Abstract
Background
Since its introduction over two decades ago, the surgical laser has served in the lithotripsy of urinary calculi, resection of bladder tumours, bladder neck incisions, and prostate enucleation. Concerns regarding the safe use of holmium lasers have resulted in potentially excessive and overly precautious theatre regulations. We aimed to evaluate the preconceived impressions and practice patterns at a single site surrounding laser use in endourology.
Methods
We designed a three-part online questionnaire that could be accessed using a smart device or computer. This survey was distributed to all theatre staff involved in laser surgery at our single site, including surgical, nursing, and anaesthetic staff of varying seniority. It asked questions regarding holmium laser safety, provided an up-to-date summary of published literature surrounding the safe use of lasers, and finally gave participants further option to alter the answers to several previously encountered questions.
Results
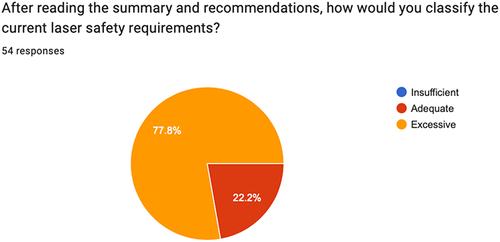
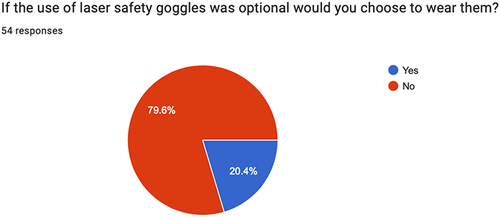
A total of 54 theatre staff completed the survey, including 17 theatre nurses (31.5%), 10 urology consultants (18.5%), 8 urology registrars (14.8%), 7 anaesthetic registrars (13%), 4 anaesthetic consultants (7.4%). About 51.9% of participants believed that current laser safety protocols were adequate, with 38.9% finding them excessive. After reading recently published information on laser safety, 22.2% thought current laser safety measures were adequate (57% decrease) and 77.8% found them to be excessive (100% increase). About 74.1% of participants found that laser safety goggles impair their vision and that 79.6% would choose not to wear them if they were optional.
Conclusion
Strict laser safety guidelines reflect an overestimated risk associated with using holmium laser in operating theatres. Laser safety regulations should be re-evaluated to align with current research and potential hazards inherent to the device. In doing so, a more effective distribution of staff could enable greater access to laser surgery, thereby reducing patient morbidity and hospital wait times.
Keywords:
Background
Holmium:yttrium-aluminum-garnet (Ho:YAG) laser energy source is the cornerstone of endourology and minimally invasive interventions such as ureteroscopy, holmium enucleation of prostate (HoLEP), and transurethral resection of bladder tumours (TURBT).Citation1 The field of laser surgery is constantly evolving, incorporating different laser platforms, modifications such as pulse modulation and various energy sources such as holmium or thulium. With the incidence of stone disease increasing in recent years, there has been a shift towards primary ureteroscopy (URS) with laser lithotripsy in the acute setting. As the overall demand for primary laser surgery increases in the future, additional strain will be placed on the hospitals to provide emergency theatres that are deemed “laser safe” and staffed by laser qualified personnel. Despite the many benefits of laser use in urology, some disadvantages remain. Laser equipment is costly, the operating surgeon requires training, and strict safety precautions must be adhered to.Citation2
The holmium laser is classified as a class 4 laser, meaning it can cause skin and eye damage from direct contact.Citation1 URS is regarded as a safe and effective procedure overall, however adverse events can occur and involve patients, surgeons, and theatre staff alike. The majority of complications involve the patient, with ureteric injury, bleeding, thermal damage, and delayed ureteric stricturing being well reported and often correlate to user experience.Citation2,Citation3 Extracorporeal injury to the surgeon, patient, and theatre staff, however, is possible but less common.Citation3 The majority of the literature on laser surgery focuses on outcomes and intra-operative complications. There is a scarcity of information on laser usage, practical considerations, and specific guidance on the correct set up and usage of the laser.Citation4 This lack of discussion may contribute to the fear of laser usage in theatre and the strict safety measures that are implicated.
