Abstract
Urethral duplication (UD) is a rare-congenital anomaly that can affect the genito-urinary system. The aim of this case report is to show our experience in this case, including the investigation and operative techniques that we utilized. In the literature review, we will show that different types of duplication, radiological investigations, and surgical techniques have been used to treat this condition.
Keywords:
Introduction
Urethral duplication is a rare-congenital pathology that is more common in boys, with few cases reported in girls.Citation1,Citation2 It can have different clinical manifestations, such as deformed penis, double urinary streams, urinary tract infection, urine incontinence, urethral discharge, and out-flow obstruction.
Different classification systems for this anomaly were reported in the literature.Citation3–Citation6 In most previously reported cases, the accessory urethra ends most commonly with a dorsally opened urethra (epispadias) but can also end in a ventrally opened midline urethra.
Case Presentation
History, Physical Examination and Investigations
A nine-year-old boy who was previously healthy presented to the outpatient department complaining of double urinary stream that was initially noticed after a circumcision was performed a few weeks after birth. Other urinary symptoms, history of urethral discharge and urinary tract infections, and previous hospitalizations were not reported. A general examination showed the boy appeared healthy. Genital examination showed a circumcised penis with a mild degree of dorsal penile chordee. He had two urethral openings: one was normal in size and orthotopic in position at the glans, while the other was small in size and located on the dorsal part of the penis (epispadias) 1 cm proximal to the normal urethra ().
A scrotal examination was normal. With regard to investigations, renal and bladder ultrasounds were normal, and bladder emptying was complete. A voiding cysto-urethrogram (VCUG) was conducted using an 8-Fr feeding tube. We cannulated the normal urethra and normal saline with iodinated contrast media (250 cc), which was infused slowly into the urinary bladder under gravity control, to obtain fluoroscopic images. The results showed the urethra was normal and the shape, size and capacity of the urinary bladder were normal with no vesico-ureteral reflux (VUR). Then, cannulation of the accessory urethra was performed using a 4-Fr feeding tube that was inserted just about1 cm from the accessory meatus. The minimal amount of contrast media was injected under fluoroscopic images (retrograde urethrogram). Antero-Posterior and oblique exposures were taken and it showed complete duplication of the urethra down to the bladder. The voiding phase showed two completely duplicated urethras that started from the bladder ad had two separate lumens and two separate openings distally ().
Surgical Procedure
At the time of surgery, a cysto-urethroscopy was performed that showed a normal urethra, a normal intact external urethral sphincter, and a normal prostatic urethra; the bladder neck and bladder were observed and were also normal. The accessory urethra was cannulated using a hydrophilic small catheter (3-Fr) (0.35”/150 cm/RoadrunnerR UniGlide™/COOK MEDICAL). The catheter passed easily through the meatus towards the bladder and was easily seen to enter the bladder from a point anterior to the bladder neck position.
After cystoscopy, cannulation of the accessory urethra was performed with a 3-Fr hydrophilic catheter and a Foley catheter (10 Fr) was inserted in normal urethra, the penile skin was completely degloved, and the accessory urethra excised down as deep as possible behind the symphysis pubis. The dissection was confined to the hydrophilic catheter and was close to the bladder wall but did not actually reach it, and involved the lining of the accessory urethra so as not to jeopardize the surrounding vessels, nerves, or the normal ventral urethra (,,,). During dissection, it was observed that tethering of the accessory urethra had induced a mild degree of dorsal chordee. Once this was excised, the traction disappeared, and the dorsal chordee corrected. Foley catheter was kept in place for 4 days (). The patient was discharged 1 day after the procedure.
Figure 6 Traction disappeared and the dorsal chordee corrected after excision of the accessory urethra.

The post-operative period was uneventful, and the patient was followed for 9 months, during which he had only one urinary stream and a straight penis.
Discussion
Although a number of theories have been proposed to describe this condition, including misalignment of the termination of the cloacal membrane with the genital tubercle,Citation7 the actual mechanism that causes this disorder remains unknown.
