Abstract
Background
When technically feasible, partial nephrectomy (pN) is preferred over radical nephrectomy (rN) due to similar oncological control with preservation of renal function. Here, we evaluate the incorporation of pN into practice for small renal masses and examine the associated outcomes.
Methods
We included patients who had undergone either a partial or radical nephrectomy in Alberta, Canada for renal cell carcinomas with pathology tumor stage T1a between 2002 and 2014 (N=1449). Patients were excluded if they had multiple tumors or if they were on dialysis prior to nephrectomy.
Results
pN use increased over the duration of the study period. Patients treated after the introduction of guidelines (2007) recommending the use of pN were significantly more likely to receive a pN (OR: 2.709, 95% CI: 1.944–3.775; p<0.001) after adjusting for baseline estimated glomerular filtration rate (GFR), age, and sex. Patients who received rN were at significantly increased risk of death (HR: 1.528, 95% CI: 1.029–2.270; p=0.036) after controlling for baseline GFR, age, and sex. Baseline GFR significantly affected odds of receiving pN (p<0.050) in the entire cohort, but subgroup analysis of more recently diagnosed patients (2011–2014) showed that only patients with kidney failure (GFR <15) were less likely to have received pN.
Discussion
The utilization of pN for patients with pT1a renal cell carcinoma has increased significantly over time and has been accelerated by the introduction of guideline recommendations. Patients treated with pN over the study period had superior overall survival.
Background
Renal cell carcinoma (RCC) is responsible for between 80% and 85% of all primary renal neoplasms. In Canada, approximately 6600 new kidney cancer diagnoses were made in 2017 and 1900 patients died from their disease.Citation1 The increased utilization of diagnostic imaging in general has resulted in more small renal masses being detected,Citation2 allowing for early intervention.
In the absence of metastatic disease, surgery is the preferred treatment approach for eligible patients with small renal masses <4 cm. After nephrectomy, 10-year overall survival rates of 75–80% have been reported.Citation3 Partial nephrectomy (pN), if technically feasible, is preferred over radical nephrectomy (rN) because pN is associated with similar oncologic outcomes but significantly lower rates of chronic renal dysfunction.Citation3,Citation4 The benefits of pN may extend beyond renal preservation. Patients who undergo pN may be at a decreased risk of cardiovascular disease, anemia, malnutrition, and neuropathy compared to patients who undergo rN.Citation5
These findings have led to AmericanCitation6 and EuropeanCitation7 guidelines recommending pN as the standard of care for small renal tumors where technically feasible.
In our jurisdiction (Alberta, Canada), pN was initially recommended as the standard treatment for T1a RCC in 2007. Although some controversy remains regarding the optimal surgical approach for small RCC masses,Citation8 pN has become the primary treatment approach in most jurisdictions.Citation6,Citation7 The goal of this study was to evaluate uptake of pN over time and to investigate current pN/rN practice patterns and outcomes in T1a disease.
Methods
We identified 1679 patients diagnosed between 2002 and 2014 that received a pN or rN for T1a RCC through the Alberta Cancer Registry (ACR). Patient/treatment data were collected from the Discharge Abstract Database (DAD), the National Ambulatory Care Reporting System Database (NACRS), ACR, and through manual chart review. Patients were excluded (n=230) for inaccessible or incomplete medical records, multiple tumors, actual tumor size >4 cm after chart review, if they never underwent pN/rN, or because they were on dialysis prior to nephrectomy. This led to a final cohort of N=1449.
Patients were stratified into pre-/post-guideline eras (2002–2007 and 2008–2014, respectively) based on the introduction of clinical practice guideline recommendations for pN use in T1a tumors. Patients were also stratified into “modern era” based on >70% pN rates (2011–2014).
GFR was calculated according to Levey et alCitation9 or Levey et alCitation10 where appropriate.
Patient and treatment characteristics were compared using monovariate (Chi-square, t-test, or Mann–Whitney, where appropriate), or multivariate analyses (logistical regression). Survival was compared using Kaplan-Meier estimates, Log-rank, and Cox Regression. Statistics were performed using SigmaPlot V13.0 (Systat Software Inc.; Chicago, Illinois) or SPSS V19.0 (IBM; Armonk, New York).
