Abstract
Objective
To evaluate factors correlated with pain during prostate biopsy and willingness to undergo transrectal ultrasound-guided prostate biopsy (TR-PBx) again without anesthesia in patients undergoing TR-PBx without anesthesia.
Methods
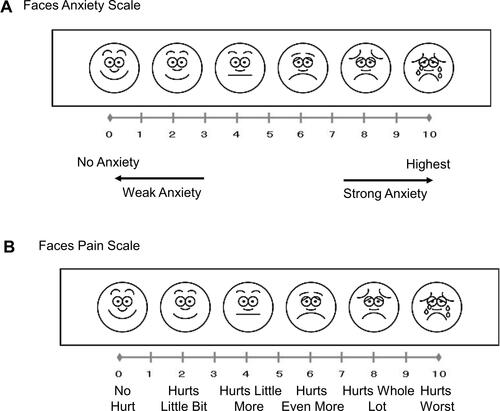
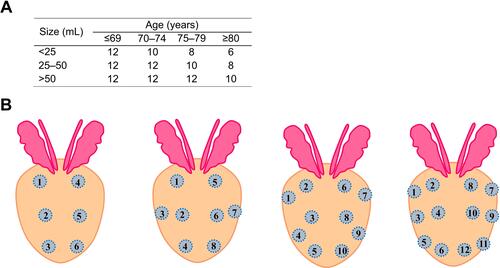
This retrospective, single-center study evaluated 624 patients who underwent TR-PBx without anesthesia. Based on a nomogram using patient age and prostate volume, 6–12 core biopsy samples were allocated. Anxiety was evaluated using the Faces Anxiety Scale before the TR-PBx. Pain was evaluated using the Faces Pain Scale at each puncture and immediately after confirmation of cessation of bleeding from the rectum after the transrectal probe was pulled out. The question “If this operation must be repeated, would you agree to undergo it again under same conditions?” was asked after the procedure was completed. The change in pain at each puncture and factors correlated with post-procedural pain were calculated using multiple regression analysis, and factors predicting an answer of “yes” to the question using binary logistic analysis were evaluated.
Results
Scores on the Faces Pain Scale significantly increased from the first core sample to last as the number of samples increased. However, the number of samples did not show significant correlation with pain evaluated after the procedure was complete. Time during the biopsy and the anxiety score had a significant correlation with the pain scale score for the completed procedure. Short duration of TR-biopsy and a low anxiety score predicted a reply of “Yes” to the question.
Conclusion
A long operative time during the TR-PBx procedure and strong pre-procedure anxiety can increase pain for patients undergoing the procedure without anesthesia and cause patients to be unwilling to undergo TR-PBx again without anesthesia.
Introduction
Transrectal ultrasound-guided biopsy (TR-PBx) is the golden standard to detect prostate cancer for patients in whom the disease is suspected.Citation1 However, 65–90% of patients who undergo TR-PBx experience pain,Citation2 and various causes of pain during the procedure have been reported. To reduce this pain, the effect of local anesthesia for patients who underwent TR-PBx has been studied.Citation3,Citation4 The following types of local anesthesia have been reported: intraprostatic local anesthesia, intrarectal local anesthesia, periprostatic nerve block, intrarectal anesthetic gel, and pelvic plexus bloc.Citation4–Citation6 Furthermore, the infiltration-free local anesthesia technique (INFLATE) for transrectal prostatic biopsies with no further needle insertions has recently been introduced for local anesthetic infiltration using transcutaneous electrical nerve stimulation.Citation7 Among these techniques, pelvic nerve block using lidocaine or prilocaine has been reported to have a significant effect on relieving pain during TR-PBxCitation3–Citation8 and is likely the most acceptable method in the current outpatient setting.Citation4,Citation8 Although a randomized study and meta-analysis have shown that periprostatic nerve block alleviates pain during TR-PBx,Citation4,Citation8 lidocaine injection can cause severe pain in comparison with probe insertion and needle piercingCitation8 and an increased risk of systemic infection because of administration via the rectal route. However, the difference in risk between with and without periprostatic nerve block appears to be low.Citation9 Moreover, a prospective studyCitation10 reported that the 10-core biopsy procedure was painful in 131 of 275 patients (47.6%), uncomfortable but not painful in 93 (33.8%), and neither painful nor uncomfortable in 51 (18.6%). Together these findings indicate that local anesthesia in this setting is painful, and some TR-PBx patients do not experience pain caused by the procedure. In this situation, TRUS-PBx without anesthesia is performed at our institute owing to the increase in medical cost and additional risk of morbidity from local anesthesia.Citation11 The issue of whether or not to use an anesthetic in all patients who undergo TR-PBx has not been addressed to date,Citation3–Citation5 although it is critical to know which factors have an effect on the experience of severe pain in the setting of TR-PBx. Although age,Citation4 prostate volume (PV),Citation12 number of biopsy core samples,Citation3 core sampling sites,Citation8 and presence of anxietyCitation13 have been reported as significant predictors for pain during TR-PBx, these results are from studies of patients who received some type of anesthesia or in which the number of patients was small. Therefore, the present study aimed to evaluate factors correlated with pain for patients undergoing TR-PBx without anesthesia.
