Abstract
Background
Seizure is an occurrence of sudden, paroxysmal, abnormal alteration in electrographic activity at any point from birth to the end of the neonatal period. However, little is known about the number of seizures and the associated factors in the study area. Therefore, this study aimed to estimate the number of seizures and associated factors in neonates admitted with birth asphyxia to the neonatal intensive care unit in the Northwest Amhara Region Comprehensive Specialized Hospitals, Northwest Ethiopia, in 2023.
Methods
A multicenter institution-based retrospective follow-up study was conducted among 423 neonates who had a follow-up visit at Comprehensive Specialized Hospitals of Northwest Ethiopia from October 1, 2019, to January 30, 2023. by reviewing the charts of neonates with asphyxia registered from October 01, 2019, to January 30, 2023. A simple random sampling technique was used to select the study participants. Data were extracted using an abstraction sheet, entered into EPidata version 4.6.0.0, and exported to STATA version 14 for analysis. A negative binomial Poisson regression model was best fitted for both bi-variable and multivariable analyses.
Results
The mean number of seizures was 5.4515 (95% CI], 5.164–5.738) per 28-day follow-up period. Hypoglycemia (AIRR = 1.17, 95% CI = (1.06 1.28), intraventricular hemorrhage (AIRR = 1.16, 95% CI = 1.16 (1.06 1.26), stage two hypoxic-ischemic injury (AIRR=11,49, 95% CI =5.9 22.23), stage three hypoxic-ischemic injury (AIRR = 13.22, 95% CI = (6.80 25.68) were significant.
Conclusions and Recommendations
The current study showed that the mean number of seizures in newborns with perinatal asphyxia was higher than that in newborns without perinatal asphyxia: Hypoglycemia, intraventricular hemorrhage, and hypoxic-ischemic injury in the second and third stages were significant factors in the occurrence of seizures.
Introduction
Perinatal asphyxia (PNA) is a significant global health problem that affects newborns during the perinatal period.Citation1,Citation2 Perinatal asphyxia causes not only mortality but also seizures and short- and long-term neurological development implications, including cognitive and motor impairments, which are almost untreatable events.Citation3
Neonatal seizures are common neurological disorders that affect newborn infants.Citation4 Neonatal seizures are a common and possibly life-threatening medical condition that can cause brain damage and long-term neurological impairment in newborns.Citation5
Globally, the incidence of seizures is 1.5–3/1000 live births.Citation6 In Iran prevalence of 2.4%-9%,Citation7 and 5.5% in IndiaCitation8 in the Netherlands 1.8–2.8 per 1000).Citation9 In Italy, 5.0/1000, 54.9/1000, and 85.6/1000 neonates in the 31st-36th, 28th-30th, and <28 weeks of pregnancy, respectively, experience seizures.Citation10
Previous studies have identified several risk factors for seizures in neonates with PNAs. Accordingly, metabolic disorders, especially hypoglycemia, and hypocalcemia, often reflect brain injury such as ischemia (hypoxic-ischemic injury and/or perinatal ischemic stroke), intracranial infection, intracranial hemorrhage, hypomagnesemia, and infection.Citation11,Citation12 Low APGAR in the 5th minute, the occurrence of infections and seizures within the first day, hypothermia, hypoglycemia, hypoxemia, stages II and III of HIE, acute kidney injury thrombocytopenia and electrolyte imbalance are all factors that represent a major risk for neonatal seizures.Citation13–16
Currently, in underdeveloped countries, particularly Ethiopia, there is no successful or launched approach to therapeutic hypothermia to protect the brain and combat immune cells in the developing brain.Citation17 The primary goal of treating patients with epilepsy is to keep them seizure-free; however, in low-income countries, approximately three-quarters of patients with epilepsy do not receive treatment. In addition, the availability of antiseizure medications is low.Citation18
There are significant barriers to the implementation of this program in developing countries due to lack of resources, lack of information on the epidemiology and determinants of seizures in our countries, especially in the Amhara region, lack of resources for the diagnosis and treatment of seizures with EEG, lack of prevention materials for seizures, such as therapeutic hypothermia rooms, and lack of adequate cardiotocography (CTG) on the labor side. Despite these findings, the mechanisms underlying neonatal seizures remain poorly understood, and further research is needed to identify new risk factors and the interplay between different risk factors. Therefore, this study aimed to determine the number of seizures and factors associated with neonatal birth asphyxia the comprehensive specialized hospitals of the northwest Amhara region in 2023.
