Abstract
Congenital syphilis (CS), previously considered by many paediatricians as a “historical disease”, has re-emerged as a significant preventable neonatal infection. While low-income countries have the highest burden of disease globally, notifications have increased in many high-income countries (HIC) in recent years. This literature report provides an overview of the current strategies for testing and treating syphilis in pregnancy (SIP) and CS and describes the changing global epidemiology of SIP. National SIP guidelines are reviewed with reference to testing in pregnancy and treatment of CS. The report highlights that there is an ongoing crisis of CS in HICs worldwide and a disproportionate burden is being experienced by vulnerable populations in these countries. Action is needed to address this crisis, and interventions aimed at overcoming social and structural barriers to antenatal care access for vulnerable populations should be prioritised.
Keywords:
Introduction
Despite an estimated decrease in the global incidence of CS of 12% between 2012 and 2016, the disease has re-emerged as a major public health concern in HIC where rates have historically been very low.Citation1–6 Data suggests that the rise in CS disproportionately affects the vulnerable populations in these countries.Citation1,Citation2,Citation7–16 While the African region holds the highest burden of the disease – estimated by the World Health Organization (WHO) as 62% of the worldwide CS burden, this review will focus on this trend in HIC.Citation17
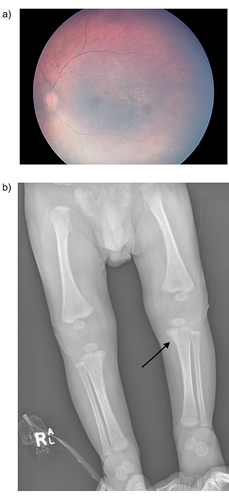
Congenital syphilis (CS) is caused by the vertical transmission of Treponema pallidum. Syphilis has been named “the great mimicker”, and the consequences of CS are both varied and devastating. In cases where SIP goes untreated, 67% of women will have an adverse outcome of pregnancy, including 26% who will have a fetal loss or stillbirth.Citation18 Infants that survive may develop serious short- and long-term health consequences including meningitis, anaemia, bone abnormalities, and other disability.Citation19 Diagnosis can be difficult given that neonates are often asymptomatic at birth. In addition to specific syphilis testing, investigations for an infant at risk of CS should include ophthalmology examination, chest and long bone radiographs, assessment of cerebrospinal fluid (CSF), full blood count (FBC), and blood chemistry (see ).Citation20
Figure 1 Typical features of congenital syphilis. (a) Chorioretinitis as evidenced by mottled “salt and pepper” pigmentary retinal changes on fundoscopy. (b) Early erosions of the mid metaphysis of the distal femur and medial proximal tibia (Wimberger’s sign – see arrow) and generalised periostitis on long bone X-ray. Reprinted from Wu MX, Moore A, Seel M, et al. Congenital syphilis on the rise: the importance of testing and recognition. Med J Aust. 2021;215(8):345–346 e341. © 2021 AMPCo Pty Ltd.Citation19
With universal antenatal screening, SIP can be effectively treated with administration of penicillin, and thus CS is entirely preventable.Citation21 The WHO EMTCT program is a global initiative for the elimination of mother-to-child transmission (MTCT) of HIV, syphilis, and hepatitis B virus.Citation22 In 2014, WHO released the first edition of the global EMTCT guidance, the “Orange Book”,Citation23 to provide guidance for quality healthcare provision, interventions, and monitoring in order to make progress towards elimination. As of 2023, 17 countries have been validated by WHO to have achieved elimination of MTCT of syphilis to a level where it is no longer a public health threat – most of which are lower- and upper-middle income countries, as well as some small HIC including Oman and Anguilla.Citation24
Methodology
An exhaustive literature search was performed of databases including PubMed, Cochrane Library, UptoDate, CINAHL, and ClinicalKey. Papers published in the last decade were screened for review in more detail based on the relevancy of their titles and abstracts. Relevant epidemiological data were extracted and collated for the review.