Methods
This retrospective, single-center study was approved by the institutional review board of Nara Medical University (No. 2782) and complies with the 1964 Declaration of Helsinki and its later amendments. Informed consent was waived because of the retrospective nature of the present study. Informed consent for TR-PBx was obtained from all the patients. All the data were anonymized and confidentiality was maintained. Of 737 patients who underwent TR-PBx between July 2013 and April 2020, 624 patients had complete data available and were enrolled in the study. The indication criteria for biopsy were as follows: abnormal prostate-specific antigen (PSA) value, with the cut-off value defined by the age-specific reference range (<65 years, 3.1 ng/mL; ≥65 years–<70 years, 3.6 ng/mL; ≥70 years, 4.1 ng/mL);Citation11 abnormal findings on digital rectal examination; and abnormal findings on transrectal ultrasound.
Biopsy Procedure
The TR-PBx was performed in an outpatient setting. Patients were placed in the dorsal lithotomy position. None of the patients received anesthesia. In order to prevent infection caused by biopsy, the patients who underwent TR-PBx between July 2013 and February 2017 received premedication with a single dose of 1-g cefazolin by intravenous infusion approximately 30 minutes before TR-PBx, and the patients who underwent TR-PBx between March 2017 and April 2020 received premedication with 500-mg levofloxacin approximately 3 hours before TR-PBx. Pre-procedural anxiety was evaluated using the Faces Anxiety Scale, with scores ranging from 0 to 10 (10 being the worst anxiety; ).Citation14,Citation15 After digital rectal examination was performed, a transrectal probe (Toshiba Medical, Tochigi, Japan) was inserted in the rectum, and the same transrectal probe was used in all the biopsies. The number of allocated biopsy core samples was from 6 to 12 depending on the patient’s age and PV ().Citation11 The order of core sampling was fixed as shown in .Citation11 The low-echoic area was estimated, and PV was calculated using the following formula: length × width × height × 0.5236.Citation16 The biopsy procedure was performed using an 18-gauge, 25-cm-long biopsy gun (Bard, Covington, GA, USA). Pain was evaluated using the Faces Pain Scale, with scores ranging from 0 to 10 (10 being the worst pain; ).Citation17,Citation18 The scale was administered at each puncture by a nurse standing by the patient. Immediately after confirmation of cessation of bleeding from the rectum after the transrectal probe was pulled out, pain from the procedure overall was evaluated using the Faces Pain Scale, and the nurse asked the question, “If this operation must be repeated, would you agree to undergo it again under same conditions?” The TR-PBx duration was defined as the time (minutes) from the first firing of the needle biopsy gun to the removal of the probe.