Methods
Study Design and Period
A multicenter institution-based retrospective follow-up study was conducted from October 1, 2019, to January 30, 2023. (The data were retrospectively extracted from February/ 2023 to July 2023.
Study Setting
This study was conducted in four specialized hospitals (CSH) in the northwestern Amhara region. These were Felege Hiwot CSH, Tibebe Ghion CSH, Debre Tabor CSH, and Debreberhan CSH. Approximately 8516 newborns were admitted annually at all hospitals and 2045 were neonates with perinatal asphyxia. The average annual numbers of newborns admitted at the FCSH, TGCSH, DTCSH, and DBCSH were 1836, 1920, 1560, and 3200 respectively. These hospitals are the last referral option for other healthcare facilities. These hospitals had neonatal units with mixed medical staff (neonatal nurses, nurses, general practitioners, pediatricians, and other staff). This team, working in collaboration, provides a diagnosis of the neonate’s problem and holistic care, including documentation. The main services provided for neonates with PNA in the neonatal unit include general neonatal care, blood and exchange transfusions, phototherapy, and ventilatory support, such as continuous positive air pressure and the only medications phenobarbitone and phenytoin.Citation11
Population
Source population
Neonates with perinatal asphyxia admitted to the neonatal intensive care units of the Northwest Amhara Region Comprehensive Specialized Hospitals in Northwest Ethiopia.
Study Population
All perinatal asphyxia neonates were admitted to the NICU in selected comprehensive specialized hospitals in the Amhara region in northwest Ethiopia from October 1, 2019, to January 30, 2023.
Inclusion Criteria and Exclusion Criteria
All perinatal asphyxia neonates were admitted to the NICU in comprehensive specialized hospitals in northwest Ethiopia from October 01, 2019, to January 30, 2023. Newborns with incomplete information in their medical charts and lost medical cards were excluded.
Sample Size Determination
The sample size was calculated by using a single population formula by assuming a 95% confidence interval and 5% margin of error, number of seizures, and factors associated with perinatal asphyxia among neonates. Applying the formula n= (z (α/2)) 2 p (1-p)/d2 Where, n= the minimum sample size, z (α/2) is the desired level of confidence interval 95% (1.96). sample size become, n = 383+10% non-respondent rate=423.
A maximum sample (423) was used in this study.
Sampling Technique and Procedure
Four comprehensive specialized hospitals were considered for the study: FHCSH, TGCSH and DBCSH for 550, 360, 480, and 655 per year, respectively. A total of 8180 newborns were admitted to the hospital between October 01, 2019, and January 30, 2023.
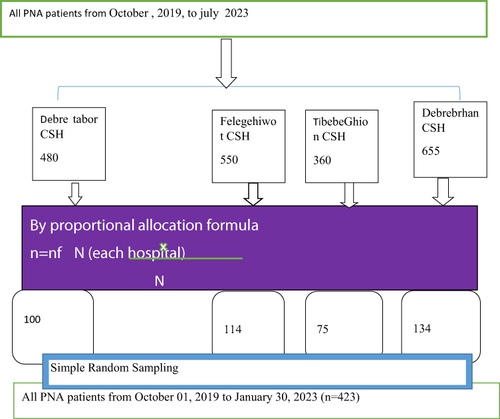
In total, 423 samples were selected from 2045 neonates. Proportional allocation was performed for each hospital based on the final sample size. The sampling frame was prepared by collecting the number of admitted patients from the registration book. After identifying patients who fulfilled the inclusion criteria, study subjects were selected using a simple random sampling technique with lottery methods ().
Variables of the Study
Dependent Variables
Number of Seizure.
Independent Variables
Socio-Demographic Maternal and Neonatal
Sex of the neonate, gestational age, and age of the mother; birth weight; place of delivery.
Maternally Related Factors
Placental hemorrhage, current pregnancy, mode of delivery, prolonged rupture of membranes (PROM), ANC, oligohydramnios, preeclampsia, eclampsia, gestational hypertension, DM, Prolonged labor, and parity.
Clinical Factors
MAS, RDS, IVH, hypoxic-ischemic encephalopathy (HIE), meningitis, and hypoglycemia.