Epidemiology of Congenital Syphilis – Rising Numbers in High Income Countries
Western Pacific Region
In Australia, 2020 marked the highest number of cases (n=17) diagnosed in one year since 2001.Citation7 Twenty-four cases of CS were reported in New Zealand from 2017 to 2021 where prior to 2016, there had been only one reported case which was in 2011.Citation25 In China, CS rates have increased from 0.01/100 000 live births in 1991, to 19.68/100 000 live births in 2005, which is an average yearly rise of 71.9%.Citation26 This prompted the 2010 issue of the 10-year Plan for Syphilis Control and Prevention in China, with a goal to reduce CS to <15/100 000 live births. As a result, increased coverage of testing for pregnant women, increased treatment of SIP and prophylactic treatment of newborns born to women with SIP were effectively implemented.Citation27 Between 2011 and 2018, CS incidence in China reduced from 91.6/100 000 cases per live births to 18.4/100 000.Citation27 During this time, rates of SIP continued to increase, however MTCT and CS decreased.Citation27 In Japan, syphilis cases have increased to levels not seen since the 1970s, including a pronounced increase in cases in heterosexual men and women and a concomitant rise in CS.Citation5,Citation6
Region of the Americas
In the United States (US), CS rates have increased almost every year since 2012.Citation2 From a record low of 8.4 cases per 100000 live births in 2014, there has been a 927% increase to 77.9 cases per 100 000 live births in 2021. This is a 319% increase in 5 years alone, from 24.4/100 000 live births in 2017.Citation2 In 1998, Canada announced a national goal of maintaining syphilis rates less than0.5/100 000 population.Citation28 Despite this, syphilis cases began to steadily increase in the early 2000s, with a more rapid increase since 2017. From 2016 to 2020, infectious syphilis rates among females alone increased by 773%, compared to a 73% increase in rates among males. Ninety-six CS cases were reported in 2021Citation29 – a massive increase from 4 reported cases in 2016(2400% increase), and a maximum of 10 reported each year between 2011 and 2017.Citation1 Mexico reported an increased incidence of syphilis between 2010 and 2019, most concentrated in the population of reproductive age, with a notable increase in cases in women aged 24–29 years old.Citation3 Alongside this, an exponential growth in CS cases has been reported, with 372 cases reported in 2019 compared to 62 cases in 2010.Citation3
European Region
In England, infectious syphilis cases are increasing among women in particular, with rates in 2022 the highest since 1948, and demonstrating a 236% increase since 2014.Citation30 The rate of SIP has been steadily increasing, with a rise from 56/100 000 women between 2016 and 2017 to 72/100 000 women between 2020 and 2021. There were 39 confirmed cases of CS in England between January 2015 and December 2021.Citation15,Citation31 In 2019, 72 confirmed cases of CS were reported in the European Union/European Economic Area (EU/EEA), marking the 2nd consecutive year in which case numbers have notably increased. Previously, CS rates across the EU/EEA had been steadily declining since 2010, with just 44 cases in 2016. The vast majority of cases in recent years occurred in Bulgaria, followed by Portugal.Citation4
Testing in Pregnancy (See )
Table 1 National Guidelines for Testing and Treatment of SIP in Select HICs
Table 2 National Guidelines for Testing for and Treatment of CS in Select HICs
WHO guidelines recommend testing all pregnant women for syphilis during the first antenatal care visit.Citation21 Trinh et al reviewed 62 STI treatment guidelines published during 2003–2017, representing 128 countries. Fifty-seven (92%) of the guidelines recommended universal syphilis testing in pregnancy and 46 (81%) recommended initial testing early in pregnancy. In addition to universal testing at the first antenatal visit, 21 (46%) guidelines recommended repeat syphilis testing in the third trimester or at delivery.Citation44,Citation45 Many guidelines include repeat syphilis testing for at-risk populations in the third trimester and at delivery, with most guidelines specifying risk factors that would meet this criterion. Common identified risk factors include multiple sexual partners, illicit drug use, incarceration, homelessness, or living in areas with high syphilis prevalence or experiencing outbreaks.Citation20,Citation33 Numerous cases of CS have occurred after a woman tested negative on initial antenatal bloods and was not re-tested due to not being identified as “at-risk” – an assumption that can be subjective.Citation8,Citation11,Citation46,Citation47 WHO does not specifically recommend repeat testing in current guidelines, but an increasing number of individual jurisdictions are now recommending routine universal additional testing in the third trimester for all women. Of the 62 guidelines included in the study by Trinh et al, 57 (92%) recommend universal syphilis testing during pregnancy and 46 (74%) recommend repeat testing in pregnancy, including 21 (46%) that recommend this be done in the third trimester or at delivery. Of the 115 countries with maternal syphilis seroprevalence data available, 40 (35%) recommend universal repeat testing in pregnancy and 52 (45%) recommend repeat universal testing only for high-risk women. The study also found that countries with SIP rates 1% or higher were more likely to recommend universal repeat testing.Citation45
Australian guidelines are state-based, and most recommend syphilis testing for women in pregnancy at the first antenatal visit, as well as re-testing for women at high risk of infection or reinfection at 28–32 weeks and at delivery, or more frequently depending on the level of risk.Citation20,Citation37–39 Universal retesting of all women is recommended in Queensland (QLD) Citation20 and Western Australia (WA) at 28 and 36 weeks.Citation38 The New Zealand Sexual Health Society (NZSHS) official national guideline currently advises routine syphilis testing as part of first antenatal bloods, but NZSHS has since released a statement strongly recommending that all pregnant women be retested for syphilis at 28–32 weeks.Citation42 A study of CS cases in the US in 2018 found that half of all reported cases that year could be attributed to gaps in prenatal testing and treatment including inadequate treatment of diagnosed SIP, inadequate testing, or acquired infection after initial negative testing in a woman not identified as high risk.Citation46 US guidelines now recommend testing of all pregnant women at the first prenatal visit and additionally for high risk women at 28 weeks and at delivery.Citation33 Studies in the US found that universal third trimester syphilis re-testing would cost an additional $420 000 US dollars to prevent each case of CSCitation48 and was not cost effective in areas of low CS prevalence <3.5/100 000 live births.Citation49 Given the increased prevalence in recent years, at 77.9 cases per 100 000 live births in 2021,Citation2 the cost vs benefit analysis should be revisited. Canadian guidelines recommend routine testing at first prenatal visit, with re-testing at 28–32 weeks and at delivery for those at ongoing risk of infection or reinfection, or in areas experiencing outbreaks of syphilis.Citation34 UK guidelines recommend routine testing in early pregnancy. Twenty-two (56%) babies born with CS in England between 2015 and 2021 were born to women who tested negative for syphilis during initial antenatal testing.Citation15,Citation31 However, routine re-testing later in pregnancy has been considered and is not recommended, after a 2020 review by the United Kingdom National Screening Committee deemed that it would cost 1.8 million pounds to prevent one case of CS and is therefore not cost effective.Citation35
There are a number of issues that arise from retesting only high-risk women. A risk-based retesting approach is not consistently effective as this method depends on accurate and consistent identification of risk. In multiple countries employing this method, CS cases have resulted where pregnant women tested negative for syphilis at initial antenatal screening, and were not rescreened later in pregnancy due to not being identified as high-risk.Citation15,Citation31,Citation42,Citation50,Citation51 A risk-based retesting approach may result in perceived stigmatization of some womenCitation42,Citation52 - women may not disclose their high-risk status due to perceived stigma or a lack of awareness of high-risk demographics and sexual practices.Citation52 Likewise, healthcare professionals may make assumptions of risk profiles and not thoroughly and explicitly explore all risk factors with every woman.Citation44 On the other hand, cost vs benefit is a consideration in most countries, and false-positive results are not insignificant, and can be a result of infection, vaccinations, autoimmune disease, older age, IVDU and pregnancy.Citation36,Citation53 In the UK in 2011, 23% of women with positive maternal treponemal serology had false-positive test results.Citation36
Given the dynamic nature of cost vs benefit assessments, limitations of risk-based re-testing, and the rapidly rising rates of CS, it is imperative that all HICs review their guidelines and consider introducing recommendations for universal syphilis re-testing for all women in the third trimester.
