Abstract
Background
Implementing accurate data management systems ensure safe and efficient transfer of confidential health care data. However, health care professionals overlooked their important tasks of medical data processing. Hence, using high-quality electronic health record (EHR) applications in health care is important to minimize medical errors. Therefore, this review tries to indicate the roles of EHR in advancing quality health care service provisions.
Methods
The keywords identified were EHR, EMR, medical data processing, medical data retention, medical data destruction, health care, and patient care, and a few related terms with different combinations. PubMed (National Library of Medicine), Google Scholar, and Google search engine were used to search for articles from those databases. Searching was done using boolean words “AND”, “OR”, and “NOT” using all [All fields] and [MeSH Terms] searching strategies.
Results
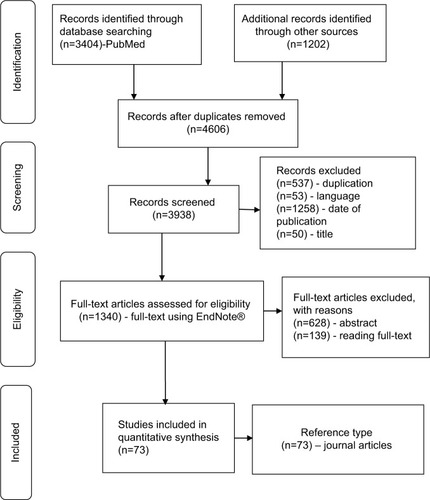
Articles were screened using the title, checked by their abstract, and the remaining related full-text materials were included or excluded by two individuals deciding its eligibility. Finally, 73 materials issued from 2013–2018 were used for qualitatively synthesizing and reconciling the idea to produce this review article.
Conclusion
Poor medical data processing systems are the key reasons for medical errors. Employing standardized data management systems reduce errors and associated sufferings. Therefore, using electronic tools in the health care institution ensures safe and efficient data management. Therefore, it is important to establish appropriate medical data management systems for efficient health care delivery.
Background
The mission of health care institutions – restoring patient’s health – demands effective and efficient medical data for evidence-based intervention.Citation1 Installing an appropriate health care data management system with valid case definition enables efficient data extraction,Citation2 improves communication for clinical decision making in medical practice,Citation2–Citation8 and clinical research,Citation9,Citation10 and upgrades the quality of health care services.Citation11 Healthcare professionals are responsive to improve recording, distributing, monitoring, and implementing preventive measures to decrease morbidity.Citation12 This requires consistent, complete, comprehensive, and accurate information which attracts more attention in the health care industry.Citation3
The health care industry uses a paper-based record (PBR) and/or electronic health record (EHR) system to manage patient’s data. The EHR has become an integral part of medical care,Citation13 which transforms health care service qualityCitation14,Citation15 and improves clinicians’ satisfaction and facilitates patients’ decision.Citation8,Citation16 Accurate information from EHR enables physicians’ order entry and measures clinical validity, which in turn upgrades the quality of patient care.Citation17 This functionality is crucial during diagnosis and therapy,Citation15 which benefits medical and legal practices too.Citation18
Decision-support embedded features – standardized checklists, alert signals, predictive tools, and guidelinesCitation1 – motivate and encourage health care organization leaders and persuade physicians to better utilize best practice alerts (BPAs) in a more effective and efficient way.Citation19 In line with this, research reports backed up a position that health care practices are being transformed from PBR to EHR systems,Citation17 although a report revealed that, in the eye care practice, EHR is less versatile for recording.Citation20
Patient data were readily accessible and transferableCitation21 from the EHR system. This helps to make an accurate diagnosis and decision makingCitation22 by reducing the access time and use.Citation1,Citation2 Notification signal flags or BPAs prompt about “what content” and “with whom” to shareCitation23–Citation25 that trigger potential adverse events (AEs) using easily identifiable displays that alert patient records reviewers.Citation26 This enhances patient’s engagement in health care service provisionCitation27 and decision-making processes,Citation28 as it builds trustCitation29 and confidenceCitation30 that helps to identify specific and actionable adherence barriers.Citation31 In addition, automatic email text and telephone reminders can be sent to patients in order to motivate and maximize patients compliance.Citation32
Poor data management practices are the reasons for recurrent errors and associated injuries or death,Citation33 which is mostly happening due to illegible PBRCitation34 (mistakes in recording or transcribing).Citation35
The EHR application improves the process,Citation36 trustworthiness, safety, and efficiency of patient care delivery.Citation29 Hence, implementing standardized policies, processes, and procedures for an appropriate health care data management system that advances the quality of health services and efficiency,Citation34,Citation37 avoids non-value adding activities,Citation34 and ensures major quality and safety improvement.Citation16,Citation17,Citation23,Citation34 Therefore, this paper intends to indicate the roles of EHR in improving the quality of health care service provisions.