Operational definition
Number of Seizures
The number of seizures was counted based on the physician’s diagnosis on the follow-up sheet.
Perinatal Asphyxia
Inability to initiate and maintain breathing at birth and a 5-minute APGAR score of 7.Citation19
Prolonged Labor is Defined
As the combined duration of the first stage of labor being more than 12 hours in primiparas.Citation20
Prolonged Rupture of Membrane
Duration of rupture of the membrane of the amniotic sac and chorion >18 h till delivery.Citation21
Meconium Stained Amniotic (MAS)
Based on the physician’s diagnosis in the neonatal medical chart with MAS.
Data Collection Tool and Procedure
Data were gathered through a record review using a structured checklist, which was adapted and modified based on various studies. This paper is divided into four sections. Four health professionals with BSC neonatal nurses and three supervisors with MSc from health professionals from other hospitals outside the study units were recruited as data collectors and supervisors, respectively. Charts were retrieved using the patient registration number found in the lottery method, and four data clerks in each hospital supported them by identifying the charts.
Data Quality Assurance
The questionnaire was preliminarily reviewed at the four hospitals to identify important variables, and the quality of the data was further assured through careful planning of the questionnaire to maintain the validity of the tool, which was reviewed by a subject expert. Based on this, modifications were made to the method. These modified variables were neonatal seizures diagnosed by EEG, and the drugs used when neonates developed seizures were modified variables because EEG and pyridoxine were not available in the study settings. A half-day training was delivered to the data collectors and the supervisor aimed at briefing the objective of the study, and what was expected from them. The principal investigator and supervisor checked the collected data daily for its completeness, and corrective measures were taken accordingly.
Data Management and Statistical Analysis
Data were checked, coded, and analyzed using STATA version 14. Descriptive statistics were calculated and presented in tables, graphs, and text (percentages, means, and standard deviations). The assumption was a Poisson distribution regarding the independence of variation, and the mean and variance of the model were checked identically. Multicollinearity was checked using the Variance Inflation Factor (VIF), and the model adequacy was tested by plotting the residuals against the fitted values and an extension of the Poisson family. The negative binomial Poisson regression was selected as the best-fitted model because of the over-dispersion variance of 9.02, which is greater than the mean of 5.45. The best-fit negative binomial regression model was selected. Variables with a p-value of < 0.2 in the bi-variable Poisson regression analysis, were candidates for multivariable analysis. Finally, in the multivariable negative binomial regression analysis, an adjusted incident rate ratio (AIRR) with a 95% CI) was reported to indicate an association between the number of seizures and the associated factors at a P-value of 0.05.
Patient and Public Involvement in This Study
The study participants/public were not directly involved in the design, conduct, reporting, or dissemination of this study.
Result
A total of 423 neonatal charts from February 2023 to January 2023 were included in selected Amhara comprehensive specialized hospitals according to sample size determination; 423 medical charts were included.
Socio-Demographic Characteristics
A total of 423 PNA neonates’ charts were reviewed, and 423 (100%) met the enrollment criteria. In this study, out of 423 neonates, 264 (62.41%) were male. The majority of the neonates, 366 (82.52%) were born in hospitals. The mean (standard deviation) maternal age of the neonates was 29.69 (6.74) years, with 271 (64.07) being between the ages of 20 and 34 ().
Table 1 Socio-Demographic Characteristics of Mothers and Neonates at NICU in Northwest Amhara, Ethiopia, 2023 (n=423)
Obstetrical History of Mother’s and Complications of the Mother
A total of 400 mothers (94.56%) had ANC follow-ups; and of these, 277 (65.48%) had regular ANC follow-ups throughout their pregnancies. The majority of the mothers in the total sample were multipara 246 (58.16%). Among the 423 mothers, 333 (78.12%) had singleton birth In terms of maternal complications, more than one-third of the mothers experienced obstetric complications during the index pregnancy. PROM, eclampsia, preeclampsia, chorioamnionitis, and maternal anemia accounted for 42 (9.93%), 37 (8.75%), 73 (17.26%), 77 (18.20%), and 55 (13.000%) of have maternal obstetric complications in the current pregnancy, respectively ().