Treatment of SIP (See )
WHO recommends treatment of primary, secondary, or early latent syphilis in pregnancy with a single dose of benzathine penicillin G (BPG) 2.4 million units (MU) intramuscularly (IM), or if BPG is unavailable, procaine penicillin 1.2 MU IM once daily for 10 days.Citation32 IM penicillin is recommended as first-line therapy for the treatment of syphilis in pregnant women in 95% of the guidelines reviewed by Trinh et al.Citation45 Six (10%) of these recommended a single dose regardless of syphilis stage (less than WHO-recommended management), and 8 (14%) recommended 3 doses regardless of stage/duration. Depending on local laboratory capacity and clinician expertise, it can be difficult to reliably differentiate the various stages of syphilis,Citation34 and as such treatment guidelines vary. WHO recommends treatment for SIP of unknown stage/duration as per late latent syphilis, with 3 weekly doses of BPG 2.4 MU IM over 3 consecutive weeks. The WHO guideline offers oral erythromycin or IM ceftriaxone as alternative for treatment of SIP but specifies that they do not treat or prevent CS in the foetus. Forty-two (68%) of the guidelines offered at least one alternative to penicillin, and only 20 (48%) of those specified that it would not treat or prevent CS. Most guidelines (48% of those reviewed by Trinh et al) advise desensitisation for those allergic or hypersensitive to penicillin.Citation45
Diagnosis and Treatment of CS (See )
To assist the clinician, there are many available updated guidelines and reviews addressing the diagnosis and treatment of CS, most of which are generally in agreement.Citation20,Citation36,Citation44 CS should be considered in any newborn with clinical suspicion of CS, or where the mother had suspected or confirmed SIP without documentation of completion of adequate and appropriate treatment at least 30 days prior to delivery. Definitive diagnosis of CS can be complex as maternal treponemal and nontreponemal IgG antibodies can be transferred via the placenta, complicating interpretation of reactive tests in neonates. Additional factors must be considered, including stage of diagnosed SIP, adequacy and timing of SIP treatment, clinical, laboratory and radiographic findings consistent with CS and comparison of maternal and neonatal nontreponemal test (NTT) titres. Serum NTTs should be performed on all neonates with suspected CS, as umbilical cord blood is at risk of contamination with maternal blood. A serum NTT titre that is 4x higher than the mothers NTT titre (on the same type of NTT) at delivery should be considered a confirmed case of CS.Citation40
Ten days of IV penicillin is universally recommended as treatment for CS, with age-dependent dosing in most guidelines. A common scenario that occurs in infants born to mothers with SIP is when the infant has no clinical signs concerning for CS and has negative tests (NTT titre is equal to or less than the maternal titre and treponemal IgM is negative), but there is no documentation of adequate and appropriate treatment of SIP at least 30 days prior to delivery, with proven serologic response to treatment. Many guidelines from HICs recommend erring on the side of caution in this scenario and treating the newborn with 10 days of IV penicillin.Citation20,Citation41 However, some guidelinesCitation41 recommend a single dose of IM benzathine penicillin in these circumstances, provided that a complete evaluation of the infant has occurred (FBC, CSF, and imaging) and is normal, and follow up is ensured.Citation54
Congenital Syphilis in High Income Countries – Vulnerable Populations Disproportionately Affected
There is a common theme among many HIC, of disproportionately high rates of infectious syphilis and CS in Indigenous and socially vulnerable populations, due to social and structural barriers to care.Citation1,Citation2,Citation7–16
Indigenous Populations
In Australia, yearly rates of CS during the past decade are on average almost 20x higher in Aboriginal and Torres Strait Islander infants (see ).Citation7 Of note, 31 (53%) of the 58 CS cases reported Australia-wide between 2011 and 2020 were Aboriginal and/or Torres Strait IslanderCitation10 and of 62 CS cases reported between 2016 and September 2022, 52 (81%) were born to mothers diagnosed with syphilis late in pregnancy, including 10 cases diagnosed within 30 days of delivery.Citation7 Of the 18 deaths from CS reported between 2016 and September 2022, 12 (67%) were Aboriginal and/or Torres Strait Islander infants.Citation7 A study of SIP and CS in WA reported on the 9 cases of CS diagnosed between January 2019 and June 2021. All women had infrequent, or no antenatal care. Seven of the 9 cases were born to Aboriginal and/or Torres Strait Islander women, the majority of whom had unstable housing and complex social issues.Citation11 A study examining infectious syphilis rates among different demographics in Australia from 2011 to 2019 identified factors associated with significantly higher notification rates, including Aboriginal and Torres Strait Islander communities, areas of socio-economic disadvantage and IVDU.Citation9 Social factors impacting the sexual health of Aboriginal and Torres Strait Islander people include barriers to healthcare access, poverty, substance use, and social and educational disadvantage.Citation12
Figure 2 CS notification rates by year and Indigenous status of mother – Australia 2017–2021. Y axis = number of notifications. X axis: Aboriginal and/or Torres Strait Islander (blue), Other Australians (Orange).