As urethral duplication is a rare anomaly that can affect the lower urinary tract, it can be difficult to order the appropriate imaging study and plan a suitable surgical technique to repair it, and this pathological condition may easily be under diagnosed, especially in patients with associated anomalies, such as exstrophy, epispadias and hypospadias.Citation8 However, the discovery of a second meatus or the suspicion of a second urethra usually warrants a voiding & retrograde cystourethrogram that will aid to make appropriate diagnosis and to plan surgical repair. In this case report, we performed voiding cystourethrogram and retrograde study of the accessory meatus that demonstrated the diagnosis of this congenital anomaly. The duplicated urethra is almost always dorsal to a normal functional urethra, potentially resulting in urinary continence in the accessory urethra as the sphincteric function is intact.Citation9
Urethral duplication is a complex anomaly and the different manifestations probably have different embryological origins.Citation10 Therefore, other congenital anomalies such as those in the Genitourinary and Gastrointestinal tracts as well as malformations of the Cardiovascular and Skeletal systems, may be associated with this pathology.Citation8–Citation14 Salle JL et alCitation8 reported that 6 out of 16 patients with different types of UD (37.5%) had associated VUR. Bladder duplication was described by Woodhouse and Williams,Citation12 the conditions may coexist when the duplication of the bladder extends caudally to produce a collateral urethral duplication. Gyftopoulos el alCitation13 reported 2 distinct cases of diphallia; in the first case, true complete penile duplication was associated with multiple malformations, including a cloacal anomaly, colon and bladder duplication, a horseshoe kidney, a bifid scrotum with undescended testes, a hypoplastic right leg, and a ventricular septum defect and the second patient presented with true, complete diphallia and bladder and urethral duplication but an absence of other anomalies. A recent publication of PatelCitation14 reported a case of UD associated with imperforate anus and hypospadias.
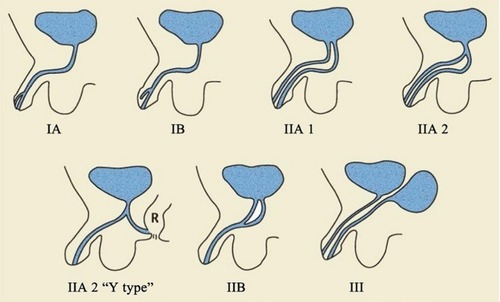
In a literature review, we found that 4 different classification systems are available for this anomaly.Citation3–Citation6 The Effman et alCitation3 classification system describes 3 types of urethral duplication that vary depending on the radiological location of the accessory urethra []. In the first, Type I, there is a blind-ending accessory urethra (incomplete urethral duplication), and this condition is further classified into two subclasses, Type I-A and I-B. In Type I-A, the distal-duplicated urethras open on the dorsal or ventral surface of the penis but do not communicate with the urethra or bladder. In Type I-B, a rare condition, a proximal-accessory urethra opening originating in the urethral channel ends blindly in the peri-urethral tissues. In the second, Type II, there is a completely patent accessory urethra; these cases are classified into 2 subtypes: A when there are two meatuses and B when there is one. Type II A is further classified into two subtypes: type II-A1 and -A2. In type II-A1, two noncommunicating urethras arise independently from the bladder, while in type II-A2, a second channel arises from the first and courses independently into a second meatus in a Y shaped manner (Y-type). In type II-B, two urethras arise from the bladder or posterior urethra and unite into a common channel distally. In the third, type III, an accessory urethra arises from a duplicate or septate bladder.
Figure 8 Effman classification system of UD.
In Ain Shams,Citation6 Abou Zeid and his colleagues recently proposed a simple classification dependent on the orientation of the accessory urethral channel: a sagittal type (the accessory urethra presents above or below the normal urethra) and a collateral type (the accessory urethra presents side by side with the normal urethra). Because it remains controversial whether Y-type UD represents a type of duplication or a congenital fistula between the perineum and/or anal canal, these authors excluded this type from their classification.