Table 2 Obstetric History and Complications Characteristics of Mothers Whose Neonates Were Admitted at NICU in Northwest Amhara, Ethiopia, 2023 (n=423)
Neonatal-Related Factors and Clinical Co-Morbidities
Three fourth of the 337 (79.67%) newborns had a birth weight of more than 2500 g, as can be seen from the 423 newborn records examined. The mean (±SD) birth weight was 3099.53 (±546.24) grams. Regarding gestational age, majority of the babies (349; 82.51%) were born after 37 weeks of gestation. In terms of comorbidities, neonates admitted to the NICU had neonatal MAS, 86 (20.33%) had meningitis, and 126 (29.86%) 202 (47.75%) had jaundice, according to a review of 423 charts ().
Table 3 Neonatal Related and Clinical Co-Morbidities of the Neonates in Northwest Amhara, Ethiopia, 2023 (n=423)
Table 4 Bi-Variable and Multivariable Logistic Regression for the Number of Seizures Among PNA Neonates Admitted to the NICU of Selected Northwest Amhara Comprehensive Specialized Hospitals, Amhara, Ethiopia, 2023. (n=423)
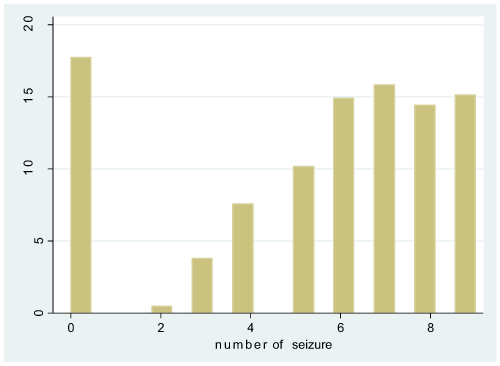
The mean number of seizures among neonates with birth asphyxia was 5.4515 (95% CI: 5.164–5.738) per 28-day follow-up period. The minimum and maximum values are 0 and 9, respectively. About three hundred forty-eight (82.27%) of PNA patients during follow-up had developed recurrent seizures .
Factors Associated with Seizure Among PNA
All independent variables were regressed with the dependent variable in bivariate negative binomial regression analysis. In Bivariable negative binomial regression analysis mode of delivery, prolonged labor, gestational DM, Eclampsia, hypoglycemia, meconium aspiration syndrome, IVH, HIE, and neonatal birth weight due to the number of seizures among PNA were fitted and eligible (p< 0.2) for multivariable analysis ().
The negative binomial regression analysis showed that hypoglycemia, intraventricular hemorrhage, and hypoxic-ischemic injury stage two and stage three variables were significantly associated with the number of seizure recurrences.
The number of seizures was 17% greater among neonates who developed hypoglycemia as compared to not develop hypoglycemia (AIRR = 1.17, 95% CI = (1.06 1.28).Neonates with intraventricular hemorrhage and increases the number of seizures by 16% as compared with the patients without intraventricular hemorrhage (AIRR = 1.16, 95% CI = (1.06 1.26). Besides, patients who had stage 2 hypoxic-ischemic injury increased number of seizures by 49%) compared to those stage 1 hypoxic ischemic injury (AIRR=11.49, 95% CI =5.9 22.23). Moreover, the frequency of seizure rate was 22% times greater in those patients with stage 3 hypoxic-ischemic injury as compared to those with stage 1 hypoxic-ischemic injury (AIRR = 13.22, 95% CI = (6.80 25.68) ().
Discussion
This study aimed to estimate the number of seizures and associated factors among neonates admitted with perinatal asphyxia at comprehensive specialized hospitals in northwest Ethiopia. The results of the current study showed that the mean number of seizures in neonates with perinatal asphyxia patients during the follow-up period was 5.4515 per person for 28 days follow-up (AIRR=5.4515, 95% CI: 5.164–5.738).