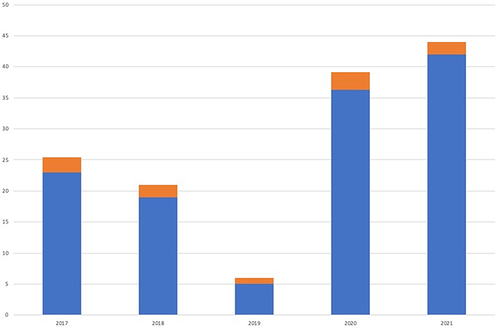
In New Zealand, 24 cases of CS were identified between 2017 and 2021. Fourteen (58%) of these occurred in women who had late, or no antenatal care and 6 (25%) were new infections in pregnancy, after initially testing negative for syphilis. The highest yearly rate was 8 cases in 2020, all of which were born to Māori (n=6) or Pacific Islander (n=2) women.Citation8
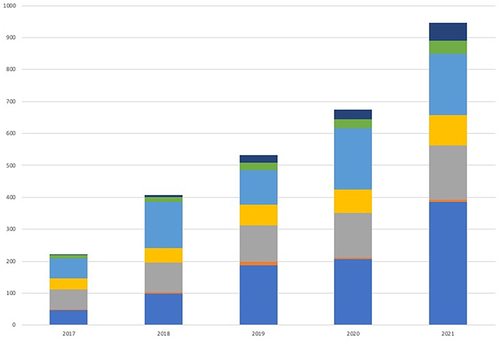
In the US in 2021, CS rates were disproportionately higher in racial and ethnic minority groups than in white Americans, including American Indian/Alaska Native (9.4x higher), Native Hawaiian/Pacific Islander (4.7x higher), African American (4.1x higher), and Hispanic populations (2.3x higher)Citation2 (see ). CS rates were also disproportionately high for those living in poverty, and illicit drug users.Citation2,Citation13 A recent study of CS hospitalisations in MississippiCitation55 found a 1000% increase from 10 hospitalisations in 2016 to 110 in 2022 and identified significant racial and socioeconomic disparities. Over 71% of infants hospitalised with CS between 2016 and 2022 were African American, and 91% were covered by the Medicaid program, which was used in this study as an indicator for low socioeconomic status.
Figure 3 CS notification rates by year and race/Hispanic ethnicity of mother – US 2017–2021. Y axis = number of notifications. X axis: American Indian or Alaska Native (blue), Black or African American (gray), Native Hawaiian or other Pacific Islander (light blue), Multiracial (dark blue), Asian (Orange), Hispanic or Latino (yellow), White (green).
In recent years, syphilis outbreaks in Canada have disproportionately affected First Nations, Métis and Inuit populations.Citation14 In Canada in 2020, 86% of all confirmed CS cases were within the three Prairie provinces alone.Citation1 Incomplete antenatal care has been identified as a major risk factor for CS, and this can be associated with social and structural health determinants including low income, living in rural areas, housing instability, domestic violence, cultural barriers, stigma, discrimination and racism, and substance use.Citation14
Disproportionate rates of CS among Indigenous and disenfranchised populations are linked to structural, social, economic, and cultural barriers to care often as a result of racial and socioeconomic inequity.Citation14,Citation43,Citation56,Citation57 Historical racism, discrimination, and exploitation of Indigenous populations in HICs results in intergenerational trauma and mistrust of healthcare professionals and the healthcare system.Citation58,Citation59 As a result, Indigenous populations are vulnerable to missed healthcare opportunities due to avoidance and lack of engagement with the healthcare system.Citation58–60 A 2022 reportCitation61 on cultural safety in health care for Indigenous Australians was based on data collated from a number of surveys of the general Australian population and of patients in Australian public hospitals. It found that in 2020, 22% of Indigenous Australians reported that they or their families had been racially discriminated against by medical professionals in the previous year and that in 2018–2019, 32% of Indigenous Australians who did not access health care when needed attributed this to cultural barriers including language, discrimination, and lack of access to culturally appropriate health care.Citation61 A 2016 studyCitation62 of Intuit youth in Nunavut, Canada, identified factors affecting access to sexual and reproductive health care. Major barriers to care include lack of trust in healthcare providers, stigma and taboo surrounding sexual health, and feelings of powerlessness that particularly affect female Intuit youth, and are compounded by sexual abuse and violence.Citation62 An understanding of intersectionality in these populations is important; other risk factors for syphilis (substance misuse, remote living, low education levels, socio-economic disadvantage, poverty) are more prominent in Indigenous populations and in turn contribute to their relative risk.Citation62–64
Other Disadvantaged Populations
There is a similar theme of inequitable distribution of infectious syphilis and CS in HICs that do not have large Indigenous populations, where disproportionately high numbers occur in disenfranchised and socially vulnerable populations. In England in 2022, the rate of infectious syphilis in the population with black ethnicity was 80% higher than the rate in those of white ethnicity. The rate of infectious syphilis in the most deprived areas (index of multiple deprivation (IMD) quintile 1) was approximately 2.5x higher than that of the least deprived areas (IMD quintile 5).Citation30 A retrospective review of case reports of all confirmed and suspected cases of CS in England since 2015Citation15 identified a number of risk factors including lifestyle (IVDU, sex work), incarceration, social inequalities, and poor engagement with health services resulting in late or no antenatal care. A third of women diagnosed with SIP in 2020 reported complicating social issues including mental health challenges (13.6%), social services involvement (12.3%), housing concerns (9.7%), domestic violence (7.7%), and substance misuse (7.2%), and half were unemployed.Citation15 Although there are comparatively low rates of CS in England, it remains a public health concern due to the devastating outcomes, and the health inequity that it represents.Citation36,Citation65
