Abstract
Background
It is necessary to investigate the effects of physical activity (PA) on the recovery of adults and the elderly, considering PA positively affects pathologies that share similarities with COVID-19. We present the results of a systematic review whose objective was to analyze the physical, functional, psychological, and social effects of PA in adults and the elderly during and/or after hospitalization for COVID-19.
Methods
Searches were conducted between July and August 2021, following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. Randomized clinical trials (RCTs) and non-randomized interventional studies were included in the databases: PubMed, Web of Science, Scopus, EBSCOhost, Science Direct, Cochrane Library, Physiotherapy Evidence Database (PEDro), and electronic search engines. Study quality was assessed using the PEDro for RCTs and the methodological index scale for non-randomized studies. This systematic review included original articles investigating the physical, functional, psychological, and social effects of any PA program on adults and older adults.
Results
A total of 302 studies were found. After applying filters according to the eligibility criteria, five studies were finally included for analysis, three RCTs and two intervention studies without a control group. Although the studies measured different variables of the physical, functional, and psychological components, the results showed significant differences in the variables between the control and intervention groups in both the RCTs and the single-group studies. The variables assessed in the social aspect were less homogeneous.
Conclusion
In the available scientific evidence, respiratory muscle training was the most widely used intervention, which showed positive results in the physical, pulmonary, psychological, and social components. More research is required on the effects of PA on the population studied.
Introduction
In December 2019, an outbreak of acute respiratory disease characterized by fever, dry cough, and shortness of breath began in Wuhan (People’s Republic of China). Weeks later, a novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing coronavirus disease 2019 (COVID-19) was identified.Citation1 The disease evolves similarly to the influenza virus, with general pain, sputum, weakness, and headache.Citation2 However, in other cases, several risk factors are associated with COVID-19 complications and mortality, including chronic respiratory disease (8.0%), cardiovascular disease (13.2%), hypertension (8.4%), diabetes (9.2%), and cancer (7.6%).Citation3–6 In addition to the aforementioned, some people experience psychological symptoms such as irritability, anxiety, depression, and sleep disorders, among others.Citation7
The severity of the disease depends mainly on the immune system and age of the infected individual, where most (86.6%) of the patients with confirmed cases are between the ages of 30 and 79 years. Also, patients aged >65 years tend to present a worse prognosis and may need between 7 and 11 days of hospitalization, intensive care, or a ventilator to help them breathe.Citation8,Citation9 All the above make older adults’ infection forecasts even higher than the rest due to the comorbidity, geriatric syndromes, and frailty associated with aging.Citation10
The confinement to contain the COVID– 19 outbreak increased sedentary time and altered life habits, mainly in older adults. Similarly, during and after the COVID-19 infection, patients of this age group decrease their physical activity (PA) levels, bringing with them a general physical condition in general, such as aerobic capacity, loss of muscle mass, and strength.Citation11 This leads to a decrease in the autonomy and functionality of people, affecting their well-being and quality of life (QoL) even after illness.Citation7,Citation12
Because COVID-19 is a multisystem disease that, in some cases, can affect different organs and functions, its approach and treatment must be interdisciplinary. The early initiation of a structured and adapted PA program, in accordance with the patient’s age, fitness levels, previous comorbidities, and disease severity, contributes to improvement in cognitive, respiratory, neuromuscular, and osteoarticular function.Citation13,Citation14 It also reduces the clinical sequelae, restores functional capacity, and, above all, shortens the length of stay in the intensive care unit (ICU).Citation13,Citation14
It is necessary to investigate the favorable effects of PA and physical exercise (PE) on the recovery of these patients, considering that there is sufficient evidence that protective factors against noncommunicable diseases are established through these interventions. Additionally, PA and PE positively affect multiple pathologies that share similarities in terms of symptoms and their possible pathogenic mechanisms.Citation15
Non-pharmacological interventions, such as PE and pulmonary rehabilitation, are effective in patients with chronic obstructive pulmonary disease and are currently used in patients with COVID-19.Citation16 For example, respiratory muscle training is performed to decrease the incidence of COVID-19 symptoms and improve dyspnea, exercise capacity, and, thus, QoL.Citation16 In addition, relaxation exercises are implemented to manage anxiety and sleep problems. Economic interventions are also used because they do not require any technology or special equipment.Citation17–20 Moreover, PA and PE have a positive effect on both mental health and physical health.Citation21
Therefore, this systematic review aimed to analyze the available scientific evidence regarding the effects of a PA program on adults and older adults during and after hospitalization for COVID-19.
Materials and Methods
This review was registered in the “International Prospective Register of Systematic Reviews” (PROSPERO; registration number, CRD42021267517).