The study was lower than that in the previous study, which was conducted in Ireland 28,Citation22 and in the USA greater than 7 and 11,Citation18,Citation23 possibly because all studies were conducted with a prospective study design and the use of EEG is a simple way to determine the number of seizures and risks with the help of imaging.Citation24 However, premature infants were recruited from a different population due to immature brain development, the main seizures occurring early compared to mature infants.Citation23
This study revealed neonates who have been developing hypoglycemia increased the number of recurrences of seizures by 17% as compared with neonates who did not develop hypoglycemia, which is supported by a study conducted in IranCitation7 and China.Citation25 A possible explanation for this is that hypoglycemia increases the main excitatory neurotransmitters (Glutamate, Glycine), which increases the probability of developing seizures.Citation26 Another possible explanation is that as the blood glucose level drops, there is inadequate glucose delivery to the neural tissue and brain, leading to loss of consciousness or seizures.Citation27
This study showed that patients with intraventricular hemorrhage, increased the number of seizures by 16% in patients without intraventricular hemorrhage, which is supported by a study conducted in Italy,Citation10,Citation28 Finland,Citation29 possibly due to a severe form of bleeding in the brain that carries a high risk of injury to brain tissueCitation30 which leads to Internal bleeding and swelling are also characterized by an increased amount of fluid in the brain enlargement of the ventricles and blood clotting in the brain, then the brain signals or electrical impulses are compressed, which can lead to brain cell damage, which in turn triggers seizure.Citation31–33
Neonate stage 2 and stage 3 hypoxic-ischemic injuries increased the number of seizures compared to Stage 1 hypoxic-ischemic injuries by 49% and 22%, respectively. This study was supported by the USA,Citation34 New Zealand,Citation35 the USA,Citation12 and the United Kingdom.Citation36 The possible reason for When hypoxia and ischemia occur, a series of events occur that lead to a decrease in energy production in the brain, which can lead to an increase in glutamate, an excitatory neurotransmitter, and/or a brain messenger that causes excessive activity in the cerebral cortex; in conjunction with an increase in glutamate, there is a lack of reduced neurotransmitters and changes in cell membranes that affect energy production, which leads to hypoxia and ischemia, and can reduce energy production in the brain impulses and seizures.Citation12,Citation34,Citation35
Strengths and Limitations of This Study
This study was conducted in multi-institutions in Amhara Ethiopia (4 hospitals), and it covers a diverse population, which enhances the external validity. However, this study has some limitations such as using a chart review or secondary data source make difficult to assess the number of different types of neonatal seizure. The hospital’s service context and supplies were assessed. Moreover, there is uncertainty regarding the actual number of seizures during the neonatal period due to the lack of facility-based studies with EEG confirmation. In addition,the fact that therapeutic hypothermia is not universally used in all specialized hospitals.
Conclusion
The current study indicated that the mean number of seizures in newborns with birth asphyxia was higher than that reported in other studies conducted on different populations of newborns. Hypoglycemia, intraventricular hemorrhage, and hypoxic-ischemic injury in the second and third stages are significant factors in the occurrence of seizures, and hypoglycemia should be prevented through appropriate nutritional therapy in asphyxiated neonates. Perinatal asphyxia among HIE stages 2 and 3 and intraventricular hemorrhage were strictly followed indoors to reduce the number of seizures. Therapeutic hypothermia is better management for the treatment of birth asphyxia; therefore, all hospitals should use therapeutic hypothermia.
Abbreviations
ANC, antenatal care; APGAR, Activity Pulse Grimace Appearance Respiration; PROM, prolonged rupture of membranes; CSH, comprehensive specialized hospitals; CNS, central nervous system; EEG, electroencephalogram; MAS, meconium aspiration syndrome; NICU, neonatal intensive care unit; RDS, respiratory distress syndrome; VIF: Variance Inflation factor
Ethics Approval
In this study, it was impossible to obtain informed consent from parents or guardians. Ethical approval was obtained from the Institutional Review Board (IRB) of the School of Nursing, College of Medicine and Health Science, University of Gondar (reference No. (Ref.no. SN/036/2015 E.C). A waiver permission letter was obtained from hospital administrators before the data collection and since the neonates were not directly involved in this study (the data were obtained from charts review) informed consent was not required, but extracted data from medical records were kept confidentially. All methods were carried out following the declarations of Helsinki and relevant guidelines and regulations. So, anonymity was maintained by using the identified number instead of the patient’s name. Besides, all data extracted were kept confidential and not used for any other purpose than the stated objective.
Author Contributions
All authors made a significant contribution to the conception, study design, execution, acquisition of data, analysis, and interpretation and took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors do not have competing interest.