Geographical distribution of syphilis and CS cases in China remains disproportionately concentrated in some counties, with the vast majority of CS cases occurring within 5 provinces.Citation27,Citation66 Risk factors such as rural-to-urban migration, stigma, and suboptimal routine testing may contribute to this disparity.Citation16 The proximate determinants of syphilis spread are poorly understood, and further research is required to assess the contributing factors.Citation27
Optimisation of antenatal testing and treatment services will not overcome the structural barriers to seeking antenatal care. The data indicates that many individuals in vulnerable populations – including but not limited to Indigenous populations – eg victims of domestic violence and control, those who misuse substances, and those living in poverty – do not have the education, empowerment, and resources to seek antenatal care.Citation67–69 Major structural barriers that these women face include (1) lack of health literacy and limited understanding of the risks of sexually transmitted infections and MTCT, (2) lack of empowerment to seek antenatal care, compounded by stigma, racism, and discrimination, and (3) poverty and a lack of resources to facilitate healthcare attendance.Citation67–69 In order to address the crisis of CS and implement effective preventative strategies, the social inequity, discrimination, and intersectionality that it represents must first be acknowledged and understood. National structural strategies must be implemented to achieve locally effective change.
Public Health Initiatives
Many HICs have initiated public health campaigns in response to increasing CS rates. In Australia, the Fourth National Sexually Transmissible Infections Strategy 2018–2022 was published in 2019.Citation70 It aims to implement effective programs targeting priority populations with a focus on human rights, reducing stigma and discrimination and improving access and equity, as well as closing the gap between Aboriginal and Torres Strait Islander health status and that of other Australians.Citation70 New Zealand launched the National Syphilis Action Plan in 2019, which includes a plan for increased health promotion and awareness among high-risk groups and improving affordable and equitable health care, with a focus on addressing barriers to access for Māori women in particular.Citation71 In January 2021, the US Department for Health and Health Services launched the Sexually Transmitted Infections National Strategic Plan in response to the rise in STIs. The five-year plan aims to improve STI prevention and treatment with a focus on public health, health disparities, stigma, and the social determinants of health.Citation72 Specifically, it targets a reduction in CS rates of 15% by 2025 and 50% by 2030, with specific targets for reduction of cases in American Indian and African American populations.Citation72 Multiple US state-based innovative initiatives have been launched in an attempt to address the issue of CS as a result of barriers to healthcare access. These include a podcast launched by the Department of State Health Services in Texas, strategizing sessions to address CS launched by the Oklahoma State Department of Health, and the implementation of 9 regional CS case review boards in Louisiana to identify missed opportunities for prevention.Citation43 In 2019, the Public Health Agency of Canada (PHAC) established the Syphilis Outbreak Investigation Coordinating Committee (SOICC) with the aim to share syphilis epidemiology and best practices on territorial, state, and federal levels.Citation1
Discussion
Syphilis screening in pregnancy, whether performed through traditional or reverse sequence algorithms, reliably picks up syphilis infections. It appears that many HICs that are experiencing increasing rates of CS have updated their guidelines to recommend additional testing following testing at first antenatal visit, particularly for high-risk women and in areas experiencing infectious syphilis outbreaks. HIC where prevalence of CS is becoming particularly high should make it a priority to update their official guidelines and consider universal re-testing for all women in the third trimester.
With these measures in place, the failure to prevent CS in HIC is largely due to missed opportunities for recommended testing, diagnosis, and treatment of SIP.Citation22 Data from HIC indicate that many CS cases are born to women who had late, or no antenatal care and therefore would have been missed diagnoses during pregnancy regardless of guidelines that recommend repeat testing in pregnancy.Citation8,Citation11,Citation73 Barriers to adequate antenatal care are numerous and challenging to address and include structural barriers such as financial pressure, communication and language barriers, lack of transportation and childcare, and inability to take time off work, as well as social barriers such as domestic and family violence, mental health issues, stigma, racism, discrimination, and lack of trust in healthcare providers.Citation9 Inadequate contact tracing also contributes to rising numbers of SIP. Many sexual contacts remain undetected and untreated if traditional contact tracing methods are employed.
