Abstract
Peyronie’s disease (PD) is a condition of the penis, characterized by the presence of localized fibrotic plaque in the tunica albuginea. PD is not an uncommon disorder, with recent epidemiologic studies documenting a prevalence of 3–9% of adult men affected. The actual prevalence of PD may be even higher. It is often associated with penile pain, anatomical deformities in the erect penis, and difficulty with intromission. As the definitive pathophysiology of PD has not been completely elucidated, further basic research is required to make progress in the understanding of this enigmatic condition. Similarly, research on effective therapies is limited. Currently, nonsurgical treatments are used for those men who are in the acute stage of PD, whereas surgical options are reserved for men with established PD who cannot successfully penetrate. Intralesional treatments are growing in clinical popularity as a minimally invasive approach in the initial treatment of PD. A surgical approach should be considered when men with PD do not respond to conservative, medical, or minimally invasive therapies for approximately 1 year and cannot have satisfactory sexual intercourse. As scientific breakthroughs in the understanding of the mechanisms of this disease process evolve, novel treatments for the many men suffering with PD are anticipated.
Introduction
Peyronie’s disease (induratio penis plastica; PD) is a condition of the penis, characterized by the presence of localized fibrotic plaques in the tunica albuginea and affecting 3.2–8.9% of the adult male population.Citation1–Citation3 The true prevalence of PD may be even higher as many patients are reluctant to discuss their condition with a physician or may not seek medical help if the symptoms are not disabling.Citation4 At present, most authorities support the hypothesis that PD generally arises from repetitive (micro)trauma to the erect penis during sexual activities. However, not all penile trauma leads to the development of PD. Abnormal wound healing appears to be more common in men with PD and there is evidence for a genetic predisposition.Citation5 Furthermore, studies have shown that risk factors for atherosclerosis and endothelial dysfunction such as hypertension, dyslipidemia, diabetes mellitus, and smoking are more common in men with PD.Citation6–Citation8
The underlying etiology of PD appears to be an imbalance between profibrotic and antifibrotic substances. Profibrotic substances include transforming growth factor β-1 (TGF-β1), fibrin, plasminogen activator inhibitor-1, and tissue inhibitors of metalloproteinases, and are found to be overexpressed or aberrantly expressed.Citation9 Antifibrotic substances include matrix metalloproteinases, which are a class of molecules responsible for collagen degradation.Citation10 The wound healing cascade begins with exposure of platelets to collagen and the release of chemoattractant molecules such as TGF-β1, platelet-derived growth factor, tumor necrosis factor-α, interleukin-1, and fibrin, which act as a matrix for repair.Citation9 Inhibition of the fibrinolytic system or an inability to degrade the intravasated fibrin leads to its persistence in the tunica and continues to exert a proinflammatory response.Citation11 This response ultimately leads to the formation of a palpable plaque secondary to the excessive deposition of collagen and extracellular matrix, with disorganization of collagen fibers and loss of elastic fibers.Citation11 There are other theories on plaque formation which include cytokine and/or growth factor overexpression and free radical production.Citation12
PD usually presents in men aged 40–70 years and has two phases. The acute phase, lasting for 6–18 months, is often characterized by the development of penile curvature and onset of pain with erection. The acute phase is followed by a chronic phase, characterized by negligible penile pain, and the establishment of a stable penile abnormality.Citation6 Patients presenting with PD can exhibit any single or combination of penile plaque, curvature, pain, and erectile dysfunction (ED). Plaques are typically located on the dorsal or lateral aspect of the penis, causing an upward or lateral defection during erection. As many patients are embarrassed by or unaware of their PD, they are unlikely to mention the topic unless specifically questioned by a treating physician.Citation13 PD is generally a progressive disorder that uncommonly resolves completely. It is difficult to predict an individual’s prognosis at the initiation of the disease. Only penile pain, if present, resolves spontaneously within the first year in the majority of patients.Citation14 In most circumstances, PD progressively worsens over time, as reported in 48% of men with PD in a recent study.Citation15 Two-thirds of patients with PD are likely to have risk factors for arterial disease and therefore will develop ED over the long term.Citation8 Treatment options are chosen based upon disease severity, patient preference, and surgeon’s training. Options include oral medications, intralesional injection therapy, plication procedures, incision and grafting, and placement of a penile prosthesis with or without manual modeling or other ancillary straightening techniques.Citation2
Nonsurgical treatment of PD
Numerous nonsurgical treatment options have been utilized since PD was first descriptively named in 1743. The majority of studies evaluating oral medications lack controls or an adequate number of subjects, are of short duration, and focus on reduction of deformity as the critical measurement of outcome.Citation16 Despite various reports in the literature of deformity stabilization and/or reduction outcomes, recent guidelines indicate that the available evidence shows generally no significant benefit from oral therapies for reducing penile deformity.Citation16,Citation17 However, the standard of care still involves an initial trial of either oral or intralesional treatment at first presentation.Citation13 An accepted goal of medical therapy is to shorten the acute phase of PD in order to stabilize the plaque or diminish disease progression.Citation18
Oral therapy
Vitamin E (tocopherol)
Vitamin E is a fat soluble natural antioxidant that theoretically plays a role in DNA repair.Citation13 Its antioxidant properties have been hypothesized to inhibit nitric oxide synthesis as well as oxygen free radical-induced fibrosis in human cavernosal cells.Citation19 Despite double-blind, placebo-controlled, randomized studies showing no significant improvement, tocopherol remains the most common nonsurgical therapy because of its safety, availability, and low cost.Citation20,Citation21
Potassium para-aminobenzoate (Potaba®)
