Abstract
Pneumococcal pneumonia is a serious disease with considerable morbidity and mortality in the elderly. Despite adequate antibiotic treatment, the long-term mortality of pneumococcal pneumonia remains high. Preventive measures in the form of vaccination, therefore, are warranted. Twenty-three-valent polysaccharide vaccines have a broad coverage but limited efficacy. Pneumococcal conjugate vaccines have been shown in children to be able to prevent invasive and mucosal pneumococcal diseases. It should be realized that the serotype composition of current pneumococcal conjugate vaccines is not tailored for the elderly, and that replacement disease can occur. Yet, the current 13-valent conjugate vaccine has been shown to protect against infections with vaccine serotypes. Long-term mortality of pneumococcal pneumonia should be included in policy making about the introduction of these vaccines for the elderly.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Pneumococcal disease
Streptococcus pneumoniae is an encapsulated Gram-positive, facultative anaerobic bacterium. It can cause mucosal infections such as otitis media, sinusitis, and non-bacteremic pneumonia, and also invasive diseases such as bacteremia, bacteremic pneumonia, and meningitis. In terms of frequency, otitis media is, by far, the most common pneumococcal infection, with every child having gone through 1 or (in many cases) more episodes.Citation1 The World Health Organization estimates that annually 476,000 (range 333,000–529,000) children under 5 years of age die due to pneumococcal infections, mainly pneumonia.Citation2 Global data on the incidence of invasive pneumococcal disease in the elderly suggest a similarly high burden.Citation3 Both the mucosal and the invasive forms of pneumococcal diseases therefore have received considerable attention in the medical literature. The New England Journal of Medicine has, since 1812, published 21,112 articles, which can be retrieved using “pneumonia” as the search term: 1734 with otitis media, 15,018 on meningitis, and 6710 on sepsis (accessed on September 25, 2017). The Lancet, since 1830, shows remarkable comparable numbers: pneumonia 22,867, otitis media 2,184, meningitis 10,543, and sepsis 9,642 (accessed on September 25, 2017). Clearly, pneumonia is represented most prominently in the medical literature as disease manifestation of infection with S. pneumoniae.
Young children, who have a high nasopharyngeal carriage rate, are most probably the reservoir from which S. pneumoniae spreads to the elderly population. Dochez and Avery have already speculated about the transmission of pneumococcal disease:
Although there are in the literature instances of the apparent contagiousness of lobar pneumonia, it has been commonly assumed that most cases of the disease represent probable infection with a pneumococcus dwelling during health on the buccal mucous membrane of normal human beings.
They thus suggest that most infections would result from bacteria, already carried in the nasopharyngeal area. Why a healthy carrier at a given point in time becomes infected could be due to “a sudden accession of virulence of the pneumococcus, or unusual depression of resistance of the individual”; the latter condition is now termed immunocompromised. Through either one or both of these mechanisms, “this organism, the pneumococcus, is supposed to be able to penetrate the lungs and set up disease”.Citation4
Etiology
In the past, community-acquired pneumonia (CAP) was considered in practice to be equivalent to pneumococcal pneumonia. Indeed, in the 1930s, before the introduction of antibiotics, in over 95% of cases, S. pneumoniae could be cultured from patients with CAP.Citation5 Nowadays, despite greatly improved diagnostic techniques, S. pneumoniae can be demonstrated in, on average, 25% (range 12%–68%) of cases.Citation6,Citation7
A variety of diagnostic tests, including sputum culture, blood culture, urine antigen test, and serological responses, can be performed to identify the causative agent of CAP.Citation8 An expectorated sputum sample can be cultured for respiratory pathogens or be analyzed by molecular methods. Similarly, blood cultures can be performed in case of a bacteremic pneumonia. Urinalysis can detect the presence of pneumococcal cell wall polysaccharides or serotype-specific capsular polysaccharides.Citation9,Citation10 An indirect, but specific, method to investigate the involvement of S. pneumoniae in CAP is the analysis of the serological response, that is, the increase in serotype-specific antibodies during the course of disease.Citation11 However, the latter test cannot be used during the diagnostic phase because it requires a blood sample >10 days after the onset of disease.
A comprehensive microbiological and virological analysis of the biological specimens described above reveals the varied etiology of CAP.Citation12–Citation14 Viruses such as influenza and respiratory syncytial virus can cause CAP. Major bacterial causes for CAP (in Europe) apart from S. pneumoniae, in descending order of importance, are as follows: Chlamydia species, Mycoplasma pneumoniae, Chlamydophila pneumoniae, Haemophilus influenzae, Legionella pneumophila, Pseudo-monas aeruginosa, Staphylococcus aureus, Chlamydophila psittaci, Coxiella burnetii, and Moraxella catarrhalis.Citation15,Citation16
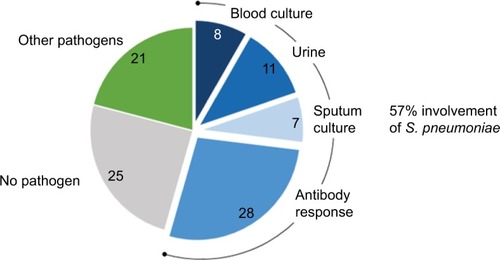
The data in show that, even when using an extensive diagnostic toolset, including serological responses, in 25% of CAP patients, no causative agent can be identified. An alternative but invasive diagnostic tool for establishing the causative agent for CAP is transthoracic needle aspiration (TTNA) biopsy. This is a procedure that has been used from as early as 1883 to diagnose pulmonary malignancies.Citation17 The biopsy is taken after a chest radiography has been used to identify consolidation adjacent to the chest wall. Additionally, anatomic landmarks are used to indicate where the needle should be inserted. The needle should be inserted immediately below the inferior angle of the scapula for lower lobe consolidation, through the anterior chest wall for upper lobe consolidation, and through the intercostal space lateral to the right nipple for right middle lobe consolidation. A very big advantage of this procedure is its minimally invasive nature, making it a desired alternative to surgical intervention.Citation18 The presence of a single pathogen in diseased tissue of patients with pneumonia and the absence of this in the same tissue in healthy control subjects is the most convincing evidence of the etiology of pneumonia.Citation19 Due to TTNA’s high specificity and relatively high yield, it is the most acceptable and uncontaminated single way of determining the etiology of pneumonia. The use of CT for guidance allows for good visualization and detection of smaller lesions as well. However, TTNA is not a widely practiced procedure due to concerns regarding the potential adverse effects. These potential complications include, but are not limited to, pneumothorax, hemorrhage, and air embolism. A postprocedure pneumothorax is the most common nonfatal complication, usually caused by large bullae in the path of the biopsy.
