Abstract
Purpose
Preclinical evaluation of PCA3 and AMACR transcript simultaneous detection in urine to diagnose clinical significant prostate cancer (prostate cancer with Gleason score ≥7) in a Russian cohort.
Patients and Methods
We analyzed urine samples of patients with a total serum PSA ≥2 ng/mL: 31 men with prostate cancer scheduled for radical prostatectomy, 128 men scheduled for first diagnostic biopsy (prebiopsy cohort). PCA3, AMACR, PSA and GPI transcripts were detected by multiplex reverse transcription quantitative polymerase chain reaction, and the results were used for scores for calculation and statistical analysis.
Results
There was no significant difference between clinically significant and nonsignificant prostate cancer PCA3 scores. However, there was a significant difference in the AMACR score (patients scheduled for radical prostatectomy p=0.0088, prebiopsy cohort p=0.029). We estimated AUCs, optimal cutoffs, sensitivities and specificities for PCa and csPCa detection in the prebiopsy cohort by tPSA, PCA3 score, PCPT Risk Calculator and classification models based on tPSA, PCA3 score and AMACR score. In the clinically significant prostate cancer ROC analysis, the PCA3 score AUC was 0.632 (95%CI: 0.511–0.752), the AMACR score AUC was 0.711 (95%CI: 0.617–0.806) and AUC of classification model based on the PCA3 score, the AMACR score and total PSA was 0.72 (95%CI: 0.58–0.83). In addition, the correlation of the AMACR score with the ratio of total RNA and RNA of prostate cells in urine was shown (tau=0.347, p=6.542e–09). Significant amounts of nonprostate RNA in urine may be a limitation for the AMACR score use.
Conclusion
The AMACR score is a good predictor of clinically significant prostate cancer. Significant amounts of nonprostate RNA in urine may be a limitation for the AMACR score use. Evaluation of the AMACR score and classification models based on it for clinically significant prostate cancer detection with larger samples and a follow-up analysis is promising.
Introduction
An early-stage prostate cancer (PCa) diagnosis has become common due to mass PSA (prostate specific antigen) screening.Citation1,Citation2 However, 75% of men with PSA ≥4 ng/mL (traditionally used cutoff)Citation3,Citation4 are not diagnosed with PCa on biopsy.Citation5 The PSA “gray zone” level of 4–10 ng/mL (sometimes 2–10 ng/mL)Citation3,Citation6 needs more accurate noninvasive diagnostic biomarkers to avoid the false-positive results because of benign prostate hyperplasia (BPH), recent digital rectal examination, catheterization and recent ejaculation.Citation4,Citation7 Another PSA test limitation is the indolent, non-csPCa (clinically nonsignificant prostate cancer) with Gleason score (GS) <7 overdiagnosis. For patients with these PCa forms, the harm caused by the diagnosis and treatment can exceed that of the disease itself.Citation8,Citation9 There are some approaches to dividing csPCa and non-csPCa in different studies.Citation10–Citation14 The main feature of non-csPCa in these studies is Gleason grade 6 or less. These forms of PCa have the negligible rate of lymph node metastases; the very low risk of progression after primary treatment; the general safety of active surveillance and the very low rates of progression of men with GS6 disease in active surveillance.Citation15 Usually additional non-csPCa criteria based on PSA density, number of cancer positive cores (for biopsy samples), percent of PCa involvement in any of the cores, etc are used.Citation10,Citation11,Citation16
The 2018 NCCN Guidelines recommend that clinicians consider the use of biomarkers to improve the specificity of PSA testing before performing a biopsy.Citation17 PCA3 noncoding RNA has been extensively evaluated as a urine diagnostic biomarker.Citation18 In contrast to BPH, an elevated level of PCA3 expression is specific for PCa.Citation19 It allows one to distinguish PCa from BPH with acceptable sensitivity and specificity.Citation19,Citation20 However, the ability of PCA3 to distinguish clinically significant prostate cancer (csPCa) from non-csPCa is controversial.Citation17,Citation21,Citation22
The diagnostic value of some biomarkers is currently being studied. One of them is AMACR. AMACR protein is a peroxisomal and mitochondrial enzyme. The AMACR gene is significantly expressed in PCa relative to benign prostate epithelium.Citation23 There were several studies devoted to the PCa early diagnosis by AMACR biomarker in urine and blood.Citation24–Citation26 Neither AMACR nor PSA mRNA levels alone but relative AMACR value score were predictive in RNA obtained from postmassage urine specimen.Citation25 But only 21 patients were in this study.