Potassium para-aminobenzoate was first introduced in 1959 as an oral therapy for PD after it was shown to decrease collagen production in vitro when added to fibroblast cells.Citation22 Its hypothesized mechanism of action involves the enhancement of three endogenous antifibrotic processes: oxygen uptake, glycosaminoglycan secretion, and monoamine oxidase activity.Citation23 Two double-blind, placebo-controlled, randomized studies evaluating the efficacy of Potaba have been published. Shah et al in 1983 reported improvement of symptoms, particularly pain, when compared to placebo; however, these findings were not statistically significant.Citation24 In a more recent study in 2005, Weidner et al published results that demonstrated significant stabilization of preexisting penile deviation and reduction of plaque size, but no significant reduction of pain or preexisting curvature.Citation25 Potaba is currently a first-line therapy for PD because of its tolerability and availability.Citation23
Colchicine
The mechanism of action of colchicine remains unknown but it is hypothesized to reduce lactic acid production, which decreases uric acid deposition and decrease collagen synthesis.Citation13 Akkus et al demonstrated a reduction in plaque size, degree of curvature, and pain symptoms in response to colchicine therapy.Citation26 In another uncontrolled study, Kadioglu et al demonstrated that the efficacy of colchicine increases when used in specified patient groups without any vascular disease risk factors, presenting in the first 6 months of disease, a degree of curvature less than 30 degrees, and without ED.Citation27 A recent nonrandomized study demonstrated that using tocopherol with colchicine in the early stages of PD reduced plaque size, curvature, and pain.Citation28 A recent study by Akman et al retrospectively evaluated patients that were treated with colchicine in the acute phase of PD. They found that the predictive factors for curvature alterations in PD patients were mild deformities mainly in those with lateral curvature, which mostly shifted to the dorsal side after treatment.Citation29 However, another double-blind placebo-controlled study by Safarinejad demonstrated no difference in pain relief, plaque size, or penile curvature.Citation30 Further studies are necessary to clarify the beneficial effects of colchicine in the treatment of PD. The side effects include nausea, vomiting, and diarrhea.Citation13
Tamoxifen
Tamoxifen is a nonsteroidal antiestrogen. Its mechanism of action is unknown but it is hypothesized to modulate TGF-β1, which reduces fibrosis.Citation13 Two uncontrolled studies, Apaydin et al in 1998Citation31 and Ralph et al in 1992,Citation32 reported a decrease of plaque size, penile deviation, and pain. However the results of a double-blind, placebo-controlled randomized study done by Teloken et al reported that the effect on curvature, plaque size, and pain was not significant.Citation33 In the absence of a demonstrable benefit, this drug is not routinely recommended for the treatment of PD.
L-carnitine
L-carnitine’s mechanism of action is not fully understood but it is hypothesized to increase mitochondrial respiration, which decreases free radical formation.Citation34 Biagiotti and Cavallini performed a double-blind, randomized study in 2001 that compared acetyl-L-carnitine with tamoxifen, which was previously shown to have no benefit over placebo, and demonstrated that acetyl-L-carnitine was more effective in reducing pain and disease progression.Citation35 Cavallini et al in 2002 compared the efficacy of oral propionyl-L-carnitine or tamoxifen combined with intralesional verapamil injections. They demonstrated that the combination of propionyl-L-carnitine and verapamil was efficacious and suggested it as the treatment of choice for advanced PD.Citation36 Another doubleblind, placebo-controlled, randomized study by Safarinejad et al in 2007 found that oral propionyl-L-carnitine treatment was not superior to placebo.Citation20 It is possible that an insufficient dose of this agent was used in light of a recent review suggesting that the minimum dose necessary for an effect was at least 3–3.5 g per day.Citation37 The drug has a relatively safe profile, with reported side effects of mild euphoria and gastrointestinal upset.Citation34
Pentoxifylline
Pentoxifylline is a nonspecific phosphodiesterase inhibitor with a hypothesized mechanism of action of upregulating cyclic adenosine monophosphate and decreasing type I collagen production, which remedies the abnormal collagen phenomenon.Citation34 Valente et al in 2003 collected data from in vivo and in vitro models that demonstrated decreased levels of profibrotic factors and plaque size after treatment with pentoxifylline.Citation38 Other studies document that pentoxifylline reduced calcium content in the plaque and collagen fiber deposition and altered elastogenesis by antagonizing the effects of TGF-β1.Citation39–Citation41 Safarinejad et al conducted a doubleblind, placebo-controlled, randomized study that reported a significant effect of pentoxifylline therapy on reducing penile curvature and plaque volume particularly in patients in the early stages of established PD.Citation42 These somewhat promising results with pentoxifylline need further confirmation. This drug is associated with relatively mild side effects, most commonly nausea, dizziness, and headache.Citation34
Phosphodiesterase type 5 (PDE5) inhibitors
PDE5 inhibitors have been shown to decrease oxidative stress-associated inflammatory changes, as observed in the pathophysiology of PD. Its mechanism of action results in an increase of cavernosal smooth muscle levels of cyclic guanosine monophosphate. PDE5 inhibitors, when given continuously over long periods, induce an elevation of nitric oxide and cyclic guanosine monophosphate which act as antifibrotic agents to reduce collagen deposition, profibrotic factor release, oxidative stress, and myofibroblast numbers.Citation11 Levine and Latchamsetty demonstrated that sildenafil was a safe, effective, and well-tolerated first-line therapy for PD patients with ED.Citation43 In another study by Levine et al, sildenafil reduced the incidence of postoperative ED in patients who underwent surgical correction of PD using pericardial grafting after plaque incision. However these results were not statistically significant.Citation44 Valente et al performed a study in a rat model with a PD-like plaque induced by TGF-β1, demonstrating that sildenafil caused a reduction in plaque size.Citation38 Ferrini et al performed a similar rat model study with a PD-like plaque elicited by TGF-β1 or fibrin injection into the tunica albuginea. Long-term oral treatment with vardenafil slowed and reversed the early stages of the PD-like plaque in this rat model.Citation45 Chung et al reported septal scar resolution and improved International Index of Erectile Function-5 questionnaire symptom scores in a study with low-dose daily tadalafil.Citation46 Palmieri et al concluded that extracorporeal shockwave therapy (ESWT) in addition to 5 mg of tadalafil once daily produced significant improvement in erectile function and quality of life for patients with PD and ED.Citation47 Further studies are mandated before any of these methods of treatment can be recommended.