Figure 1 Microbiological etiology of CAP. A total of 349 CAP patients from 2 clinical trials were enrolled. Conventional microbiological analysis (blood culture, urinalysis, and sputum culture) identified Streptococcus pneumoniae as a causative organism. Determination of serotype-specific antibodies in serum showed S. pneumoniae involvement in an additional 28% of patients. Most commonly identified pathogens in the other pathogens category were Coxiella burnetti, Legionella species, Mycoplasma pneumoniae, Haemophilus influenzae, Chlamydophila psittaci, influenza A virus, and Staphylococcus aureus. Data from van Mens et al.Citation11
Although S. pneumoniae is a single bacterial species for the immune system and, therefore, for host defense and susceptibility, it is a collection of different bacterial species because of its polysaccharide capsule. Currently, 93 different types of polysaccharide capsules of S. pneumoniae are known to exist, subdivided in serologically distinguishable groups and types.Citation20 The 23 most prevalent serotypes are responsible for 80%–90% of all invasive pneumococcal diseases.Citation21 It must be kept in mind that great variation exists in serotype prevalence for the type of pneumococcal disease, the age category of risk groups, and geographical region. Pneumococcal serotypes 1 and 3 appear to have preferences for the lung, while serotypes/groups 6, 10, and 23 more often cause meningitis.Citation22,Citation23 In an observational study, the serotype distribution in isolates from patients with invasive pneumococcal disease was found to differ between children (common serotypes 4, 6B, 19F, and 18C) and adults where serotypes 3, 4, and 9V dominated.Citation24 Globally, serotypes 14, 19A, and 19F are most common in children, while in adults and the elderly, serotypes 3, 6A, 7F, and 19A are prevalent.Citation25
The most frequent pneumococcal serotypes in Europe are 1, 3, 7F, 14, and 19A, but rather big differences can be found between European countries.Citation26 On a global scale, the regional differences are much bigger. These aspects are important for the development of pneumococcal vaccines (see also below), because these vaccines should cover as many serotypes as possible, certainly the most common serotypes and the serotypes associated with the most severe disease. Furthermore, the vaccines should be immunogenic in the major risk groups and, preferably, induce long-lasting immunity.Citation26
Pneumococcal vaccines and vaccination
Two types of pneumococcal vaccines exist, which, from an immunological point of view, have a different mechanism of action depending on whether it is a polysaccharide or a so-called conjugate vaccine (). The difference in composition of the vaccines is that the polysaccharide vaccines contain a mixture of purified capsular polysaccharides, while the conjugate vaccines contain the capsular polysaccharides covalently linked (conjugated) to a protein carrier.
Table 1 Physical, chemical, and immunological characteristics of pneumococcal polysaccharides
The current 23-valent polysaccharide vaccine (PPSV23) covers the largest number of serotypes. These 23 serotypes cause 85%–90% of the invasive pneumococcal pneumonia cases in adults in the USA and several other countries.Citation27 The efficacy of PPSV23 in preventing CAP in adults is low (relative risk 0.54, 95% CI: 0.18–1.65).Citation28 Theoretically, the capsular polysaccharides of all 93 serotypes would constitute an all-inclusive and, therefore, complete pneumococcal vaccine. There is, however, a maximum amount of polysaccharide that can be included in a single dosage, and that maximum is reached with 23 serotypes (25 µg polysaccharide per serotype). In dose–response studies, it was found that a vaccine containing 12.5 µg polysaccharide per serotype resulted in lower antibody titers than 25 µg.Citation27
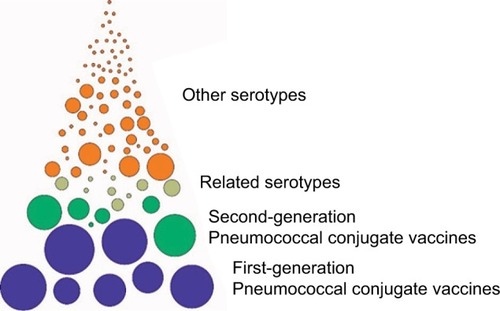
Moreover, because of the so-called law of diminishing returns, addition of extra serotypes would not lead to a proportional increase in serotype coverage (). The major drawbacks of PPSV23 are 2-fold: 1) this vaccine is not immunogenic in young children and 2) polysaccharide vaccines do not induce immunologic memory (). Both drawbacks of polysaccharide vaccines can be overcome by coupling of the polysaccharide to a protein carrier, pioneered by Avery and Goebel.Citation29 This Nobel prize worthy discovery was made at a time when all medical research was focused on antibiotics; so, it took over half a century before the principles of Avery were put into practice for the production of polysaccharide conjugate vaccines. The first generation of pneumococcal conjugate vaccines was the 7-valent conjugate vaccine (PVC7), consisting of serotypes 4, 6B, 9V, 14, 18C, 19F, and 23F. This vaccine soon became a part of the standard vaccination schedules for children. After introduction of PCV7, a sharp decline in vaccine-serotype invasive pneumococcal disease was observed in children.Citation30,Citation31 Apart from protection against invasive disease, PCV7 also induced mucosal protection, reducing nasopharyngeal colonization and subsequently also reducing the transmission of vaccine serotypes to others. As a result, vaccine-type invasive pneumococcal disease also decreased in the unvaccinated community due to herd protection, particularly in the elderly >65 years of age.Citation32–Citation34 The net benefit of PCV7 introduction was limited by the occurrence of the so-called replacement disease, which is invasive pneumococcal disease caused by serotypes not included in the vaccine. For example, 19A became a frequently occurring serotype that induced CAP, the most frequent serotype in some populations.Citation32–Citation35 The fact that 19A became so prevalent while 19F was incorporated in PCV7 came as a surprise. Up till that moment, it was assumed that antibodies against a serotype within one serogroup would lead to cross-protection: antibodies against 6A would also protect against an infection with 6B.Citation36–Citation39 Apparently, cross protection within serogroups is not operational for serogroup 19.Citation40 Replacement disease especially occurs in older adults and persons with comorbidity. Thus, large-scale implementation of PCV7 has dramatically changed the pneumococcal landscape through the direct effects in children and by indirect herd effects in nonvaccinated persons.Citation30,Citation33,Citation34 Serotype replacement disease, next to expanding the coverage, has been one of the