Methods
The keywords identified were EHR, EMR, electronic health record, electronic medical record, medical data recording, medical data processing, medical data retention, medical data destruction, health care, patient care, animal data, and plant data with different combinations. Searching was done using boolean words “AND”, “OR”, and “NOT”.
We used [((EHR OR EHR[MeSH terms]) OR EMR) OR (EMR[MeSH terms]) OR (electronic health record) OR (electronic health record[MeSH terms]) OR (electronic medical record) OR (medical data recording[MeSH terms]) OR (medical data processing) OR (medical data processing[MeSH terms]) OR (medical data retention) OR (medical data retention[MeSH terms]) OR (medical data destruction) OR (medical data destruction[MeSH terms])] AND [((health care) OR (health care)[MeSH terms]) OR (patient care) OR (patient care)[MeSH Terms])] to search articles from PubMed and Google Scholar databases and Google search engine. Information was extracted from downloaded materials and used for qualitative synthesis.
Result
PubMed (National Library of Medicine [NLM]) databases and Google Scholar databases, as well as the Google search engine, were used for downloading published materials using EndNote® Version XCitation5 for Window’s application. Published materials which were searched using the EndNote application were subsequently screened and checked for relevance using titles, abstracts, and full-text articles, which was done by two individuals, independently inspecting for its eligibility. From a total of 4,606 searched published materials, 73 full-text materials issued from 2013–2018 were used for the development of this review after passing the subsequent screening, selections, and checking processes. Information generated from referenced materials was qualitatively synthesized and the idea was reconciled to produce this review article. The overall study selection process is depicted in .
Discussion
Patient health care data management processes
Although the health care industry is an information enterprise, its data recording practices and its data protection laws vary considerably among hospitals and countries.Citation38,Citation39 The overall health care data management policies must define confidentiality and prevent reconstruction after destruction controlled by security personnel.
The document destruction policy must define the medical data retention policy and its codes of practice that must file the advantages and disadvantages of destroying or maintaining medical data.Citation40
The benefits of EHR implementation
Implementing EHR increases the quality of services and ensures the safety of patients upon using decision-support tools result in error reduced services that increase clinicians and patient’s satisfaction, which in turn increases the health care seeking-behavior of clients.
Currently, about 1,000 EHR applications are published every monthCitation42 for the purpose of increasing performance,Citation41,Citation42 reducing fatigue, improving accessibility, ensuring compliance, fidelity, and satisfaction,Citation41,Citation43 with acceptable safety gains.Citation44
The EHR tool was implemented in the United States and the United Kingdom, which own the largest private and public health care systems in the world, respectively, and succeeded in providing quality patient care.Citation45 It is an essential tool for the application of modern information technology that improves the quality of health care servicesCitation46 consistent with medico-legal considerations.Citation18
Accessing the EHR tool facilitates the health care delivery,Citation19,Citation24 made more accurate decisions,Citation22 and contributes to the health care quality improvement and research outputCitation47,Citation48 at reduced cost.Citation49,Citation50 The tool also ensures the safe transfer of health care data that meets the patient’s expectation,Citation51 supports the continuity of patient care,Citation11 and maintains the compliance with medication adherence.Citation52,Citation53 Moreover, the tool helps diabetes goal achievement, while the service delivery process is assisted from non-physician workers.Citation54
The data generated from the EHR measure prevention, process, and outcome metric.Citation55 Implementing high-quality EHR improves epidemic surveillance,Citation56 decreases the length of patient stay,Citation40 achieves work efficiencyCitation33,Citation40 by reducing non-value adding activities,Citation34 achieves goals,Citation3 and helps to make for timely decisions at reduced cost.Citation49,Citation57 The system reduces the nurses and the clerk’s time spent to access data to make timely interventions.Citation1 In its effectiveness, it ensures the quality of services at a reduced cost.Citation58 The potential benefits of EHR are improving quality, ensuring continuity of patient care, efficiency, and positive financial return on investment.Citation50
The effective use of EHR improves the patient’s safety,Citation48 trust, and their satisfaction on the health care system appeared orienting patients towards a health related information sources.Citation59 Patients usually want to control how and what details to be notified when their data are accessed.Citation23 The tools could be customized to notify and ensure the safe transfer of patient private confidential data,Citation33 and they need to get protected.Citation60