The oral pharmacotherapies as evaluated by randomized controlled trials are summarized in .
Table 1 Efficacy of oral therapy evaluated by randomized trials
Intralesional injection therapy
Corticosteroids
The mechanism of action of corticosteroids was hypothesized to inhibit phospholipase A2 and suppress immune response.Citation48 Historically, the first documented use of intralesional corticosteroids for PD was reported by Bodner et al in 1954, which noted a decrease in plaque size and penile pain following therapy.Citation49 Follow-up studies demonstrated that corticosteroid injections had no therapeutic benefit,Citation50,Citation51 as seen in the single-blinded, placebo-controlled, randomized study performed by Cipollone et al in 1998, which showed no statistically significant benefit.Citation52 Lack of evidence for benefit and side effects such as local tissue atrophy, fibrosis, and immune suppression currently limit the clinical use of this option. Therefore corticosteroid injections are not currently recommended as an intralesional therapy for PD.Citation23
Collagenase
Collagenase, also classified as specific matrix metal loproteinase-1, 8, and 13, degrades interstitial collagens, specifically type II collagen.Citation13 The therapeutic potential of collagenase was initially introduced more than two decades ago in both in vitro and in vivo studies by Gelbard et al.Citation53,Citation54 These researchers utilized highly purified clostridial collagenases to test their effect on various human tissues in vitro, including human pericardium, human corpus cavernosum, tunica albuginea, and PD plaques. These experiments with collagenase resulted in a remarkable reduction in the size of the PD plaque, along with microscopic fraying and dispersal of collagen bundles, when compared with plaques injected with normal saline. Moreover, elastic fibers, vascular smooth muscle, and axonal myelin sheaths were not affected by collagenase application.Citation53 In the following period, the investigators performed an in vivo pilot study that injected intralesional collagenase in 31 men with PD.Citation54 After 4 weeks of treatment, 65% of patients exhibited objective improvement, 93% reported elimination of pain, and intercourse was restored in 75% of patients. Additionally, the researchers noted that penile plaques were either significantly altered or disappeared in four patients and reduced by 20%–100% in 16 others. Studies have reported that immunoglobulin G antibodies to collagenase were higher in men with PD versus healthy men, implying that intralesional collagenase has a documented benefit.Citation55 A double-blind, placebo-controlled, randomized study demonstrated a significant response with collagenase injections in patients with small plaques and minor penile deformity.Citation56 Although not placebo-controlled, a recent study employing two intralesional collagenase injections within 24–72 hours over three injection cycles demonstrated improvement with decreases in both plaque size and penile curvature in men with PD.Citation57 Collagenase can be used in both the acute and chronic phases of PD. Because of its potential efficacy, intralesional collagenase has just completed phase III clinical trials in men with PD. Collagenase is associated with minimal adverse side effects such as injection site pain, ecchymosis, and rarely corporal rupture.Citation13,Citation23
Verapamil
Verapamil is a calcium channel antagonist that augments collagenase activity, increases cytokine expression associated with early inflammation and wound formation, and inhibits in vitro fibroblast proliferation in PD plaques.Citation58,Citation59 Levine et al in 1994 reported that intralesional verapamil injection resulted in a significant reduction in penile curvature.Citation60 Additional uncontrolled studies have reported a decrease in penile pain, curvature, deformity, an increase in girth and rigidity, improved erectile function, and subjective softening of the plaque.Citation61,Citation62 Rehman et al performed the only randomized placebo-controlled study in 1998 with verapamil injection therapy and demonstrated that there was no statistically significant change in penile curvature reduction.Citation63 Because only one study evaluating the efficacy of verapamil included a placebo arm, more controlled studies are required. Verapamil remains a relatively safe and inexpensive form of therapy with minor adverse effects such as nausea, lightheadedness, penile pain, and ecchymosis.Citation23
Interferons
Interferons are cytokines that play a regulatory role in the inflammatory response of the immune system. Interferon-α-2b inhibits the proliferation of fibroblasts, increases collagenase activity, decreases collagen production, and has been used in a number of studies for intralesional injection treatment of P D. Citation18 Initial in vitro studies demonstrated the inhibitory role of interferon-α and interferon-β on collagen production in fibroblasts derived from Peyronie’s plaques.Citation64 Since then, several studies confirmed the beneficial effect in men with PD.Citation65–Citation68 Two single-blind, placebo-controlled studies showed a statistically significant benefit of interferon-α-2b with improvements in penile curvature, plaque size and density, penile pain on erection, erectile function, and penile hemodynamics. This therapy is associated with minor side effects such as sinusitis, minor penile swelling with ecchymosis, and flu-like symptoms of fever, chills, and arthralgia.Citation69,Citation70 The use of over-the-counter anti-inflammatory agents prior to intralesional injection can abrogate the flu-like such effect.
Randomized controlled intralesional therapy studies are summarized in .