arguments for development of 10- and 13-valent conjugate vaccines.Citation41–Citation43 These vaccines incorporate more of the most predominant serotypes, including the replacement serotypes ().Citation44–Citation46 Also, after introduction of PCV13, serotype replacement continues. Across Europe, 24F and 15A now are the emerging serotypes not included in the PPSV23.Citation47 In other continents, other serotypes may emerge, such as 23B, 21, and 35B in the USA.Citation48,Citation49 The emerging serotypes in Europe, also including 22F and 8 that are PPSV23 serotypes, appear to be less invasive with a relative low case: carrier ratio.Citation47 It is too early to tell whether these or other serotypes should be added to the next generation of PCVs. It is also too early to tell whether serotype replacement has come to an end or is still ongoing. At any rate, it is to be expected that the next generation of pneumococcal conjugate vaccines would need to have an expanded coverage. Multivalency ceiling, as discussed above for polysaccharide vaccines, is not an issue for PCV because in the conjugate vaccines, typically only 2–4 µg of polysaccharide is used per serotype. A multivalency ceiling could exist when considering carrier-specific immune suppression (via carrier-induced epitopic suppression, high-dose tolerance as such, or otherwise). This phenomenon has been observed in clinical studies and was reviewed by Findlow and Borrow.Citation50 The solution can be to use a carrier protein (or a combination of several different carrier proteins) different from other vaccine components.
Figure 2 Pneumococcal serotypes and pneumococcal vaccines.
Pneumococcal vaccination in the elderly
For the elderly (aged ≥65 years), the recommended vaccine in terms of coverage is PPSV23.Citation51 This vaccine does protect the elderly against invasive pneumococcal disease, but not completely.Citation52–Citation55 The reason(s) why polysaccharide vaccines have limited effectivity in the elderly is not entirely clear. A decline in functionality of the immune system could be one of the underlying mechanisms. In healthy elderly, both immunoglobulin (Ig) A and IgG anti-pneumococcal antibody levels have been shown to increase during the ages of 70–90.Citation56 The functional antibody activity, as assessed by opsonophagocytosis, IgG antibody avidity, and passive protection in mice, however, is decreased in the elderly.Citation57 These data suggest that even though there is an increase in the antibody titer, a reduction in the functionality of the antibodies occurs with age, which can explain the limited effectivity of PPSV23 in the elderly. Opsonophagocytosis is mediated primarily by neutrophils, which circulate through the bloodstream, phagocytosing and killing microbes. A decrease in the functional activity of neutrophils due to aging could therefore also contribute to increased vulnerability of the elderly. Indeed, neutrophils of the elderly population showed a significant decline in phagocytic killing of pneumococci opsonized with antibodies and complement.Citation58 All these lead to a decline of the ability to generate an adequate immune response and thus increasing the susceptibility to bacterial infections, including pneumonia.
The term that has been coined to describe the declined functionality of the immune system in the elderly is immunosenescence, which is the accumulation of age-associated alterations that result in a progressive deterioration in the immune system. Immunosenescence and its associated chronic low-grade systemic “inflamm aging” contribute to the development and progression of pulmonary disease in older individuals.Citation59–Citation61 Many other alterations, which affect both the innate and adaptive immune systems, have been described, which cannot be addressed in detail in this review.Citation62–Citation66 All these lead to a decline of the ability to generate an adequate immune response and thus increasing the susceptibility to bacterial infections, including pneumonia.Citation67
Whether the limited effectivity of pneumococcal polysaccharide vaccines in the elderly is due to immunosenescence, there is an obvious need for better vaccines for this risk category. The obvious choice would be a conjugate vaccine. In the Netherlands, the efficacy of PCV13 has been tested in older, but otherwise healthy adults.Citation68 In a randomized, double-blind, placebo-controlled trial, over 80,000 participants >65 years of age were enrolled and followed-up for a period of maximum 2 years.Citation69 For CAP caused by vaccine-type pneumococcal strains, the vaccine efficacy was 45.6% (95% CI: 21.8–62.5). For any pneumococcal CAP, vaccine efficacy was lower at 30.6% (95% CI: 9.8–46.7); for any-cause CAP, No protective effect was found for any-cause CAP, vaccine efficacy 5.1% (95% CI: −5.1 to 14.2).Citation69,Citation70 Based on the outcome of this study, the current advice for vaccination of the elderly against CAP and other pneumococcal disease now tends to be the use of conjugate vaccines.Citation71,Citation72 Based on the data from the GRADE study, 1620 people would be needed to vaccinate (NNV) in order to prevent one case of hospitalized CAP.Citation73 When taking into account the cumulative effect of preventing cases over a 5-year period, the NNV with PCV13 would be substantially lower at 576.Citation74 Based on the CAPiTA study, an estimate was made of the quality-adjusted life years, costs of vaccination, and efficacy of the vaccine using incremental cost-effectiveness ratios. It was concluded that vaccination of high-risk individuals in the age category of 65–74 years is cost saving, and when medium-risk individuals aged 65–74 years are included, an incremental cost-effectiveness ratio of €2900 results.Citation75
Outcome of pneumonia
William Osler in his book, The Principles and Practice of Medicine (first edition published in 1892), summarizes the prognosis of pneumococcal pneumonia as follows: “In a disease which carries off one in every four or five of those attacked the prognosis in a large number of cases is necessarily grave”.Citation76 In the era before antibiotics were available, the overall mortality rate of pneumococcal pneumonia was 20%–25%. Osler continues by pointing out the risk groups:
In children and in healthy adults the outlook is good. In the debilitated, in drunkards, and in the aged the chances are against recovery. So fatal is it in the latter class (the elderly) that it has been termed the natural end of the old man.
