Abstract
Background
Growing demand exists for high-quality Traditional Chinese Medicine (TCM) care, particularly through Nurse-led TCM clinics (TCM-NLCs). Nurses with extensive experience in TCM departments represent a potential workforce for this healthcare model. This qualitative study aims to investigate the willingness of these candidates to engage in TCM-NLCs, with a specific focus on their main concerns and apprehensions when facing new challenges.
Methods
Individual semi-structured face to face interviews were conducted with senior nurses from two TCM hospitals in Shanghai. Each participant had a minimum of three years of work experience in a TCM related department. Conventional qualitative content analysis was utilized.
Results
Fourteen participants were interviewed and data saturation was achieved. Nurses exhibited strong interest in practicing in TCM-NLCs. They believed that such innovative TCM nursing service model not only extends nursing role, provides greater empowerment and opportunities for professional development but also meets patients’ diverse healthcare needs, reduces reliance on other healthcare providers such as doctors, and increases hospital revenue. However, challenges such as deficiencies in evidence-based TCM nursing education, the absence of standardized practice guidelines, and limited prescriptive privileges were identified as primary obstacles to engaging in TCM-NLCs practice, potentially undermining the specialization of this advanced nursing practice model.
Conclusion
Although the nurses interviewed were highly motivated, they generally lacked confidence to practice independently in TCM-NLCs. A pressing priority is to address their concerns by providing appropriate resources as well as education and policy support to enhance their competency and ensure their practice autonomy, therefore building a more qualified pool of professionals for advanced TCM nursing practice.
Introduction
Introducing nurse-led clinics (NLCs) into primary care signifies an innovative manifestation of advanced nursing practice.Citation1 These clinics adeptly meet patients’ care needs in a timely manner,Citation2 enhancing healthcare accessibility and continuity, thereby mitigating global medical services shortagesCitation3 and contributing to containing healthcare costs.Citation4 Empirical evidence substantiates that NLCs outperform conventional care models in disease management, patient adherence, and patient satisfaction.Citation3 NLCs offer a spectrum of specialized services, such as peripherally inserted central catheter (PICC) insertion and maintenance,Citation5 diabetic foot ulcer care,Citation4 wound, ostomy, and continence care.Citation4 These clinics are prevalent and well-established in large general hospitals in China. A survey across 581 hospitals in 19 provinces revealed that 56.8% had established 926 NLCs.Citation6 In contrast, the development of nurse-led Traditional Chinese Medicine clinics (TCM-NLCs), where specialist nurses deliver care based on TCM nursing techniques, lags behind. Another survey encompassing 971 hospitals across 29 provinces found that only 21.3% had implemented TCM-NLCs.Citation7
Ancient TCM texts already recorded a wealth of nursing theories and practical knowledge. However, it was not until 1984, when China began offering higher education in TCM nursing, that TCM nursing was separated from TCM to become an independent discipline.Citation8 TCM nursing emphasizes the “Holistic Concept” and “Nursing based on Syndrome Differentiation”. The former views diseases as a disharmony between the individual and the environment, with the goal of nursing being to help patients restore a state of harmony; while the latter refers to nurses using approaches such as observation, listening, questioning, and pulse-taking to analyze patient’s physical signs to determine the TCM syndrome, and then formulating a nursing plan based on the identified syndrome.Citation8 Although both TCM physicians and TCM nurses base their practice on TCM theories, physicians focus on diagnosis and prescribing treatments, while nurses primarily perform health education and apply TCM techniques.Citation8 Currently, over 50 TCM nursing techniques, such as acupressure, auricular acupressure, gua sha, cupping, etc., are utilized in clinical settings.Citation9 Patients favor TCM techniques due to fewer side effects, less pain, ease of operation, and cost-effectiveness.Citation9 Nursing students from some overseas schools are also sent to China to study TCM nursing.Citation10
As an alternative to traditional physician-led care models, NLCs empower nurses to assume a more prominent role in healthcare delivery,Citation3 representing a revolutionary working model for nurses.Citation11 Aligned with Ajzen & Fishbeins’s Theory of Planned Behaviour, attitude is a disposition to respond with some degree of favorableness or unfavorableness to a psychological object and can be used to explain and predict human behavior.Citation12 It also serve as the most proximal predictor of behavioural intention.Citation13 Positive attitudes predispose individuals to approach tendencies while negative attitudes predispose them to avoidance tendencies.Citation12 Negative attitudes among nurses have been demonstrated to directly impede the successful introduction of new nursing roles.Citation14 Thus, it is pivotal to consider nurses‘attitudes during any changes in nursing practice.Citation15 Senior nurses with extensive experience in TCM-related departments emerge as optimal candidates for implementing advanced TCM nursing practice. To address the growing demand for chronic disease management, two TCM hospitals in Shanghai, China plan to introduce TCM-NLCs. This study aimed to address the void in current knowledge about senior nurses’ perspectives on the development of TCM-NLCs and their willingness to engage in independent practice within such clinics. Only three English articles related to TCM-NLCs published in peer-reviewed journals were identified. These articles either share the operational experiences of TCM-NLCs in a specific hospital,Citation16 report the work experiences of nurses who have part-time positions in TCM-NLCs,Citation11 or describe the development status of TCM-NLCs in a certain province in China.Citation17 However, none of them adequately address our research aim, highlighting the necessity of the current study. The Theory of Planned Behaviour also suggests that many behaviors pose difficulties of execution that may limit volitional control; therefore, judgments of a behavior’s difficulty must also be considered.Citation12 Only when individuals have a sufficient degree of actual control over the behavior will they carry out their intentions when opportunities arise.Citation12 Thus, besides nurses’ attitudes, we also focus on their perceived potential challenges and obstacles in practicing in TCM-NLCs in this study. The findings would assist administrators in considering the attitudes and concerns of senior nurses when adopting innovative healthcare service models in TCM institutions. Additionally, it might aid the government in better planning the sustainable development of TCM-NLCs, thereby enhancing TCM nursing service capabilities across the city.
