischmannRMLong-Term (52-Week) Results Of a Phase 3, Randomized, Controlled Trial Of Apremilast, An Oral Phosphodiesterase 4 Inhibitor, In Patients With Psoriatic Arthritis (PALACE 2). [abstract]Arthritis Rheum201365Suppl 1081523280587
- EdwardsCJBlancoFJCrowleyJLong-term 52-week results of PALACE 3, a Phase III, randomized, controlled trial of apremilast, an oral phosphodiesterase 4 inhibitor, in patients with psoriatic arthritis and current skin involvement [abstract 212]Rheumatology201453Suppl 1i138
- KavanaughAMeasePJGomez-ReinoJJLongterm (52-week) results of a phase III randomized, controlled trial of apremilast in patients with psoriatic arthritisJ Rheumatol201542347948825593233
- MeasePJGladmanDDKavanaughALong-Term Safety and Tolerability Of Apremilast, An Oral Phosphodiesterase 4 Inhibitor, In Patients With Psoriatic Arthritis: Pooled Safety Analysis Of Three Phase 3, Randomized, Controlled Trials. [abstract]Arthritis Rheum201365Suppl 1031023203607
- ZhangRMaratos-FlierEFlierJSReduced adiposity and high-fat diet-induced adipose inflammation in mice deficient for phosphodiesterase 4BEndocrinology200915073076308219359377
- MeasePJGladmanDDKavanaughAChange in weight from baseline during the PALACE clinical trial program with apremilast, an oral phosphodiesterase 4 inhibitor: Pooled results from 3 phase 3, randomized, controlled trials. [abstract]Ann Rheum Dis201473Suppl 21055
- LebwohlMGBachelezHBarkerJPatient perspectives in the management of psoriasis: results from the population-based Multinational Assessment of Psoriasis and Psoriatic Arthritis SurveyJ Am Acad Dermatol201470587188124576585
- SettyARCurhanGChoiHKObesity, waist circumference, weight change, and the risk of psoriasis in women: Nurses’ Health Study IIArch Intern Med2007167151670167517698691
- RichardGLangleyMDBoniESecukinumab in Plaque Psoriasis–Results of Two Phase 3 TrialsN Engl J Med2014371432633825007392