This latter sentence later was transformed into the saying “pneumonia is old man’s friend”. Risk groups for pneumococcal pneumonia, apart from the elderly, according to Osler, are the debilitated and drunkards. Chronic alcohol abuse indeed suppresses the immune systemCitation77 and may lead to a higher susceptibility for pneumococcal infections.Citation78 Four out of the 6 observational studies found an increased risk for pneumococcal pneumonia in alcohol abusers (odds ratios ranging from 2.9 to 11.4).Citation79 We can only speculate whether the current recognized additional risk groups for pneumococcal pneumonia (chronic lung [including asthma], heart, liver, or kidney disease; diabetes; various types of cancer; absence of spleen; and smoking) could be grouped under the heading “debilitated” in Osler’s time and age.Citation80,Citation81 In the song “Baby it’s cold outside”, written in 1944 by Frank Loesser for the movie Neptune’s Daughter, the male singer appeals to a health risk of the woman he is trying to convince to stay with him:“[…] if you caught pneumonia and died […]”. The discovery and implementation of antibiotics offered adequate treatment options for pneumonia and greatly reduced the death rate.Citation82 Modern hospitalization and adequate antibiotic treatment has resulted in a 30-day survival of >95% of the overall patient population admitted to the hospital with CAP, and thus, prognosis of pneumonia has improved tremendously.Citation83
The vast majority of pneumonia deaths occur in the second- and third-world countries, but also in the USA, pneumonia remains the eigth leading cause of death, with 15.9 deaths per 100,000 population in 2014. Figures in Europe are also similar.Citation84,Citation85 Among infections, pneumonia is the leading cause of hospitalization and death for nursing home residents.Citation86,Citation87 Nursing home-acquired pneumonia patients show mortality rates as high as 40% of the patients who required hospitalization.Citation88
The patients who survive hospitalization for CAP may still experience adverse outcomes after hospital discharge, and these include readmission and death due to a relapse of pneumonia or because of another cause. In the PORT cohort trial, 30% of CAP patients had died after a median follow-up of 5.9 years.Citation83 Risk factors for late mortality are increased age (>65 years of age), immune suppression, and cardiovascular disease.Citation89–Citation91 In our own studies, the (all-cause) long-term mortality of CAP patients is equally high: after 1 year, 17% of these patients have died, and after 5 years, it was 27%.Citation92,Citation93
Three scenarios can be envisioned on the relation between cardiovascular disease and CAP mortality. Preexisting cardiovascular disease as a comorbidity does have a negative impact on survival rates of CAP.Citation94 In the second scenario, pneumococcal pneumonia can lead to a ventilation–perfusion mismatch pattern.Citation95 This compromised state of oxygenation leads to an increase in myocardial oxygen demand and, as a result, stress on the myocardium. In the third scenario, the pneumococci invade the myocardium and form microlesions that cause cardiac dysfunction.Citation96,Citation97 The pneumococci that invade the myocardium form biofilms, making them resistant to antibiotic killing. Moreover, pneumococci that grow in biofilms release large amounts of pneumolysin, thereby killing resident cardiac macrophages and evading the host response.Citation98 Via any of these or other pathophysiologic events, major acute cardiac events could be induced. Indeed, patients with pneumococcal pneumonia are substantially more likely to experience simultaneous or subsequent acute cardiac events.Citation99–Citation101
In Osler’s time, pneumococcal pneumonia was the natural end of the old man. Now, after more than a century of improved medical care, the long-term mortality figures seem to indicate that pneumococcal pneumonia predicts the natural end of the old man. From the above data, it is clear that cardiac involvement, either preexisting or induced, predicts a poor long-term outcome. Recent data from our own group indicate that, on top of and beyond classical pneumonia severity, scoring systems such as Curb65 and PSI, biomarkers for cardiac function (cardiac troponin T), are associated with long-term mortality.Citation93 Future treatments aimed at preventing cardiovascular events could improve long-term survival of patients with pneumococcal pneumonia.Citation102
Costs of hospitalization
Milder forms of CAP can be treated by the general practitioner or in an outpatient setting, but ~20%–60% of CAP patients need to be hospitalized. The direct costs of hospitalization account for 56% of the economic burden of CAP in Europe. The remainder of the costs is caused by medication, outpatient care, and loss of workdays of the patients.
The average duration of a hospital stay for CAP varies between different countries. In the Netherlands, the mean hospitalization period was found to be 7.5–12.1 days;Citation103,Citation104 in the USA, a similar range of 4–12 days has been found.Citation105–Citation109 A comparison of hospitalization costs for CAP in various European countries and the USA shows great differences (). It has been recognized that comparision between several countries of the costs of hospitalization is difficult to nearly impossible due to different settings and health-care systems.Citation117 Even within a given country, substantial differences can be found, as is evident from for the range in hospitalization costs within the Netherlands and the USA. Characteristics of the patient population (age and comorbidities), severity of CAP in relation to intensive care unit (ICU) admission, length of hospital stay, and level of the hospital (second or third level) contribute to this variation. Particularly, the length of a hospital stay is a major cost driver because a general ward stay amounts to 57% of the total hospital costs, followed by ICU nursing with 16%.Citation116 From such a cost breakdown, it also becomes clear that treatment strategies that result in a reduction of the length of stay lead to a substantial reduction in costs.Citation103
Table 2 Costs of hospitalization of community-acquired pneumonia
With an ongoing increase in life expectancy and an aging population in general, the costs of hospitalization probably will increase further in the future. These trends will also affect the cost-effectiveness of preventive measures such as vaccination.
Conclusion
Pneumococcal pneumonia was and still remains a serious disease that mainly affects young children and the elderly. Despite adequate antibiotic treatment, the long-term mortality of pneumococcal pneumonia remains high. Preventive measures therefore are warranted. Pneumococcal conjugate vaccination can prevent invasive and mucosal pneumococcal diseases in children and also in the elderly. It should be recognized that the serotype composition of current pneumococcal conjugate vaccines is not tailored for the elderly, and that replacement disease still could occur. Yet the 13-valent conjugate vaccine has been shown to be protective against the vaccine-included serotypes. Long-term mortality of pneumococcal pneumonia should be included in policy making about introduction of these vaccines for the elderly.