Table 2 Efficacy of intralesional therapy evaluated by randomized trials
Topical therapy and iontophoresis
Aminopropionitrile, hydrocortisone, and verapamil are topical medications with varying results in the treatment of PD.Citation71–Citation74 Iontophoresis is the utilization of electrokinetic transport of charged molecules for the enhancement of transdermal drug delivery to diseased tissue, particularly plaques in PD.Citation75 Martin et al demonstrated that topically administered verapamil gel was not present in the tunica albuginea at excisional surgery the next day,Citation73 but was detected to a small degree in PD plaques after iontophoresis.Citation76 In spite of initial successful reports with iontophoresis of dexamethasone and verapamil,Citation77–Citation79 recent double-blind placebo-controlled randomized trials failed to demonstrate statistically significant improvements in penile curvature. Greenfield et al suggest iontophoresis in patients whose major complaint is pain or those who have mild penile curvature and do not wish to undergo intralesional therapy or surgical correction of their penile curvature.Citation80
Extracorporeal shockwave therapy (ESWT)
Penile ESWT has been proposed as a possible nonsurgical PD treatment, but few reports have reported any beneficial effects.Citation81,Citation82 Most studies did not observe any significant improvement in penile curvature.Citation83–Citation85 An exploratory meta-analysis in 2004 by Hauck et al did not reveal any significant benefits of ESWT on improvement of penile curvature or plaque size.Citation86 Two double-blind, placebo-controlled, randomized trials have been published. Chitale et al did not observe any significant benefit of ESWT on PD.Citation87 Palmieri et al demonstrated that ESWT appears to expedite pain resolution compared to the natural course of the disease.Citation88 Currently, ESWT is not recommended as a treatment for PD because it has not been shown to improve or even stabilize the plaque or penile curvature.Citation89
Penile traction devices
Gradual expansion of tunica tissue by traction exerted by a penile extender device induces new connective tissue formation.Citation90 Preliminary studies conducted by Levine et al and Gontero et al have demonstrated nonsignificant curvature reduction and increased penile length.Citation91,Citation92 Further long-term controlled studies are necessary. Raheem et al suggested that vacuum pump therapy may have similar effects on improving penile curvature and pain symptoms.Citation93
Surgical options for PD
The ideal candidate for surgical intervention for PD is a patient whose plaque has stabilized (normally at least 12 months since diagnosis) and penile curvature prevents satisfactory sexual intercourse. Attempts at medical management are attempted initially but, with more severe curvature – normally greater than 60 degrees – surgery may be considered as a primary treatment. Concomitant ED is always evaluated when deciding on surgical options for patients with severe PD.Citation94
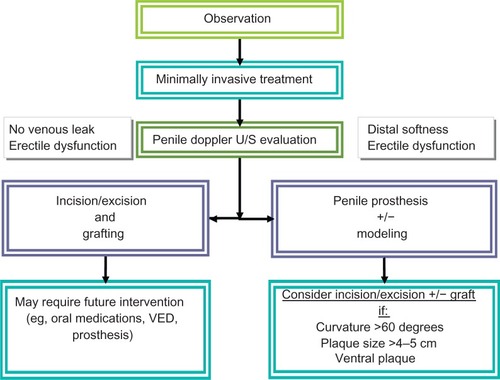
A proposed treatment algorithm for PD is provided in .
Figure 1 Algorithm for treatment of Peyronie’s disease.
Penile plication
For a patient with less severe penile curvature, one option includes shortening the side directly opposite to the curvature to equalize in length both sides of the penis. The ideal candidate for this is a man with adequate penile length, curvature less than 60 degrees, good preoperative erectile function, and no hourglass defect.Citation95 In one study, patients underwent penile plication and greater than 80% of participants agreed that their residual curvature was decreased to less than 20 degrees and their rigidity was equivalent or better than before the procedure. The intuitive common complaint with this procedure is loss of penile length. Such men had their penile length measured before and after the procedure, with a surprising overall length change of +0.6 cm.Citation96
Tunica albuginea plication can be performed using a variety of techniques. The Yachia procedure involves degloving the penis and making a longitudinal incision in the tunica albuginea opposite the plaque.Citation97 The edges are then brought together horizontally using sutures which shorten the unaffected side and overall straightening of the penis.Citation98 The Essed–Schroeder technique doesn’t involve entry or violation of the venoocclusive mechanism; instead sutures are placed in the tunica albuginea and tightened to effectively plicate and straighten the penis.Citation97,Citation99 Overall, success rates of plication procedures range from 70%–100% with rates of patient satisfaction typically over 80%.Citation96,Citation100–Citation109
Data published about plication techniques are summarized in .
Table 3 Data published on plication techniques
Incision and grafting procedures
A more invasive approach involves incising the plaque to release penile curvature and using a graft to augment the missing tunica albuginea. Patients with extensive curvature (greater than 60 degrees), multiple areas of plaque, or those without adequate penile length are candidates for incision and grafting. Similar to penile plication, the penis is degloved exposing Buck’s fascia. The fascia is then entered, avoiding the dorsally located neurovascular bundles. Peyronie’s plaques have a firm texture due to fibrotic changes and can be easily distinguished from the surrounding tunica albuginea. An artificial erection is induced and over the area of the plaque a Y-type or H-type incision is made for tunical release. The tunical defect is then measured and a graft is constructed 10% larger to accommodate possible graft contracture during the healing process.Citation110 The graft is sutured into the defect in a watertight manner and Buck’s fascia is then reapproximated. A final artificial erection is induced to assess for potential vascular leakage. The circumcision is closed in a routine fashion with a mild compression dressing. Most procedures are done on an outpatient basis.