Recently, several promising low-invasive approaches have been proposed, including the detection of several biomarkers, such as MiPS and Stockholm-3.Citation18 Simultaneous detection of PCA3 and AMACR transcripts was also studied.Citation27 An increase in the PCa diagnosis sensitivity and specificity was demonstrated when using PCA3 and AMACR combination rather than each of them separately. However, this study did not analyze the applicability of these markers for PCa with GS ≥7 detection.
We evaluated the diagnostic potential of simultaneous PCA3 and AMACR transcript detection in total urine RNA of Russian patients with a serum PSA ≥2 ng/mL. We collected and analyzed urine samples of 31 men with PCa scheduled for radical prostatectomy (RPE) and 128 men scheduled for first diagnostic biopsy (prebiopsy cohort). PCA3, AMACR, PSA and GPI (a housekeeping gene) transcripts were detected by multiplex reverse transcription quantitative polymerase chain reaction (RT-qPCR), and the results were used for scores calculation and statistical analysis.
Patients and Methods
Patient Cohorts
All patients were recruited at the Clinic of Urology (Sechenov University, Moscow, Russia) and Moscow City Hospital No. 50 (Department of Urology, AI Yevdokimov Moscow State University of Medicine and Dentistry, Moscow, Russia). Urine RNA testing was performed at the Federal Research and Clinical Center of Physical-Chemical Medicine by a trained employee who was not aware of the biopsy results at the time of testing. Harmonized protocol approved on September 14, 2017 by the local ethics committee of The First Moscow State Medical University named after I.M. Sechenov (Sechenov University, Moscow, Russia) was followed by all centers. Informed consent was obtained from all participants included in the study. Patient information was anonymized and remained confidential. Samples were collected between September 15, 2017, and February 27, 2018.
The inclusion criteria were: total serum PSA (tPSA) ≥2.0 ng/mL, and aged from 40 to 90 years. The exclusion criteria were: previous anti-androgen therapy or bladder catheterization/cystostomy.
Thirty-nine patients scheduled for RPE with primary diagnosis PCa were recruited. Two men were excluded based on the exclusion criteria. Eligible patients who had a sufficient PSA RNA signal in urine (31 men) were divided into two groups based on histopathological examination results: RPE/non-csPCa (13 patients with non-csPCa), and RPE/csPCa (18 patients with csPCa). The prebiopsy cohort comprised 128 patients (94%) provided urine samples with sufficient PSA RNA signal of 136 men scheduled for the first diagnostic biopsy.
Prostate biopsy and postoperative specimens were evaluated by experienced pathologists. Our purpose was primary evaluation of PCA3 and AMACR transcript simultaneous detection in urine to diagnose csPCa in a Russian cohort. We needed first to understand if the AMACR alone or in combination with PCA3 and tPSA was suitable for predicting high Gleason grade (≥7) that is the main feature used for dividing PCa into non-csPCa and csPCa. In this study we used a rough dividing of cancers into csPCa and non-csPCa based only on the Gleason grade as some other authors.Citation12–Citation14
Clinical data as results of DRE, age, tPSA and family history of PCa were obtained and used for PCa and csPCa risk evaluation by PCPTRC (Prostate Cancer Prevention Trial Risk Calculator Version 2.0, https://riskcalc.org/PCPTRC/).Citation28,Citation29 One hundred and eighteen patients from the prebiopsy cohort were eligible for this analysis, 10 were excluded because of age (younger than 55) or tPSA level (higher than 50 ng/mL).
Sample Collection and Processing
The total urine samples were obtained from patients after DRE. Isolation of RNA from urine (~8.5 mL) was carried out with “DNA/RNA Sorbent” kit, (Lytech Co. Ltd, Russia) in accordance with the manufacturer’s protocol. We treated 30 µL (one third) of obtained RNA by DNase use “rDNase Set” (Macherey-Nagel, Germany) in accordance with the manufacturer’s recommendations.
Reverse transcription was performed using a mixture of four reverse primers (one for each transcript, at 0.5 µM) with the MMLV RT kit (Evrogen, Russia).
Multiplex qPCR was carried out using TaqMan probes with ROX, Cy5, FAM and HEX fluorophores for PSA, GPI, PCA3 and AMACR cDNAs, respectively. The primer sequences were located in the second and third exons of the PSA (NM_001648.2), in the eighth and sixth to seventh exon-exon junction of the GPI (NM_001184722.1), in the second and third exons of the AMACR (NM_014324.5) and in the third and fourth exons of the PCA3 (NR_132312.1). The qPCR mixture contained 0.3 µM of each primer and 0.25 µM of each probe, and 5⨰ qPCRmix-HS (Evrogen, Russia) was used. Plasmid standards were used for evaluation of the number of cDNA molecules. All qPCR reactions were performed in duplicate using the reaction profile: 95°C for 8 min, followed by 40 cycles of 95°C for 20 seconds, 62°C for 25 seconds, 72°C for 45 seconds with fluorescence acquisition at 72°C.