Acknowledgment
We would like to acknowledge and express our sincere gratitude to my colleagues for their invaluable comments, suggestions, and support for the proposal, and for providing me with the materials I needed to write. We express our gratitude to the University of Gondar Institutional Review Board for revising this proposal.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are not publicly available due to confidentiality but are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Amare AT. Etiology, clinical features, and short-term outcome of seizures in newborns admitted to the University Of Gondar Hospital, Ethiopia. Pediatric Health, Medicine and Therapeutics. 2019;Volume 10:107–113. doi:10.2147/PHMT.S228241
- Daka DT, Wubneh CA, Alemu TG, Terefe B. Incidence and predictors of mortality among neonates admitted with perinatal asphyxia at west Oromia tertiary hospitals, Ethiopia, 2022. BMC Pediatric. 2023;23(1):475. doi:10.1186/s12887-023-04313-6
- Wosenu L, Worku AG, Teshome DF, Gelagay AA. Determinants of birth asphyxia among live birth newborns in University of Gondar referral hospital, northwest Ethiopia: a case-control study. PLoS One. 2018;13(9):e0203763. doi:10.1371/journal.pone.0203763
- Abend NS, Wusthoff CJ. Neonatal seizures and status epilepticus. J Clini Neuro. 2012;29(5):441–448.
- Lai Y-H, C-S H, Chiu N-C, Tseng C-F, Huang Y-L. Prognostic factors of developmental outcome in neonatal seizures in term infants. Pediatr Neonatol. 2013;54(3):166–172. doi:10.1016/j.pedneo.2013.01.001
- Glass HC. Neonatal seizures: advances in mechanisms and management. Clini Perina. 2014;41(1):177–190. doi:10.1016/j.clp.2013.10.004
- Nemati H, Karimzadeh P, Fallahi M. Causes and factors associated with neonatal seizure and its short-term outcome: a retrospective prognostic cohort study. Iranian J Child Neuro. 2018;12(3):59–68.
- Anand V. Neonatal seizures: predictors of adverse outcome. J Pediatr Neurosci. 2014;9(2):97. doi:10.4103/1817-1745.139261
- Loman AM, ter Horst HJ, Lambrechtsen FA, Lunsing RJ. Neonatal seizures: etiology employing a standardized work-up. European J Pediatric Neuro. 2014;18(3):360–367. doi:10.1016/j.ejpn.2014.01.014
- Pisani F, Facini C, Pelosi A, Mazzotta S, Spagnoli C, Pavlidis E. Neonatal seizures in preterm newborns: a predictive model for outcome. Eur J Paediatr Neurol. 2016;20(2):243–251. doi:10.1016/j.ejpn.2015.12.007
- Amare HT, Amare AT. Etiology, clinical features, and short-term outcome of seizures in newborns admitted to the university of Gondar hospital, Ethiopia. Pedia Health Med Therap. 2019;Volume 10:107–113.
- Pandav K, Ishak A, Chohan F, Edaki O, Quinonez J, Ruxmohan S. Hypoxic-ischemic encephalopathy-induced seizure in an 11-year-old female. Cureus. 2021;13(7):1
- Cavallin F, Menga A, Brasili L, et al. Factors associated with mortality among asphyxiated newborns in a low-resource setting. J Matern Fetal Neonatal Med. 2022;35(6):1178–1183. doi:10.1080/14767058.2020.1743670
- Talebian A, Jahangiri M, Rabiee M, Masoudi Alavi N, Akbari H, Sadat Z. The etiology and clinical evaluations of neonatal seizures in kashan, Iran. Iranian J Child Neuro. 2015;9(2):29–35.
- C-W KIM, JANG C-H, H-M KIM, CHOE B-H, KWON S-H. Clinical characteristics and prognosis of neonatal seizures. J Korean Pedia Soc. 2003;1:1253–1259.