The approach to reporting the systematic review was in line with the PRISMA.Citation22 The study evidence quality for RCTs was evaluated using data derived from the Physiotherapy Evidence Database (PEDro) as it provides information resources to support evidence-based clinical practice.Citation23 The methodological index for non-randomized studies (MINORS) scale was used for intervention studies.Citation24
Below is the PICOS strategy used in the review:
Population: Patients aged >18 years who were hospitalized for COVID-19.
Intervention: Intervention studies that incorporated programs of PA, PE, physical therapy, or pulmonary rehabilitation in patients during or after hospitalization for COVID-19.
Comparison: Patients who followed the usual medical care.
Result: Physical effects (dyspnea, fatigue, the 6-minute walk test), functional effects (pulmonary function test forced expiratory), psychological effects (anxiety, sleep quality and depression), and social effects of a PA program in adults and older adults (activities of daily living and quality of life).
Study design: Randomized clinical trials and intervention studies.
Research question: What are the effects of a PA program on adults and older adults during and after hospitalization for COVID-19 for physical effects, psychological effects, and social effects?
Information Sources and Searches
The systematic review was performed from July to August 2021 in nine databases and electronic search engines: PubMed, Web of Science, Scopus, EBSCOhost, Science Direct, Cochrane Library, PEDro, SciELO, and Google Scholar. In addition, the exact keywords were combined with Boolean operators (ie, AND and OR) and Medical Subject Heading (MeSH) terms centered on the title and abstract. Updated literature in Spanish, English, and Portuguese was considered without specifying the publication date. We selected the studies that included patients aged >18 years who were hospitalized for COVID-19 and intervention studies that incorporated programs of PA, PE, physical therapy, or pulmonary rehabilitation in patients during or after hospitalization for COVID-19. The main reasons for exclusion in the systematic review were as follows: gray or unconventional literature and specific COVID-19 studies without PA programs or containing programs with passive gymnastics, management guidelines for COVID-19, or recommendations for PA during the COVID-19 pandemic.
The search strategy was adapted to the characteristics of each of the search engines. We used the following keywords: COVID, SARS, coronavirus, SARS-CoV-2, physical activity, physical exercise, aerobic capacity, resistance training, aerobic exercise, therapeutic exercise, physical therapy, physiotherapy, physical rehabilitation, respiratory rehabilitation, and pulmonary rehabilitation. For example, the Cochrane database used the following strategy: “(‘physical activity’ OR ‘physical exercise’ OR ‘aerobic capacity’ OR ‘resistance training’ OR ‘aerobic exercise’ OR ‘fitness’ OR ‘therapeutic exercise’ OR ‘physical therapy’ OR ‘physical rehabilitation’ OR ‘respiratory rehabilitation’ OR ‘pulmonary rehabilitation’ OR physiotherapy):ti AND (‘Covid’ OR ‘SARS’ OR ‘coronavirus’ OR ‘SARS-CoV-2’):ti.” The authors performed a reference review of the definitive studies, where a study was included for the analysis. The complete strategy of all search engines is shown in Supplementary Table 1.
Selection of Studies
Two authors independently exported the search engine results to an online reference manager (EndNote version 18.2.0.13302). Here, the duplicate studies were automatically deleted. Subsequently, the reviewers removed those duplicates not detected by the program through a detailed manual inspection. Discrepancies between evaluators were resolved by mutual agreement or by a third evaluator. The titles and abstracts were reviewed, verifying each article’s inclusion and exclusion criteria. Then, a complete reading of the remaining studies was performed, and by consensus, the final list of studies included in the review was selected.
Data Extraction and Quality Assessment
Two investigators independently extracted the following data using an Excel form: characteristics of the studies, characterization of the population, demographic data of the participants, methodology of the study, details of the intervention, outcomes of interest, and monitoring and analysis of the results ().
Table 1 Characteristics of the Included Studies
PEDroCitation23 was used to determine the quality of RCTs, which helps users quickly assess whether studies have sufficient internal validity and the statistical information necessary for their results to be interpretable. Non-randomized intervention studies were evaluated with the MINORS scale,Citation24 determining whether the studies had sufficient quality to be included in reviews. Any disagreement was resolved through discussion by the authors.
Data Analysis
Because of the limited number of studies, diversity of variables analyzed, and use of different scales for evaluating the same variable, the authors analyzed the data descriptively, using numbers, means, percentage distributions, standard deviations, and frequencies.