Postoperatively, patients may be advised to use a penile stretching device on a daily basis, possibly with oral medications such as a low-dose PDE5 inhibitor.Citation13,Citation91,Citation111 The use of a PDE5 inhibitor hypothetically increases penile blood flow. Patient satisfaction ranges from 35%–75% with the main complaints postoperatively being decreased penile length and new onset ED.Citation95
The type of graft used often depends on the surgeon’s preference. Saphenous vein, buccal mucosa, acellular porcine dermal matrix, pericardium, and small intestine submucosa are just some of the many available grafts. Buccal mucosa exhibits good elasticity but concerns about oral numbness and mouth tightness demand more long-term follow-up with this approach.Citation95,Citation112 Small intestine submucosa contains collagen, fibroblast growth factor, and fibronectin, which are vital in the healing process.Citation113–Citation114 Recurrence (up to 33% within 3 months), hematoma, infection, and penile shortening have brought this graft material into question.Citation115 Preputial dermal flaps were initially promising but high recurrence, presence of inclusion cysts, and poor patient satisfaction have since been reported.Citation116 Pericardial grafts have the benefit of not requiring a harvest site and exhibit substantial tensile strength.Citation117 The pericardium acts as a scaffold that tunica albuginea grows into and with time the graft is enzymatically dissolved.Citation118
Penile prosthesis implantation
Because PD is often associated with ED, preoperative penile vascular studies using color duplex Doppler ultrasound is recommended.Citation94,Citation110 If a venous leak is identified it is suggested that a PDE5 inhibitor be tried prior to penile prosthesis placement.Citation13 In one study, up to 61% of patients with venous leak responded to oral drugs, changing the need for an inflatable penile prosthesis.Citation119 Penile prosthesis has the advantage of both straightening the curvature and providing patients with ED a functional erection. Both malleable and inflatable devices can be used, however higher satisfaction rates are achieved with the inflatable version. The success rate of penile straightening using penile prosthesis for patients with concomitant PD is higher if the curvature is less than 30 degrees. In men with more severe penile curvatures, incision and grafting or plication procedures may be necessary with simultaneous placement of an inflatable penile prosthesis. When comparing inflatable penile prosthesis to incision and grafting, postoperative erectile function domain scores were significantly higher for patients who had undergone inflatable penile prosthesis implantation. While this approach to surgery offers very good outcomes, there are also still risks that need to be fully discussed with the patient. These include infection, device malfunction, repeat operation, and erosion complications.Citation120
In patients with minimal curvature (less than 30 degrees), placement of the prosthesis alone results in penile straightening by acting as a tissue expander and softening the plaque over time. Commonly, manual modeling is used in combination with a penile prosthesis to correct mild to moderate curvatures.Citation120 Once the prosthesis is inserted, the device is inflated and the surgeon can assess the degree of penile straightening. When the device alone cannot straighten the penis, force is applied to bend the penis in the direction opposite to the curvature.Citation117 This helps to stretch or fracture the plaque and straighten the penis. The success rate with the modeling technique is very high.Citation121 In patients with bottleneck deformities or with severe curvature (greater than 60 degrees), manual modeling alone is less likely to be effective; in such cases incision in the plaque with or without grafting can be performed as previously described.Citation117
Conclusion
PD is not an uncommon disorder, with recent epidemiologic studies documenting a prevalence of 3–9% of adult men affected. The actual prevalence of PD may be even higher. As the definitive pathophysiology of PD has not been completely elucidated, further basic research is required to make progress in the understanding of this enigmatic condition. Currently, nonsurgical treatments are used for those men who are in the acute stage of PD, whereas surgical options are reserved for men with established PD who cannot successfully penetrate. Future oral treatment options may be directed toward increasing tissue expression of matrix metalloproteinases or inhibition of tissue inhibitors of metalloproteinase activity. This area of research will evolve rapidly as the molecular mechanisms underlying PD are further elucidated. Intralesional treatments are growing in clinical popularity as a minimally invasive approach for the initial treatment of PD. Surgical approaches are considered only when men with PD do not respond to medical or minimally invasive therapies for at least 1 year and when patients cannot have satisfactory sexual intercourse. As scientific breakthroughs in the understanding of the mechanisms of this disease evolve, novel treatments for the many men suffering with PD are anticipated.
Disclosure
The authors report no conflicts of interest in this work.
References
- MulhallJPCreechSDBoorjianSASubjective and objective analysis of the prevalence of Peyronie’s disease in a population of men presenting for prostate cancer screeningJ Urol20041712350235315126819
- BellaAJPerelmanMABrantWOLueTFPeyronie’s disease (CME)J Sex Med200741527153817970969
- TaylorFLLevineLAPeyronie’s DiseaseUrol Clin North Am200734517534.vi17983892
- RosenRCataniaJLueTImpact of Peyronie’s disease on sexual and psychosocial functioning: qualitative findings in patients and controlsJ Sex Med200851977198418564146
- ChungEDe YoungLBrockGBRat as an animal model for Peyronie’s disease research: a review of current methods and the peer-reviewed literatureInt J Impot Res20112323524121776004