Conclusion
There is a crisis of CS in HIC worldwide, with rising cases disproportionately affecting vulnerable populations. It is unacceptable that we are seeing this trend in countries that have widespread availability of penicillin and ample resources for education, testing, and treatment. Worldwide efforts in the first decade of the century led to significant reductions in CS rates across the globe. A global effort is needed again now – with a new focus. The imperative aim in HIC should be to address structural and psychosocial barriers that employ community-based interventions, point of care testing and peer led services – this is not a simple goal but encouragingly some countries have recognised these disparities and have begun implementation of committees and programs to address the problem.
Disclosure
The authors report no conflicts of interest in this work.
References
- Aho J, Lybeck C, Tetteh A, et al. Rising syphilis rates in Canada, 2011–2020. Canada Commun Dis Rep. 2022;48(2/3):52–60. doi:10.14745/ccdr.v48i23a01
- Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2021. Atlanta, U.S; 2023.
- Garcia-Cisneros S, Herrera-Ortiz A, Olamendi-Portugal M, Sanchez-Aleman MA. Re-emergence of syphilis in women of reproductive age and its association with the increase in congenital syphilis in Mexico during 2010-2019: an ecological study. BMC Infect Dis. 2021;21(1):1–992. doi:10.1186/s12879-021-06680-w
- European Centre for Disease Prevention and Control. Congenital Syphilis. Annual Epidemiological Report for 2019. Stockholm: ECDC: ECDC; 2022.
- Spiteri G, Unemo M, Mardh O, Amato-Gauci AJ. The resurgence of syphilis in high-income countries in the 2000s: a focus on Europe. Epidemiol Infect. 2019;147:e143. doi:10.1017/S0950268819000281
- Kanai M, Arima Y, Shimada T, et al. Increase in congenital syphilis cases and challenges in prevention in Japan, 2016-2017. Sex Health. 2021;18(2):197–199. doi:10.1071/SH21004
- Health AGDo. National Syphilis Surveillance Quarterly Report, Quarter 3: 1 July to 30 September 2022. Australian Government Department of Health; 2022.
- Ltd. TIoESaR. Sexually Transmitted Infections in New Zealand: Supplementary Annual Surveillance Report 2021. Porirua, New Zealand; 2022.
- Carter A, McManus H, Ward JS, et al. Infectious syphilis in women and heterosexual men in major Australian cities: sentinel surveillance data, 2011-2019. Med J Aust. 2023;218(5):223–228. doi:10.5694/mja2.51864
- Institute. K. HIV, Viral Hepatitis and Sexually Transmissible Infections in Australia: Annual Surveillance Report 2021. Sydney: Kirby Institute, UNSW; 2021.
- Health. GoWADo. Public Health Review of Congenital Syphilis Cases in WA Jan 2019 – June 2021: Summary Report 2021; 2021.
- MacPhail C, McKay K. Social determinants in the sexual health of adolescent Aboriginal Australians: a systematic review. Health Soc Care Community. 2018;26(2):131–146. doi:10.1111/hsc.12355
- Prevention. CfDCa. Health disparities in HIV/AIDS, viral hepatitis, STDs, and TB: African Americans/Blacks. Available from: https://www.cdc.gov/nchhstp/healthdisparities/africanamericans.html. Accessed March 26, 2023.
- Canada. PHAo. Syphilis in Canada, Technical Report on Epidemiological Trends, Determinants and Interventions; 2020.
- Prochazka M, Evans J, Thorn L, Sinka K. Tracking the Syphilis Epidemic in England: 2010 to 2019. London: Public Health England; 2021.
- Tucker JD, Cohen MS. China’s syphilis epidemic: epidemiology, proximate determinants of spread, and control responses. Curr Opinion Infect Dis. 2011;24(1):50–55. doi:10.1097/QCO.0b013e32834204bf
- Gilmour LS, Walls T. Congenital Syphilis: a Review of Global Epidemiology. Clin Microbiol. 2015:e00126–00122.
- Organization WH. Syphilis. Available from: https://www.who.int/news-room/fact-sheets/detail/syphilis. Accessed June 20, 2023.
- Wu MX, Moore A, Seel M, et al. Congenital syphilis on the rise: the importance of testing and recognition. Med J Aust. 2021;215(8):345–346 e341. doi:10.5694/mja2.51270
- Queensland Health. Queensland Clinical Guidelines; 2018.
- World Health Organization. Guideline on Syphilis Screening and Treatment for Pregnant Women. Geneva: World Health Organization; 2017.
- O’Connor NP, Burke PC, Worley S, Kadkhoda K, Goje O, Foster CB. Outcomes After Positive Syphilis Screening. Pediatrics. 2022;150(3). doi:10.1542/peds.2022-056457
- Organization. WH. Elimination of Mother-to-Child Transmission (EMTCT) of HIV and Syphilis. Global Guidance on Criteria and Processes for Validation. Geneva: WHO; 2014.
- Organization WH Validation of elimination of mother-to-child transmission of HIV, syphilis and hepatitis B. Available from: https://www.who.int/initiatives/triple-elimination-initiative-of-mother-to-child-transmission-of-hiv-syphilis-and-hepatitis-b/validation. Accessed June 20, 2023.