Results
Characteristics of Intervention Studies
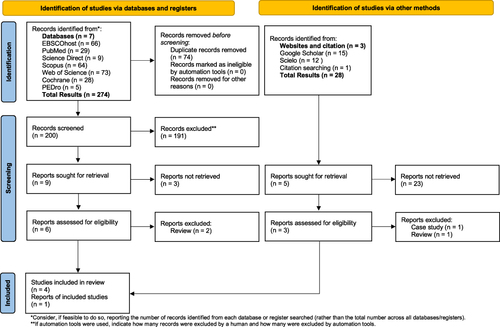
After a comprehensive search of the literature on our topic of interest, 302 titles were identified for inclusion. Of these, 274 titles were identified in seven databases and 28 titles through other search methods. For the selection of our studies, 74 automatically duplicated titles were discarded. The titles and abstracts were then reviewed, eliminating 191 studies that did not meet the eligibility criteria. Subsequently, six studies were evaluated through a full-text review, where four studies were included in the review. Using other search methods, an article was found to obtain five studies for the review. There were three RCTsCitation25–27 and two intervention studies without a control group (CG)Citation28,Citation29 (). The review of an institutional ethics board was not necessary for the research.
Figure 1 Flow diagram showing the number of studies identified and selected for inclusion in the systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020.
Characteristics of Participants
The studies included 254 patients, all diagnosed with COVID-19. The distribution by sex was 58.7% for men, and the mean age of the whole sample was 51.7±10.4 years. At follow-up, 96.2% of the population completed the intervention. In RCTs, the exercise group and CG did not differ in the baseline characteristics of the participants. Only two studies reported clinical symptoms,Citation25,Citation28 the most relevant being fever, cough with sputum, fatigue, and dyspnea. Three studies reported a previous history of disease,Citation26–28 such as hypertension, diabetes, osteoporosis, cancer; previous hospitalization; and engaging in regular exercise prior to infection. Neither of the participants of studies included reported clinical complications. The complete details of the features are shown in .
Description of the Intervention
Sessions were performed twice a day in the studies of,Citation25,Citation27,Citation28 once a day in the study of,Citation29 and twice a week in the study of,Citation26 where an additional respiratory rehabilitation session was performed per day. The intervention time was 5 days in the studies ofCitation25,Citation27 and 3–6 weeks in the studies of.Citation26,Citation28,Citation29 The duration of each session ranged from 20 to 30 min for the studies, except for the study of,Citation26 which did not specify. Several studies included respiratory muscle training,Citation26,Citation28,Citation29 followed by relaxation techniques also used in three studies,Citation25,Citation27,Citation28 two of which used accompaniment with music to obtain better results.Citation27,Citation28
Three studiesCitation26,Citation28,Citation29 evaluated the physical, lung function, psychological, and social components. However, one studyCitation28 did not include the lung function results. Two studiesCitation25,Citation27 evaluated only the psychological component.
Primary Outcomes
The primary outcomes were anxiety and sleep quality, which were assessed in most results 80% and 60%, respectively.
Anxiety
Four studiesCitation25–27,Citation29 evaluated anxiety using different scales: Spielberger State-Trait Anxiety Inventory used in two studies,Citation25,Citation27 Self-Rating Anxiety Scale (SAS) used in two studies,Citation26,Citation27 Trait Anxiety Scale used in one study,Citation27 and Hamilton Anxiety Rating Scale used in one study.Citation29 The results of all studies were statistically significant within the intervention group, and in the three RCTs,Citation25–27 they were statistically significant compared with those in the CG (P < 0.05).
Sleep Quality
Sleep quality was investigated in three studiesCitation25,Citation27,Citation28 using different scales: Sleep State Self-Rating Scale used in one study;Citation25 Richards–Campbell Sleep Questionnaire used in one study;Citation27 and sleep quality used in one study,Citation28 which was evaluated through three questions “sleep well”, “wake up two to three times at night”, and “do not sleep.” Two studiesCitation25,Citation27 presented statistically significant results after the intervention (P < 0.05), and in one studyCitation28 in the items “good” and “wake up one to two times a night”, the results were also statistically significant after the intervention (P < 0.0001).
Secondary Outcomes
Two studies each evaluated the following variables, representing 40% of the total studies.
The 6-Minute Walk Test
Two studiesCitation26,Citation29 evaluated the 6-min walk test (6MWT), which reported significant differences before and after the intervention (P = 0.020). OneCitation26 of these studies also showed statistically significant results compared with those in the CG.
Dyspnea
Two prospective intervention studiesCitation28,Citation29 evaluated dyspnea, showing highly significant results between before and after the exercise intervention (P < 0.0001 and P = 0.022, respectively).
Depression
Two studies evaluated depression. The study ofCitation26 used the Self-Rating Depression Scale, which did not report statistically significant results within and between groups. On the other hand, the study ofCitation29 used the Hamilton Depression Rating Scale, which showed statistically significant results in the intervention group (P = 0.0032).