We used two aliquots (~8.5 mL) of the same urine sample for repeatability testing.
Data Analysis
We calculated the PCA3 score as the PCA3 RNA content normalized by PSA RNA content and multiplied by 1000: (PCA3 cDNA copies/PSA cDNA copies)×1000. The AMACR and GPI scores were calculated likewise: (AMACR cDNA copies/PSA cDNA copies)×1000, (GPI cDNA copies/PSA cDNA copies)×1000, respectively. The samples with less than 400 copies of PSA cDNA per qPCR reaction were considered uninterpretable.
Also we used PCPT Risk CalculatorCitation28,Citation29 for PCa and csPCa risk evaluations.
For the one-tailed Mann–Whitney criteria p-value calculation, a web-based tool, Wilcoxon–Mann–Whitney Test Calculator, https://ccb-compute2.cs.uni-saarland.de/wtest/Citation30 was used. Logistic regression model (sklearn 0.20.0) was trained on 60% of the data to predict PCa and csPCa based on three features: tPSA (protein concentration ng/mL), PCA3 score and AMACR score. Classification metrics are reported by applying trained model to the remaining 40% of the data (the optimal cutoff points were defined using the Youden method). The web-based tool EasyROC was used for the ROC curve plotting and analysisCitation31 (the optimal cutoff points were defined using the Youden method). For the Kendall, Spearman and Pearson correlation calculations, and for the linear regression analysis followed by plotting, RStudio version 1.1.453 was used.
Results
Recruitment of Patients and Analysis of Samples
The diagnostic accuracy of the prostate biopsy is not absolute. The histopathological analysis of surgical material provides more accurate GS determination.Citation32,Citation33 Therefore, we first recruited patients scheduled for surgery (tPSA ≥2 ng/mL). We collected and analyzed urine samples of 39 patients scheduled for RPE. Thirty-one of them were eligible and provided urine samples with sufficient PSA RNA signal.
Subsequently, the prebiopsy cohort was recruited. The final cohort comprised 128 patients (94%) who provided urine samples with sufficient PSA RNA signal out of 136 men scheduled for the first diagnostic biopsy (tPSA ≥2).
In the multiplex qPCR-based urine sample analysis we used PSA mRNA as reference transcript. PSA is a gene with the prostate-specific expression. There is only a slight difference in PSA expression level between normal and tumor prostate cells.Citation34 We calculated the PCA3 score as the normalized PCA3 RNA content multiplied by 1000. The AMACR score was calculated likewise.
The content ratio of GPI (a housekeeping geneCitation35) RNA to PSA RNA is proportional to the ratio of total RNA and RNA of prostate cells in urine. We calculated the GPI score as the PCA3 and AMACR scores to test the assumption that the fraction of prostate cell RNA in total urinary RNA can affect the analysis results (see below).
We tested two aliquots of urine samples obtained from 13 patients for evaluation of our approach repeatability. There was a high correlation between test and retest results. Pearson’s coefficients of correlation were 0.991 (p=5.005e–11), 0.991 (p=5.201e–11) and 0.963 (p=1.404e–07) for the PCA3, AMACR and GPI scores respectively.
We obtained histopathological examination results for prebiopsy cohort after urine analysis completion. The clinical characteristics of the prebiopsy cohort and groups of patients scheduled for surgery are given in .
Table 1 Clinical Characteristics of Patients
Evaluation of the Diagnostic Potential of PCA3 and AMACR Scores
The eligible patients scheduled for surgery who provided urine samples with sufficient PSA RNA signal were divided into two groups following the results of pathomorphological examination of their surgical material: RPE/non-csPCa group comprised 13 patients with non-csPCa scheduled for RPE, RPE/csPCa group comprised 18 patients with csPCa scheduled for RPE. Prebiopsy cohort was divided into three groups: BPH group (67 men), non-csPCa group (28 men) and csPCa group (33 men).