Materials and Methods
Study Design and Participants
A qualitative approach based on semi‐structured individual depth interviews, chosen over focus groups, was utilized to create a private environment conducive to respondents expressing authentic thoughts without external influence. The study adhered to the Consolidated Criteria for Reporting Qualitative Research (COREQ) guidelines.Citation18
Two TCM hospitals in Shanghai that intended to introduce TCM-NLCs were selected as the study sites. PurposiveCitation19 and snowballCitation20 sampling strategies were adopted to recruit nurses with a minimum of three years of work experience in a TCM-related department and holding a senior professional title, yet not currently practicing in a TCM-NLC. In mainland China, nurses are classified into four levels, from lowest to highest: junior nurse, senior nurse, associate chief nurse, and chief nurse. Those who hold a professional title refers to the last three categories were potential interviewees. Furthermore, we only selected participants who have either visited TCM-NLCs in other hospitals, or have been exposed to the daily operations of various NLCs through media or peer communication, ensuring their ability to contribute valuable information during the interviews. Initial participants were identified through recommendations from nurse managers at each study site. Maximum variation in gender, educational levels, work experience, and department of employment was considered to ensure diversity in perceptions. The sample size was determined when data saturation occurred, with no emergence of new themes. Considering there is currently no unified standard to determine when data saturation is reached in qualitative study, we referenced the “Principles for Specifying Data Saturation” proposed by Francis et al.Citation21 This involves an initial analysis sample (at least 10 interviews) and a stopping criterion (after 10 interviews, if no new themes emerge in the following three interviews, it can be defined as the data saturation point).
Procedures
Following a review of relevant literature, we crafted the initial interview guide and tested the guide on two qualified nurses through pre-interview sessions. Pilot testing results were examined by the research team and led to the refinement of the probe questions and finalization the formal interview guide (Appendix 1). The initial two questions served as general icebreakers designed to instigate discussion and foster a relaxed atmosphere, encouraging participants to engage with the facilitator in a natural manner. The final question aimed at uncovering any potential blind spots or gaps in the interview guide. The remaining questions were posed without a specific sequence and all designed as open-ended queries to elicit comprehensive information.
The formal on-site interviews took place in a hospital conference room and were scheduled at participants’ convenience between November 1st and December 31st, 2023. All interviews were audio-recorded with consent. Using a 2:1 format, two interviewers engaged with one participant— one posed questions, and the other recorded the conversation and noted nonverbal cues. Effective communication skills were applied, and participants were encouraged to actively express genuine feelings and provide additional information or clarifications for ambiguous answers. No other individuals were present in the conference room during the interviews, each lasting approximately 35 minutes. Reflective journals were written by the interviewers after each session to enhance subsequent interviews. At the outset, participants’ demographic information, work experience, and pathways for acquiring knowledge and training in TCM nursing were collected. The interviewers were two postgraduate students specializing in nursing science with a focus on TCM nursing.
Data Collection and Analysis
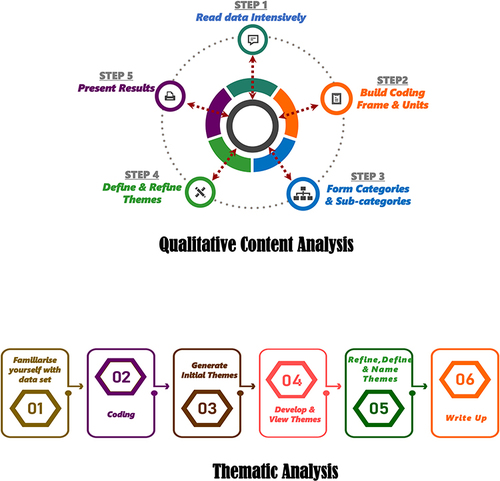
Data collection and analysis occurred concurrently. Audio recordings were textualized into Chinese using a speech-to-text app (Xunfei Hearing, version 6.0.3550). The transcribed sentences were then uploaded to a laptop and cleaned to produce a readable document. Two interviewers cross-validated the data for integrity. A researcher (PJ-X), holding an Australian NAATI certificate, translated all texts into English. Qualitative content analysis (QCA)Citation22 was employed to establish coding units within the coding frame derived from the transcripts, performed independently by two analysts (LP-Y & YM-W). Given the probes in this study were open-ended rather than based on a preexisting theory, we employed conventional QCA rather than directed or summative QCA approaches.Citation23 Encoded views were categorized based on the similarity of open coding or spindle coding regarding the topic. Categories and sub-categories were formed deductively and inductively in an iterative, systematic process within each concept domain,Citation24 and were connected conceptually. The final themes were refined by integrating frameworks independently constructed by the two analysts. Results obtained at each step were cross-verified against the research questions to optimize accuracy and reliability. QCA, widely utilized in nursing studies,Citation25 is characterized by its flexibility. It focused on meanings, intentions, consequences, and context,Citation26 allowing for deductive, inductive, or combined approaches, considering both manifest and latent meaning.Citation27 Unlike thematic analysis, which follows a more linear six-phase process, QCA positions the research question at the center of a circular process, revisited repeatedly during the five phases of analysisCitation24 ().
Rigour
Several measures were implemented to minimize bias in portraying and summarizing participants’ perceptions. First, the research team, comprising of staff from diverse backgrounds, included registered nurses, TCM practitioner, clinical psychologist, public health officer, and health policy researcher, was established. Second, two researchers independently analyzed data, constructed coding framework, and refined categories. Regular meetings were conducted where key research members exchanged ideas, ensuring consistency, integrity, and reliability in the coding data process, resolving disputes through discussion and consensus. Third, a neutral stance was maintained during interviews and data analysis. Finally, self-reflection and a reflexive approachCitation28 were consistently applied by researchers throughout the study. In addition, all researchers underwent uniform online training before commencing the study to enhance consistency and quality.
Ethical Considerations
The protocol was reviewed and approved by the Human Research Ethics Committee (HREC) of Shanghai Sanda University, Shanghai, China (No. 2023007). Participants were provided with detailed information regarding the purpose, procedures, and voluntary nature of the study, along with an explanation of their rights. Written informed consent was obtained from all the participants. Specifically, the consent form also included a statement confirming that participants agreed to the publication of their anonymized responses. Following transcription, only the transcripts were stored on a password-protected server, and the recordings were deleted. Anonymity was maintained using codes (eg, N1, N2) for participants’ names. Identifying information was removed from transcripts, and there were no dual role conflicts between researchers and participants. Only research team members were authorized to access the data during and after the study. All participants agreed to the publication of their anonymized responses.