Quality of Life
Two studiesCitation26,Citation29 measured the QoL through the short form – 36 health survey (SF-36). In the study of,Citation26 the scores in the eight dimensions were statistically significant between the intervention group and the two groups (P < 0.05). In the study of,Citation29 only two dimensions presented significant results after the intervention: physical functioning (P = 0.014) and role-physical (P = 0.009).
Activities of Daily Living
Two studiesCitation26,Citation28 analyzed the activities of daily living (ADLs) endpoint. In the study of,Citation26 no significant improvement was noted either within the intervention group or between the intervention group and CG. On the other hand, in the study of,Citation28 significant improvement was observed only in the intervention group (P< 0.0001).
Quality Assessment
The quality of three randomized studiesCitation25–27 was evaluated using PEDro.Citation23 On the other hand, two studiesCitation28,Citation29 were reviewed using the MINORS scale because these were intervention studies and, thus, could not be evaluated using the same criteria.Citation24
The PEDro helps users quickly identify whether RCTs have sufficient internal validity (criteria 2–9) and statistical information necessary for their results to be interpretable (criteria 10–11). The studies not in the PEDro were reviewed through independent, rigorous reading by the reviewers. The results were recorded in a spreadsheet where “Yes” or “No” was written if the study met or did not meet the criteria established by the PEDro. Any disagreement was resolved through discussion. presents the elements selected for methodological evaluation according to the PEDro criteria and all complete information of the quality assessment.
Table 2 Quality of the Studies Included in the Review Using the PEDroCitation23
The studies ofCitation25–27 presented initial comparability, good follow-up, comparison between groups, and point estimates and variability. None of the studies had concealed allocation, blind subjects, blind therapists, blind assessors, and intention-to-treat analysis, which are common in the PEDro. shows that the studies ofCitation25–27 met the same criteria of the PEDro, except for that of.Citation26 Random allocation was met by approximately 97% of the studies in this database. The items concealed allocation, blind subjects, blind therapists, blind assessors, and intention-to-treat analysis that were not satisfied in any of the studies were reported in 27%, 6%, 1%, 36%, and 28% of the studies in the PEDro. The mean PEDro score was 5.1 ± 1.6, and the quality of the studies included in this review had a mean of 4.6 ± 0.57, classifying the studies as regular quality, which could hinder the development of the review.Citation23 Finally, these studies performed intragroup and intergroup comparisons.
For non-randomized studies,Citation28,Citation29 the MINORS scale was used, which is a list containing eight essential points: at least one explicit research aim, information about the inclusion of consecutive patients, prospective data collection, appropriate assessment for the research goal, impartial evaluation of the endpoints, significant follow-up period, loss to follow-up not exceeding 5%, and prospective calculation of the sample size. The score of each section ranged from 0 to 2 depending on the quality (0, uninformed appearance; 1, inadequately informed appearance; and 2, adequately informed appearance). The overall assessed score was according to the following quality parameters, with 16 being the ideal score: 0–4, low quality; 5–10, medium quality; and 11–16, high quality.Citation24 These data are presented in .
Table 3 Methodological Items for Non-Randomized Studies Using the MINORS ScaleCitation24
The studies ofCitation28,Citation29 presented similar characteristics; did not report on the impartial evaluation of the results, rates of abandonment of the follow-up, and prospective sample size estimation; and adequately reported other points. The total score of the MINORS scale for each of these studies was 10, ranking studies with medium quality.Citation24
Effect According to the Type of Intervention
Relaxation Exercises
Two studiesCitation25,Citation27 included relaxation exercises in their intervention, which only evaluated anxiety and sleep problems. The study ofCitation25 used Jacobson’s technique, which consisted of muscle contraction–distension, that is, contracting a muscle or a group of muscles for a few seconds and then loosening the contraction progressively. As such, Jacobson argued that if muscle tension is accompanied by anxiety, the individual can reduce the anxiety by learning to relax that muscle tension, decreasing almost entirely the muscle contractions and experiencing a feeling of relaxation. Jacobson’s technique remains one of the most commonly used techniques to reduce anxiety and stress worldwide.Citation30 This study evaluated anxiety and sleep problems; both variables obtained statistically significant post-intervention results (P< 0.05).
The study ofCitation27 performed an intervention of progressive relaxation exercises accompanied by music during the sessions. As in the previous study, progressive muscle relaxation is a deep relaxation technique based on the principle that muscle tension is a physiological response of the human body to disturbing thoughts. This technique leads to voluntary and regular relaxation of the main muscle groups and, thus, relieves the whole body.Citation27 In addition, the music component facilitates the process and could affect the reduction of anxiety, improve the QoL, relieve stress, and even facilitate social integration.Citation31 In this study, it effectively reduced and improved the anxiety and sleep problems in patients with COVID-19 (P<0.05).