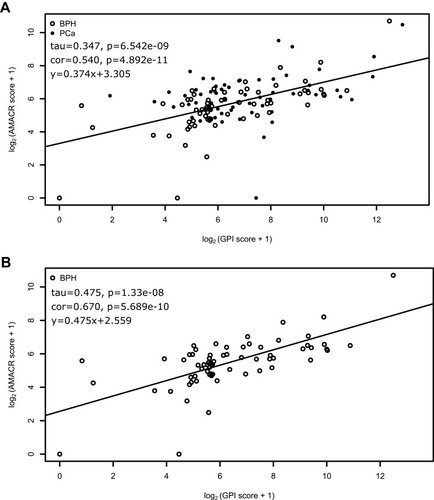
We found a significant difference in the PCA3 score between BPH and non-csPCa group in prebiopsy cohort analysis (p=0.0074, Mann–Whitney test, ). There was also a significant difference in tPSA between these groups of patients in prebiopsy cohort (p=0.016). We did not find significant difference in the AMACR score between patients with BPH and non-csPCa (p=0.12, ).
Figure 1 PCA3 and AMACR scores in groups of patients with BPH, non-csPCa and csPCa. Box whiskers correspond to 5th and 95th percentile outliers are not shown. (A) PCA3 score, prebiopsy cohort, (B) AMACR score, prebiopsy cohort, (C) PCA3 score, patients scheduled for RPE, (D) AMACR score, patients scheduled for RPE.
There was no significant difference in the PCA3 score or tPSA between patients with non-csPCa and csPCa (prebiopsy cohort: PCA3 score p=0.29, , tPSA p=0.17, patients scheduled for RPE: PCA3 score p=0.35, , tPSA p=0.35). However, we found a significant difference in the AMACR score between patients with csPCa and non-csPCa scheduled for RPE (p=0.0088, ) and biopsy (p=0.029, ).
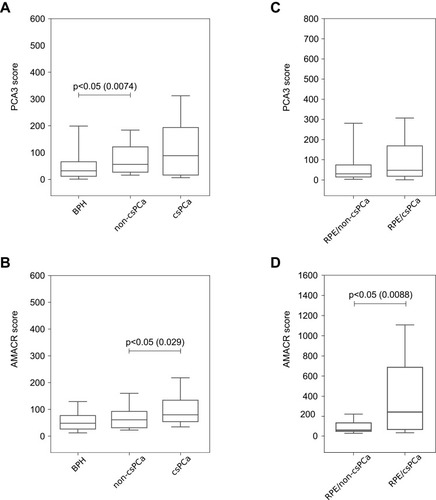
Logistic regression (sklearn v. 0.20.0) model was trained on three features (the PCA3 score, the AMACR score and tPSA) for PCa and csPCa detection in the prebiopsy cohort. Also we analyzed clinical data of 118 patients by PCPTRC (10 patients were excluded by age or tPSA level, see “Material and Methods” section). The ROC curve analysis was applied to evaluate the accuracy of tPSA, the PCA3 and AMACR scores, PCPTRC prognoses and classification models for PCa or csPCa prediction in the prebiopsy cohort. ROC curves for PCa and csPCa detection by PCA3 and AMACR score, PCPTRC and classification models are shown in . Classification metrics for PCa and csPCa detection using all these features and classification models are given in . In the PCa ROC analysis, the classification model area under the curve (AUC) was the highest: 0.77 (95%CI: 0.63–0.86), the tPSA AUC was the lowest: 0.643 (95%CI: 0.547–0.739). In the csPCa ROC analysis the classification model AUC was the highest: 0.72 (95%CI: 0.58–0.83), the tPSA AUC was the lowest: 0.612 (95%CI: 0.495–0.729), AUC of the AMACR score was 0.711 (95%CI: 0.617–0.806). AUCs of the classification model, the AMACR and PCA3 scores were significantly greater than 0.5. AUC of the AMACR score for csPCa detection was higher than AUC of PCPTRC risk estimation. However, this difference was insignificant.
Figure 2 PCa and csPCa detection in the prebiopsy cohort. The number of patients is indicated by n. (A) ROC curves for PCa detection by AMACR score and PCA3 score (whole prebiopsy cohort), (B) ROC curves for csPCa detection by AMACR score and PCA3 score (whole prebiopsy cohort), (C) ROC curves for PCa detection by AMACR score, PCA3 score and PCPTRC, (D) ROC curves for csPCa detection by AMACR score, PCA3 score and PCPTRC, (E) ROC curve for PCa detection by classification model, (F) ROC curve for csPCa detection by classification model.