Radiological investigation is mandatory to establish a diagnosis, identify the type of the anomaly and rule out associated with other anomalies. In our patient, renal ultrasound was used to assess the upper tract system. VCUG and a retrograde urethrogram were performed in two views for better visualization of the two urethras. Contrast-enhanced voiding urosonography (ceVUS) followed by voiding cystourethrography (VCUG) was performed by PatelCitation14 in a 3-month-old premature male infant with imperforate anus and hypospadias. Images from the ceVUS demonstrated a distinct linearity arising dorsally from the posterior urethra that partially opacified with contrast which was confirmed an urethral duplication by VCUG. Bhadury S et al also used MRI,Citation15 which allows excellent tissue contrast and can provide multi-planar scans, to demonstrate the precise size, shape and position of the two urethras in one patient.
Cysto-urethroscopy may provide a benefit when performed before surgery to identify the functional urethra and find the opening of the accessory urethra in the bladder. In most previously reported cases, similar to our case, the accessory urethra was not scoped due to its narrowed lumen. Maynak Baid et al published a case of a 15-year-old boy in whom cysto-urethroscopy was performed to successfully visualize two completely duplicated urethras.Citation16
The treatment of UD should be individualized for each patient according to the type of UD and the clinical presentation. Higher-grade types usually require complex multiple surgeries, while low-grade incomplete UD may remain untreated. In our case, we performed a complete excision of the dorsal accessory urethra and corrected the associated dorsal penile curvature during the procedure.
Lopes and his colleagues reported that the type of UD was associated with the number of surgeries needed and the postoperative complication rate.Citation17 Mane SB et al described a single-stage repair protocol in which the buccal mucosa forms a tube for urethroplasty in cases of Y-duplication and reported it achieved good final outcomes.Citation18 Mori et al described a case treated with complete excision of the accessory urethra from the normal urethra in a rare type IIA2 (Y-type) patient who had an accessory urethra that opened into the scrotum.Citation19 Abou Zeid et alCitation6 chose treatment options according to the classification he proposed.
Macedo et al reported a rare case in which none of a newborn baby boy’s urethras functioned. They initially performed a Mitrofanoff procedure to allow clear intermittent catheterization (CIC) to treat chronic urine retention.Citation20 Acimi et alCitation21 injected sclerosing agent into the accessory urethra, a procedure associated with a risk of injury to and fibrosis of the corpora cavernosa. Injecting sclerosing substance into the accessory urethra may damage the corporal bodies of the penis. Salle JL et alCitation8 proposed a complex treatment scheme dependent on the type of duplication.
Conclusion
A good imaging study is necessary to diagnose the type of UD, and treatment planning for this pathology must be individualized for each patient depending on the type of deformity, the severity of the symptoms and other associated anomalies.
Ethical Consideration
The study was approved by the Institutional Ethical Committee at the Faculty of Medicine, Mu’tah University.
Consent for Publication
Informed written consent was obtained from the parents of the child described in this study to publish the clinical data and photographs.
Acknowledgment
The authors are very thankful to all the associated personnel in any reference that contributed to the purpose of this study.
Disclosure
This research is not funded by any source and the authors report no conflicts of interest.
References
- Arena S, Arena C, Scuderi MG, Sanges G, Arena F, Di Benedetto V. Urethral duplication in males: our experience in ten cases. Pediatr Surg Int. 2007;23(8):789–794. doi:10.1007/s00383-007-1967-x17576574
- Wani SA, Munianjana NB, Jadhav V, Ramesh S, Gowrishankar BC, Deepak J. Urethral duplication in children: experience of twenty cases. J Indian Assoc Pediatr Surg. 2019;24(4):275–280. doi:10.4103/jiaps.JIAPS_164_1831571759
- Effmann EL, Lebowitz RL, Colodny AH. Duplication of the urethra. Radiology. 1976;119(1):179–185. doi:10.1148/119.1.179943804
- Williams DI, Kenawi MM. Urethral duplications in the male. Eur Urol. 1975;1(5):209–215. doi:10.1159/0004556271233186
- Das S, Brosman SA. Duplication of the male urethra. J Urol. 1977;117(4):452–454. doi:10.1016/S0022-5347(17)58496-7850318
- AbouZeid AA, Safoury HS, Mohammad SA, et al. The double urethra: revisiting the surgical classification. Ther Adv Urol. 2015;7(2):76–84. doi:10.1177/175628721456176025829951
- AB B. Hypospadias and other urethral abnormalities In: Kelalis PP, King LR, Belman AB, editors. Clinical Pediatric Urology. 3rd ed. Philadelphia: WB Saunders; 1992:619–664.