- Al-Momen H, Muhammed MK, Alshaheen AA. Neonatal seizures in Iraq: cause and outcome. Tohoku J Exp Med. 2018;246(4):245–249. doi:10.1620/tjem.246.245
- Cakir U, Ceran B, Tayman C. Two useful umbilical biomarkers for therapeutic hypothermia decision in patients with hypoxic-ischemic encephalopathy with perinatal asphyxia: netrin-1 and neuron-specific enolase. Fetal Pediatr Pathol. 2022;41(6):977–986. doi:10.1080/15513815.2022.2041778
- McBride MC, Laroia N, Guillet R. Electrographic seizures in neonates correlate with poor neurodevelopmental outcome. Neurology. 2000;55(4):506–513. doi:10.1212/WNL.55.4.506
- Ethiopian neonatal intensive care unit national guidline 2021, Ministry of Health. Available from: https://www.slideshare.net/yesuuskiristoos/nicu-2021-ethiopia. Accessed 27 May 2024
- Cunningham FG, Leveno KJ, Bloom SL, Spong CY, Dashe JS. Williams Obstetrics. 24 ed. New York, NY, USA: Mcgraw-Hill; 2014.
- Al-Lawama M, AlZaatreh A, Elrajabi R, Abdelhamid S, Badran E. Prolonged rupture of membranes, neonatal outcomes and management guidelines. J Clini Med Res. 2019;11(5):360. doi:10.14740/jocmr3809
- Rennie JM, de Vries LS, Blennow M, et al. Characterization of neonatal seizures and their treatment using continuous EEG monitoring: a multicentre experience. Arch Dis Childhood-Fetal Neonatal Ed. 2019;104(5):1.
- Glass HC, Shellhaas RA, Wusthoff CJ, et al. Contemporary profile of seizures in neonates: a prospective cohort study. J Pediatr. 2016;174:98–103. e1. doi:10.1016/j.jpeds.2016.03.035
- Boylan GB, Stevenson NJ, Vanhatalo S, editors. Monitoring Neonatal Seizures. Seminars in Fetal and Neonatal Medicine. Elsevier 18(4):202-8; 2013 doi:10.1016/j.siny.2013.04.004
- Yang G, Zou LP, Wang J, et al. Neonatal hypoglycemic brain injury is a cause of infantile spasms. Exp Ther Med. 2016;11(5):2066–2070. doi:10.3892/etm.2016.3107
- Kligman R.M BRE, Jenson HB, Stanton BF. Nelson Textbook of Pediatrics. 21th ed. Philadelphia: Elsevier; 2020.
- De Angelis LC, Brigati G, Polleri G, et al. Neonatal hypoglycemia and brain vulnerability. Frontiers in Endocrinology. 2021;12:634305. doi:10.3389/fendo.2021.634305
- Spagnoli C, Falsaperla R, Deolmi M, Corsello G, Pisani F. Symptomatic seizures in preterm newborns: a review on clinical features and prognosis. Italian J Pedia. 2018;44(1):1–7.
- Hirvonen M, Ojala R, Korhonen P, et al. The incidence and risk factors of epilepsy in children born preterm: a nationwide register study. Epilepsy Res. 2017;138:32–38. doi:10.1016/j.eplepsyres.2017.10.005
- Vasudevan C, Levene M, editors. Epidemiology and Etiology of Neonatal Seizures. Seminars in Fetal and Neonatal Medicine. Elsevier 18(4):185-91; 2013 doi:10.1016/j.siny.2013.05.008
- Özek E, Kersin SG. Intraventricular hemorrhage in preterm babies. Turkish Arch Pedia. 2020;55(3):215.
- Al Yazidi G, Boudes E, Tan X, Saint-Martin C, Shevell M, Wintermark P. Intraventricular hemorrhage in asphyxiated newborns treated with hypothermia: a look into incidence, timing and risk factors. BMC Pediatric. 2015;15(1):1–9. doi:10.1186/s12887-015-0415-7
- Kaur A, Luu TM, Shah PS, Ayoub A, Auger N. Neonatal Intraventricular hemorrhage and hospitalization in childhood. Pediatr Neurol. 2020;103:35–42. doi:10.1016/j.pediatrneurol.2019.09.007
- Jacobs SE, Berg M, Hunt R, Tarnow-Mordi WO, Inder TE, Davis PG. Cooling for newborns with hypoxic ischaemic encephalopathy. Cochrane Database Syst Rev. 2013;2013(1):1.
- Zhou KQ, McDouall A, Drury PP, et al. Treating seizures after hypoxic-ischemic encephalopathy-current controversies and future directions. Int J Mol Sci. 2021;22(13). doi:10.3390/ijms22137121.
- Gunn AJ, Thoresen M. Neonatal encephalopathy and hypoxic-ischemic encephalopathy. Handbook Clin Neurol. 2019;162:217–237.