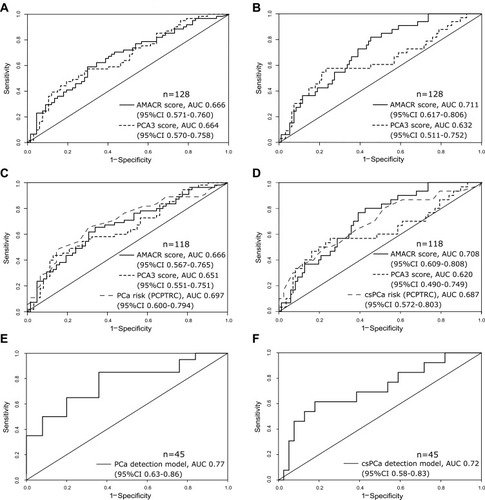
Table 2 Classification Metrics of tPSA, The PCA3 Score, The AMACR Score and Classification Models
The AMACR and GPI Score Association
We examined a correlation between each oncomarker (PCA3 and AMACR) content and GPI score in the total prebiopsy cohort to test the assumption that the fraction of prostate cell RNA in total urinary RNA can affect the analysis results. For the AMACR-GPI and PCA3-GPI scores, the Kendall’s correlation coefficient (tau) was 0.347 (p=6.542e-09) and 0.069 (p=0.2479, statistically insignificant), respectively.
Then tau was calculated only for patients with BPH in the prebiopsy cohort to exclude the PCa influence on the PCA3 and AMACR scores. We obtained a significant tau value for the AMACR score (0.475, p=1.33e-08), whereas tau was insignificant for the PCA3 score (−0.131, p=0.1165). The relationships between log2(AMACR score+1) and log2(GPI score+1) in patients with BPH and in total prebiopsy cohort are depicted in .
Discussion
In this study, we evaluated the diagnostic potential of the simultaneous quantitative detection of PCA3, AMACR, PSA and GPI transcripts in urine of men with tPSA ≥2 ng/mL by multiplex qPCR. Patients scheduled for RPE and the first diagnostic biopsy was recruited. We compared the urine RNA qPCR results with the histopathological examination results for these patients.
Our PCA3 score AUC for PCa detection in the prebiopsy cohort (0.664) is consistent with the Cui et al meta-analysis values in the 0.57–0.85 range.Citation36 The PCA3 sensitivity (0.475) and specificity (0.806) of PCa detection conforms to the previously reported sensitivity (0.469–0.95) and specificity (0.216–1.00) for PCa detection by PCA3.Citation36 The PCA3 score AUC (0.66) and the AMACR score AUC (0.67) for PCa detection in the prebiopsy cohort was very close to the PCA3 AUC (0.67) and AMACR score AUC (0.66) reported by Ouyang et al.Citation27
No significant difference was found in the PCA3 score between non-csPCa and csPCa groups. The previous data on the differences in the PCA3 scores between non-csPCa and csPCa are controversial.Citation37–Citation39 In our opinion, these contradictions are at least in part due to the sample size variability as well as the ratio of subgroups with different GS in the GS ≥7 group in different human populations, etc.
There were several studies evaluated AMACR RNA in urine for early detection of PCa.Citation25–Citation27 But the main purpose of this study was to evaluate AMACR RNA as a marker of csPCa. We first show a significant difference in the AMACR score between csPCa (Gleason grade ≥7) and non-csPCa groups (Gleason grade <7), both for patients scheduled for RPE and for biopsy. Also the AMACR score had relatively high AUC (0.711), that was significantly greater than 0.5 (95%CI: 0.617–0.806), in csPCa detection. In our view, the AMACR is a prospective urine marker for csPCa detection. Also there is first data about urine AMACR transcript detection (and PTPRC using) for PCa and csPCa diagnosis in the Russian cohort. Additionally, we first showed the association between the AMACR and GPI scores. PCA3 expression is highly specific for the PCa cells, whereas AMACR expression is relatively high in such tissues as: kidney, bladder tissue, hematopoietic tissue, etc https://www.proteinatlas.org/ENSG00000242110-AMACR/tissue.Citation40 Thus, we expected an increase in the AMACR score not only for patients with PCa, but also for patients with significant amounts of nonprostate RNA in urine (patients with high GPI score). Therefore, diagnostic systems based on the AMACR transcript should be used with GPI or similar housekeeping gene for estimation of prostate RNA content in the total urine RNA.
We found a significant difference in tPSA between BPH and non-csPCa groups of patients in the prebiopsy cohort, but not between the same groups of the patients scheduled for surgery. No significant difference was found in the tPSA between patients with non-csPCa and csPCa scheduled for surgery or for biopsy. This result is consistent with the data about the non-csPCa overdiagnosis by PSA test.Citation21
We obtained classification models based on three features: the PCA3 score, the AMACR score and tPSA for PCa and csPCa detection in prebiopsy cohort. The AUC of the PCa prediction was 0.77 and the AUC of the csPCa prediction was 0.72. In our opinion, further evaluation of the multiplex qPCR for early PCa and csPCa detection with larger sample size and a follow-up analysis will allow a more accurate refinement of the cutoff and higher specificity and/or sensitivity for models based on combination of AMACR score, PCA3 score and tPSA. The AMACR score and classification models based on it may further help to make an appropriate decision about biopsy performing and treatment options.