The interoperability of medical information among health care institutions increases the medical staff’s understanding of the disease, diagnosis, and decision-making processes.Citation61 The EHR allows automated disease surveillance, and helps in participation and promotion of safe and effective health care practices.Citation56
The challenges of implementing EHR
The EHR is perceived as a “double-edged sword” as it improves quality on the one hand and increases privacy and safety risks on the other hand.Citation34 These are important concerns of patients’ for transferring their health care data.Citation23,Citation33
Although its adoption rate is currently rising, EHR is found at a low rate, particularly in developing countries.Citation46,Citation62,Citation63 Some of the factors for this low adoption rate include behavioral factors (lack of perceived benefits,Citation28 poor confidence,Citation64 dissatisfaction,Citation59 physicians’ resistance,Citation65 lack of stakeholders interest,Citation49 and ignorance on more advanced systems),Citation60,Citation66 technical factors (interoperability,Citation64 lack of financial support or specific financial incentives,Citation49 and lack of technology infrastructure),Citation47 legal factors (lack of legal frameworkCitation64 and lack of comprehensive EHR national policy and strategy),Citation47 socio-demographic factors (age and education level of physicians),Citation59 practice related factors (high skill demandCitation28 and lack of training),Citation67 and knowledge related factors (poor awareness).Citation64
The Delphi study disclosed the barriers of medical practices to implement EHR, as hindered by a myriad of intrinsic (behavioral and cognitive) and extrinsic (economic and technological) barriers when faced with the initial decision to invest in an EMR system.Citation50
Healthcare service at a distance
Traditional telephone services were the milestones of modern telemedicine. Implementing electronic communication applications with high computational power enables the control of operations at a distance possible. Although reducing medical errors is an international agenda, physicians still commit different types of errors during manual medical data processing incurred during recording and/or fail to timely record health care data.Citation35 Errors associated with medical data are common and costly. However, the social, spiritual, psychological, and ethical scopes of the technology, as well as the technical feasibilities of the technology, must be considered, and all stakeholders must contribute while planning and implementing new health care technologies. The PBR systems are practically more error-prone, however, the mere replacement of the system with EHR could not ensure accuracy.Citation34 Hence, efficient processing, usage, and storage of medical data are important for both clinical and public health decisions.
The future perspectives
The promising EHR implementation systems, people, process, and product factors play an integral role in the fate of its implementation.Citation11 The stakeholder’s benefit from the systems which protect the patient’s need and ensure their privacy.Citation24 The access to accurate and complete clinical information is the main component of effective decision making.Citation69 This is facilitated by decision-support EHR tools - BPAs - and designed for behavioral health integration with the needs of health care institutions and the benefits of improving the patient experiences,Citation36 for instance, alcohol use.Citation30 The system can be used to update the current condition of a patient as input to obtain a corresponding recommendation for medical tests, possible diseases, and treatment plans.Citation69 Research indicated that the EHR “active choice” significantly increased influenza vaccination rates and ordering of colonoscopy and mammography screening services.Citation8
The successes or challenges of voice input application can be used to transcribe doctor’s dictation and facilitate the collection, indexation, storage, and retrieval processes of medical information.Citation17 According to a study, EHR promotes services but could not favor collaborative team’s culture and professionals.Citation70
The shift in the use of EHR by the health builds trusts and presents an opportunity to monitor admission, diagnosis, and outcome to inform public health policy and service provision.Citation58 The EHR vendors should be encouraged to incorporate social knowledge networking features into the systems.Citation71
Authors have also identified two issues demanding the researcher’s attention for more elaborated reasons for uncertainties. First, one national level research reported the adoption level of EHR as it was higher in rural practices than urban counterparts, reversing the earlier trends.Citation72 Another similar research also reported the necessity of considering the patient’s behavioral aspects while using the tool during patient rendering procedures so as to increase patient’s engagement level.Citation73 These issues may call for behavioral scientists to address this particular patient concern.