In the painting, The Triptych of the Hermit Saints (), St. Jerome, St. Antony, and St. Giles are depicted on the 3 separate panels. All the 3 Saints are old men, a risk group for pneumococcal pneumonia. The Triptych is a painting of Hieronimus Bosch, one of the greatest Dutch painters. All of his paintings depict scenes beyond imagination, and even 600 years after his death, the debates on the interpretation of his works continues. Triptych of the Hermit Saints is on permanent display in the Gallerie dell’Accademia, Venice, Italy, but was brought to “‘s Hertogenbosch in 2016 on the occasion of Bosch” 600th anniversary. The center panel depicts St. Jerome kneeling in a desert-like landscape and surrounded by symbols of evil. In the left panel, St. Anthony, the Abbot, is situated in a landscape that has in the background, a burning village. Also, he is surrounded by demons of all sorts. The third hermit, St. Giles, in the right-hand panel clearly stands out. He is praying in his cave and appears to be at total ease, although he has been shot by an arrow. It does not take much imagination (or a bit of bias) to envision the arrow as the syringe by which St. Giles has been vaccinated. For that reason, he is immune against the great variety of demons that also surround him. The variety of demons represent, of course, all the serotypes of pneumococci. On the desk of St. Giles, we see a book of prayers and a roll of paper with something written on it. Maybe, they are the names of other people and other saints, saved thanks to vaccination.
Figure 3 Detail of the right panel of The Triptych of the Hermit Saints by Hieronymus Bosch (1493), Gallerie dell’Accademia, Venice, Italy.
In times of despair, St. Giles, as a patron saint, is called upon in case of infectious disease, either acute or chronic, both for the elderly as for the (very) young. It has to be admitted that, also in case of drought, idiocy, or marital infertility, St. Giles is called upon for help. At any rate, in order to be protected against S. pneumoniae, it is better to be vaccinated than to rely on protection by St. Gilles.
Acknowledgments
GT Rijkers reports receiving grants from Pfizer for research on pneumococcal vaccines and lecturing fees from Pfizer and GlaxoSmithKline.
Disclosure
The authors report no conflicts of interest in this work.
References
- HendleyJOClinical practice. Otitis mediaN Engl J Med2002347151169117412374878
- https://www.who.int/immunization/monitoring_surveillance/burden/estimates/Pneumo_hib/en/Accessed October 16, 2017
- https://www.who.int/medicines/areas/priority_medicines/Ch6_22Pneumo.pdfAccessed October 16, 2017
- DochezARAveryOTVarieties of pneumococcus and their relation to lobar pneumoniaJ Exp Med19152111413219867855
- HeffronRPneumonia, with Special Reference to Pneumococcus Lobar PneumoniaCambridge, MAHarvard University Press1939
- DrijkoningenJJRohdeGGPneumococcal infection in adults: burden of diseaseClin Microbiol Infect201420Suppl 5455124313448
- WelteTTorresANathwaniDClinical and economic burden of community-acquired pneumonia among adults in EuropeThorax201267717920729232
- EndemanHSchelfhoutVVoornGPvan Velzen-BladHGruttersJCBiesmaDHClinical features predicting failure of pathogen identification in patients with community acquired pneumoniaScand J Infect Dis20084071572019086245
- PrideMWHuijtsSMWuKValidation of an immunodiagnostic assay for detection of 13 Streptococcus pneumoniae serotype-specific polysaccharides in human urineClin Vaccine Immunol20121981131114122675155
- HuijtsSMPrideMWVosJMDiagnostic accuracy of a serotype-specific antigen test in community-acquired pneumoniaEur Respir J20134251283129023397295
- van MensSPMeijvisSCEndemanHLongitudinal analysis of pneumococcal antibodies during community-acquired pneumonia reveals a much higher involvement of Streptococcus pneumoniae than estimated by conventional methods aloneClin Vaccine Immunol201118579680121367978
- RendonARendon-RamirezEJRosas-TaracoAGRelevant cytokines in the management of community-acquired pneumoniaCurr Infect Dis Rep2016181026874956
- McCullohRJPatelKRecent developments in pediatric community-acquired pneumoniaCurr Infect Dis Rep2016181426960931
- PletzMWRohdeGGWelteTKolditzMOttSAdvances in the prevention, management, and treatment of community-acquired pneumoniaF1000Res20165300
- WoodheadMBlasiFEwigSGuidelines for the management of adult lower respiratory tract infections – full versionClin Microbiol Infect201117Suppl 6E1E59
- AlibertiSKayeKSThe changing microbiologic epidemiology of community-acquired pneumoniaPostgrad Med201312563142
- HernesSSHagenEToftelandSTransthoracic fine-needle aspiration in the aetiological diagnosis of community-acquired pneumoniaClin Microbiol Infect201016790991119681958
- IdehRCHowieSREbrukeBTransthoracic lung aspiration for the aetiological diagnosis of pneumonia: 25 years of experience from The GambiaInt J Tuberc Lung Dis201115672973521477423
- ScottJAHallAJThe value and complications of percutaneous transthoracic lung aspiration for the etiologic diagnosis of community-acquired pneumoniaChest199911661716173210593800
- GenoKAGilbertGLSongJYPneumococcal capsules and their types: past, present, and futureClin Microbiol Rev201528387189926085553
- FedsonDSNicolas-SponyLKlemetsPPneumococcal polysaccharide vaccination for adults: new perspectives for EuropeExpert Rev Vaccines2011101143116721810065
- HausdorffWPBryantJKloekCParadisoPRSiberGRThe contribution of specific pneumococcal serogroups to different disease manifestations: implications for conjugate vaccine formulation and use, part IIClin Infect Dis20003012214010619741