Statistical Analysis
Statistical analysis was performed using PRISM software, version 8.00 (Graph Pad, San Diego, CA, USA). The χ2-test was used to evaluate differences between categorical variables. Parameters with normal distributions were compared using an unpaired t-test, whereas those that did not demonstrate a normal distribution were compared using the Mann–Whitney U-test to evaluate differences between two groups. Parameters with a normal distribution were compared using one-way analysis of variance, whereas those that did not demonstrate a normal distribution were compared using the Kruskal–Wallis test to evaluate differences between three or more groups. The D’Agostino–Pearson test was used to evaluate the distribution. The test for the linear trend was used to evaluate the tendency for continuous variables. Multivariate linear regression analysis was used to evaluate factors correlated with the Faces Pain Scale. Multivariate logistic regression analysis was used to evaluate the predictive factor for the reply of “Yes” to the question, “If this operation must be repeated, would you agree to undergo it again under same conditions?” A p value <0.05 was considered statistically significant.
Results
Patient characteristics were: mean age at biopsy 70.4 (±7.6) years, mean PSA at biopsy 68.6 (±416) ng/mL, and mean PV by transrectal ultrasound 34.3 (±16.8) mL. The number of core biopsy samples was: 6 cores in 22 patients, 8 cores in 64 patients, 10 cores in 131 patients, and 12 cores in 407 patients. Of the 624 study patients, 351 (56.3%) were diagnosed with prostate cancer by TR-PBx ().
Table 1 Patient Characteristics, Pathological Findings, and Biopsy Data
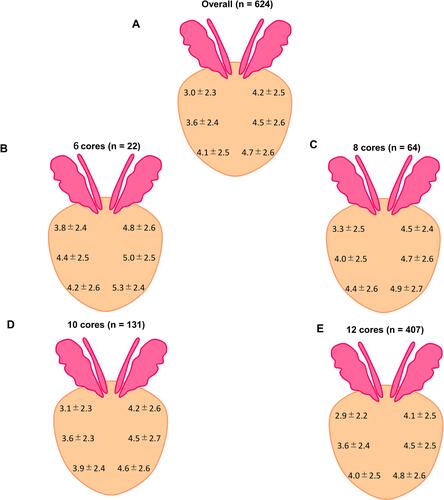
The Faces Pain Scale score increased significantly as the number of core samples increased for patients overall based on the test for linear trend, as follows: Core 1, 2.9 ± 2.3; Core 2, 3.3 ± 2.3; Core 3, 3.6 ± 2.4; Core 4, 3.8 ± 2.4; Core 5, 4.0 ± 2.5; Core 6, 4.1 ± 2.6; Core 7, 4.2 ± 2.5; Core 8, 4.3 ± 2.5; Core 9, 4.5 ± 2.6; Core 10, 4.6 ± 2.6; Core 11, 4.7 ± 2.6; Core 12, 4.7 ± 2.7 (). Trends in severe pain as the number of cores increased were shown among patients with 6 cores (), 8 cores (), 10 cores (), and 12 cores (). Comparison of the Faces Pain Scale scores based on the core sampling sites showed these results for patients overall: pain experienced with samples of right lobe at the apex (4.1 ± 2.5) was significantly (p < 0.001) higher than samples at the base (3.0 ± 2.3) was not significantly (p = 0.27) higher than samples on the left lobe base (4.2 ± 2.5; ). Duration of the TR-PBx (95% CI, 0.01–0.085, p = 0.012) and the Faces Anxiety Scale score (95% CI: 0.058–0.20, p = 0.0005) were significantly (p = 0.016) correlated with the Faces Pain Scale score for the completed procedure ().
Table 2 Predictive Factors for the Faces Pain Scale Scores
Figure 3 The Faces Pain Scale at each core taken (A) in total number of patients (B) in patients who underwent 6 core biopsies (C) in patients who underwent 8 core biopsies (D) in patients who underwent 10 core biopsies (E) in patients who underwent 12 core biopsies.
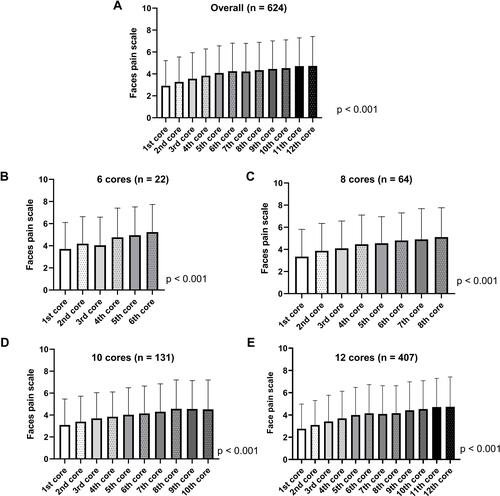
Figure 4 The Faces Pain Scale at each site of cores taken during biopsy (A) in total number of patients (B) in patients who underwent 6 core biopsies (C) in patients who underwent 8 core biopsies (D) in patients who underwent 10 core biopsies (E) in patients who underwent 12 core biopsies.