Respiratory Muscle Training
Three studiesCitation26,Citation28,Citation29 included respiratory muscle training in their intervention. The first studyCitation26 included pulmonary resistance, cough, stretching, and home breathing exercises in its program. The following variables were analyzed: 6MWT, forced expiratory volume in 1s (FEV1), forced vital capacity (FVC), FEV1/FVC, diffusing capacity of the lungs for carbon monoxide (DLCO), SAS, and QoL, where statistically significant differences were found between and compare to CG before and after the intervention (P<0.05). On the other hand, no statistically significant differences were noted in the depression and ADL variables.
The study of,Citation28 as in the previous one, included the combination of respiratory muscle training and psychological intervention, in which the patient listened to light music daily. The physical components fatigue, dyspnea, and oxygen saturation showed statistically significant post-intervention results (P=0.003, P<0.0001, and P=0.004, respectively). The psychological components sleep problems and ADLs also showed highly statistically significant results (P < 0.0001).
The study ofCitation29 used Liuzijue’s technique in their intervention, which consisted of the coordination and combination of movements and breathing patterns with specific sounds: Xu, He, Hu, Si, Chui, and Xi. In this study, different components were assessed and showed statistically significant post-intervention results: the physical components 6MWT (P=0.020) and dyspnea (P=0.022), pulmonary function components maximal inspiratory pressure and peak inspiratory flow (P<0.001), and psychological components anxiety (P<0.001) and depression (P=0.0032). No statistically significant results were noted in the social component QoL.
Discussion
Here, we describe the results derived from the systematic review of the physical, functional, psychological, and social effects of PA in adults and older adults during or after hospitalization for COVID-19. This systematic review included five studies, three RCTs, and two non-randomized intervention studies according to eligibility criteria. We found that there were a limited number of studies registered in the seven databases and two search engines and the references cited at the time of systematic review. We considered that the small number of intervention studies was due to the novelty of COVID-19 and the limited knowledge regarding SARS-CoV-2, the disease and its effects, and, indeed, both physical and psychosocial treatments for patients. To organize this section, the results of the physical and functional variables are discussed first, followed by the results of the psychological and social variables.
The studies reviewed included relatively few physical variables, 6MWT and dyspnea, measured by two studies. Both variables showed significant results in the post-intervention groups. These variables are essential in rehabilitation after hospital discharge for COVID-19. In this regard, the study ofCitation32 was conducted in an Italian population that measured dyspnea and the 6MWT. Here, the patients presented with dyspnea and shortness of breath even when performing minimal activities. In addition, only a small percentage of patients could perform the 6MWT, resulting in low performance after discharge from the ICU.
For this reason, this study concluded that patients should be placed in a rehabilitation unit once they leave the ICU, for which an early rehabilitation protocol adapted to these patients would be proposed. Similarly, another studyCitation33 highlighted the need to follow-up patients with hospital discharge. This study evaluated the benefits of the 6MWT and concluded that this test is pertinent because it is correlated with COVID-19 severity and functional impairment and can be used to determine improvement in exercise capacity.
Regarding the variables of lung function, the COVID-19 particularly affects lung function, given that in moderate and severe cases, it causes acute respiratory syndrome. However, few studies evaluated variables such as FEV1, FVC, and DLCO.Citation26 This finding is important considering that current scientific evidence shows that PA and PE are protective factors for multiple diseases and coronavirus-like symptoms.Citation15
One study found improvement in dyspnea and respiratory muscle strength at the level of specific respiratory muscle training. The study estimated aerobic fitness, generating statistically significant changes for the intervention in maximal oxygen consumption (VO2 max).Citation34
The systematic review of the literature on the psychological effects of PA in adults and older adults during or after hospitalization for COVID-19 is limited; however, there is evidence of a reduction in the levels of physical activity in these patients, leading to an increase in post-pandemic sedentary lifestyle.Citation35 This result may be related to the limited knowledge of the disease study in the psychological, physical, functional, and social fields. However, the studies reviewed showed the actual results concerning the psychological effects in three variables: anxiety, sleep problems, and depression.Citation36 Of these variables, the most frequently evaluated is anxiety, followed by sleep problems. Overall, the studies reviewed showed statistically significant results in the intervention group, especially for anxiety and sleep problems. On the other hand, the results for depression were heterogeneous.
Psychological conditions during and after COVID-19 have been identified, where patients report higher anxiety and depression levels than health professionals and the general population.Citation37 Similarly, a literature reviewCitation38 concludes that the COVID-19 pandemic has affected the population’s mental health, particularly hospitalized patients with notable symptoms of anxiety, depression, and sleep disorders. These can be associated with psychosocial components, including the isolation that patients with COVID-19 experience and the series of uncertain situations resulting from a novel virus, which are related to negative emotions such as the fear of death that, in some cases, can lead to anxiety before death.