- TanTQMasonEOJrWaldERClinical characteristics of children with complicated pneumonia caused by Streptococcus pneumoniaePediatrics20021101612093940
- ImöhlMReinertRROcklenburgCvan der LindenMAssociation of serotypes of Streptococcus pneumoniae with age in invasive pneumococcal diseaseJ Clin Microbiol20104841291129620107087
- HachelMLascolsCBouchillonSHiltonBMorgensternDPurdyJSerotype prevalence and antibiotic resistance in Streptococcus pneumoniae clinical isolates among global populationVaccine2013314881488723928466
- AlibertiSManteroMMirsaeidiMBlasiFThe role of vaccination in preventing pneumococcal disease in adultsClin Microbiol Infect201420Suppl 55258
- RobbinsJBAustrianRLeeCJConsiderations for formulating the second-generation pneumococcal capsular polysaccharide vaccine with emphasis on the cross-reactive types within groupsJ Infect Dis1983148113611596361173
- DiaoWQShenNYuPXLiuBBHeBEfficacy of 23-valent pneumococcal polysaccharide vaccine in preventing community-acquired pneumonia among immunocompetent adults: a systematic review and meta-analysis of randomized trialsVaccine2016341496150326899376
- AveryOGoebelWFChemo-immunological studies on conjugated carbohydrate-proteins. II. Immunological specificity of synthetic sugar protein antigensJ Exp Med19295053355019869645
- WhitneyCGFarleyMMHadlerJDecline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccineN Engl J Med2003348181737174612724479
- FitzwaterSPChandranASantoshamMJohnsonHLThe worldwide impact of the seven-valent pneumococcal conjugate vaccinePediatr Infect Dis J201231550150822327872
- LexauCALynfieldRDanilaRActive Bacterial Core Surveillance TeamChanging epidemiology of invasive pneumococcal disease among older adults in the era of pediatric pneumococcal conjugate vaccineJAMA2005294162043205116249418
- van DeursenAMvan MensSPSandersEAInvasive Pneumococcal Disease Sentinel Surveillance Laboratory GroupInvasive pneumococcal disease and 7-valent pneumococcal conjugate vaccine, the NetherlandsEmerg Infect Dis201218111729173723092683
- MyintTTMadhavaHBalmerPThe impact of 7-valent pneumococcal conjugate vaccine on invasive pneumococcal disease: a literature reviewAdv Ther201330212715123397399
- DaganRSerotype replacement in perspectiveVaccine200927Suppl 3C22C2419545935
- VestrheimDFSteinbakkMAabergeISCaugantDAPostvaccination increase in serotype 19A pneumococcal disease in Norway is driven by expansion of penicillin-susceptible strains of the ST199 complexClin Vaccine Immunol201219344344522237889
- ScottJRHanageWPLipsitchMPneumococcal sequence type replacement among American Indian children: a comparison of pre- and routine-PCV7 erasVaccine201230132376238122094283
- MillerEAndrewsNJWaightPASlackMPGeorgeRCHerd immunity and serotype replacement 4 years after seven-valent pneumococcal conjugate vaccination in England and Wales: an observational cohort studyLancet Infect Dis2011111076076821621466
- KimHWLeeSKimKHSerotype 6B from a pneumococcal polysaccharide vaccine induces cross-functional antibody responses in adults to serotypes 6A, 6C, and 6DMedicine (Baltimore)20169537e485427631247
- GrantLRO’BrienSEBurbidgePComparative immunogenicity of 7 and 13-valent pneumococcal conjugate vaccines and the development of functional antibodies to cross-reactive serotypesPLoS One201389e7490624086394
- VesikariTKarvonenAKorhonenTImmunogenicity of 10-valent pneumococcal nontypeable Haemophilus influenzae Protein D Conjugate Vaccine when administered as catch-up vaccination to children 7 months to 5 years of agePediatr Infect Dis J2011308e130e14121540760
- LeeHChoiEHLeeHJEfficacy and effectiveness of extended-valency pneumococcal conjugate vaccinesKorean J Pediatr2014572556624678328
- AdlerHFerreiraDMGordonSBRylanceJPneumococcal capsular polysaccharide immunity in the elderlyClin Vaccine Immunol2017246e00004e0001728424198
- PrincipiNEspositoSDevelopment of pneumococcal vaccines over the last 10 yearsExpert Opin Biol Ther201818171729022363
- RijkersGTFixing a hole: preventing pneumococcal pneumonia by vaccinationFront Immunol2016734927679637
- RijkersGTvan MensSPvan Velzen-BladHWhat do the next 100 years hold for pneumococcal vaccination?Expert Rev Vaccines20109111241124421087102
- Tin Tin HtarMChristopoulouDSchmittHJPneumococcal serotype evolution in Western EuropeBMC Infect Dis20151541926468008
- KaurRCaseyJRPichicheroMEEmerging Streptococcus pneumoniae strains colonizing the nasopharynx in children after 13-valent pneumococcal conjugate vaccination in comparison to the 7-valent era, 2006–2015Pediatr Infect Dis J20163590191627420806
- RichterSSDiekemaDJHeilmannKPDohrnCLRiahiFDoernGVChanges in pneumococcal serotypes and antimicrobial resistance after introduction of the 13-valent conjugate vaccine in the United StatesAntimicrob Agents Chemother2014586484648925136018
- FindlowHBorrowRInteractions of conjugate vaccines and co-administered vaccinesHum Vaccin Immunother20161222623026619353
- Recommended Adult Immunization Schedule, by Vaccine and Age GroupCenters for Disease Control and PreventionAtlanta, GA2015
- MaruyamaTTaguchiONiedermanMSEfficacy of 23-valent pneumococcal vaccine in preventing pneumonia and improving survival in nursing home residents: double blind, randomised and placebo controlled trialBMJ2010340c100420211953
- Leventer-RobertsMFeldmanBSBrufmanICohen-StaviCJHoshenMBalicerRDEffectiveness of 23-valent pneumococcal polysaccharide vaccine against invasive disease and hospital-treated pneumonia among people aged ≥65 years: a retrospective case-control studyClin Infect Dis201560101472148025669354