In response to the question, “If this operation must be repeated, would you agree to undergo it again under same conditions?” of the 624 patients 370 (59.3%) answered “Yes,” 126 (20.2%) answered “No,” and 128 (20.5%) answered that “It is difficult to decide Yes or No.” In multivariate analysis, a short duration of the TR-PBx procedure (odds ratio [OR] 0.96; 95% CI, 0.93–0.99; p = 0.016) and low anxiety score (OR, 0.93, 95% CI, 0.87–0.99; p = 0.022) predicted the reply “Yes” for the question, “If this operation must be repeated, would you agree to undergo it again under same conditions?” ().
Table 3 Predictive Factors for the Reply of “Yes” to the Post-Procedure Question: “If This Operation Must Be Repeated, Would You Agree to Undergo It Again Under Same Conditions?”
Discussion
The present study shows that, for patients who underwent TR-PBx without anesthesia, a long duration of TR-PBx and a high anxiety score predict a high pain score and unwillingness to undergo the procedure again. Furthermore, 59.6% of patients answered “Yes” to the question, “If this operation must be repeated, would you agree to undergo it again under same conditions?” To the best knowledge of these authors, this study is the first to precisely evaluate patients’ experience of pain during TR-PBx without anesthesia in a moderate sample size. The results indicate that anesthesia and/or treatment to reduce anxiety before TR-PBx should be considered in patients with high anxiety and that the duration of TR-PBx should be as short as possible to improve pain during the procedure.
The number of core samples taken has been considered to be a predictor for pain during TURS-PBx;Citation3 however, across the literature some authors did not agree on this point.Citation19,Citation20 In the present study, the pain during TR-PBx gradually accumulated from the first core sampling to the last, which is called pain accumulation.Citation21 However, the number of core biopsy samples did not predict overall pain after the procedure was complete, in contrast to the predictive value of a long duration of TR-PBx. Demirtaş et alCitation22 reported no significant difference between patients who underwent multiparametric magnetic resonance imaging-guided fusion prostate biopsy and those who underwent the standard TR-PBx with regard to visual analog pain scale score (p = 0.070), although the number of cores taken in the patients who underwent the former procedure was significantly higher than that in the patients who underwent the latter procedure. Furthermore, Arsov et alCitation20 reported that procedural pain in patients who received magnetic resonance imaging-guided in-bore biopsy (mean pain score ± standard deviation [SD], 2.95 ± 2.15) with a mean number of 5.6 cores and mean procedure time of 42 minutes was significantly higher (p < 0.001) than those values for patients who received magnetic resonance imaging/ultrasound fusion-guided plus systematic biopsy (mean pain score ± SD, 1.95 ± 1.56) with a mean number of 17.4 cores and mean procedure time of 28 minutes. These results, considered with the findings of the present study, indicate that the duration of TR-PBx has strong correlation with pain caused by the procedure itself, and not the number of core samples. In these patients, the duration of TR-PBx is longer as a higher number of core samples are taken; therefore, pain accumulation may be caused by the longer duration of the procedure, not by the higher number of cores sampled.
Anxiety before undergoing TR-PBx is another important factor for pain during the procedure.Citation10,Citation13,Citation23 Pre-procedure anxiety for patients undergoing TR-PBx has a significant linear correlation with pain during the procedure, as shown in the present study. When receiver operating characteristic analysis was performed to evaluate the correlation between significant pain (Faces Pain Scale score of ≥4.0)Citation24 or “Yes” for the question, “If this operation must be repeated, would you agree to undergo it again under same conditions?” and the anxiety score, the cut-off values (the point closest to the upper left-hand corner of the curve) was 3.5 and 4.5. Therefore, treatment to reduce anxiety can be considered when a patient has a score of ≥4 on the Faces Anxiety Scale. Other studies have investigated the possibility of music,Citation24 sedation,Citation25 stress management,Citation26 and short time for preparation to undergo TR-PBxCitation13 to reduce pre-procedure anxiety; however, the use of these methods to alleviate anxiety in this setting has not been established.