Conclusion
Medical data processing is one of the most basic tasks of the health care professionals. Computerized physician order entry applications having decision-support fields reduce avoidable medical errors using inbuilt memory aid. These automatic notification alert signals enable appropriate and timely intervention that ensures safer and efficient health care. The design policies of electronic technology must meet pre-stated standards and guidelines to ensure confidentiality. User-friendly technologies ensure the efficient and timely transfer of health care data for quality patient care meeting the needs of the patients and the organization.
Author contributions
All authors contributed towards data analysis, drafting and critically revising the paper, gave final approval of the version to be published and agree to be accountable for all aspects of the work.
Abbreviations
| AEs | = | adverse events |
| BPAs | = | best practice alerts |
| EHR | = | electronic health record |
| EMR | = | electronic medical record |
| NLM | = | National Library of Medicine |
| PBR | = | paper-based record |
Disclosure
The authors report no conflicts of interest in this work.
References
- TierneyWMSidleJEDieroLOAssessing the impact of a primary care electronic medical record system in three Kenyan rural health centersJ Am Med Inform Assoc201623354455226260246
- XuYLiNLuMDevelopment and validation of method for defining conditions using Chinese electronic medical recordBMC Med Inform Decis Mak201616111027542973
- WeirCRStaggersNGibsonBA qualitative evaluation of the crucial attributes of contextual information necessary in EHR design to support patient-centered medical home careBMC Med Inform Decis Mak20151513025881181
- WeberGMKohaneISExtracting Physician Group intelligence from electronic health records to support evidence based medicinePLoS One201385e6493323734227
- HalpernYHorngSChoiYSontagDElectronic medical record phenotyping using the anchor and learn frameworkJ Am Med Inform Assoc201623473174027107443
- LakinJRIsaacsESullivanEEmergency physicians’ experience with advance care planning documentation in the electronic medical record: useful, needed, and elusiveJ Palliat Med201619663263827203483
- BookmanKWestDGindeAEmbedded clinical decision support in electronic health record decreases use of high-cost imaging in the emergency department: embed studyAcad Emerg Med201724783984528391603
- PatelMSVolppKGSmallDSUsing active choice within the electronic health record to increase influenza vaccination ratesJ Gen Intern Med201732779079528337690
- Aref-EshghiEOakeJGodwinMIdentification of dyslipidemic patients attending primary care clinics using electronic medical record (EMR) data from the Canadian primary care sentinel surveillance Network (CPCSSN) databaseJ Med Syst20174134528188559
- DeshazoJPHoffmanMAA comparison of a multistate inpatient EHR database to the HCUP nationwide inpatient sampleBMC Health Serv Res201515138426373538
- JawhariBKeenanLZakusDBarriers and facilitators to electronic medical record (EMR) use in an urban slumInt J Med Inform20169424625427573333
- VieiraDSSantosNCCostaDKRecording actions to prevent child morbidity in children’s health cardsCien Saude Colet20162172305231327383363
- VaughnVMLinderJAThoughtless design of the electronic health record drives overuse, but purposeful design can nudge improved patient careBMJ Qual Saf2018278583586
- TweyaHFeldackerCGadabuOJDeveloping a point-of-care electronic medical record system for TB/HIV co-infected patients: experiences from Lighthouse trust, Lilongwe, MalawiBMC Res Notes20169114626945749
- ZhangXYZhangPRecent perspectives of electronic medical record systemsExp Ther Med20161162083208527284289
- WalkerEMcmahanRBarnesDKatenMLamasDSudoreRAdvance care planning documentation practices and accessibility in the electronic health record: implications for patient safetyJ Pain Symptom Manage201855225626428943360
- ZengXThe impacts of electronic health record implementation on the health care workforceN C Med J201677211211426961833
- SiegelDMKinscherffRRecording routine forensic mental health evaluations should be a standard of practice in the 21st centuryBehav Sci Law201836337338929696698
- ChenHButlerEGuoYFacilitation or hindrance: physicians’ perception on Best Practice Alerts (BPA) Usage in an Electronic Health Record SystemHealth Commun2018217
- WolffsohnJSNarooSAChristieCAnterior eye health recordingCont Lens Anterior Eye201538426627125814427