This study did not meet the requirement for ethics board review. The study was determined to be low risk as assessed by the ARECCI ethical review system.Citation11
Results
The entire cohort had a mean follow-up of 54 months. Median age was 59 years (range: 21–87 years) with 39.8% females, and a median GFR of 75.9 mL/min/1.73m2 ().
Table 1 Patient Characteristics
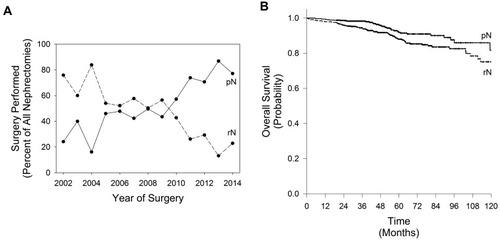
In total, n=879 patients received pN and n=570 patients received rN. In general, pN utilization increased over time (). The lowest utilization of pN occurred in 2004 (16.1% of nephrectomies were pN), and the highest in 2013 (86.8% of nephrectomies were pN). Year-over-year significant increases/decreases in pN use occurred in 2004, 2005, 2009, 2010, 2011, 2013, and 2014 (all p<0.050).
Figure 1 Partial (pN) and Radical (rN) Nephrectomy Utilization and Outcomes. (A) Illustrates the shift in pN/rN utilization over time. (B) Depicts a Kaplan–Meier estimate of survival (Log-Rank p=0.002). In both panels: rN (dashed line) and pN (solid line).
Overall, patients who received pN had similar sex compared to rN patients (38.5% vs 41.8% female, respectively, p=0.202); however, pN patients were significantly younger (median 59 vs 60 years, respectively, p=0.033) and had significantly higher baseline GFR (median 78.4 mL/min/1.73m2 vs 71.6 mL/min/1.73m2, respectively, p<0.001).
Overall survival (OS) was higher in patients who received pN compared to those who received rN (94.8% vs 87.0%, respectively, p=0.002) (). Multivariate analysis identified rN use (HR 1.528, 95% CI: 1.029–2.270, p=0.036), lower GFR (HR: 4.080, 95% CI: 1.673–9.951, p=0.002), older age (60-<80 years) (HR: 2.775, 95% CI: 1.767–4.358, p<0.001) and (≥80 years) (HR: 6.688, 95% CI 3.258–13.729, p<0.001) as factors significantly associated with poorer survival outcomes. Female sex was associated with significantly superior outcomes (HR: 0.600, 95% CI: 0.397–0.906, p=0.015). Guideline era (2002–2006 vs 2007–2014) did not significantly impact survival outcomes (p=0.345) ().
Table 2 Cox Regression for Factors Associated with Risk of Death from Any Cause
Patients who received nephrectomies in the pre-guideline era (2002–2006) were significantly less likely to have received pN compared to patients receiving nephrectomies in the post-guideline era (pre: 37.3%, post: 64.4%, p=0.001). In the pre-guideline era pN patients were significantly younger than rN patients (median 53 years vs 60 years; p=0.015) and had higher baseline GFR (median 68 mL/min/1.73m2 vs 59 mL/min/1.73m2). Patient age (p=0.896) and sex (p=0.888) were similar between guideline eras; however, baseline GFR was significantly higher in the post-guideline era patients (median GFR pre: 62.9 mL/min/1.73m2, post: 77.5 mL/min/1.73m2, p<0.001). Multivariate analysis of the entire cohort found that baseline GFR significantly affected the relative odds of receiving a partial nephrectomy with decreasing GFR values associated with decreasing likelihood of receiving a pN, with the exception of GFR values in the 30–44 mL/min/1.73m2 range (GFR ≥90 reference, GFR 60–89: OR: 0.716, GFR 45–59: OR 0.597, GFR 15–29: OR 0.249, GFR <15: OR <0.001, all p<0.05; GFR 30–44: OR 0.607 p=0.064). The relative odds of receiving a pN in the entire cohort was also significantly affected by pre/post-guideline era, with patients in the post-guideline era significantly more likely to receive a pN (OR: 2.709, 95% CI: 1.944–3.775, p<0.001). Patient sex or age did not affect the relative odds of receiving a pN in the entire cohort (p>0.05) (). In the modern era (2011–2014), the odds of receiving a pN were not significantly affected by GFR, Age, or Sex, with the exception of patients with kidney failure (GFR <15), who remained significantly less likely to receive a pN (OR: <0.001, p<0.001).