Prostate volume has been reported as predictor for pain caused by TR-biopsy.Citation12,Citation27 In the present study, PV did not correlate with pain caused by TR-biopsy. Sonmez et alCitation12 reported the PV cut-off value that indicated higher risk of experiencing pain during TR-PBx was >61.6 mm3; however, in the present study, only 39 (6.2%) patients had a PV > 61.6 mm3, which may explain the discrepancy between the previous study results and those of the present study.
The biopsy sampling site is another factor in the experience of pain during TR-PBx. Bastide et alCitation27 reported that patients for whom the first biopsy sampling started at the apex of the prostate had higher pain scores than those in whom the sampling started from the base. Their results suggest puncture at the prostate apex may cause more severe pain compared with the base. In contrast, Rodríguez et alCitation28 reported that the amount of discomfort during prostate biopsy was not associated with the location of the sampling site. Similarly, in the present study, the site where needle pierced did not seem correlate with pain caused by the biopsy.
Patient age has been reported both to correlate with pain during TR-PBxCitation4 and not to correlate with pain,Citation13 as in the present study. Macefield et alCitation29 reported that anxiety was stronger in young patients age 50–69 years who underwent prostate biopsy. Therefore, the differences in findings among reports for the correlation of age with pain can reflect the proportion of young patients studied, especially those age <60 years, and is not considered to be a confounding factor of anxiety. In the present study, only 17 of the 624 patients were age <60 years and were evaluated for the predicting factors for pain, including anxiety. Therefore, it seems that in the present study that patient age had no significant correlation with pain during TR-PBx.
The body mass index (BMI) did not show any significant correlation with pain during TR-PBx in the present study and in the study by Sonmez et al.Citation12 Obesity could be significantly correlated with hemorrhoidsCitation30 and prostatitis.Citation31 Therefore, BMI could have had a significant correlation with pain during TR-PBx. However, BMI appears to have no significant correlation with pain during TR-PBx.
The cancer detection rate in patients with 6, 8, 10, and 12 cores removed in the present study was heterogenous. It was observed to increase as the number of cores removed decreased (chi-squared test: p < 0.001). In the present study, the number of cores was determined according to age and PV, and old age and small prostate size have been reported to be indicators of positive results of TR-PBx.Citation32,Citation33 Although the mean PSA in the patients with 12 cores was higher than that in the patients with 10 cores, the proportion of patients with >20-ng/mL PSA among the patients with 12 cores (15.5%, 63/407) was nearly the same as that among the patients with 10 cores (16.0%, 21/131). Therefore, the heterogeneity of the cancer detection rate may be caused by age and PV.
The present study has some limitations. First, data were obtained from a single institution. Second, the operators of TR-PBx were mosaic: ≥10 operators worked as urologists for 1–4 years, and the differences among operators may have affected the duration of the TR-PBx procedure.
Conclusions
Even in patients who underwent TR-PBx without anesthesia, 59.3% (370 of 624) agreed to undergo TR-PBx again under same conditions. A long duration of the TR-PBx procedure and strong anxiety had a significant correlation with strong pain during TR-PBx performed without anesthesia, whereas a short time during the TR-PBx procedure and weak anxiety correlated with patients who received TR-PBx without anesthesia agreeing to undergo the procedure again under same conditions.
Acknowledgment
We would like to thank Enago for English language editing.
Disclosure
The authors declare that they have no conflicts of interest.