Results
Thematic redundancy was reached after the 11th interview, with no new information emerging from the subsequent three interviews, resulting in a total of 14 nurses interviewed (data saturation point was 14). Demographic characteristics are detailed in , with an average age of 30.1 years and an average TCM department work experience of 6.4 years, reflecting a generally youthful cohort. Senior nurses aged 40 and above were either practicing in a TCM-NLC that did not meet the inclusion criteria, or declined invitations, citing a nearly unanimous reason—satisfaction with their current, stable positions and a lack of consideration for other career changes. Only five of 14 participants had taken one TCM nursing course at the tertiary level. Furthermore, three of them attended these courses as electives rather than compulsory modules of their undergraduate program. According to the 8th question in the interview outline, all 14 nurses interviewed expressed a willingness to practice in TCM-NLCs, with their levels of enthusiasm ranging from “Willing” to “Very Willing”. Specifically, six nurses indicated they were “Willing”, while the remaining eight expressed they were “Very Willing”. From respondents’ perceptions and attitudes toward TCM-NLCs, we distilled and finalized four main themes, ie, motivation, strengths, constraints, and threshold and incentives, further elucidated with interview quotations.
Table 1 Sample Characteristics (n = 14)
High Motivation Towards Practicing in TCM-NLCs (Theme 1: Motivation)
The overarching impetus behind the establishment of TCM-NLCs stems from the escalating clinical demands for TCM nursing services. All participants demonstrated keen interest and enthusiasm for this novel working model which represents the specialization and extension of nurses’ roles. In addition, participants asserted that hospital managers and physicians have also expressed a favorable view toward the proliferation of TCM-NLCs.
Increased Perceived Professional Benefits
The autonomy inherent in practicing within TCM-NLCs contributes significantly to the recognition and augmentation of nurses’ professional value and societal status. For nurses employed in TCM hospitals, obtaining certification as advanced practice nurses (APNs) and working in TCM-NLCs represents a crucial pathway for personal career development.
Patients’ inherent misperception that nurses can only give injections and dispense medication should be changed. TCM-NLCs have proved this point. (N6)
Most nurses are engaged in repetitive routine nursing duties on the wards from the beginning of their career to retirement. The TCM-NLCs offers the possibility of becoming an expert nurse with delivering highly specialized and innovative TCM care. (N13)
The goal of many nurses may have been to become an administrator. However, the number of positions for nursing managers was very limited. Becoming an expert nurse working in TCM-NLCs offers another option. Furthermore, this career path is well-suited to frontline nurses as it emphasizes clinical talent more than managerial skills. (N5)
TCM-NLCs are unique products generated from TCM hospitals rather than general hospitals. Nurses can not only conduct routine nursing research but also design TCM nursing research relying on TCM-NLC. This broadens the research topic scope and further develops their research talents. (N12)
In NLCs, nurses relieve patients’ suffering through independent assessment, diagnosis, and treatment, gaining their trust. Such perceived professional benefits and career fulfillment are not something that can be felt by an ”operator” who merely carries out medical orders. (N1)
Extensive Support from Other Stakeholders
Support from Patients
Participants reported that many patients, having benefited from TCM nursing care during their hospitalization, express a desire to sustain this care post-discharge. In this context, TCM-NLC is recognized as an innovative transitional nursing model.
I work in the ward. Many hospitalized patients have asked me, “How can I register for your specialist appointment to continue with these TCM nursing care programs after discharge?” (N11)
Patients with chronic illnesses, such as those with post-stroke sequelae, exhibit a significant demand for TCM rehabilitation nursing care post-discharge. This demand can be addressed at TCM-NLCs. This is a form of transitional nursing. (N1)
Many patients complain that auricular acupoint stickers often come off after getting wet in the shower. Patients are unfamiliar with specific acupoint locations. Therefore, accurately reapplying the stickers to the correct acupoints requires registering another appointment in the acupuncture department and waiting in line for an acupuncturist’s assistance. This process is both expensive and time-consuming. A TCM-NLC could easily address this issue for them. (N8)
Support from Hospital Manager and Physicians
Some nurses stated that hospital managers and physicians warmly embraced the concept of TCM-NLCs. Given the disproportionate ratio of nurses to TCM physicians, they considered the establishment of TCM-NLCs could not only alleviate the workload on physicians but also significantly augment the hospital’s service capacity, thereby contributing to substantial revenue growth.
Physicians have enthusiastically welcomed TCM-NLCs. Although they primarily prescribe herbal medicines in outpatient clinics, the therapeutic effects can be further enhanced with combined non-pharmacological TCM treatments like Gua-sha, cupping, or moxibustion. The busy outpatient schedules of physicians limit their ability to provide these treatments, making TCM-NLCs a valuable supplementary service provider. (N13)
Due to the increasing patient demand, the establishment of TCM-NLCs may significantly boost hospital revenue. (N14)
Department of Acupuncture is a specialized department at TCM hospital. Despite offering evening outpatient services to the public, the limited number of acupuncturists still cannot meet the demands of the vast patient population. My colleague (an acupuncturist) mentioned that if non-invasive procedures such as body/auricular acupressure and cupping could be handed over from Department of Acupuncture to TCM-NLCs for provision, it would free up acupuncturists to attend to more acute cases. (N8)
Strengths of TCM-NLCs Over Other NLCs (Theme 2: Strengths)
TCM-NLCs exhibit distinctive advantages in the management of chronic diseases, sub-health conditions, and the practice of “Preventive Treatment of Disease”. These strengths distinguish them from other NLCs and render them irreplaceable in these specific domains.
Managing Chronic Diseases with TCM Nursing Techniques
In the case of chronic diseases such as diabetes and persistent insomnia, TCM-NLCs do not merely replicate the service model provided in conventional nurse-led diabetes clinics and counseling center, respectively. Instead, TCM-NLCs offer distinctive health education and nursing consultation grounded in the principles of TCM for patients.