- Salle JL, Sibai H, Rosenstein D, Brzezinski AE, Corcos J. Urethral duplication in the male: review of 16 cases. J Urol. 2000;163(6):1936–1940. doi:10.1016/S0022-5347(05)67602-110799233
- Al-Wattar KM. Congenital prepubic sinus: an epispadiac variant of urethral duplication: case report and review of literature. J Pediatr Surg. 2003;38(4):E10. doi:10.1053/jpsu.2003.50148
- Onofre LS, Gomes AL, Leao JQ, Leao FG, Cruz TM, Carnevale J. Urethral duplication–a wide spectrum of anomalies. J Pediatr Urol. 2013;9(6 Pt B):1064–1071. doi:10.1016/j.jpurol.2013.03.00623623406
- Pippi Salle JL, Sibai H, Jacobson AI, Fehri M, Brzezinski A, Homsy YL. Bladder exstrophy associated with complete urethral duplication: a rare malformation with excellent prognosis. J Urol. 2001;165(6 Pt 2):2434–2437. doi:10.1016/S0022-5347(05)66223-411371992
- Woodhouse CR, Williams DI. Duplications of the lower urinary tract in children. Br J Urol. 1979;51(6):481–487. doi:10.1111/bju.1979.51.issue-6534829
- Gyftopoulos K, Wolffenbuttel KP, Nijman RJ. Clinical and embryologic aspects of penile duplication and associated anomalies. Urology. 2002;60(4):675–679. doi:10.1016/S0090-4295(02)01874-512385932
- Patel H, Watterson C, Chow JS. Case of urethral duplication seen by voiding urosonography. Clin Imaging. 2018;49:106–110. doi:10.1016/j.clinimag.2017.11.01129216522
- Bhadury S, Parashari UC, Singh R, Kohli N. MRI in congenital duplication of urethra. Indian J Radiol Imaging. 2009;19(3):232–234. doi:10.4103/0971-3026.5488419881093
- Baid M, Dutta A. Urethral duplication in a 15-year-old: case report with review of the literature. Rev Urol. 2014;16(3):149–151.25337048
- Lopes RI, Giron AM, Mello MF, et al. Urethral duplication type influences on the complications rate and number of surgical procedures. Int Braz J Urol. 2017;43(6):1144–1151. doi:10.1590/s1677-5538.ibju.2016.026928191791
- Mane SB, Obaidah A, Dhende NP, et al. Urethral duplication in children: our experience of eight cases. J Pediatr Urol. 2009;5(5):363–367. doi:10.1016/j.jpurol.2009.01.00619231292
- Mori K, Shin T, Tobu S, et al. A case of urethral duplication arising from the posterior urethra to the scrotum with urinary stone in a 6-year-old male. Case Rep Pediatr. 2014;2014:290623.25525546
- Macedo A Jr., da Cruz ML, Parizi JLG, et al. An unusual presentation of urethral duplication presenting with chronic bladder retention, left scrotal transposition and left renal agenesis. Int Braz J Urol. 2018;44(2):409–410. doi:10.1590/s1677-5538.ibju.2016.011929064654
- Acimi S, Haouari H, Malah N. Ureteral duplication in a boy. Prog Urol. 2003;13(4):698–699.14650310