Our purpose was primary evaluation of PCA3 and AMACR transcript simultaneous detection in urine to diagnose csPCa in a Russian cohort. The main limitation of our study was sample size insufficient for comparison of the different classificators. We obtained AUCs with relative broad confidence intervals and we could not show statistically significant differences between AUCs of different classifiers. There may be other limitations of our study associated with the characteristics of the Russian cohort. This cohort included only Caucasian men. Also there was no PSA screening in the Russian Federation unlike some other countries as the USA.Citation41 There may be difference between estimations obtained for the Russian cohort and data obtained in countries with mass PSA screening as the USA.
Conclusion
The AMACR score is a good predictor of csPCa in the Russian cohort. However, significant amounts of nonprostate RNA in urine samples of some patients may be a limitation for AMACR score use. Further evaluation of the AMACR score and classification models based on the tPSA, the PCA3 and AMACR score for PCa and csPCa detection with larger samples and a follow-up analysis is promising.
Abbreviations
PSA, prostate specific antigen; RT-qPCR, reverse transcription quantitative polymerase chain reaction; csPCa, clinically significant prostate cancer; GS, Gleason score; AUC, area under the ROC curve; non-csPCa, clinically nonsignificant prostate cancer; PCa, prostate cancer; BPH, benign prostate hyperplasia; RPE, radical prostatectomy; qPCR, quantitative polymerase chain reaction; tPSA, total PSA; PCPTRC, Prostate Cancer Prevention Trial Risk Calculator; ROC curve, Receiver operating characteristic curve.
Ethics Approval and Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Declaration of Helsinki and its later amendments. Harmonized protocol was approved September 14, 2017 by the local ethics committee of The First Moscow State Medical University named after I.M. Sechenov (Sechenov University, Moscow, Russia) followed by all centers. Informed consent was obtained from all participants included in the study. Patient information was anonymized and remained confidential. Samples were collected between September 15, 2017 and February 27, 2018.
Acknowledgments
The authors thank the Ministry of Education and Science of Russian Federation and the Russian Foundation for Basic Research for their support.
Disclosure
Elena S Kotova reports grants from Ministry of Education and Science of Russian Federation, grants from Russian Foundation for Basic Research, grants from Russian Foundation for Basic Research, during the conduct of the study. Yulia A Savochkina is an employee of Lytech Ltd. Alexander O Vasilyev reports grants from Russian Foundation for Basic Research according, during the conduct of the study. Elena A Prilepskay reports grants from Russian Foundation for Basic Research, during the conduct of the study. Konstantin A Babalyan reports grants from Ministry of Education and Science of Russian Federation, during the conduct of the study. Alexander Govorov reports grants from Russian Foundation for Basic Research, during the conduct of the study. Elena S Kostryukova reports grants from Ministry of Education and Science of Russian Federation, during the conduct of the study. Elena I Sharova reports grants from Ministry of Education and Science of Russian Federation, grants from Russian Foundation for Basic Research, during the conduct of the study. The authors reports no other potential conflicts of interest in this work.