The hospital where I work has diabetes NLCs. However, many patients with diabetic foot ulcers, who used Chinese herbal steam baths during their hospitalization, wish to continue receiving this care after discharge due to its satisfactory effects. They questioned why there were no TCM-NLCs providing such nursing care. This is a typical example of why TCM-NLCs cannot be replaced by conventional NLCs. (N9)
Considering the unique advantages of TCM in chronic disease management, nurses can offer personalized TCM guidance. For example, in the case of patients with chronic insomnia, nurses may throw them in some TCM diet tips and suggest them practice Qigong exercises. (N13)
Preventive Nursing Care of Diseases
“Preventive Treatment of Disease” (also known as “Zhi-Wei-Bing” in Chinese) is a concept in TCM, signifying the application of preventive treatments according to a projected predisposition towards a disease, in order to avoid falling ill or to diminish the chances of the illness worsening.Citation29 Implementing preventive nursing care based on the philosophy of “Zhi-Wei-Bing” could be beneficial in enhancing sub-health or pre-disease states.
Many people nowadays are in a sub-health or pre-disease state and are keen to seek help from TCM. What they’re really after might not be pills but some tips on staying healthy. With such a huge population in China, it’s tough for doctors to give detailed health advice in regular clinics. That’s where TCM-NLCs, with nurses offering TCM-based health tips, can make a real difference. (N2)
A variety of techniques that embody the philosophy of “Zhi-Wei-Bing”, such as Dog-Days Moxibustion and Dog-Days Plaster, are only available at TCM-NLCs. (N3)
Constraints to the Specialization of TCM-NLCs (Theme 3: Constraints)
Nine participants (64.3%) expressed diminished confidence in undertaking independent practice within TCM-NLCs. These apprehensions are also potential impediments to the specialization and development of TCM-NLCs.
Deficiencies in Knowledge and Skills
Participants in this study lacked confidence in delivering advanced TCM nursing practice mainly because of their insufficient knowledge and skills.
I need to enhance my TCM theory and skills to treat my patients more effectively. (N10)
Nurses who graduated from general medical universities, rather than TCM universities, generally have not received systematic TCM education, making them uncompetitive to work as APNs in TCM-NLCs. (N5)
Routine TCM nursing work in the ward involves simply executing medical orders and doesn’t necessarily require proficiency in “Nursing based on Syndrome Differentiation”. Whereas, when practicing in TCM-NLCs, nurses need to independently diagnose the patient and formulate the best clinical decision after a thorough assessment of patient’s medical history. This process cannot be accomplished without a rich knowledge base of TCM. (N4)
Absence of Guidelines to Guide Standardized Practice in TCM-NLCs
Participants found it difficult to implement standardized TCM nursing practices without guidelines to refer to. Nurses usually refer patients on their first-visit to the physicians for advice, and then followed up with TCM nursing techniques according to physicians’ diagnosis and assessment. This practice, in essence, contradicts the original intention of establishing TCM-NLCs and diminishes the inherent value of TCM-NLCs.
Physicians make clinical decisions based on clinical practice guidelines. There should also be standardized guidelines to guide APNs’ practice in TCM-NLCs. (N7)
In NLCs, including TCM-NLCs, nurses generally refer patients to physicians for seeking diagnosis advice at patients’ first visit due to safety concern. (N1)
Restrictions on Nurses’ Prescriptive Privileges
Stringent restrictions on APNs prescribing privileges not only impair the autonomy of TCM-NLCs but also undermines nurses’ professional enthusiasm and professional identity.
Unlike many developed countries, most nurse in China don’t have the right to prescribe medicine. This is one of the overarching reasons why patients tend to visits physicians despite a long waiting time and short consultation time. (N6)
Without prescriptive privileges, nursing services delivered in NLCs involve examinations and medications still require prior authorization from physicians. This significantly diminishes the autonomy of APNs, causing them to feel inferior to physicians despite their extensive clinical experience. (N1)
Without the right to prescribe necessary examinations and medications, APNs are compelled to frequently refer their patients to physicians. This interruption in the nursing procedure discourages nurses enthusiasm and job passion. (N11)
While the prescriptive authority is granted, sound laws and regulations must also be formulated to protect and oversee APNs’ prescribing behavior in TCM-NLCs. (N5)
Insufficient Resources, Infrastructure, and Policy Backing
Participants posit that the lack of essential resources, infrastructure, and limited publicity acts as impediments to the establishment and development of TCM-NLCs. Policy support is warranted.
While many hospitals have NLCs, these clinics are not equipped with smoke extraction equipment, making it impossible to offer moxibustion services. (N8)
The hospital’s website only showcases profiles of physician experts and does not provide information about nurse experts. This hampers the promotion of TCM-NLCs to the public, resulting in many patients being unaware of their existence. (N9)
We want to know how does the salary and career promotion path for APNs in TCM-NLCs compare to that of regular nurses? The government has not issued a unified policy document with detailed descriptions and explanations. (N12)
Elevated Qualification Standards Accompanied by Competitive Financial Incentives (Theme 4: Threshold & Incentives)
Respondents unanimously concurred on the necessity of instituting rigorous criteria for the selection of highly qualified APNs working for TCM-NLCs. Accordingly, competitive remuneration packages should be provided.