Concerns regarding the safety of holmium laser have recently been addressed and published as part of the Canadian Urological Association (CUA) best practice reports by Bhojani et al 2020,Citation5 They report that in the last two decades, there have been no reported injuries associated with the use of Ho:YAG laser.Citation2,Citation3 Further, they refute the standardised mandatory wearing of laser safety goggles for all operating room staff, providing evidence that corneal injury from exposure to laser energy occurs at distances within 5cm and that prescription glasses are as protective as laser safety goggles.Citation1,Citation4 Here, we present a review of laser theatre staffs’ opinions and preconceived notions regarding laser safety and protocols at our single site. Our goal was to characterise the preconceived impressions regarding laser safety held by all intraoperative staff, including anaesthetic and nursing staff. By advocating for an update to the stringent laser safety regulations, we aim to improve access to emergency and after-hours laser surgery to benefit both the patient and hospital system alike.
Methodology
We designed a short three-part questionnaire that could be accessed on smartphones or any computer (). The three-part survey was emailed to an institutional Email list comprising all doctors and nurses affiliated with urology surgery at our single site. Part one consisted of questions relating to laser safety. Part two allowed participants to view the summary and recommendations from the CUA best practice guidelines (). Finally, part three gave participants the option to re-evaluate their answers to part one ().
Table 1 Laser Safety Survey Parts and Questions
Table 2 Recommendations on Ho:YAG Laser Safety by the Canadian Urological Association
Data were collected anonymously through the survey application. Analysis of data and formulation of figures was performed by the lead investigator.
Results
Demographics
We had a total of 54 responses to our radiation safety quiz; the breakdown consisted of 17 theatre nurses (31.5%), 10 urology consultants (18.5%), 8 urology registrars (14.8%), 7 anaesthetic registrars (13%), 4 anaesthetic consultants (7.4%) (Supplementary Figure 1 in Supplementary File 1).
Institutional Laser Safety and Laser Utilisation
The majority of participants (57.4%) have undergone formal laser safety training (Supplementary Figure 2 in Supplementary File 1). About 61.1% of respondents had been involved in more than 20 procedures using Ho:YAG laser (Supplementary Figure 3 in Supplementary File 1).
Key Results
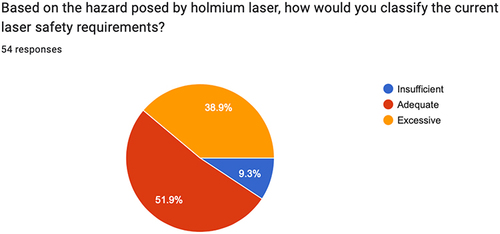
Just over half (55.6%) of responders answered true to the question – Eye damage can occur by looking into the “green light beam” even if the laser is not activated? (). About 70.4% did not believe that normal prescription glasses would protect against laser-induced eye damage (). Only 38.9% of respondents correctly answered <5cm for the question “If the laser fibre is activated and there is no intervening barrier (no fluid or solid), what is the minimum distance for the laser to cause damage? (). About 74.1% of participants found that laser safety goggles impair their vision and that 79.6% would not choose to wear them if they were optional ( + ). Prior to reading the CUA's best practice recommendations, approximately half (51.9%) of participants believed that current laser safety protocols were adequate, with 38.9% feeling they were excessive (). After reading the findings, however, 22.2% thought current laser safety measures were adequate and 77.8% found them to be excessive ().
Figure 1 Responses to the above question “Eye damage can occur by looking into the green light beam even if the laser is not activated” expressed as a percentage of True/False.
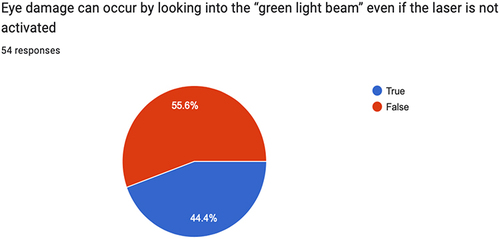
Figure 2 Responses to the above question “Normal prescription glasses protect against laser induced eye damage” expressed as a percentage of True/False.
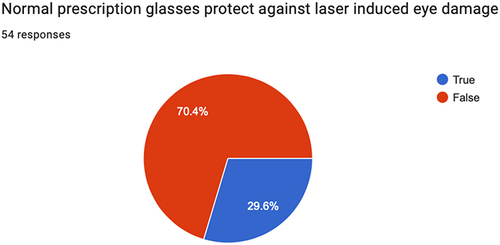
Figure 3 Responses to the above question “If the laser fibre is activated and there is no intervening barrier (no fluid or solid) what is the minimum distance to avoid injury?” represented as a percentage of total answers.
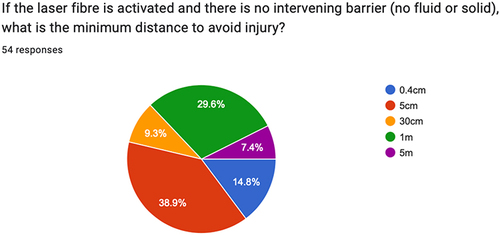
Figure 4 Responses to the above question “Do you find that the laser protection glasses impair your vision?'” represented as a percentage of Yes/No answers.