Table 3 Relative Odds (Adjusted) of Receiving a Partial Nephrectomy
Discussion
The management of small renal masses has rapidly evolved. Relative to rN, pN is often a more technically challenging procedure; however, the benefits from preserving renal function have led to wide-spread adoption into clinical practice.
The utilization of pN as a proportion of total nephrectomies for T1a RCC generally increased over time from 2002 to 2014 (); however, from 2002 to 2009 6 of 8 years had pN utilization rates between 40% and 50%. In 2007, Van Poppel et alCitation12 reported positive complications/safety outcomes from the Phase III EORTC intergroup trial which led to adoption of pN as standard of care in our local consensus/evidence-based clinical practice guidelines; however, this did not correlate with immediate significant increases in pN use when comparing year-over-year use. Major year-over-year increases in pN use become apparent post-2009, perhaps representing a delay in surgeon uptakeCitation13 or correlating with the reporting of oncological outcomes from the EORTC intergroup phase III trial.Citation3 Regardless, patients treated in the pre-guideline era, when compared to the post-guideline era, were significantly (OR: 2.709, p<0.001) less likely to receive a pN.
In our cohort, pN patients had significantly improved overall survival (), which is likely associated with patient selection as phase III randomized data have shown equivalent outcomes in clinically and pathologically eligible patients,Citation3 however, pN’s superiority did persist when controlled for baseline GFR, age, sex, and guideline era (). As expected, low baseline GFR (15–29 mL/min/1.73m2) was associated with decreased survival. Patients with kidney failure at presentation (GFR <15 mL/min/1.73m2) were not at a significantly increased risk of death, likely due to limited statistical power (n=18). Also expected, older age was associated with increased risk of death from any cause and like others,Citation14 we found that women had significantly reduced risk of death when compared to males.
Early studies evaluating pN recommended that the procedure should be reserved for highly selected patients.Citation15 Over time these recommendations shifted to include all patients who are surgically eligible if the procedure is technically feasible. This transition was apparent in our cohort. In our overall cohort, the adjusted odds of receiving a pN was significantly associated with baseline GFR, with a clear trend towards decreasing pN use with decreased baseline GFR (). Age or gender did not appear to affect the odds of receiving a pN in the entire cohort; however, patients aged ≥80 years did trend towards higher rN use (p=0.131).
To evaluate more recent practice patterns we subdivided our cohort into the “modern era” which consisted of all years where pN represented at least 70% of nephrectomies performed in T1a patients (2011–2014). In this subgroup, no patients with baseline kidney failure (GFR <15 mL/min/1.73m2) received a pN, but otherwise, GFR, age, or sex had no effect on the relative odds of receiving a pN (all p>0.050). This suggests that local guideline recommendations (that all surgically eligible patients should receiving a pN where technically feasible) were adopted within 4 years.
As pN use has now been adopted in most jurisdictions, it is important to analyze how that adoption took place as the focus now shifts to utilizing pN for larger renal masses.Citation16 Despite consensus on evidence-based guidelines in our jurisdiction, a clear lag in uptake was apparent before fairly rapid adoption of recommendations.
This major limitations for this study include the inability to adjust for all clinically relevant patient characteristics and decisions that influence the use of pN vs rN. Also, we did not examine the effects of the surgical approach used (open vs laparoscopic vs robot-assisted laparoscopic). Additionally, ablation techniques that may have been used to treat small renal cell carcinomas were not analyzed. However, we do report on a relatively large real-world population of patients with sufficient time to allow for analysis of temporal trends.