- Ochoa-GondarOVila-CorcolesARodriguez-BlancoTEffectiveness of the 23-valent pneumococcal polysaccharide vaccine against community-acquired pneumonia in the general population aged ≥60 years: 3 years of follow-up in the CAPAMIS studyClin Infect Dis201458790991724532544
- RijkersGTPneumococcal vaccination in elderlyPneumococcal Conjugate Vaccines, Future MedicineLondon, UK20123245
- BátoryGJancsóAPuskásERédeiALengyelEAntibody and immunoglobulin levels in aged humansArch Gerontol Geriatr1984321751886476977
- Romero-SteinerSMusherDMCetronMSReduction in functional antibody activity against Streptococcus pneumoniae in vaccinated elderly individuals highly correlates with decreased IgG antibody avidityClin Infect Dis199929228128810476727
- SimellBVuorelaAEkströmNAging reduces the functionality of anti-pneumococcal antibodies and the killing of Streptococcus pneumoniae by neutrophil phagocytosisVaccine201129101929193421236231
- MurrayMAChotirmallSHThe impact of immunosenescence on pulmonary diseaseMediators Inflamm2015201569254626199462
- PeraACamposCLópezNImmunosenescence: implications for response to infection and vaccination in older peopleMaturitas2015821505526044074
- KovacsEJBoeDMBouleLACurtisBJInflammaging and the lungClin Geriatr Med201733445947128991644
- LeeSKimHWLeeJHKimKHFunctional immune responses to 11 non-PCV13 serotypes after immunization with a 23-valent pneumococcal polysaccharide vaccine in older adultsVaccine201735374960496528778614
- van de VosseEvan Ostaijen-Ten DamMMVermaireRRecurrent respiratory tract infections (RRTI) in the elderly: a late onset mild immunodeficiency?Clin Immunol2017180111111928487087
- RothAGlaesenerSSchützKMeyer-BahlburgAReduced number of transitional and naive B cells in addition to decreased BAFF levels in response to the T cell independent immunogen Pneumovax®23PLoS One2016113e015221527031098
- HeaneyJLPhillipsACCarrollDDraysonMTSalivary functional antibody secretion is reduced in older adults: a potential mechanism of increased susceptibility to bacterial infection in the elderlyJ Gerontol A Biol Sci Med Sci201570121578158526328602
- AhnJGKimHWChoiHJLeeJHKimKHFunctional immune responses to twelve serotypes after immunization with a 23-valent pneumococcal polysaccharide vaccine in older adultsVaccine201533384770477526277073
- AwDSilvaABPalmerDBImmunosenescence: emerging challenges for an ageing populationImmunology2007120443544617313487
- HakEGrobbeeDESandersEARationale and design of CAPITA: a RCT of 13-valent conjugated pneumococcal vaccine efficacy among older adultsNeth J Med200866937838318990781
- BontenMJHuijtsSMBolkenbaasMPolysaccharide conjugate vaccine against pneumococcal pneumonia in adultsN Engl J Med2015372121114112525785969
- van WerkhovenCHBontenMJThe Community-Acquired Pneumonia immunization Trial in Adults (CAPiTA): what is the future of pneumococcal conjugate vaccination in elderly?Future Microbiol20151091405141326347153
- BlackCLWilliamsWWWarnockRPneumococcal vaccination among Medicare beneficiaries occurring after the advisory committee on immunization practices recommendation for routine use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults aged ≥65 yearsMMWR Morb Mortal Wkly Rep2017662772873328704347
- DirmesropianSWoodJGMacIntyreCRCost-effectiveness of 13-valent pneumococcal conjugate vaccine (PCV13) in older AustraliansVaccine201735344307431428693751
- Advisory Committee on Immunization PracticesGrading of Recommendations, Assessment, Development, and Evaluation (GRADE) for pneumococcal vaccines for adults aged ≥65 yearsUS Department of Health & Human Services Available from: https://www-cdc-gov.proxy.library.uu.nl/vaccines/acip/recs/grade/pneumo-vac-adult.htmlAccessed September 29, 2017
- McLaughlinJMSwerdlowDLIsturizREJodarLRethinking number-needed-to-vaccinate for pneumococcal conjugate vaccines in older adults: current and future implicationsVaccine201735405360536528863866
- MangenMJRozenbaumMHHuijtsSMCost-effectiveness of adult pneumococcal conjugate vaccination in the NetherlandsEur Respir J20154651407141626160871
- OslerWThe Principles and Practice of Medicine Available from: https://archive.org/details/principlesandpr00mccrgoogAccessed September 29, 2017
- CookRTAlcohol abuse, alcoholism, and damage to the immune system–a reviewAlcohol Clin Exp Res1998229192719429884135
- RushBEffects of Ardent Spirits upon the Human Body and Mind, with an Account of the Means of Preventing and of the Remedies for Curing ThemPhiladelphia, PAThomas Dobson1810
- CruickshankHCJefferiesJMClarkeSCLifestyle risk factors for invasive pneumococcal disease: a systematic reviewBMJ Open20142046e005224
- RuizMEwigSTorresASevere community-acquired pneumonia. Risk factors and follow-up epidemiologyAm J Respir Crit Care Med1999160392392910471620
- AlmirallJSerra-PratMBolíbarIBalassoVRisk factors for community-acquired pneumonia in adults: a systematic review of observational studiesRespiration201794329931128738364
- PodolskySHThe changing fate of pneumonia as a public health concern in 20th-century America and beyondAm J Public Health200595122144215416257952
- MortensenEMKapoorWNChangCCFineMJAssessment of mortality after long-term follow-up of patients with community-acquired pneumoniaClin Infect Dis200337121617162414689342
- https://www.cdc.gov/nchs/data/nvsr/nvsr65/nvsr65_04.pdfAssessed October 19, 2017
- https://www.who.int/medicines/areas/priority_medicines/Ch6_22Pneumo.pdfAssessed October 19, 2017
- Beck-SagueCBanerjeeSJarvisWRInfectious diseases and mortality among US nursing home residentsAm J Public Health19938312173917428259806