Nurses working for TCM-NLCs are going to deal with all sorts of diseases, just like GPs. This requires their medical knowledge to be very comprehensive. (N10)
In order to make the best clinical decision independently, nurses working for TCM-NLCs should also possess excellent communication skills and emergency talents, besides knowing a bunch about TCM. This requires a high level of comprehensive quality from practitioners. (N7)
If you want to set the bar high for getting into this field, you better make sure the pay and chances for moving up the professional ladder are attractive. (N6)
Unified criteria in educational level, professional title and work experience should be established for nurses who intend to work in TCM-NLCs. Those who fulfill the minimum requirements can apply for the assessment and be awarded the qualification after passing the assessment. Policies and assessment standards should be formulated by the national health authorities. Chinese education authorities may also consider adding TCM-NLC practice courses in undergraduate or postgraduate nursing programs, so as to train eligible candidates at an earlier stage. (N9)
Discussion
Approximately 28.6% of the participants (n = 4) frequently highlighted words including “the feeling of being valued”, “meaningful”, and “promising” alongside “improved clinical outcomes” during interviews. Their statement implied the shared endorsement for TCM-NLCs amongst various stakeholders, including patients, hospital managers, doctors, and nurses. TCM-NLCs integrate preventive, therapeutic, and rehabilitative functions, addressing patients’ multifaceted healthcare needs.Citation17 In response to the plight of prolonged wait times for healthcare services in China currently, any initiatives aimed at reversing this situation are highly welcomed.Citation15 This sentiment of the interviewed nurses is also reinforced by a survey, which revealed that 91.5% of outpatients recognized the necessity of establishing TCM-NLCs to cater to their needs.Citation30 Efficiently managed nurse-led care also alleviates doctors’ workload,Citation31 and covers gaps in the junior doctors’ rota due to the reduction of their hours.Citation3,Citation32 Additionally, it creates a stream of additional revenue and profit for hospitals.Citation33,Citation34 An umbrella review, after summarizing a large body of evidence, cautiously provided unbiased results indicating that NLCs offer comparable or superior care to usual care with high levels of patient satisfaction. This is because NLCs reduce patients’ waiting times while maintaining their safety and save healthcare resources and costs.Citation3 Researchers predict that NLCs are thereby likely to accelerate growth.Citation3 In the long term, the growth of TCM-NLCs may also help promote a broader integration of traditional and modern medical practices. This also aligns with the World Health Organization’s definition of Future Health Service Delivery, which envisions an efficient blend of both traditional and conventional medicine.Citation35 According to the nurse interviewed (n = 3; 21.4%), extended autonomy and scope of practice in the TCM-NLCs will foster a heightened sense of accomplishment and self‐recognition, and increase acceptance of their professional roles by others. This may also explain previous findings indicating higher levels of job satisfaction and professional identity amongst nurses working in TCM-NLCs.Citation36 An estimated 16.3% of nurses in tertiary hospitals in China encounter career bottleneck when they are mid-career, with a capped number of positions for nurse manager or chief nurse, and they can find themselves shifted to administrative units in the hospital involved with such tasks as food and laundry among others.Citation37 Developing TCM-NLCs presents an alternative career trajectory or advancement opportunity for these nurses employed in TCM hospitals. It is worth noting that upon database search, we found no studies available on other traditional medical systems-based NLCs, apart from TCM-NLCs. Considering the potential benefits of traditional medicine, we also encourage other regions where traditional medicine is popular, such as India, South Korea, and Arab countries, to consider developing the nurse-led Ayurveda nursing clinics, Korean medicine nursing clinics, Unani medicine nursing clinics respectively, by referencing the TCM-NLCs model.
TCM-NLCs require guidelines and standards to effectively guide nurses in their practice. Safe and effective practice necessitates knowledge, skills, judgment, and attitudes outlined in all standards of practice.Citation38 Conversely, the absence of clearly defined and normalized professional roles can jeopardize the functioning and operation of TCM-NLCs.Citation11 As early as 2016, the “National Nursing Development Plan (2016–2020)” issued by the National Health and Family Planning Commission of China proposed leveraging TCM nursing in disease treatment, chronic disease management, and rehabilitation, thus expanding the scope of TCM nursing services.Citation16,Citation17 Regrettably, to date, the development of TCM-NLCs remains in its infancy, lacking uniform guidelines and standards to elucidate and standardize the practice scope and procedures within these clinics.Citation11 A previous cross-sectional survey also indicated that there is currently no standardized management and audit system for several aspects of TCM-NLCs, including personnel allocation, clinic responsibilities, operating hours, practitioner qualifications, and safety and quality control.Citation17 Nurses have no reference for decision-making beyond their personal experience. They also face difficulties in implementing standardized care protocols for new visit patients.Citation11 It is noteworthy that, in response to the question “What services do you think should be delivered in TCM-NLCs?”, nearly all nurses prioritized clinical/medical tasks, overlooking the assessment of patients’ psychological, familial, and social support. This contradicts the core philosophy of the nursing professionCitation39 and the original intent of establishing NLCs,Citation40 which is to allow a holistic view of patients that incorporates aspects of family, community, and work environment, as opposed to discrete clinical outcomes. In developed countries, NLCs commonly provide services include health assessments for monitoring patient conditions and symptoms, health education to facilitate compliance and a healthy lifestyle, and care coordination.Citation1 APNs in NLCs employ a holistic framework to work with clients to stabilize their condition and maximize their health.Citation1 A holistic approach therefore is also indispensable in the TCM-NLCs to address both illness and psychosocial facets, offering additional benefits for patients rather than duplicating a medical model. This includes fostering shared decision-making, collaborating with patients in healthcare management, and improving overall quality of life by building supportive relationships with patients and considering their emotions and social networks in nursing practice.Citation11 Overall, the formulation of practical guidelines and standards specific to TCM-NLCs is imperative, alongside the clarification of nursing role boundaries for TCM APNs using a nursing framework.Citation11