- UstaMFBivalacquaTJJabrenGWRelationship between the severity of penile curvature and the presence of comorbidities in men with Peyronie’s diseaseJ Urol200417177577914713809
- BjekicMDVlajinacHDSipeticSBMarinkovicJMRisk factors for Peyronie’s disease: a case-control studyBJU Int20069757057416469028
- KadiogluATefekliAErolBOktarTTuncMTellalogluSA retrospective review of 307 men with Peyronie’s diseaseJ Urol20021681075107912187226
- El-SakkaAIHassobaHMChuiRMBhatnagarRSDahiyaRLueTFAn animal model of Peyronie’s-like condition associated with an increase of transforming growth factor beta mRNA and protein expressionJ Urol1997158228422909366377
- Del CarloMColeAALevineLADifferential calcium independent regulation of matrix metalloproteinases and tissue inhibitors of matrix metalloproteinases by interleukin-1beta and transforming growth factor-beta in Peyronie’s plaque fibroblastsJ Urol20081792447245518433786
- Gonzalez-CadavidNFRajferJTreatment of Peyronie’s disease with PDE5 inhibitors: an antifibrotic strategyNat Rev Urol2010721522120212516
- LinCSLinGWangZMaddahSALueTFUpregulation of monocyte chemoattractant protein 1 and effects of transforming growth factor-beta 1 in Peyronie’s diseaseBiochem Biophys Res Commun20022951014101912127997
- HellstromWJMedical management of Peyronie’s diseaseJ Androl20093039740518974422
- GelbardMKDoreyFJamesKThe natural history of Peyronie’s diseaseJ Urol1990144137613792231932
- MulhallJPSchiffJGuhringPAn analysis of the natural history of Peyronie’s diseaseJ Urol200617521152118 discussion 211816697815
- RalphDGonzalez-CadavidNMironeVThe management of Peyronie’s disease: evidence-based 2010 guidelinesJ Sex Med201072359237420497306
- MontorsiFAdaikanGBecherESummary of the recommendations on sexual dysfunctions in menJ Sex Med201073572358821040491
- GurSLiminMHellstromWJCurrent status and new developments in Peyronie’s disease: medical, minimally invasive and surgical treatment optionsExpert Opin Pharmacother20111293194421405946
- AhujaSKSikkaSCHellstromWJStimulation of collagen production in an in vitro model for Peyronie’s diseaseInt J Impot Res19991120721210467520
- SafarinejadMRHosseiniSYKolahiAAComparison of vitamin E and propionyl-L-carnitine, separately or in combination, in patients with early chronic Peyronie’s disease: a double-blind, placebo controlled, randomized studyJ Urol200717813981403 discussion 140317706714
- ShindelAWBullockTLBrandesSUrologist practice patterns in the management of Peyronie’s disease: a nationwide surveyJ Sex Med2008595496418042214
- ZarafonetisCJHorraxTMTreatment of Peyronie’s disease with potassium para-aminobenzoate (potaba)J Urol19598177077213655401
- TrostLWGurSHellstromWJPharmacological Management of Peyronie’s DiseaseDrugs20076752754517352513
- ShahPJR GNAdibRSPryorJPA multicentre double-blind controlled clinical trial of potassium-paraaminobenzoate (Potaba) in Peyronie’s diseaseProg Reprod Biol Med19836167
- WeidnerWHauckEWSchnitkerJPotassium paraaminobenzoate (POTABA) in the treatment of Peyronie’s disease: a prospective, placebo-controlled, randomized studyEur Urol200547530535 discussion 535–53615774254
- AkkusECarrierSRehmanJBrezaJKadiogluALueTFIs colchicine effective in Peyronie’s disease? A pilot studyUrology1994442912958048212
- KadiogluATefekliAKoksalTUstaMErolHTreatment of Peyronie’s disease with oral colchicine: long-term results and predictive parameters of successful outcomeInt J Impot Res20001216917511045911
- Prieto CastroRMLeva VallejoMERegueiro LopezJCCombined treatment with vitamin E and colchicine in the early stages of Peyronie’s diseaseBJU Int20039152252412656907
- AkmanTSanliOUluocakNThe most commonly altered type of Peyronie’s disease deformity under oral colchicine treatment is lateral curvature that mostly shifts to the dorsal sideAndrologia201143283321219379
- SafarinejadMRTherapeutic effects of colchicine in the management of Peyronie’s disease: a randomized double-blind, placebo-controlled studyInt J Impot Res20041623824314973528
- ApaydinESemerciBKefiACikiliNGursanAMulazimogluNThe use of tamoxifen in the treatment of Peyronie’s diseaseInt J Impot Res199810S57
- RalphDJBrooksMDBottazzoGFPryorJPThe treatment of Peyronie’s disease with tamoxifenBr J Urol1992706486511486392
- TelokenCRhodenELGrazziotinTMRosCTSogariPRSoutoCATamoxifen versus placebo in the treatment of Peyronie’s diseaseJ Urol19991622003200510569556
- SmithJFWalshTJLueTFPeyronie’s disease: a critical appraisal of current diagnosis and treatmentInt J Impot Res20082044545918650828
- BiagiottiGCavalliniGAcetyl-L-carnitine vs tamoxifen in the oral therapy of Peyronie’s disease: a preliminary reportBJU Int200188636711446848
- CavalliniGBiagiottiGKoverechAVitaliGOral propionyl-l-carnitine and intraplaque verapamil in the therapy of advanced and resistant Peyronie’s diseaseBJU Int20028989590012010235
- KarlicHLohningerASupplementation of L-carnitine in athletes: does it make sense?Nutrition20042070971515212755
- ValenteEGVernetDFerriniMGQianARajferJGonzalez-CadavidNFL-arginine and phosphodiesterase (PDE) inhibitors counteract fibrosis in the Peyronie’s fibrotic plaque and related fibroblast culturesNitric Oxide2003922924414996430
- SmithJFShindelAWHuangYCPentoxifylline treatment and penile calcifications in men with Peyronie’s diseaseAsian J Androl20111332232521102473
- ShindelAWLinGNingHPentoxifylline attenuates transforming growth factor-beta1-stimulated collagen deposition and elastogenesis in human tunica albuginea-derived fibroblasts part 1: impact on extracellular matrixJ Sex Med201072077208520367772
- LinGShindelAWBanieLPentoxifylline attenuates transforming growth factor-beta1-stimulated elastogenesis in human tunica albuginea-derived fibroblasts part 2: Interference in a TGF-beta1/Smad-dependent mechanism and downregulation of AAT1J Sex Med201071787179720384945
- SafarinejadMRAsgariMAHosseiniSYDadkhahFA double-blind placebo-controlled study of the efficacy and safety of pentoxifylline in early chronic Peyronie’s diseaseBJU Int201010624024819863517
- LevineLALatchamsettyKCTreatment of erectile dysfunction in patients with Peyronie’s disease using sildenafil citrateInt J Impot Res20021447848212494281