- New Zealand Sexually Transmitted Infection (STI) Surveillance Dashboard. Available from: https://www.esr.cri.nz/our-services/consultancy/public-health/sti/. Accessed June 17, 2022.
- Chen Z-Q, Zhang G-C, Gong X-D, et al. Syphilis in China: results of a national surveillance programme. Lancet. 2007;369(9556):132–138. doi:10.1016/S0140-6736(07)60074-9
- Qiao Y, Wang X, Wang Q, Li Z, Jin X, Wang A. Screening and Treatment of Syphilis for Pregnant Women — china, 2011−2018. China CDC Weekly. 2020;2(26):476–480. doi:10.46234/ccdcw2020.123
- Canada. H. Proceedings of National STD Consensus Meeting and National Goals for the Prevention and Control of Sexually Transmitted Diseases in Canada; 1997.
- Canada PHAo. Canada Communicable Disease Report: antimicrobial Use and Stewardship. Canada Commun Dis Rep. 2022;48:587.
- Agency. UHS. Sexually transmitted infections (STIs): annual data tables. UK Government. Health surveillance and reporting programmes. Web site. Available from: https://www.gov.uk/government/statistics/sexually-transmitted-infections-stis-annual-data-tables. Accessed October 13, 2023.
- (ISOSS). ISOSS. ISOSS Syphilis Report 2022. NHS England; 2022.
- World Health Organization. WHO guidelines for the treatment of Treponema pallidum (syphilis). Available from: http://www.who.int. Accessed October 31, 2023.
- Prevention. CfDCa. Sexually Transmitted Infections Treatment Guidelines, 2021: syphilis During Pregnancy. Available from: https://www.cdc.gov/std/treatment-guidelines/syphilis-pregnancy.htm. Accessed April 12, 2023.
- Canada. Go. Syphilis guide: key information and resources. Available from: https://www.canada.ca/en/public-health/services/infectious-diseases/sexual-health-sexually-transmitted-infections/canadian-guidelines/syphilis.html#a1.2. Accessed April 12, 2023.
- Committee. UNS. Antenatal screening programme: syphilis. Antenatal screening programme Web site. Available from: https://view-health-screening-recommendations.service.gov.uk/syphilis/. Accessed May 8, 2022.
- Kingston M, French P, Higgins S, et al. UK national guidelines on the management of syphilis 2015. Int J STD AIDS. 2016;27(6):421–446. doi:10.1177/0956462415624059
- Australian Government Department of Health. Pregnancy Care Guidelines: syphilis. Available from: https://www.health.gov.au/resources/pregnancy-care-guidelines/part-f-routine-maternal-health-tests/syphilis#:~:text=Notification%20of%20confirmed%20or%20probable,an%20urgent%20public%20health%20priority.&text=In%20areas%20affected%20by%20an%20ongoing%20syphilis%20outbreak%2C%20recommend%20testing,6%20weeks%20after%20the%20birth. Accessed October 31, 2022.
- Government of Western Australia Department of Health. STI screening recommendations in pregnant and post-partum women. In: Silver Book. Government of Western Australia; 2021.
- Government of South Australia. Management of Syphilis During Pregnancy. Clinical Programs and Practice Guidelines; 2022.
- Centers for Disease Control and Prevention (CDC). Congenital Syphilis. STI Treatment Guideline; 2021.
- Kimberlin DW, Barnett ED, Lynfield R, Sawyer MH; Committee on Infectious Diseases AAoP. Red Book: 2021–2024 Report of the Committee on Infectious Diseases. 32ed. American Academy of Pediatrics; 2021
- The New Zealand Sexual Health Society. NZSHS Position Statement on Re-Testing Pregnant Women for Syphilis Infection or Reinfection. NZSHS Executive Committee; 2020.
- Fang J, Partridge E, Bautista GM. Congenital Syphilis Epidemiology, Prevention, and Management in the United States: a 2022 Update. Cureus. 2022;14(12). doi:10.7759/cureus.33009
- Freyne B, Nourse C, Walls T. Congenital Syphilis: controversies and Questions, A Global Perspective. Pediatr Infect Dis J. 2023;42(5):e166–e169. doi:10.1097/INF.0000000000003808
- Trinh T, Leal AF, Mello MB, et al. Syphilis management in pregnancy: a review of guideline recommendations from countries around the world. Sex Reprod Health Matters. 2019;27(1):69–82. doi:10.1080/26410397.2019.1691897
- Kimball A, Torrone E, Miele K, et al. Missed Opportunities for Prevention of Congenital Syphilis — United States, 2018. MMWR Morb Mortal Wkly Rep. 2016;2020;69:661–665.
- Seiler N, Pearson W, Bachmann L, et al. Congenital Syphilis in the Medicaid Program: assessing Challenges and Opportunities Through the Experiences of Seven Southern States. Women’s Health Issues. 2023;1–10.