Challenges related to nurse prescribing were frequently highlighted during the interviews and were perceived as undermining the specialization of TCM-NLCs. Nurse prescribing has proven to be a positive addition to clinical practice.Citation41 In high-income countries including USA, Canada, Australia, and New Zealand, APNs are eligible to prescribe within their scope of practice under a variety of independent (or unsupervised) and supplementary models;Citation42,Citation43 at least 13 European countries have enacted legislation on nurse prescribing.Citation42 However, in China, only a few pilot programs allow nurses to prescribe medical consumables, such as dressings and a limited number of topical drugs, while they are not permitted to prescribe oral or injectable medications,Citation36 failing to satisfy the comprehensive practice needs.Citation44 The inability to prescribe necessary medications has compelled Chinese nurse specialists to refer patients attending NLCs to physicians, resulting in a disruption of specialty care.Citation15 This finding aligns with previous studies indicating that nurse specialists believed that lack of prescriptive privilege hindered their ability to provide holistic care to patients.Citation15 Some nurses claimed that considerable patients prefer one-stop services, which they are unable to provide without specific prescriptive authority.Citation11 Consequently, NLCs might struggle to gain recognition from patients, particularly those with weak care autonomy.Citation11 Granting APNs a certain range of prescribing privileges to operate TCM-NLCs is worth considering; after all, there is a wealth of evidence available confirming the benefits of such authorization, including enhanced patient access to medications and advice,Citation43 improved patient outcomes and satisfaction, reduced patient admission rates and lengths of stay,Citation44 enhanced teamwork, fewer prescriptions of costly medications,Citation45 and alleviation of the primary physician shortage.Citation44 In developed countries, APNs typically manage NLCs with significant autonomy, and independently accept and provide higher quality care for referrals from physicians.Citation46 Their satisfaction and identity with the nursing profession is also enhanced by this high level of professional autonomy.Citation44 While full liberalization of nurse prescribing requires legislative endorsement and additional time to validate its feasibility,Citation11 we encourage incremental and secure improvements. A Cochrane systematic review demonstrated that nurses were as effective as physicians in prescribing medications for a range of chronic diseases.Citation47 Therefore, it is recommended to grant APNs the right in prescribing oral and titrated drugs within the context of chronic disease management first, with due protection against legal liability in their prescribing behavior. Cautious accreditation and monitoring of nurse prescribing within the policy framework are necessary.Citation44
As per the formal definition by the International Council of Nurses (ICN), APNs who run the nurse-led care should have acquired additional expert or specialist knowledge, clinical skills, and complex decision-making capabilities. However, a majority of interviewed nurses acknowledged that insufficient TCM knowledge and skills obstructed their ability to manage complex healthcare issues within a TCM setting. This can also compromise the autonomy of the nurses working in TCM-NLCs, as they have to rely on physician diagnoses and advice.Citation11 Extending nurses’ roles without adequate educational and training preparation also leads to ambiguity and a lack of understanding about their roles and scope of practice.Citation48 This aligns with expectations, given that only 35.7% of respondents had minimal TCM nursing education at the tertiary level. This circumstance is largely attributable to the current undergraduate nursing education system in mainland China, where TCM nursing courses are only delivered as compulsory modules in TCM universities, and their representation within the curriculum is notably limited (see Appendix 2). For instance, at Shanghai University of Traditional Chinese Medicine, the TCM-based Bachelor of Nursing Science (BNS) program includes only two compulsory TCM nursing courses, ie, “Fundamentals of TCM Nursing (3 credits)” and “TCM Clinical Nursing (2 credits)”, which account for only 5/280 of the total curriculum credits. In general universities or medical universities, only a small proportion of mainstream biomedical nursing programs (eg, BNS) integrate a selective or extended TCM course into curriculum framework.Citation49 Moreover, these courses lack consensus regarding course names, objectives, and content, thus failing to provide students with comprehensive knowledge and skills in TCM nursing.Citation49 Graduates from these institutions only received brief On-the-Job training upon employment in TCM hospitals. Our interview data indicated that 64.3% of the participants only acquired TCM nursing skills through repetitive procedural practices after employment in TCM hospital. Such fragmented knowledge and skill training inadequately prepares nurses for advanced TCM nursing practice in NLCs. A prior multicenter cross-sectional survey also revealed that although registered nurses in TCM hospitals generally viewed evidence-based TCM nursing positively, they lacked the competencies to implement these practices.Citation10 Ensuring the practice competence standards of nurses working for NLCs through education is warranted,Citation1 as knowledge facilitation is the initial step for Chinese nurses in evidence-based practice.Citation10,Citation50 The Master’s-level preparation for APNs is recommended by the ICNCitation51 and has been commonly accepted.Citation11 We propose increasing the investment in TCM nursing education and setting up specialized directions at the tertiary level. In particular, at least a comprehensive course should be offered at postgraduate stage to introduce the evidenced-based TCM nursing knowledge, qualification access, job duties, laws and regulations required to operate the TCM-NLCs, as well as the research methodology of TCM nursing. Concurrently, health service managers should improve the talent incentive system for TCM APNs, given the external motivators such as improved working conditions and financial incentives usually act as an incentive amongst nurses to assume more responsibilities in a nurse-led healthcare model.Citation31
In addition to staff support, the development of TCM-NLCs may be constrained by insufficient organizational preparedness, funding and public awareness. Some interviewees expressed concerns about the hospital administrator’s lack of attention to the TCM-NLCs, citing shortages in necessary infrastructures/facilities and inadequate publicity for TCM-NLCs. A previous study conducted in a TCM hospital revealed that only 17.8% of patients were aware of TCM-NLCs, with some individual NLCs experiencing no patient visits throughout the day.Citation11 Such disparities in organizational resource allocation could adversely impact the effective implementation of doctor-nurse substitution strategies.Citation31 Apart from encouraging physicians to introduce and refer eligible patients to NLCs, it is necessary to promote TCM-NLCs and TCM APNs through various media channels, including television/broadcast, the hospital’s official website, WeChat accounts, community brochures, and other social and online platforms.Citation11 Additionally, improvements are needed in legislation and supervision regarding the scope of services, consultation processes, quality evaluation, and fee mechanism for TCM-NLCs. It is worth mentioning that digital engagement in nursing field is prevalent. For instance, Cairo University Hospital has successfully utilized telehealth and artificial intelligence to provide nurse-led patient education to orthopedic patients with restricted mobility.Citation52 Therefore, exploring how digital technologies can expand the service scope and improve the service quality of TCM-NLCs is also valuable. In conclusion, to align with the dynamic changes and expansion of nursing roles and scopes of practice in TCM-NLCs, policymakers and hospital managers should give due consideration to these multiple hindrances. Furthermore, measures developed to address these hindrances and challenges should not only be thoroughly discussed at stakeholder meetings but also carefully validated and improved in pilot projects before further generalization in nationwide TCM-NLCs.
Methodological Limitations
While our sample encompassed various departments, the overall sample size was relatively small, and we only adopted purposive and snowball sampling strategies. Moreover, this study was only conducted in two TCM hospitals located in Shanghai. Differences in health policies across regions may elicit varied insights on advanced nursing practice in TCM-NLCs from nurses in other areas. Therefore, we must acknowledge the potential bias in sample selection and the limited generalizability of the current findings. We suggest that others exercise caution when applying these results to other healthcare settings or cultural contexts.
In addition, our focus on understanding nurses’ willingness to practice at TCM-NLCs led us to interview those without prior TCM-NLC experience. Feedback from nurses with relevant practice experience could have further enriched our current findings, shedding light on specific barriers encountered in TCM-NLC practice and potential shifts in their initial perceptions towards TCM-NLCs.