Acknowledgments
This project was supported through operational funding from Cancer Control Alberta. This data was presented in part at the 2017 Canadian Urology Association annual meeting.
Disclosure
The authors report no conflicts of interest in this work.
References
- Cancer.ca. Canadian cancer society. Canadian Cancer Statistics 2017. [cited 36, 2018] Available from:http://www.cancer.ca/~/media/cancer.ca/CW/cancer%20information/cancer%20101/Canadian%20cancer%20statistics/Canadian-Cancer-Statistics-2017-EN.pdf?la=en. Accessed 130th, 2018.
- Cohen HT, McGovern FJ. Renal-cell carcinoma. N Engl J Med. 2005;353:2477–2490. doi:10.1056/NEJMra04317216339096
- Van Poppel H, Da Pozzo L, Albrecht W, et al. A prospective, randomised EORTC intergroup Phase 3 study comparing the oncologic outcome of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol. 2011;59:543–552. doi:10.1016/j.eururo.2010.12.01321186077
- MacLennan S, Imamura M, Lapitan MC, et al. Systematic review of perioperative and quality-of-life outcomes following surgical management of localised renal cancer. Eur Urol. 2012;62:1097–1117. doi:10.1016/j.eururo.2012.07.02822841673
- Huang WC, Levey AS, Serio AM, et al. Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. Lancet Oncol. 2006;7:735–740. doi:10.1016/S1470-2045(06)70803-816945768
- Campbell SC, Novick AC, Belldegrun A, et al. Guideline for management of the clinical T1 renal mass. J Urol. 2009;182:1271–1279. doi:10.1016/j.juro.2009.07.00419683266
- Ljungberg B, Bensalah K, Canfield S, et al. EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol. 2015;67:913–924. doi:10.1016/j.eururo.2015.01.00525616710
- Tobert CM, Riedinger CB, Lane BR. Do we know (or just believe) that partial nephrectomy leads to better survival than radical nephrectomy for renal cancer? World J Urol. 2014;32(3):573–579. doi:10.1007/s00345-014-1275-824671608
- Levey AS, Bosch JP, Lewis JB, et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. modification of diet in renal disease study group. Ann Intern Med. 1999;130:461–470. doi:10.7326/0003-4819-130-6-199903160-0000210075613
- Levey AS, Coresh J, Greene T, et al. Expressing the modification of diet in renal disease study equation for estimating glomerular filtration rate with standardized serum creatinine values. Clin Chem. 2012;53:766–772. doi:10.1373/clinchem.2006.077180
- Hagen B, O’Beirne M, Desai S, et al. Innovations in the ethical review of health-related quality improvement and research: the Alberta Research Ethics Community Consensus Initiative (ARECCI). Healthc Policy. 2007;2:e164–e177.19305726
- Van Poppel H, Da Pozzo L, Albrecht W, et al. A prospective randomized EORTC intergroup phase 3 study comparing the complications of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol. 2007;51:1606–1615. doi:10.1016/j.eururo.2006.11.01317140723
- Haynes B. Barriers and bridges to evidence based clinical practice. BMJ. 1998;317:276. doi:10.1136/bmj.317.7153.2739677227
- May M, Aziz A, Zigeuner R, et al. Gender differences in clinicopathological features and survival in surgically treated patients with renal cell carcinoma: an analysis of the multicenter CORONA database. World J Urol. 2013;31:1073–1080. doi:10.1007/s00345-013-1071-x23568445
- Van Poppel H, Bamelis B, Oyen R, Baert L. Partial nephrectomy for renal cell carcinoma can achieve long-term tumor control. J Urol. 1998;160(3 Pt 1):674–678. doi:10.1016/S0022-5347(01)62751-49720519
- Mir MC, Derweesh I, Porpiglia F, et al. Partial nephrectomy versus radical nephrectomy for clinical T1b and T2 renal tumors: a systematic review and meta-analysis of comparative studies. Eur Urol. 2017;71:606–617. doi:10.1016/j.eururo.2016.08.06027614693