Symptoms of anxiety and depression in patients with COVID-19 may be associated with the inflammatory process and release of cytokines due to the multisystem disease. Similarly, the effects of psychological and physical stresses experienced by patients may be related to the activation of the hypothalamic–pituitary–adrenal axis.Citation39 One studyCitation40 found that in diseases with some characteristics similar to COVID-19, such as SARS and Middle East Respiratory Syndrome (MERS), patients had psychological deterioration even 6 months after discharge from hospitalization.
The effects of COVID-19 on mental health in patients hospitalized for this disease and in the general population reported in the aforementioned studies highlight the need for further research to investigate possible treatments for patients’ mental health during and after hospitalization for COVID-19. The studies discussed in this systematic review provide information on the positive effects of the different interventions on mental health, specifically in the reduction of anxiety and improvement of sleep problems: relaxation exercises such as Jacobson’s technique, progressive muscle relaxation, Liuzijue’s technique, and breathing muscle training. Additionally, it is essential to highlight the use of music as a form of psychological intervention in the patients who participated in the studies. Overall, these significant results can be associated with pre-COVID-19 pandemic scientific evidence confirming the positive effects of PE on mental healthCitation41 and more recent studies interested in investigating mental health and PA in the general population during the COVID-19 quarantine.Citation42
In comparison with the psychological results, the social results of the studies included in this systematic review were more heterogeneous. In one study with a single group, significant improvement in the ADL variable was evident, whereas in another, no differences were noted between the control and experimental groups. These results suggest the need for further studies about the effects of PA on the social components, such as ADLs. A study found that there is improvement in mental health, quality of life, and function even with low volumes of exercise per day. However, the studies had heterogeneous aspects in the dosage of exercise, and it is recommended to continue with the intervention processes in this area.Citation43
Some studies also had heterogeneous results regarding the effects of PA on QoL. One studyCitation26 presented significant results in all eight QoL dimensions, whereas anotherCitation29 found that only two of them had significant results. Regarding this variable, the systematic review ofCitation40 found that 1 year after discharge, patients hospitalized for other viruses similar to COVID-19 had not resumed their working life level. These authors consider that one of the reasons why social life after the disease is affected could be related to symptoms such as fatigue that people who were infected continue to experience. Although it was not a direct objective of this review, it is estimated that between 10 and 20% of patients with SARS-CoV-2 present post-COVID-19 syndrome. These patients go through an acute symptomatic phase and experience the effects of the disease well beyond 12 weeks after diagnosis. Exercise is an adjuvant to stimulate the immune system by inducing mitochondrial adaptations, cell generation, and immune surveillance.Citation15
Limitations
This review of literature has some limitations. First, the scientific evidence available at the time of systematic review was limited. Second, the studies reviewed included a few physical and functional variables. Therefore, further research is needed on the effects of PA in the studied population and, in particular, RCTs.
Conclusion
This review of literature found that men had the highest incidence of COVID-19 (58.7%), which is consistent with the findings of previous studies that reported that women are less susceptible to viral infections.Citation44,Citation45 Moreover, the mean age (± standard deviation) of the whole sample was 51.7 ± 10.4 years, which is consistent with the data on the charts worldwide where the highest prevalence of confirmed cases is in the age range of 30 and 79 years.Citation10
Considering that the lungs are the organs primarily affected, this review found that respiratory muscle training was the most commonly used intervention because the main symptoms of the disease showed positive results in the components: physical and pulmonary functions, psychological, and social. The relaxation exercises intervention showed positive effects with anxiety, sleep problems, and, therefore, the QoL of the affected individuals.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
This research has been funded by Dirección General de Investigaciones of Universidad Santiago de Cali for allowing the development of this research.
Additional information
Funding
References
- Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579(7798):265–269. doi:10.1038/s41586-020-2008-3
- World Health Organization. Episode #59 - Flu & COVID-19; 2021. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/media-resources/science-in-5/episode-59---flu-covid-19?gclid=Cj0KCQjwhY-aBhCUARIsALNIC06FlghzifVA_Si2ckTbekWfamhdI129TCnEXMildGuXtMkCaFowaYkaAp_xEALw_wcB. Accessed December 14, 2022.
- Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi:10.1001/jama.2020.2648
- Wu JT, Leung K, Bushman M, et al. Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat Med. 2020;26(4):506–510. doi:10.1038/s41591-020-0822-7
- Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi:10.1056/NEJMoa2002032
- Fhon JRS, Silva LM, Leitón-Espinoza ZE, Matiello F, Araujo J, Rodrigues RAP. Atención hospitalaria al adulto mayor con COVID-19 [Hospital care for elderly COVID-19 patients.16]. Revista Latino-Americana de Enfermagem. 2020;28. doi:10.1590/1518-8345.4649.3396
- World Health Organization. Coronavirus disease (COVID-19): May 21, 2021; 2021 [ cited August 30, 2021]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-A-detail/coronavirus-disease-covid-19. Accessed December 14, 2022.