Additional information
Funding
References
- Stephan C, Jung K, Ralla B. Current biomarkers for diagnosing of prostate cancer. Future Oncol. 2015;11(20):2743–2755. doi:10.2217/fon.15.20326358139
- Tsodikov A, Gulati R, Heijnsdijk EAM, et al. Reconciling the effects of screening on prostate cancer mortality in the ERSPC and PLCO trials. Ann Intern Med. 2017;167(7):449–455. doi:10.7326/M16-258628869989
- Stephan C, Rittenhouse H, Hu X, Cammann H, Jung K. Prostate-specific antigen (PSA) screening and new biomarkers for prostate cancer (PCa). EJIFCC. 2014;25(1):55.27683457
- Polascik TJ, Oesterling JE, Partin AW. Prostate specific antigen: a decade of discovery-what we have learned and where we are going. J Urol. 1999;162(2):293–306. doi:10.1016/S0022-5347(05)68543-610411025
- Mistry K, Cable G. Meta-analysis of prostate-specific antigen and digital rectal examination as screening tests for prostate carcinoma. J Am Board Fam Pract. 2003;16(2):95–101. doi:10.3122/jabfm.16.2.9512665174
- Ross T, Ahmed K, Raison N, Challacombe B, Dasgupta P. Clarifying the PSA grey zone: the management of patients with a borderline PSA. Int J Clin Pract. 2016;70(11):950–959. doi:10.1111/ijcp.1288327672001
- Stamey TA, Yang N, Hay AR, McNeal JE, Freiha FS, Redwine E. Prostate-specific antigen as a serum marker for adenocarcinoma of the prostate. N Engl J Med. 1987;317(15):909–916. doi:10.1056/NEJM1987100831715012442609
- Sandhu GS, Andriole GL. Overdiagnosis of prostate cancer. J Natl Cancer Inst Monogr. 2012;2012(45):146–151. doi:10.1093/jncimonographs/lgs03123271765
- Loeb S, Bjurlin MA, Nicholson J, et al. Overdiagnosis and overtreatment of prostate cancer. Eur Urol. 2014;65(6):1046–1055. doi:10.1016/j.eururo.2013.12.06224439788
- Loeb S, Sanda MG, Broyles DL, et al. The prostate health index selectively identifies clinically significant prostate cancer. J Urol. 2015;193(4):1163–1169. doi:10.1016/j.juro.2014.10.12125463993
- Valerio M, Donaldson I, Emberton M, et al. Detection of clinically significant prostate cancer using magnetic resonance imaging-ultrasound fusion targeted biopsy: a systematic review. Eur Urol. 2015;68(1):8–19. doi:10.1016/j.eururo.2014.10.02625454618
- Kasivisvanathan V, Rannikko AS, Borghi M, et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med. 2018;378(19):1767–1777. doi:10.1056/NEJMoa180199329552975
- Kayano PP, Carneiro A, Castilho TML, et al. Comparison of Gleason upgrading rates in transrectal ultrasound systematic random biopsies versus US-MRI fusion biopsies for prostate cancer. Int Braz J Urol. 2018;44(6):1106–1113. doi:10.1590/s1677-5538.ibju.2017.055230325600
- Li Q, Lu H, Choi J, et al. Radiological semantics discriminate clinically significant grade prostate cancer. Cancer Imaging. 2019;19(1):81. doi:10.1186/s40644-019-0272-y31796094
- Kulac I, Haffner MC, Yegnasubramanian S, Epstein JI, De Marzo AM. Should Gleason 6 be labeled as cancer? Curr Opin Urol. 2015;25(3):238–245. doi:10.1097/MOU.000000000000016525730327
- Epstein JI, Walsh PC, Carmichael M, Brendler CB. Pathologic and clinical findings to predict tumor extent of nonpalpable (stage T1c) prostate cancer. JAMA. 1994;271(5):368–374. doi:10.1001/jama.1994.035102900500367506797
- Carroll PH, Mohler JL. NCCN guidelines updates: prostate cancer and prostate cancer early detection. J Natl Compr Canc Netw. 2018;16(5S):620–623. doi:10.6004/jnccn.2018.003629784740
- Loeb S, Partin AW. Review of the literature: PCA3 for prostate cancer risk assessment and prognostication. Rev Urol. 2011;13(4):e191.22232568
- Marks LS, Fradet Y, Deras IL, et al. PCA3 molecular urine assay for prostate cancer in men undergoing repeat biopsy. Urology. 2007;69(3):532–535. doi:10.1016/j.urology.2006.12.01417382159
- Stephan C, Ralla B, Jung K. Prostate-specific antigen and other serum and urine markers in prostate cancer. Biochim Biophys Acta. 2014;1846(1):99–112. doi:10.1016/j.bbcan.2014.04.00124727384
- Ali A, Hoyle A, Baena E, Clarke NW. Identification and evaluation of clinically significant prostate cancer: a step towards personalized diagnosis. Curr Opin Urol. 2017;27(3):217–224. doi:10.1097/MOU.000000000000038528212121