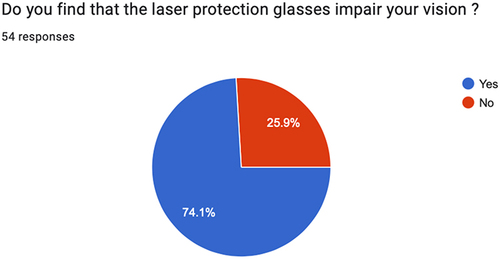
Figure 5 Responses to the above question “Based on the hazard posed by the holmium laser, how would you classify the current laser safety requirments?” represented as a percentage of Yes/No answers.
Discussion
Laser technology has improved significantly in the last two decades, with holmium laser forming a cornerstone for a variety of endourological procedures.Citation6 Risk factors for holmium laser adverse effects have been well described, relating to energy, pulse energy, and distance from the target to the laser fibre tip.Citation7 Despite current data and recommendations for the update of laser safety protocols, outdated blanket laser safety policies remain. The occupational health and safety of staff and patients remains paramount, however modern policies need to reflect current evidence-based research to ensure that scarce hospital resources can be allocated effectively.
Despite the majority of staff completing laser safety training and having been involved in >20 laser cases, the vast majority of questions were answered incorrectly. This further highlights the limited understanding staff have on how lasers work in surgery and the safety measures needed to facilitate their usage. This lack of education and scarcity of up-to-date knowledge only perpetuates outdated notions on laser safety.
A study by Althunayan et al reviewed all adverse events attributed to laser surgery by utilising both the Rockwell Laser Industries Laser Accident Database from 1992 to 2012 and the mandatory reporting systems of adverse events developed by the US Food and Drug Administration.Citation2 With regard to operator/staff injuries attributable to the Ho:YAG laser, only 11 cases of minor skin burns have been reported and occurred due to firing a broken laser fibre. Importantly, no eye injuries have been reported during the 20-year history of the two databases. Furthermore, a study conducted by Villa et al used ex-vivo porcine eyes to establish at what distance a Ho:YAG laser would cause eye damage when conducted through room air. The study compared no protection to prescription eyeglasses and laser safety goggles at a variety of commonly used laser settings. This study determined that without eye protection, a Ho:YAG laser must be activated within 5cm of the eye to cause damage.Citation8 Additionally, it was shown that prescription glasses and laser goggles were equally efficacious at preventing eye injury at all distances and all laser power settings.Citation8 It is important to recognise that these findings are specific to Ho:YAG laser and does not apply to other laser platforms such as Thulium Fibre Laser (TFL) which have been shown to cause eye damage and distances up to 10cm.Citation9
About 74.1% of staff found laser goggles to impair their vision. This is significant as endourology utilises expensive and difficult to handle equipments such as 200nm laser fibres and hydrophilic guide wires. Vision and dexterity are paramount to safely handling these devices while maintaining sterility. Similarly, the operating surgeon requires optimal vision throughout the case to ensure patient safety while performing an effective operation. These results mirror those presented by Paterson et al, where 264 Urologists who regularly perform laser surgery were asked to complete a survey. This survey revealed that 40% of urologists routinely wore laser safety goggles and that 70% of respondents reporting that laser goggles impaired their vision during surgery.Citation10
With this in mind, and after reading the best practice recommendations from the CUA- 77.8% of participants found the current laser safety requirements to be excessive. If the option of wearing laser safety goggles was given to the participating staff members, nearly 80% would choose not to wear them. Therefore, by mandating a compulsory use of laser safety goggles, a competing risk is created, as the majority of staff reported a significant reduction in their vision. Reducing the vision of the operating surgeon may impair their ability to complete a surgical case and increase the risk of adverse events to themselves, the patient, and surrounding staff. Interestingly, drug administration errors by anaesthetic staff have also been attributed to impaired vision while wearing laser safety goggles.Citation11
At our tertiary hospital, institutional laser safety includes a formal laser safety policy, a dedicated on-duty laser safety officer, and a laser safety committee. Mandated safety measures for the operating theatre include “in use” laser signs, laser warning barriers, window shades, mandatory laser goggles, and a dedicated extra numerary laser safety nurse. All laser nursing staff are required to complete their laser safety education before working in a laser theatre; however, this is not compulsory for urology or anaesthetic staff. Because of these staffing and theatre requirements, the access and ability to staff a laser safe theatre after hours is incredibly limited. This means patients who would otherwise be offered a primary ureteroscopy and laser within hours are instead offered a temporising surgery in the form of ureteric stent placement. Ureteric stenting is associated with significant patient morbidity, with patients having to wait an additional 3–4 weeks before their definitive surgery.Citation12 This means another hospital stay, another general anaesthetic, and another surgical procedure with additional surgical risks. By rationalising these strict and outdated blanket rules, more patients would receive definitive laser surgery as a primary procedure, reducing morbidity, hospital length of stay, and abolishing the need for subsequent surgeries. With rising pressures surrounding hospital bed availability, theatre staff shortages, and emergency theatre availability after hours, strict, potentially unnecessary/excessive laser safety guidelines can delay surgical timelines, contribute to bed shortages, and may impair patient outcomes.