- Nateghi S, Goudarzi F, Namin ST, Rasouli A, Noushabadi AK, Mohammadnejhad S. Severity of COVID-19 in hospitalized elderly at admission, delay in hospitalization, and death from COVID-19. Tehran Univ Med J. 2021;79(12):715–722.
- Centers for Disease Control and Prevention C. COVID-19 risks and vaccine information for older adults; 2022. Available from: https://www.cdc.gov/aging/covid19/covid19-older-adults.html. Accessed December 14, 2022.
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi:10.1016/S0140-6736(20)30211-7
- Ghram A, Ayadi H, Knechtle B, Ben Saad H. What should a family physician know about nutrition and physical exercise rehabilitation’ advices to communicate to ‘long-term COVID-19’ patients? Postgrad Med. 2022;134(2):143–147. doi:10.1080/00325481.2022.2035589
- Ghram A, Briki W, Mansoor H, Al-Mohannadi AS, Lavie CJ, Chamari K. Home-based exercise can be beneficial for counteracting sedentary behavior and physical inactivity during the COVID-19 pandemic in older adults. Postgrad Med. 2021;133(5):469–480. doi:10.1080/00325481.2020.1860394
- Barker-Davies RM, O’Sullivan O, Senaratne KPP, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. 2020;54(16):949–959. doi:10.1136/bjsports-2020-102596
- Zhao H-M, Xie Y-X, Wang C. Recommendations for respiratory rehabilitation in adults with coronavirus disease 2019. Chin Med J. 2020;133(13):1595. doi:10.1097/CM9.0000000000000848
- Jimeno-Almazán A, Pallarés JG, Buendía-Romero Á, et al. Post-COVID-19 syndrome and the potential benefits of exercise. Int J Environ Res Public Health. 2021;18(10):5329. doi:10.3390/ijerph18105329
- de GesEPOC GD. Intervenciones no farmacológicas en pacientes con EPOC en fase estable [Non-pharmacological interventions in patients with stable phase COPD]. Archivos de Bronconeumología. 2017;53:36–38. doi:10.1016/S0300-2896(17)30363-0
- Jalalmanesh S, Zargarani F. Effects of progressive muscle relaxation technique on fatigue and sleep quality in patients with multiple sclerosis; 2015.
- Chegeni PS, Gholami M, Azargoon A, Pour AHH, Birjandi M, Norollahi H. The effect of progressive muscle relaxation on the management of fatigue and quality of sleep in patients with chronic obstructive pulmonary disease: a randomized controlled clinical trial. Complement Therap Clin Pract. 2018;31:64–70. doi:10.1016/j.ctcp.2018.01.010
- Saeedi M, Ashktorab T, Saatchi K, Zayeri F, Amir Ali Akbari S. The effect of progressive muscle relaxation on sleep quality of patients undergoing hemodialysis. Iranian J CritCare Nurs. 2012;5(1):23–28.
- Aksu NT, Erdogan A, Ozgur N. Effects of progressive muscle relaxation training on sleep and quality of life in patients with pulmonary resection. Sleep Breath. 2018;22(3):695–702. doi:10.1007/s11325-017-1614-2
- Marques A, Santos T, Martins J, Matos MGD, Valeiro MG. The association between physical activity and chronic diseases in European adults. Eur J Sport Sci. 2018;18(1):140–149. doi:10.1080/17461391.2017.1400109
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi:10.1136/bmj.n71
- Sherrington C, Herbert R, Maher C, Moseley A. PEDro. A database of randomized trials and systematic reviews in physiotherapy. Manual Therap. 2000;5(4):223–226. doi:10.1054/math.2000.0372
- Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi:10.1046/j.1445-2197.2003.02748.x
- Liu K, Chen Y, Wu D, Lin R, Wang Z, Pan L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement Therap Clin Pract. 2020;39:101132.