- LevineLAGreenfieldJMEstradaCRErectile dysfunction following surgical correction of Peyronie’s disease and a pilot study of the use of sildenafil citrate rehabilitation for postoperative erectile dysfunctionJ Sex Med2005224124716422892
- FerriniMGKovaneczINolazcoGRajferJGonzalez-CadavidNFEffects of long-term vardenafil treatment on the development of fibrotic plaques in a rat model of Peyronie’s diseaseBJU Int20069762563316469038
- ChungEDeyoungLBrockGBThe role of PDE5 inhibitors in penile septal scar remodeling: assessment of clinical and radiological outcomesJ Sex Med201181472147721324095
- PalmieriAImbimboCCretaMVerzePFuscoFMironeVTadalafil once daily and extracorporeal shock wave therapy in the management of patients with Peyronie’s disease and erectile dysfunction: results from a prospective randomized trialInt J Androl2011
- TranchantCBraunSWarterJM[Mechanism of action of glucocorticoids: role of lipocortins]Rev Neurol (Paris)19891458138182533385
- BodnerHHowardAHKaplanJHPeyronle’s disease: cortisone-hyaluronidase-hydrocortisone therapyJ Urol19547240040313202225
- WinterCCKhannaRPeyronie’s disease: results with dermo-jet injection of dexamethasoneJ Urol19751148989001195471
- WilliamsGGreenNAThe non-surgical treatment of Peyronie’s diseaseBr J Urol1980523923957427014
- CipolloneGNicolaiMMastroprimianoGIantornoRLongeriDTenagliaR[Betamethasone versus placebo in Peyronie’s disease]Arch Ital Urol Androl1998701651689823662
- GelbardMKWalshRKaufmanJJCollagenase for Peyronie’s disease experimental studiesUrol Res1982101351406291216
- GelbardMKLindnerAKaufmanJJThe use of collagenase in the treatment of Peyronie’s diseaseJ Urol19851342802832991611
- HamiltonRGMintzGRGelbardMKHumoral immune responses in Peyronie’s disease patients receiving clostridial collagenase therapyJ Urol19861356416472868133
- GelbardMKJamesKRiachPDoreyFCollagenase versus placebo in the treatment of Peyronie’s disease: a double-blind studyJ Urol199314956588417217
- JordanGHThe use of intralesional clostridial collagenase injection therapy for Peyronie’s disease: a prospective, single-center, non-placebo-controlled studyJ Sex Med2008518018718173766
- RothMEickelbergOKohlerEErnePBlockLHCa2+ channel blockers modulate metabolism of collagens within the extracellular matrixProc Natl Acad Sci USA199693547854828643600
- MulhallJPAndersonMSLubranoTShankeyTVPeyronie’s disease cell culture models: phenotypic, genotypic and functional analysesInt J Impot Res20021439740512454692
- LevineLAMerrickPFLeeRCIntralesional verapamil injection for the treatment of Peyronie’s diseaseJ Urol1994151152215248189561
- LasserAVandenbergTLVincentMJHellstromWJIntraplaque verapamil injection for treatment of Peyronie’s diseaseJ La State Med Soc19981504314349785755
- LevineLAGoldmanKEGreenfieldJMExperience with intraplaque injection of verapamil for Peyronie’s diseaseJ Urol2002168621625 discussion 625–62612131321
- RehmanJBenetAMelmanAUse of intralesional verapamil to dissolve Peyronie’s disease plaque: a long-term single-blind studyUrology1998516206269586617
- DuncanMRBermanBNseyoUORegulation of the proliferation and biosynthetic activities of cultured human Peyronie’s disease fibroblasts by interferons-alpha, -beta and -gammaScand J Urol Nephrol19912589941651559
- PolatOGulOOzbeyIOzdikiciMBayraktarYPeyronie’s disease: intralesional treatment with interferon alpha-2 A and evaluation of the results by magnetic resonance imagingInt Urol Nephrol1997294654719406006
- AhujaSBivalacquaTJCaseJVincentMSikkaSCHellstromWJA pilot study demonstrating clinical benefit from intralesional interferon alpha 2B in the treatment of Peyronie’s diseaseJ Androl19992044444810452584
- AstorgaRCanteroOContrerasDIntralesional recombinant interferon alpha-2b in Peyronie’s diseaseArch Esp Urol20005366567111037665
- BrakeMLoertzerHHorschRKellerHTreatment of Peyronie’s disease with local interferon-alpha 2bBJU Int20018765465711350406
- JudgeISWisniewskiZSIntralesional interferon in the treatment of Peyronie’s disease: a pilot studyBr J Urol19977940429043494
- HellstromWJKendirciMMaternRSingle-blind, multicenter, placebo controlled, parallel study to assess the safety and efficacy of intralesional interferon alpha-2B for minimally invasive treatment for Peyronie’s diseaseJ Urol200617639439816753449
- GelbardMLindnerAChvapilMKaufmanJTopical beta-aminopropionitrile in the treatment of Peyronie’s diseaseJ Urol19831297467486842692
- MillerHCArdizzoneJPeyronie disease treated with ultrasound and hydrocortisoneUrology1983215845856868230
- MartinDJBadwanKParkerMMulhallJPTransdermal application of verapamil gel to the penile shaft fails to infiltrate the tunica albugineaJ Urol20021682483248512441945
- FitchW3rdEasterlingWJTalbertRLBordovskyMJMosierMTopical verapamil HCl, topical trifluoperazine, and topical magnesium sulfate for the treatment of Peyronie’s disease--a placebo-controlled pilot studyJ Sex Med2007447748417367443
- SinghJMaibachHITopical iontophoretic drug delivery in vivo: historical development, devices and future perspectivesDermatology19931872352388274778
- LevineLAEstradaCRShouWColeATunica albuginea tissue analysis after electromotive drug administrationJ Urol20031691775177812686831
- RiedlCRPlasEEngelhardtPDahaKPflugerHIontophoresis for treatment of Peyronie’s diseaseJ Urol2000163959910604323
- Di StasiSMGiannantoniAStephenRLCapelliGGiurioliAJanniniEAVespasianiGA prospective, randomized study using transdermal electromotive administration of verapamil and dexamethasone for Peyronie’s diseaseJ Urol20041711605160815017231
- Di StasiSMGiannantoniACapelliGTransdermal electromotive administration of verapamil and dexamethasone for Peyronie’s diseaseBJU Int20039182582912780842
- GreenfieldJMShahSJLevineLAVerapamil versus saline in electromotive drug administration for Peyronie’s disease: a double-blind, placebo controlled trialJ Urol200717797297517296390
- SkolarikosAAlargofERigasADeliveliotisCKonstantinidisEShockwave therapy as first-line treatment for Peyronie’s disease: a prospective studyJ Endourol200519111415735375