- Deras IL, Aubin SM, Blase A, et al. PCA3: a molecular urine assay for predicting prostate biopsy outcome. J Urol. 2008;179(4):1587–1592. doi:10.1016/j.juro.2007.11.03818295257
- Kanyong P, Rawlinson S, Davis J. Immunochemical assays and nucleic-acid detection techniques for clinical diagnosis of prostate cancer. J Cancer. 2016;7(5):523–531. doi:10.7150/jca.1382126958088
- Rogers CG, Yan G, Zha S, et al. Prostate cancer detection on urinalysis for alpha methylacyl coenzyme a racemase protein. J Urol. 2004;172(4 Pt 1):1501–1503. doi:10.1097/01.ju.0000137659.53129.1415371879
- Zielie PJ, Mobley JA, Ebb RG, Jiang Z, Blute RD, Ho SM. A novel diagnostic test for prostate cancer emerges from the determination of alpha-methylacyl-coenzyme A racemase in prostatic secretions. J Urol. 2004;172(3):1130–1133. doi:10.1097/01.ju.0000133560.87118.4d15311056
- Zehentner BK, Secrist H, Zhang X, et al. Detection of α-methylacyl-coenzyme-A racemase transcripts in blood and urine samples of prostate cancer patients. Mol Diagn Ther. 2006;10(6):397–403. doi:10.1007/BF0325621717154657
- Ouyang B, Bracken B, Burke B, Chung E, Liang J, Ho SM. A duplex quantitative polymerase chain reaction assay based on quantification of α-methylacyl-CoA racemase transcripts and prostate cancer antigen 3 in urine sediments improved diagnostic accuracy for prostate cancer. J Urol. 2009;181(6):2508–2514. doi:10.1016/j.juro.2009.01.11019371911
- Ankerst DP, Hoefler J, Bock S, et al. The prostate cancer prevention trial risk calculator 2.0 for the prediction of low- versus high-grade prostate cancer. Urology. 2014;83(6):1362–1368. doi:10.1016/j.urology.2014.02.03524862395
- Grill S, Fallah M, Leach RJ, et al. Incorporation of detailed family history from the Swedish family-cancer database into the prostate cancer prevention trial risk calculator. J Urol. 2014;193(2):460–465. doi:10.1016/j.juro.2014.09.01825242395
- Marx A, Backes C, Meese E, Lenhof HP, Keller A. EDISON-WMW: exact dynamic programing solution of the Wilcoxon–Mann–Whitney test. Genomics Proteomics Bioinformatics. 2016;14(1):55–61. doi:10.1016/j.gpb.2015.11.00426829645
- Goksuluk D, Korkmaz S, Zararsiz G, Karaagaoglu AE. EasyROC: an interactive web-tool for ROC curve analysis using R language environment. R J. 2016;8(2):213–230. doi:10.32614/RJ-2016-042
- Heidegger I, Skradski V, Steiner E, et al. High risk of under-grading and-staging in prostate cancer patients eligible for active surveillance. PLoS One. 2015;10(2):e0115537. doi:10.1371/journal.pone.011553725658878
- Arias-Stella JA, Shah AB, Montoya-Cerrillo D, Williamson SR, Gupta NS. Prostate biopsy and radical prostatectomy gleason score correlation in heterogenous tumors. Am J Surg Pathol. 2015;39(9):1213–1218. doi:10.1097/PAS.000000000000049926274028
- Meng FJ, Shan A, Jin L, Young CY. The expression of a variant prostate-specific antigen in human prostate. Cancer Epidemiol Biomarkers Prev. 2002;11(3):305–309.11895882
- Eisenberg E, Levanon EY. Human housekeeping genes, revisited. Trends Genet. 2013;29(10):569–574. doi:10.1016/j.tig.2013.05.01023810203
- Cui Y, Cao W, Li Q, et al. Evaluation of prostate cancer antigen 3 for detecting prostate cancer: a systematic review and meta-analysis. Sci Rep. 2016;6:25776. doi:10.1038/srep2577627161545
- Haese A, de la Taille A, Van Poppel H, et al. Clinical utility of the PCA3 urine assay in European men scheduled for repeat biopsy. Eur Urol. 2008;54(5):1081–1088. doi:10.1016/j.eururo.2008.06.07118602209
- de la Taille A, Irani J, Graefen M, et al. Clinical evaluation of the PCA3 assay in guiding initial biopsy decisions. J Urol. 2011;185(6):2119–2125. doi:10.1016/j.juro.2011.01.07521496856
- Hessels D, van Gils MP, van Hooij O, et al. Predictive value of PCA3 in urinary sediments in determining clinico‐pathological characteristics of prostate cancer. Prostate. 2010;70(1):10–16. doi:10.1002/pros.2103219708043
- Uhlén M, Fagerberg L, Hallström BM, et al. Tissue-based map of the human proteome. Science. 2015;347(6220):1260419. doi:10.1126/science.126041925613900
- Fenton JJ, Weyrich MS, Durbin S, Liu Y, Bang H, Melnikow J. Prostate-specific antigen-based screening for prostate cancer: evidence report and systematic review for the US preventive services task force. JAMA. 2018;319(18):1914–1931. doi:10.1001/jama.2018.371229801018