- Liu K, Zhang W, Yang Y, Zhang J, Li Y, Chen Y. Respiratory rehabilitation in elderly patients with COVID-19: a randomized controlled study. Complement Ther Clin Pract. 2020;39:101166. doi:10.1016/j.ctcp.2020.101166
- Özlü İ, Öztürk Z, Karaman Özlü Z, Tekin E, Gür A. The effects of progressive muscle relaxation exercises on the anxiety and sleep quality of patients with COVID-19: a randomized controlled study. Perspect Psychiatr Care. 2021;57(4):1791–1797. doi:10.1111/ppc.12750
- Sun J, Liu J, Li H, et al. Pulmonary rehabilitation focusing on the regulation of respiratory movement can improve prognosis of severe patients with COVID-19. Ann Palliat Med. 2021;10(4):4262–4272. doi:10.21037/apm-20-2014
- Tang Y, Jiang J, Shen P, et al. Liuzijue is a promising exercise option for rehabilitating discharged COVID-19 patients. Medicine. 2021;100(6):e24564. doi:10.1097/MD.0000000000024564
- Fernandez Alipazaga F. Efecto del programa de relajacion muscular de Jacobson y tecnicas cognitivas sobre los niveles de ansiedad en estudiantes de la Universidad de Huanuco-2019 [Effect of the Jacobson muscle relaxation program and cognitive techniques on anxiety levels in students from the Universidad de Huánuco - 2019]; 2021.
- Vernia-Carrasco A-M. Música y tecnología contra el Covid-19: un caso en personas mayores. Revista Prisma Social. 2021;32:244–261.
- Curci C, Pisano F, Bonacci E, et al. Early rehabilitation in post-acute COVID-19 patients: data from an Italian COVID-19 Rehabilitation Unit and proposal of a treatment protocol. Eur J Phys Rehabil Med. 2020;56(5):633–641. doi:10.23736/S1973-9087.20.06339-X
- Ferioli M, Prediletto I, Bensai S, et al. The role of 6MWT in Covid-19 follow up. Eur Respir Soc. 2021. doi:10.1183/13993003.congress-2021.OA4046
- McNarry MA, Berg RMG, Shelley J, et al. Inspiratory muscle training enhances recovery post-COVID-19: a randomised controlled trial. Eur Respir J. 2022;60(4):2103101. doi:10.1183/13993003.03101-2021
- Oliveira MR, Sudati IP, Konzen VM, et al. Covid-19 and the impact on the physical activity level of elderly people: a systematic review. Exp Gerontol. 2022;159:111675. doi:10.1016/j.exger.2021.111675
- Clemente-Suárez VJ, Beltrán-Velasco AI, Ramos-Campo DJ, et al. Physical activity and COVID-19. The basis for an efficient intervention in times of COVID-19 pandemic. Physiol Behav. 2022;244:113667. doi:10.1016/j.physbeh.2021.113667
- Conesa AG. Impacto de la pandemia de COVID-19 en los síntomas de salud mental y actuaciones de fisioterapia [Impact of the COVID-19 pandemic on mental health symptoms and physiotherapy actions]. Fisioterapia. 2021;43(1):1. doi:10.1016/j.ft.2020.11.001
- Pérez PMP, Dawaher JED, Paredes MFC. Impacto del COVID-19 en la salud mental de los pacientes hospitalizados [Impact of COVID-19 on the mental health of hospitalized patients]. Revista de la Facultad de Ciencias Médicas de la Universidad de Cuenca. 2020;38(2):55–64.
- Rodríguez-Quiroga A, Buiza C, Mon M, Quintero J. Update on COVID-19 and mental health. Medicine. 2020;13(23):1285–1296. doi:10.1016/j.med.2020.12.010
- Ahmed H, Patel K, Greenwood D, et al. Long-term clinical outcomes in survivors of coronavirus outbreaks after hospitalisation or ICU admission: a systematic review and meta-analysis of follow-up studies. medrxiv. 2020. doi:10.1101/2020.12.08.20245829
- González I, Gómez N, Ortiz R, Ibarra V, editors. Ejercicio Físico Como Tratamiento Adyuvante de Los Trastornos Mentales. Una Revisión Narrativa [Physical exercise as an adjuvant treatment of mental disorders. A narrative review]. Anales de la Facultad de Ciencias Médicas; 2018.
- Marconcin P, Werneck AO, Peralta M, et al. The association between physical activity and mental health during the first year of the COVID-19 pandemic: a systematic review. BMC Public Health. 2022;22(1):209. doi:10.1186/s12889-022-12590-6
- Bailly M, Pélissier L, Coudeyre E, et al. Systematic review of COVID-19-related physical activity-based rehabilitations: benefits to be confirmed by more robust methodological approaches. Int J Environ Res Public Health. 2022;19:15. doi:10.3390/ijerph19159025
- Li J-Y, You Z, Wang Q, et al. The epidemic of 2019-novel-coronavirus (2019-nCoV) pneumonia and insights for emerging infectious diseases in the future. Microb Infect. 2020;22(2):80–85. doi:10.1016/j.micinf.2020.02.002
- Bhopal SS, Bhopal R. Sex differential in COVID-19 mortality varies markedly by age. Lancet. 2020;396(10250):532–533. doi:10.1016/S0140-6736(20)31748-7