Conclusion
The interviewed nurses generally demonstrated interest and willingness to practice in TCM-NLCs, believing that this innovative healthcare service model can not only fulfill their career value and promote professional development but also potentially be welcomed by other stakeholders. Yet, they also acknowledge that several challenges require to be addressed to engage experienced nurses in delivering advanced TCM nursing practices. Key obstacles encompass inadequate knowledge and skills among nurses regarding evidence-based TCM nursing practices, limitations on prescriptive privileges, the absence of standardized practice guidelines, and the underdevelopment of legislative, regulatory, quality assessment, and talent incentive systems. Health service managers should carefully consider these impediments while concurrently enhancing multi-channel publicity efforts to foster the positive development of high-quality TCM-NLCs.
Abbreviations
APN(s), Advanced practice nurse(s); BNS, Bachelor of Nursing Science; COREQ, Consolidated Criteria for Reporting Qualitative Research; ICN, International Council of Nurses; NLC(s), Nurse-led clinic(s); QCA, Qualitative Content Analysis; TCM, Traditional Chinese medicine; TCM-NLC(s), Nurse-led Traditional Chinese Medicine clinic(s).
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
This work was supported by Health and Medical Research Fund [20212801], Health Bureau, Hong Kong SAR and the Teaching Development Grant from the University Grants Committee of the Hong Kong Special Administrative Region, China [LTG22-25/IICA/18] to YS-H; Shanghai Key Laboratory for Pharmaceutical Metabolite Research Project [SHZYDX2023-01] to FY-Z; and TCM Research Project, Shanghai Municipal Health Commission [2022CX007] to WJ-Z.
References
- Wong FK, Chung LC. Establishing a definition for a nurse-led clinic: structure, process, and outcome. J Adv Nurs. 2006;53(3):358–369. doi:10.1111/j.1365-2648.2006.03730.x
- Rani R, Kaur AR. Nurse led clinics in India, an innovative approach in patient management. Int J Adv Res. 2019;7(9):1190–1192. doi:10.21474/IJAR01/9772
- Connolly C, Cotter P. Effectiveness of nurse-led clinics on healthcare delivery: an umbrella review. J Clin Nurs. 2023;32(9–10):1760–1767. doi:10.1111/jocn.16186
- Shiu AT, Lee DT, Chau JP. Exploring the scope of expanding advanced nursing practice in nurse-led clinics: a multiple-case study. J Adv Nurs. 2012;68(8):1780–1792. doi:10.1111/j.1365-2648.2011.05868.x
- Yi Q, Li X, Chen T, Li Z, Cao X, Gu W. An information-based nursing quality evaluation model of daily PICC Work in outpatient clinics. Contrast Media Mol Imaging. 2022;2022:8187644. doi:10.1155/2022/8187644
- Gao F, Ding S, Huang J, et al. Investigation on the establishment and practice of nursing clinic in tertiary hospitals in China. Chin Nurs Manage. 2017;17(10):1297–1302.
- Chen X, Zhang S, Zhou J, Chen L. Investigation and reflection on the current situation of nurse-led Traditional Chinese Medicine clinic. J Trad Chin Med Manage. 2021;29(6):28–31.
- Hao Y, Liu H, Yue S, Liu X. Introducing traditional Chinese nursing: a review of concepts, theories and practices. Int Nurs Rev. 2011;58(3):319–327. doi:10.1111/j.1466-7657.2011.00918.x
- Zhou F, Lv Y, Zhao J. Evidence based practice competence of future traditional Chinese medicine nurses: a cross-sectional online study. Nurse Educ Today. 2022;110:105238. doi:10.1016/j.nedt.2021.105238
- Zhou F, Hao Y, Guo H, Liu H. Attitude, knowledge, and practice on evidence-based nursing among registered nurses in traditional Chinese medicine hospitals: a multiple center cross-sectional survey in China. Evid Based Complement Alternat Med. 2016;2016:5478086. doi:10.1155/2016/5478086
- Dong Z, Wei L, Sun X, et al. Experiences of nurses working in nurse-led clinics in traditional Chinese medicine hospitals: a focused ethnographic study. Nurs Open. 2023;10(2):603–612. doi:10.1002/nop2.1326
- Ajzen I, Fishbein M. Attitudes and the attitude-behavior relation: reasoned and automatic processes. Eur Rev Social Psychol. 2000;11(1):1–33. doi:10.1080/14792779943000116
- Conner M, Sparks P. Theory of Planned Behaviour and Health Behaviour. Predicting Health Behaviour. 2nd ed. Berkshire, UK: Open University Press; 2005:121–162.
- Ling DL, Lyu CM, Liu H, Xiao X, Yu HJ. The necessity and possibility of implementation of nurse prescribing in China: an international perspective. Int J Nurs Sci. 2018;5(1):72–80. doi:10.1016/j.ijnss.2017.12.011
- Ling DL, Hu J, Zhong MY, Li WT, Yu HJ. Attitudes and beliefs towards implementation of nurse prescribing among general nurses and nurse specialists in China: a cross-sectional survey study. Nurs Open. 2021;8(5):2760–2772. doi:10.1002/nop2.852
- Chen H, Li S-N, Jia R-J, Liu C, Zhu D-S, Ma X-L. Practice of the construction and management of TCM nursing outpatient service—takes a breast specialty in a third-grade hospital in Beijing as an example. TMR Integr Nurs. 2021;5(6):178–181. doi:10.53388/TMRIN2021178181
- Wei P, Zhang Y, Wu S, et al. Current situation and influencing factors of traditional Chinese medicine nursing clinic in Henan Province. J Healthc Eng. 2022;2022:8941922. doi:10.1155/2022/8941922
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi:10.1093/intqhc/mzm042
- Campbell S, Greenwood M, Prior S, et al. Purposive sampling: complex or simple? Research case examples. J Res Nurs. 2020;25(8):652–661. doi:10.1177/1744987120927206
- Naderifar M, Goli H, Ghaljaie F. Snowball sampling: a purposeful method of sampling in qualitative research. Strid Develop Med Educ. 2017;14(3). doi:10.5812/sdme.67670
- Francis JJ, Johnston M, Robertson C, et al. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health. 2010;25(10):1229–1245. doi:10.1080/08870440903194015
- Kuckartz U, Rädiker S. Qualitative Content Analysis: Methods, Practice and Software. 2nd ed. London, UK: SAGE Publications; 2023.