- DhawanNPandyaNKhaliliMPredictors of mortality for nursing home-acquired pneumonia: a systematic reviewBiomed Res Int2015201528598325821793
- MarrieTJPneumoniaClin Geriatr Med1992847217341423131
- Corrales-MedinaVFMusherDMShachkinaSChirinosJAAcute pneumonia and the cardiovascular systemLancet2013381986549650523332146
- RamirezJAlibertiSMirsaeidiMAcute myocardial infarction in hospitalized patients with community-acquired pneumoniaClin Infect Dis200847218218718533841
- MortensenEMMeterskyMLLong-term mortality after pneumoniaSemin Respir Crit Care Med201233331932422718218
- WagenvoortGHSandersEAde MelkerHEvan der EndeAVlaminckxBJKnolMJLong-term mortality after IPD and bacteremic versus non-bacteremic pneumococcal pneumoniaVaccine201735141749175728262334
- VestjensSMTSpoorenbergSMCRijkersGTHigh-sensitivity cardiac troponin T predicts mortality after hospitalization for community-acquired pneumoniaRespirology20172251000100628221010
- CarbonCOptimal treatment strategies for community-acquired pneumonia: high-risk patients (geriatric and with comorbidity)Chemotherapy200147Suppl 41925
- BajcMNeillyBMiniatiMMortensenJJonsonBMethodology for ventilation/perfusion SPECTSemin Nucl Med201040641542520920632
- BrownAOOrihuelaCJVisualization of Streptococcus pneumoniae within cardiac microlesions and subsequent cardiac remodelingJ Vis Exp201598
- BrownAOMannBGaoGStreptococcus pneumoniae translocates into the myocardium and forms unique microlesions that disrupt cardiac functionPLoS Pathog2014109e100438325232870
- ShenoyATBrissacTGilleyRPStreptococcus pneumoniae in the heart subvert the host response through biofilm-mediated resident macrophage killingPLoS Pathog2017138e100658228841717
- ReyesLFRestrepoMIHinojosaCASevere pneumococcal pneumonia causes acute cardiac toxicity and subsequent cardiac remodelingAm J Respir Crit Care Med2017196560962028614669
- MusherDMRuedaAMKakaASMaparaSMThe association between pneumococcal pneumonia and acute cardiac eventsClin Infect Dis200745215816517578773
- PerryTWPughMJWatererGWIncidence of cardiovascular events after hospital admission for pneumoniaAm J Med2011124324425121396508
- FeldmanCAndersonRPrevalence, pathogenesis, therapy, and prevention of cardiovascular events in patients with community-acquired pneumoniaPneumonia201681128702290
- MeijvisSCHardemanHRemmeltsHHDexamethasone and length of hospital stay in patients with community-acquired pneumonia: a randomised, double-blind, placebo-controlled trialLancet201137797822023203021636122
- VissinkCEHuijtsSMde WitGABontenMJMangenMJHospitalization costs for community-acquired pneumonia in Dutch elderly: an observational studyBMC Infect Dis20161646627589847
- KaplanVAngusDCGriffinMClermontGWatsonRSLinde-ZwirbleWTHospitalized community-acquired pneumonia in the elderly: age- and sex-related patterns of care and outcome in the United StatesAm J Respir Crit Care Med200216576677211897642
- DeFrancesCJLucasCABuleVCGolosinskiyA2006 National Hospital discharge surveyNatl Health Stat Rep200830120
- MeterskyMLMaAHouckPMBratzlerDWAntibiotics for bacteremic pneumonia: improved outcomes with macrolides but not fluoroquinolonesChest200713146647317296649
- RestrepoMIMortensenEMVelezJAFreiCAnzuetoAA comparative study of community-acquired pneumonia patients admitted to the ward and the ICUChest200813361061717989157
- HallMJDeFrancesCJWilliamsSNNational Hospital Discharge survey: 2007 summaryNatl Health Stat Report201029121
- OstermannHGarauJMedinaJPascualEMcBrideKBlasiFREACH study groupResource use by patients hospitalized with community-acquired pneumonia in Europe: analysis of the REACH studyBMC Pulm Med2014143624593248
- TichopadARobertsCGembulaIClinical and economic burden of community-acquired pneumonia among adults in the Czech Republic, Hungary, Poland and SlovakiaPLoS One201388e7137523940743
- SatoRGomez ReyGNelsonSPinskyBCommunity-acquired pneumonia episode costs by age and risk in commercially insured US adults aged ≥50 yearsAppl Health Econ Health Policy201311325125823605251
- YuHRubinJDunningSLiSSatoRClinical and economic burden of community-acquired pneumonia in the Medicare fee-for-service populationJ Am Geriatr Soc201260112137214323110409
- ThomasCPRyanMChapmanJDIncidence and cost of pneumonia in medicare beneficiariesChest2012142497398122406959
- JacobCMittendorfTGraf von der SchulenburgJMKrankheitskosten sowie gesundheitsbezogene Lebensqualität (hrQoL) bei ambulant erworbener Pneumonie (CAP) - ein systematisches [Costs of illness and health-related quality of life for community-acquired pneumonia–a systematic review]Pneumologie2011658498502 German21512972
- SpoorenbergSMBosWJHeijligenbergRMicrobial aetiology, outcomes, and costs of hospitalisation for community-acquired pneumonia; an observational analysisBMC Infect Dis20141433524938861
- WelteRFeenstraTJagerHLeidlRA decision chart for assessing and improving the transferability of economic evaluation results between countriesPharmacoeconomics2004221385787615329031
- PeetersCCTenbergen-MeekesAMHaagmansBPneumococcal conjugate vaccinesImmunol Lett19913022672741757114
- RodenburgGDde GreeffSCJansenAGEffects of pneumococcal conjugate vaccine 2 years after its introduction, the NetherlandsEmerg Infect Dis201016581682320409372
- Wikimedia Commons [homepage on the internet]Jheronimus Bosch Gallery. 2.1.17 The Hermit Saints Triptych Available from: https://commons.wikimedia.org/wiki/Jheronimus_Bosch#The_Hermit_Saints_TriptychAccessed March 9, 2018
- UN Data [homepage on the internet]Per capita GDP at current prices Available from: http://data.un.org/Data.aspx?q=GDP+per+capita&d=SNAAMA&f=grID%3a101%3bcurrID%3aUSD%3bpcFlag%3a1Accessed March 9, 2018