- SungSFChenKWuDPApplying natural language processing techniques to develop a task-specific EMR interface for timely stroke thrombolysis: a feasibility studyInt J Med Inform201811214915729500013
- Ben-AssuliOSagiDLeshnoMIroniAZivAImproving diagnostic accuracy using EHR in emergency departments: a simulation-based studyJ Biomed Inform201555314025817921
- CaineKKohnSLawrenceCDesigning a patient-centered user interface for access decisions about EHR data: implications from patient interviewsJ Gen Intern Med201530S1716
- BlumenthalDSquiresDGiving patients control of their EHR dataJ Gen Intern Med201530S14243
- MilneHHubyGBuckinghamSDoes sharing the electronic health record in the consultation enhance patient involvement? A mixed-methods study using multichannel video recording and in-depth interviews in primary careHealth Expect201619360261625523361
- MarghamTSymesNHullSAUsing the electronic health record to build a culture of practice safety: evaluating the implementation of trigger tools in one general practiceBr J Gen Pract201868669e279e28529530919
- El MiedanyYEl GaafaryMEl AroussyNToward electronic health recording: evaluation of electronic patient reported outcome Measures (e-PROMs) system for remote monitoring of early systemic lupus patientsClin Rheumatol201736112461246928567555
- HunterEGCapsule commentary on Lee et al., patient perceptions of electronic medical record use by faculty and resident physicians: a mixed methods studyJ Gen Intern Med20163111135527435253
- OzairFFJamshedNSharmaAAggarwalPEthical issues in electronic health records: a general overviewPerspect Clin Res201562737625878950
- HaroonSWooldridgeDHoogewerfJInformation standards for recording alcohol use in electronic health records: findings from a national consultationBMC Med Inform Decis Mak20181813629879953
- ZulligLLCurtisLHA population health perspective on a claims and electronic health record-based tool to screen for suboptimal medication adherenceAm Heart J201819715015229447775
- JosephCLOwnbyDRZorattiERecruitment experience for a pragmatic randomized controlled trial: using EMR initiatives and minimizing research infrastructureClin Res Regul Aff2016332–4253228479846
- EmbiPJWeirCEfthimiadisENComputerized provider documentation: findings and implications of a multisite study of clinicians and administratorsJ Am Med Inform Assoc201320471872623355462
- AjamiSBagheri-TadiTBarriers for adopting electronic health records (EHRs) by physiciansActa Inform Med201321212913424058254
- HripcsakGAlbersDJNext-generation phenotyping of electronic health recordsJ Am Med Inform Assoc201320111712122955496
- JetelinaKKWoodsonTTGunnREvaluation of an electronic health record (EHR) tool for integrated behavioral health in primary careJ Am Board Fam Med201831571272330201667
- TopMYilmazAKarabulutEValidation of a nurses’ views on electronic medical record systems (EMR) questionnaire in Turkish health systemJ Med Syst20153966725957164
- LujicSWatsonDERandallDASimpsonJMJormLRVariation in the recording of common health conditions in routine hospital data: study using linked survey and administrative data in New South Wales, AustraliaBMJ Open201449e005768
- VivantiADalyAImportant privacy considerations with electronic health record documentationNutr Diet201875333733829124874
- YangPCaoYLiuDBaiYPanFXuYThe effect of electronic medical record application on the length of stay in a Chinese General Hospital: a department- and disease-focused interrupted time-series studyJ Med Syst20143855324760225
- WoodsSSEvansNCFrisbeeKLIntegrating patient voices into health information for self-care and patient-clinician partnerships: veterans affairs design recommendations for patient-generated data applicationsJ Am Med Inform Assoc201623349149526911810
- KimSLeeK-HHwangHAnalysis of the factors influencing healthcare professionals’ adoption of mobile electronic medical record (EMR) using the unified theory of acceptance and use of technology (UTAUT) in a tertiary hospitalBMC Med Informat Decis Making201516112
- van DrongelenABootCRHlobilHSmidTvan der BeekAJProcess evaluation of a tailored mobile health intervention aiming to reduce fatigue in airline pilotsBMC Public Health201616189427565140
- FernandoBMorrisonZKalraDCresswellKSheikhAApproaches to recording drug allergies in electronic health records: qualitative studyPLoS One201494e9304724740090
- WilsonKKhansaLMigrating to electronic health record systems: a comparative study between the United States and the United KingdomHealth Policy2018122111232123930193980