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi:10.1177/1049732305276687
- Lücker P, Henning E, Kästner A, Hoffmann W. Inactive nurses’ willingness to return to active nursing during the COVID-19 pandemic: a qualitative study. J Adv Nurs. 2024;80(3):1043–1057. doi:10.1111/jan.15881
- Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–115. doi:10.1111/j.1365-2648.2007.04569.x
- Downe-Wamboldt B. Content analysis: method, applications, and issues. Health Care Women Int. 1992;13(3):313–321. doi:10.1080/07399339209516006
- Cho JY, Lee E-H. Reducing confusion about grounded theory and qualitative content analysis: similarities and differences. Qual Rep. 2014;19(32):1–20.
- Holmes AGD. Researcher Positionality-A consideration of its influence and place in qualitative research-A new researcher guide. Shanlax Int J Educ. 2020;8(4):1–10. doi:10.34293/education.v8i2.1477
- Fan X, Meng F, Wang D, et al. Perceptions of traditional Chinese medicine for chronic disease care and prevention: a cross-sectional study of Chinese hospital-based health care professionals. BMC Complement Altern Med. 2018;18(1):209. doi:10.1186/s12906-018-2273-y
- Zhong W, Huang H, Li Y. The demand on Chinese medicine nursing consultation among outpatients. J Nurs Administrat. 2013;13(3):186–188.
- Karimi-Shahanjarini A, Shakibazadeh E, Rashidian A, et al. Barriers and facilitators to the implementation of doctor-nurse substitution strategies in primary care: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2019;4(4):Cd010412. doi:10.1002/14651858.CD010412.pub2
- McDonnell A, Goodwin E, Kennedy F, Hawley K, Gerrish K, Smith C. An evaluation of the implementation of Advanced Nurse Practitioner (ANP) roles in an acute hospital setting. J Adv Nurs. 2015;71(4):789–799. doi:10.1111/jan.12558
- Browall M, Forsberg C, Wengström Y. Assessing patient outcomes and cost-effectiveness of nurse-led follow-up for women with breast cancer - have relevant and sensitive evaluation measures been used? J Clin Nurs. 2017;26(13–14):1770–1786. doi:10.1111/jocn.13496
- Lim WY, Papageorgiou N, Sukumar SM, et al. A nurse-led implantable loop recorder service is safe and cost effective. J Cardiovasc Electrophysiol. 2019;30(12):2900–2906. doi:10.1111/jce.14206
- Reddy B, Fan AY. Incorporation of complementary and traditional medicine in ICD-11. BMC Med Inform Decis Mak. 2022;21(Suppl 6):381. doi:10.1186/s12911-022-01913-7
- Wei L, Yu W, Liu Y, et al. Investigation on the establishment and practice of Chinese medicine nursing clinic. Chin Nurs Res. 2020;34(15):2771–2774.
- Zhan Q, Shang S, Li W, Chen L. Bridging the GP gap: nurse practitioners in China. Lancet. 2019;394(10204):1125–1127. doi:10.1016/s0140-6736(19)32209-3
- Pouresmail Z, Nabavi FH, Rassouli M. The development of practice standards for patient education in nurse-led clinics: a mixed-method study. BMC Nurs. 2023;22(1):277. doi:10.1186/s12912-023-01444-0
- Martsolf GR, Gordon T, Warren May L, Mason D, Sullivan C, Villarruel A. Innovative nursing care models and culture of health: early evidence. Nurs Outlook. 2016;64(4):367–376. doi:10.1016/j.outlook.2016.02.009
- Lennan E, Vidall C, Roe H, Jones P, Smith J, Farrell C. Best practice in nurse-led chemotherapy review: a position statement from the United Kingdom Oncology Nursing Society. Ecancermedicalscience. 2012;6:263. doi:10.3332/ecancer.2012.263
- Creedon R, Byrne S, Kennedy J, McCarthy S. The impact of nurse prescribing on the clinical setting. Br J Nurs. 2015;24(17):878–885. doi:10.12968/bjon.2015.24.17.878
- Maier CB. Nurse prescribing of medicines in 13 European countries. Hum Resour Health. 2019;17(1):95. doi:10.1186/s12960-019-0429-6
- Fox A, Joseph R, Cardiff L, et al. Evidence-informed implementation of nurse prescribing under supervision: an integrative review. J Adv Nurs. 2022;78(2):301–313. doi:10.1111/jan.14992
- Zhou Q, Xu Y, Yang L, Menhas R. Attitudes of the public and medical professionals toward nurse prescribing: a text-mining study based on social medias. Int J Nurs Sci. 2023;11(1):99–105. doi:10.1016/j.ijnss.2023.12.005
- Bayat Shahparast F, Piri S. Benefits of prescribing by nurses (with Emphasis on Financial and Economic Benefits): an integrated review. J Nurs Educ. 2023;12(2):36–47.
- Cooper MA, McDowell J, Raeside L. The similarities and differences between advanced nurse practitioners and clinical nurse specialists. Br J Nurs. 2019;28(20):1308–1314. doi:10.12968/bjon.2019.28.20.1308
- Weeks G, George J, Maclure K, Stewart D. Non-medical prescribing versus medical prescribing for acute and chronic disease management in primary and secondary care. Cochrane Database Syst Rev. 2016;11(11):Cd011227. doi:10.1002/14651858.CD011227.pub2
- Farrell C, Molassiotis A, Beaver K, Heaven C. Exploring the scope of oncology specialist nurses’ practice in the UK. Eur J Oncol Nurs. 2011;15(2):160–166. doi:10.1016/j.ejon.2010.07.009
- Cai Y, Boyd DL. Effect of a traditional Chinese medicine course for undergraduate nursing students: a pre-/post-test study. Nurse Educ Today. 2018;70:87–93. doi:10.1016/j.nedt.2018.08.013
- Li S, Cao M, Zhu X. Evidence-based practice: knowledge, attitudes, implementation, facilitators, and barriers among community nurses-systematic review. Medicine. 2019;98(39):e17209. doi:10.1097/md.0000000000017209
- Wilkinson J, Carryer J, Budge C. Impact of postgraduate education on advanced practice nurse activity - a national survey. Int Nurs Rev. 2018;65(3):417–424. doi:10.1111/inr.12437
- Yahia EA, Ali SR. Evaluation of nurse-led patients education using telehealth and artificial intelligence on selected outcomes among orthopedic patients with restricted mobility. Assiut Sci Nurs J. 2023;11(37):14–21.