- SrirangamSJManikandanRHussainJCollinsGNO’ReillyPHLong-term results of extracorporeal shockwave therapy for Peyronie’s diseaseJ Endourol20062088088417144855
- MichelMSPtaschnykTMusialAObjective and subjective changes in patients with Peyronie’s disease after management with shockwave therapyJ Endourol2003174144 discussion 4412639361
- StrebelRT SSSautterTHauriDExtracorporeal shock wave therapy for Peyronie’s disease does not correct penile deformityInt J Impot Res20041644845114973523
- HauckEWHauptmannABschleipferTSchmelzHUAltinkilicBMWeidnerWQuestionable efficacy of extracorporeal shock wave therapy for Peyronie’s disease: results of a prospective approachJ Urol200417129629914665898
- HauckEWMuellerUOBschleipferTSchmelzHUDiemerTWeidnerWExtracorporeal shock wave therapy for Peyronie’s disease: exploratory meta-analysis of clinical trialsJ Urol200417174074514713800
- ChitaleSMorseyMSwiftLSethiaKLimited shock wave therapy vs sham treatment in men with Peyronie’s disease: results of a prospective randomized controlled double-blind trialBJU Int20101061352135620438568
- PalmieriAImbimboCLongoNA first prospective, randomized, double-blind, placebo-controlled clinical trial evaluating extracorporeal shock wave therapy for the treatment of Peyronie’s diseaseEur Urol20095636336919473751
- HauckEWDiemerTSchmelzHUWeidnerWA critical analysis of non-surgical treatment of Peyronie’s diseaseEur Urol20064998799716698449
- TaylorFLLevineLANon-surgical therapy of Peyronie’s diseaseAsian J Androl200810798718087647
- LevineLANewellMTaylorFLPenile traction therapy for treatment of Peyronie’s disease: a single-center pilot studyJ Sex Med200851468147318373527
- GonteroPDi MarcoMGiubileiGUse of penile extender device in the treatment of penile curvature as a result of Peyronie’s disease. Results of a phase II prospective studyJ Sex Med2009655856619138361
- RaheemAAGaraffaGRaheemTAThe role of vacuum pump therapy to mechanically straighten the penis in Peyronie’s diseaseBJU Int20101061178118020438558
- RalphDJLong-term results of the surgical treatment of Peyronie’s disease with plaque incision and graftingAsian J Androl20111379721785446
- DjinovicRPenile corporoplasty in Peyronie’s disease: which technique, which graft?Curr Opin Urol20112147047721941186
- TaylorFLLevineLASurgical correction of Peyronie’s disease via tunica albuginea plication or partial plaque excision with pericardial graft: long-term follow upJ Sex Med2008522212228 discussion 2229–223018637996
- SerefogluECHellstromWJTreatment of Peyronie’s Disease: 2012 UpdateCurr Urol Rep20111244445221818660
- KadiogluAKucukdurmazFSanliOCurrent status of the surgical management of Peyronie’s diseaseNat Rev Urol201189510621304544
- EssedESchroederFHNew surgical treatment for Peyronie diseaseUrology1985255825874012950
- YachiaDModified corporoplasty for the treatment of penile curvatureJ Urol199014380822294269
- DaitchJAAngermeierKWMontagueDKModified corporoplasty for penile curvature: long-term results and patient satisfactionJ Urol19991622006200910569557
- RehmanJBenetAMinskyLSMelmanAResults of surgical treatment for abnormal penile curvature: Peyronie’s disease and congenital deviation by modified Nesbit plication (tunical shaving and plication)J Urol1997157128812919120923
- RalphDJal-AkraaMPryorJPThe Nesbit operation for Peyronie’s disease: 16-year experienceJ Urol1995154136213637658538
- GholamiSSLueTFCorrection of penile curvature using the 16-dot plication technique: a review of 132 patientsJ Urol20021672066206911956440
- SyedAHAbbasiZHargreaveTBNesbit procedure for disabling Peyronie’s curvature: a median follow-up of 84 monthsUrology200361999100312736023
- SavocaGScieriFPietropaoloFGaraffaGBelgranoEStraightening corporoplasty for Peyronie’s disease: a review of 218 patients with median follow-up of 89 monthsEur Urol462004610614 discussion 613–61415474271
- RolleLTamagnoneATimpanoMDestefanisPFioriCCerutiCFontanaDThe Nesbit operation for penile curvature: an easy and effective technical modificationJ Urol2005173171173 discussion 173–17415592068
- BellaAJBeasleyKAObiedABrockGBMinimally invasive intracorporeal incision of Peyronie’s plaque: initial experiences with a new techniqueUrology20066885285717070366
- GreenfieldJMLucasSLevineLAFactors affecting the loss of length associated with tunica albuginea plication for correction of penile curvatureJ Urol175200617523824116406919
- RichardsonBPinskyMRHellstromWJIncision and grafting for severe Peyronie’s disease (CME)J Sex Med2009620842087 quiz 208819682225
- Moncada-IribarrenI JJMartinez-SalamancaJICabelloRHernandezCManaging penile shortening after Peyronie’s disease surgeryJ Urol200717725217162057
- DublinNStewartLHOral complications after buccal mucosal graft harvest for urethroplastyBJU Int20049486786915476524
- SantucciRABarberTDResorbable extracellular matrix grafts in urologic reconstructionInt Braz J Urol20053119220315992421
- SievertKDTanaghoEAOrgan-specific acellular matrix for reconstruction of the urinary tractWorld J Urol200018192510766039
- BreyerBNBrantWOGarciaMMBellaAJLueTFComplications of porcine small intestine submucosa graft for Peyronie’s diseaseJ Urol200717758959117222639
- TornehlCKCarsonCCSurgical alternatives for treating Peyronie’s diseaseBJU Int20049477478315476507
- KendirciMHellstromWJCritical analysis of surgery for Peyronie’s diseaseCurr Opin Urol20041438138815626883
- LeungwattanakijSBivalacquaTJReddySHellstromWJLong-term follow-up on use of pericardial graft in the surgical management of Peyronie’s diseaseInt J Impot Res20011318318611525318
- MulhallJAndersonMParkerMA surgical algorithm for men with combined Peyronie’s disease and erectile dysfunction: functional and satisfaction outcomesJ Sex Med2005213213816422916
- WilsonSKDelkJR2ndA new treatment for Peyronie’s disease: modeling the penis over an inflatable penile prosthesisJ Urol1994152112111238072079
- WilsonSKClevesMADelkJR2ndLong-term followup of treatment for Peyronie’s disease: modeling the penis over an inflatable penile prosthesisJ Urol200116582582911176479