References
- Ochiai A. Changes in the roles of transrectal ultrasonography for the diagnosis of prostate cancer. J Med Ultrason. 2017;44(1):1–2. doi:10.1007/s10396-016-0756-3
- Clayton DB, Spencer CL, Amling CL. Practice patterns in transrectal ultrasound guided prostate biopsy: results of a questionnaire survey of practicing urologists. J Urol. 2008;179:712–716. doi:10.1016/S0022-5347(08)62077-7
- De Sio M, D’Armiento M, Di Lorenzo G, et al. The need to reduce patient discomfort during transrectal ultrasonography-guided prostate biopsy: what do we know? BJU Int. 2005;96(7):977–983. doi:10.1111/j.1464-410X.2005.05736.x
- Li M, Wang Z, Li H, et al. Local anesthesia for transrectal ultrasound-guided biopsy of the prostate: a meta-analysis. Sci Rep. 2017;7:40421. doi:10.1038/srep40421
- Kim DK, Lee JY, Jung JH, et al. What is the most effective local anesthesia for transrectal ultrasonography-guided biopsy of the prostate? A systematic review and network meta-analysis of 47 randomized clinical trials. Sci Rep. 2019;9(1):4901. doi:10.1038/s41598-019-41412-w
- Sönmez G, Baydilli N, Tombul ŞT, Güler G, Demirtaş A. Comparison of lidocaine and Prilocaine efficiencies in periprostatic nerve block for transrectal prostate biopsy: a randomized prospective study. uob. 2019;18(1):1–5. doi:10.4274/uob.galenos.2018.1096
- Bolat MS, Cinar O, Asci R, Buyukalpelli R. A novel method for pain control: infiltration free local anesthesia technique (INFLATE) for transrectal prostatic biopsy using transcutaneous electrical nerve stimulation (TENS). Int Urol Nephrol. 2019;51(12):2119–2126. doi:10.1007/s11255-019-02277-0
- Ashley RA, Inman BA, Routh JC, et al. Preventing pain during office biopsy of the prostate: a single center, prospective, double-blind, 3-arm, parallel group, randomized clinical trial. Cancer. 2007;110(8):1708–1714. doi:10.1002/cncr.22973
- Pradere B, Veeratterapillay R, Dimitropoulos K, et al. Nonantibiotic strategies for the prevention of infectious complications following prostate biopsy: a systematic review and meta-analysis. J Urol. 2020;7:101097JU0000000000001399.
- Peyromaure M, Ravery V, Messas A, Toublanc M, Boccon-Gibod L, Boccon-Gibod L. Pain and morbidity of an extensive prostate 10-biopsy protocol: a prospective study in 289 patients. J Urol. 2002;167(1):218–221. doi:10.1016/S0022-5347(05)65416-X
- Hori S, Tanaka N, Nakai Y, et al. Comparison of cancer detection rates by transrectal prostate biopsy for prostate cancer using two different nomograms based on patient’s age and prostate volume. Res Rep Urol. 2019;11:61–68. doi:10.2147/RRU.S193933
- Sonmez G, Tombul ST, Demirtas T, Demirtas A. Risk factors associated with pain in fusion prostate biopsy. Prostate Int. 2020;8(4):185–189. doi:10.1016/j.prnil.2020.05.004
- Saraçoğlu T, Unsal A, Taşkın F, Sevinçok L, Karaman CZ. The impact of pre-procedural waiting period and anxiety level on pain perception in patients undergoing transrectal ultrasound-guided prostate biopsy. Diagn Interv Radiol. 2012;18(2):195–199. doi:10.4261/1305-3825.DIR.4643-11.1
- McKinley S, Coote K, Stein-Parbury J. Development and testing of a Faces Scale for the assessment of anxiety in critically ill patients. J Adv Nurs. 2003;41(1):73–79. doi:10.1046/j.1365-2648.2003.02508.x
- Mino T. Development of the face scale to evaluate anxiety and fear on dental treatment. Okayama Shigakukai Zassi. 2012;31:1–12.
- Terris MK, Stamey TA. Determination of prostate volume by transrectal ultrasound. J Urol. 1991;145(5):984–987. doi:10.1016/S0022-5347(17)38508-7
- Whaley LF, Wong DL. Nursing Care of Infants and Children. St Louis: Mosby; 1987.