- Albright CM, Emerson JB, Werner EF, Hughes BL. Third-Trimester Prenatal Syphilis Screening: a Cost-Effectiveness Analysis. Obstet Gynecol. 2015;126(3):479–485. doi:10.1097/AOG.0000000000000997
- Shiber L, Todia WJ. Cost and clinical utility of repeated syphilis screening in the third trimester in a high-risk population. Am J Obstet Gynecol. 2014;210(3):267 e261–265. doi:10.1016/j.ajog.2013.12.012
- Slutsker JS, Hennessy RR, Schillinger JA. Factors Contributing to Congenital Syphilis Cases - New York City, 2010-2016. MMWR Morb Mortal Wkly Rep. 2018;67(39):1088–1093. doi:10.15585/mmwr.mm6739a3
- Matthias JM, Rahman MM, Newman DR, Peterman TA. Effectiveness of Prenatal Screening and Treatment to Prevent Congenital Syphilis, Louisiana and Florida, 2013-2014. Sex Transm Dis. 2017;44(8):498–502. doi:10.1097/OLQ.0000000000000638
- Traeger M, Stoové M. Why risk matters for STI control: who are those at greatest risk and how are they identified? Sex Health. 2022;19(4):265–277. doi:10.1071/SH22053
- Prevention. CfDCa. Immigrant, Refugee and Migrant Health: syphilis. Available from: https://www.cdc.gov/immigrantrefugeehealth/guidelines/domestic/sexually-transmitted-diseases/syphilis.html#congenital-syphilis. Accessed June 20, 2023.
- Thean L, Moore A, Nourse C. New trends in congenital syphilis: epidemiology, testing in pregnancy, and management. Curr Opin Infect Dis. 2022;35(5):452–460. doi:10.1097/QCO.0000000000000875
- Staneva M, Hobbs CV, Dobbs T. Spike in Congenital Syphilis, Mississippi, USA, 2016-2022. Emerg Infect Dis. 2023;29(10):1965–1972. doi:10.3201/eid2910.230421
- Park E, Harville E, Nelson M, Giarratano G, Buekens P, Wagman J. Gaps in the congenital syphilis prevention cascade: qualitative findings from Kern County, California. BMC Infect Dis. 2022;22(129). doi:10.1186/s12879-022-07100-3
- Eppes C, Stafford I, Rac M. Syphilis in pregnancy: an ongoing public health threat. Am J Obstet Gynecol. 2022;227(6):822–838. doi:10.1016/j.ajog.2022.07.041
- Institute of Medicine Committee on U, Eliminating R, Ethnic Disparities in Health C. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press (US); 2022.
- Brown N. History, Law, and Policy as a Foundation for Health Care Delivery for Australian Indigenous Children. Pediatr Clin North Am. 2009;56(6):1561–1576. doi:10.1016/j.pcl.2009.10.002
- Sebens Z, Williams AD. Disparities in early prenatal care and barriers to access among American Indian and white women in North Dakota. J Rural Health. 2022;38(2):314–322. doi:10.1111/jrh.12649
- Welfare AIoHa. Cultural Safety in Health Care for Indigenous Australians: Monitoring Framework. Australian Insititute of Health and Welfare; 2023.
- Corosky GJ, Blystad A. Staying healthy “under the sheets”: Inuit youth experiences of access to sexual and reproductive health and rights in Arviat, Nunavut, Canada. Int J Circumpolar Health. 2016;75:31812. doi:10.3402/ijch.v75.31812
- Ward JS, Hengel B, Ah Chee D, Havnen O, Boffa JD. Setting the record straight: sexually transmissible infections and sexual abuse in Aboriginal and Torres Strait Islander communities. Med J Australia. 2020;212(5):205–207. doi:10.5694/mja2.50492
- Minichiello V, Rahman S, Hussain R. Epidemiology of sexually transmitted infections in global indigenous populations: data availability and gaps. Int J STD AIDS. 2013;24:759–768. doi:10.1177/0956462413481526
- Simms I, Tookey PA, Goh BT, et al. The incidence of congenital syphilis in the United Kingdom: February 2010 to January 2015. Bjog. 2017;124(1):72–77. doi:10.1111/1471-0528.13950
- Ya-jie X-L, Li J. Spatial distribution characteristics and patterns of congenital syphilis in 2010 and 2015 in China. Chine J Dermatol. 2018;51(5):337–340.
- Chan EYL, Smullin C, Clavijo S, et al. A qualitative assessment of structural barriers to prenatal care and congenital syphilis prevention in Kern County, California. PLoS One. 2021;16(4):e0249419. doi:10.1371/journal.pone.0249419
- Bellerose M, Rodriguez M, Vivier PM. A systematic review of the qualitative literature on barriers to high-quality prenatal and postpartum care among low-income women. Health Serv Res. 2022;57(4):775–785. doi:10.1111/1475-6773.14008
- Escañuela Sánchez T, Linehan L, O’Donoghue K, Byrne M, Meaney S. Facilitators and barriers to seeking and engaging with antenatal care in high-income countries: a meta-synthesis of qualitative research. Health Soc Care Community. 2022;30(6):e3810–e3828. doi:10.1111/hsc.14072
- Australian Government Department of Health. Fourth National Sexually Transmissible Infections Strategy 2018–2022. Canberra; 2019.
- Ministry of Health. National Syphilis Action Plan: An Action Plan to Stop the Syphilis Epidemic in New Zealand. Wellington: New Zealand Government Ministry of Health; 2019.
- Services. USDoHaH. Sexually Transmitted Infections National Strategic Plan for the United States: 2021-2025. Washington, DC; 2020.
- Furegato M, Fifer H, Mohammed H, et al. Factors associated with four atypical cases of congenital syphilis in England, 2016 to 2017: an ecological analysis. Euro Surveill. 2017;22(49). doi:10.2807/1560-7917.ES.2017.22.49.17-00750