Conclusion
Evidence to support mandatory eye protection and stringent laser theatre safety rules is not contemporary. The continued implementation of mandatory laser safety goggles in laser specific operating theatres overestimates the inherent risk associated with modern Ho:YAG laser systems. With current laser platforms being significantly safer compared to their predecessors, institutional safety standards must be updated to reflect current research and technology. In doing so, we aim to see improved access to laser surgery with the ultimate goal of reducing patient morbidity and improving patient turnover, particularly after hours. The current study was limited by the sample size of the single site surveyed. We aim to reproduce this study at the national level in the near future.
Data Sharing Statement
Anonymised data are provided in supplementary file 2.
Ethics Statement
As this research survey involves low/negligible risk and only uses existing non-identifiable data, it is exempt from the Australian Human Resource Ethics Committee (HREC) review. This is in accordance with the Australian National Statement on Ethical Conduct in Human Research (2007) laws.
Consent
All participants gave informed consent prior to participation in the study.
Disclosure
The authors have no conflicts of interest to declare for this work.
Acknowledgments
The above abstract has been submitted and presented at the BJUI meeting.
References
- Smalley PJ. Laser safety: risks, hazards, and control measures. Las Therapy. 2011;20(2):95–106. doi:10.5978/islsm.20.95
- Althunayan AM, Elkoushy MA, Elhilali MM, Andonian S. Adverse events resulting from lasers used in urology. J Endourol. 2014;28(2):256–260. doi:10.1089/end.2013.0451
- Liang H, Liang L, Yu Y, et al. Thermal effect of holmium laser during ureteroscopic lithotripsy. BMC Urol. 2020;20(1):69.
- Herrmann TRW, Liatsikos EN, Nagele U, Traxer O, Merseburger AS. European Association of Urology guidelines on laser technologies. Actas Urológicas Españolas. 2013;37(2):63–78. doi:10.1016/j.acuro.2012.05.005
- Bhojani N, Andonian S, Watterson JD, et al. Canadian urological association best practice report: holmium:YAG laser eye safety. Can Urol Assoc J. 2020;14(12):380–382. doi:10.5489/cuaj.6941
- Kronenberg P, Traxer O. Update on lasers in urology 2014: current assessment on holmium:yttrium–aluminum–garnet (Ho:YAG) laser lithotripter settings and laser fibers. World J Urol. 2015;33(4):463–469. doi:10.1007/s00345-014-1395-1
- Donnell RF. Laser safety and clinical application in urology. AUA Update Seri. 2013;32:Lesson.
- Villa L, Cloutier J, Compérat E, et al. Do we really need to wear proper eye protection when using holmium:YAG laser during endourologic procedures? Results from an ex vivo animal model on pig eyes. J Endourol. 2016;30(3):332–337. doi:10.1089/end.2015.0232
- Lee MJ, Czajkowski S, Gershon A, et al. Better safe than sorry? Results from an ex-vivo study demonstrate that the thulium fiber laser may cause eye injury without standard protection. Can Urol Assoc J. 2022;16(8):283–288. doi:10.5489/cuaj.7770
- Paterson NR, Fitzpatrick R, Blew B, Denstedt J, Watterson J. Perceptions and practice patterns of holmium laser goggles in endourological procedures: an unnecessary evil? J Endourol. 2019;33(2):146–150. doi:10.1089/end.2018.0432
- Park JC, Herbert EN. Laser goggles alter the perceived colour of drug labels, increasing the risk for drug errors. Can J Ophthalmol. 2013;48(2):e27–8. doi:10.1016/j.jcjo.2012.10.011
- Richter S, Ringel A, Shalev M, Nissenkorn I. The indwelling ureteric stent: a ‘friendly’ procedure with unfriendly high morbidity. BJU Int. 2000;85(4):408–411. doi:10.1046/j.1464-410x.1998.00543.x-i1