- Savino F, Vagliano L, Ceratto S, Viviani F, Miniero R, Ricceri F. Pain assessment in children undergoing venipuncture: the Wong-Baker faces scale versus skin conductance fluctuations. PeerJ. 2013;1:e37. doi:10.7717/peerj.37
- Chesnut GT, Zareba P, Sjoberg DD, et al. Patient-reported pain, discomfort, and anxiety during magnetic resonance imaging-targeted prostate biopsy. Can Urol Assoc J. 2020;14(5):E202–E208. doi:10.5489/cuaj.6102
- Arsov C, Rabenalt R, Quentin M, et al. Comparison of patient comfort between MR-guided in-bore and MRI/ultrasound fusion-guided prostate biopsies within a prospective randomized trial. World J Urol. 2016;34(2):215–220. doi:10.1007/s00345-015-1612-6
- Kaver I, Mabjeesh NJ, Matzkin H. Randomized prospective study of periprostatic local anesthesia during transrectal ultrasound-guided prostate biopsy. Urology. 2002;59(3):405–408. doi:10.1016/S0090-4295(01)01538-2
- Demirtaş A, Sönmez G, Tombul ŞT, Demirtaş T. Comparison of pain levels in fusion prostate biopsy and standard TRUS-guided biopsy. Int Braz J Urol. 2020;46(4):557–562. doi:10.1590/s1677-5538.ibju.2019.0154
- Tekdogan U, Tuncel A, Nalcacioglu V, Kisa C, Aslan Y, Atan A. Is the pain level of patients affected by anxiety during transrectal prostate needle biopsy? Scand J Urol Nephrol. 2008;42(1):24–28. doi:10.1080/00365590701514555
- Song M, Li N, Zhang X, et al. Music for reducing the anxiety and pain of patients undergoing a biopsy: a meta-analysis. J Adv Nurs. 2018;74(5):1016–1029. doi:10.1111/jan.13509
- Turgut AT, Ergun E, Koşar U, Koşar P, Ozcan A. Sedation as an alternative method to lessen patient discomfort due to transrectal ultrasonography-guided prostate biopsy. Eur J Radiol. 2006;57(1):148–153. doi:10.1016/j.ejrad.2005.08.001
- Chiu LP, Tung HH, Lin KC, et al. Effectiveness of stress management in patients undergoing transrectal ultrasound-guided biopsy of the prostate. Patient Prefer Adherence. 2016;10:147–152. doi:10.2147/PPA.S96991
- Bastide C, Lechevallier E, Eghazarian C, Ortega JC, Coulange C. Tolerance of pain during transrectal ultrasound-guided biopsy of the prostate: risk factors. Prostate Cancer Prostatic Dis. 2003;6(3):239–241. doi:10.1038/sj.pcan.4500664
- Rodríguez LV, Terris MK. Risks and complications of transrectal ultrasound guided prostate needle biopsy: a prospective study and review of the literature. J Urol. 1998;160(6 Pt 1):2115–2120. doi:10.1016/S0022-5347(01)62255-9
- Macefield RC, Lane JA, Metcalfe C, et al. Do the risk factors of age, family history of prostate cancer or a higher prostate specific antigen level raise anxiety at prostate biopsy? Eur J Cancer. 2009;45(14):2569–2573. doi:10.1016/j.ejca.2009.03.016
- Lee JH, Kim HE, Kang JH, Shin JY, Song YM. Factors associated with hemorrhoids in Korean adults: Korean national health and nutrition examination survey. Korean J Fam Med. 2014;35(5):227–236. doi:10.4082/kjfm.2014.35.5.227
- Wallner LP, Clemens JQ, Sarma AV. Prevalence of and risk factors for prostatitis in African American men: the flint Men’s Health Study. Prostate. 2009;69(1):24–32. doi:10.1002/pros.20846
- Tanaka N, Fujimoto K, Yoshikawa M, et al. Prostatic volume and volume-adjusted prostate-specific antigen as predictive parameters for T1c prostate cancer. Hinyokika Kiyo. 2007;53(7):459–465.
- Al-Azab R, Toi A, Lockwood G, Kulkarni GS, Fleshner N. Prostate volume is strongest predictor of cancer diagnosis at transrectal ultrasound-guided prostate biopsy with prostate-specific antigen values between 2.0 and 9.0 ng/mL. Urology. 2007;69:103–107. doi:10.1016/j.urology.2006.09.041