- ZayyadMAToycanMFactors affecting sustainable adoption of e-health technology in developing countries: an exploratory survey of Nigerian hospitals from the perspective of healthcare professionalsPeerJ201866e443629507830
- CowieMRBlomsterJICurtisLHElectronic health records to facilitate clinical researchClin Res Cardiol2017106119
- Sayyah GilaniMIranmaneshMNikbinDZailaniSEMR continuance usage intention of healthcare professionalsInform Health Soc Care201742215316527100821
- YoshidaYImaiTOheKThe trends in EMR and CPOE adoption in Japan under the National strategyInt J Med Inform201382101004101123932755
- ParéGRaymondLde GuineaAOBarriers to organizational adoption of EMR systems in family physician practices: a mixed-methods study in CanadaInt J Med Inform201483854855824969270
- BurneyAAbbasZMahmoodNArifeenQ-UlProspects for mobile health in Pakistan and other developing countriesAIT201303022732
- BaconTSFanKCDesaiMAElectronic medical record and glaucoma medications: connecting the medication reconciliation with adherenceClin Ophthalmol20161022122526869756
- Yeboah-KorangABeigMIKhanMQHepatitis C screening in commercially insured U.S. birth-cohort patients: factors associated with testing and effect of an EMR-based screening alertJ Transl Int Med201862828929984203
- SinghKJohnsonLDevarajanRAcceptability of a decision-support electronic health record system and its impact on diabetes care goals in South Asia: a mixed-methods evaluation of the CARRS trialDiabetic Med201835121644165430142228
- ChoIBooEHLeeSYDykesPCAutomatic population of eMeasurements from EHR systems for inpatient fallsJ Am Med Inform Assoc201825673073829659868
- ZhengHGaffHSmithGDelisleSEpidemic surveillance using an electronic medical record: an empiric approach to performance improvementPLoS One201497e10084525006878
- LeightleyDChuiZJonesMIntegrating electronic healthcare records of armed forces personnel: developing a framework for evaluating health outcomes in England, Scotland and WalesInt J Med Inform2018113172529602429
- Bar-DayanYSaedHBoazMUsing electronic health records to save moneyJ Am Med Inform Assoc201320e1e17e2023462876
- de RosisSBarsantiSPatient satisfaction, e-health and the evolution of the patient-general practitioner relationship: evidence from an Italian surveyHealth Policy2016120111279129227836231
- de PietroCFranceticIE-health in Switzerland: the laborious adoption of the federal law on electronic health records (EHR) and health information exchange (HIE) networksHealth Policy20181222697429153922
- TranBLeXNguyenPFeasibility of e-health interventions on smoking cessation among Vietnamese active Internet usersInt J Environ Res Public Health2018151165
- AlanaziAIncorporating pharmacogenomics into health information technology, electronic health record and decision support system: an overviewJ Med Syst20174121927987157
- WhitacreBEThe influence of the degree of rurality on EMR adoption, by physician specialtyHealth Serv Res201752261663327256561
- TavazziLVenturaC“Observational medicine”: registries and electronic health recording for science and health systems governanceEur J Heart Fail20161891093109527594174
- BarrettAKElectronic health record (EHR) organizational change: explaining resistance through profession, organizational experience, and EHR communication qualityHealth Commun201833449650628157382
- TrudelM-CMarsanJParéGCeiling effect in EMR system assimilation: a multiple case study in primary care family practicesBMC Med Inform Decis Mak20171714628427405
- PantaleoniJLStevensLAMailesESGoadBALonghurstCASuccessful physician training program for large scale EMR implementationAppl Clin Inform201561809525848415
- MohanVSchollGGoldJAUse of EHR-based simulation to diagnose aetiology of information gathering issues in struggling learners: a proof of concept studyBMJ Simul Technol Enhanc Learn2018429294
- ZhaoCJiangJGuanYGuoXHeBEMR-based medical knowledge representation and inference via Markov random fields and distributed representation learningArtif Intell Med201887495929691122
- ZhaoJYKesslerEGGuoWATemporary removal: interprofessional communication goes up when the electronic health record goes downJ Surg Educ EpubSept232018
- RangachariPImplementing a social knowledge networking (SKN) system to enable meaningful use of an EHR medication reconciliation systemRisk Manag Healthc Policy201811455329618941
- WhitacreBERural EMR adoption rates overtake those in urban areasJ Am Med Informat Assoc2015222399408
- StreetRLLiuLFarberNJKeystrokes, mouse clicks, and Gazing at the computer: how physician interaction with the EHR affects patient participationJ Gen Intern Med201833442342829188544