Abstract
Aim
To review our 10 years of experience with the endoscopic treatment of vesicoureteral reflux (VUR) in children, emphasizing the long-term efficacy of the “combined STING-HIT” technique.
Materials and Methods
A retrospective study was performed including all children with symptomatic VUR undergoing the cystoscopic injection of bulking agents from January 2013 to December 2022 in our pediatric tertiary referral center. Three different endoscopic techniques were adopted: the “combined STING-HIT” technique, the STING technique, and the HIT technique. Treatment success was defined as symptom remission and VUR resolution on the voiding cystourethrogram (VCUG) performed at the 3-month follow-up.
Results
In the study period, 140 (F:M = 64:76) patients and 228 ureters were treated at a median patient age of 3 (2.0–6.0) years. After a single endoscopic treatment, VUR resolved in 203 (88%) ureters. The VUR resolution rate after a single endoscopic treatment was 95% (n=70/74) in case of I–II VUR, 88% (n=87/99) in case of III VUR; 83% (n=38/46) in case of IV VUR; 89% (n=8/9) in case of V VUR (p-value: 0.174). Overall, one or two endoscopic treatments succeeded in 219 (96%) ureters. The overall VUR resolution rate following one or two endoscopic treatments was 100% (74/74) in case of I–II VUR, 93% (n=92/99) in case of III VUR; 96% (n=44/46) in case of IV VUR; 100% (n=9/9) in case of V VUR (p-value: 0.083). Despite not being statistically significant, the VUR resolution rate was higher for the “combined STING-HIT” technique, both after one (92%: n=110/119; versus 85%; n=62/73 versus 86%; n=31/36; p-value: 0.225) or two (98%: n=116/119; versus 95%; n=69/73 versus 94%; n=34/36; p-value: 0.469) endoscopic treatments.
Conclusion
The endoscopic approaches were highly successful for the treatment of VUR in children. The “combined STING-HIT” technique was a safe and effective procedure, being associated with the higher resolution rate.
Introduction
Vesicoureteric reflux (VUR) consists of the backflow of urine from the bladder to the upper urinary tract due to the incompetence of the vesicoureteral junction. It is a very common urological anomaly in pediatrics with a reported incidence of nearly 1–3% of children.Citation1,Citation2
Patients with symptomatic VUR present with a wide range of severity and several treatment options have been described so far.Citation3–7 The main goal of the management of VUR is the preservation of kidney function, by minimizing the risk of potentially serious consequences, including renal scarring, hypertension, and kidney failure.Citation3–7 Ranging from continuous antibiotic prophylaxis to endoscopic, minimally invasive, or open approaches, controversy persists over the optimal management of VUR in children, particularly about the choice of the most effective treatment techniques and their best timing.Citation5–8
Thanks to its low invasiveness and morbidity, the cystoscopic injection of bulking agents has become a popular alternative for the treatment of VUR.Citation5,Citation6,Citation9–11
The first endoscopic technique for the treatment of VUR was named “subureteric Teflon injection” or “STING” procedure. It was first described by Matouschek in 1981Citation12 and subsequently independently popularized by O’Donnell and Puri in 1984.Citation13 In its original description, a specially designed 5F polyethylene catheter ending in an 18G needle was inserted cystoscopically 2–3 mm below the ureteric orifice and then advanced 0.5 cm into the space behind the intravesical ureter. 0.2–0.5 mL polytef paste (Ethicon) was then injected into the bladder submucosa to treat the urine reflux.Citation5,Citation6
In 2004, KirschCitation14 described an alternative endoscopic technique, named the hydrodistension implantation technique (HIT), in which the lumen of the distal ureter was distended by hydrostatic pressure, and the bulking agent was injected 4 mm into the submucosa of the mid/distal ureteral tunnel at the 6-o’clock position.Citation5,Citation6
To date, despite several other modifications have been proposed, including the ureteral reposition techniqueCitation7,Citation10,Citation15–18 and the double-HIT method,Citation19–21 the ideal endoscopic procedure for the treatment of VUR has yet to be identified and the choice is still dependent on the surgeon’s preference and experience.
Since 2010 in our pediatric tertiary referral center, we have adopted a new technique for the treatment of symptomatic VUR in children named the “combined STING-HIT” technique. It consists of the injection of the bulking agent into the submucosa of the intramural ureter followed by a second subureteral implantation of the paste.
The aim of this study was, therefore, to present our retrospective data and compare the efficacy of the conventional STING and HIT techniques and the “combined STING-HIT” technique.
Patients and Methods
Patient Selection
A retrospective study was performed including all children with symptomatic VUR undergoing cystoscopic injection of bulking agents from January 2013 to December 2022 in our pediatric tertiary referral center. All patients suffered from symptomatic and radiologically proven VUR, as defined by the International Reflux Study Committee.Citation22
Indications for the endoscopic treatment of VUR were recurrent febrile urinary tract infections (UTI) resistant to continuous antibiotic prophylaxis, poor compliance with continuous antibiotic prophylaxis, and severe renal scarring on the preoperative renal nuclear scan.
According to the Food and Drug Administration (FDA) regulation, the endoscopic treatment was performed in the case of symptomatic VUR grades III–V. The bulking agent was also injected in the contralateral ureter affected by VUR grade I–II in the case of bilateral VUR in symptomatic patients.
Patients with secondary VUR or VUR occurring in the setting of other congenital or acquired anomalies of the urinary tract were also included in the study (eg, isolated bladder diverticula, duplex kidney, ureterocele, posterior urethral valves, solitary kidney, or neurogenic bladder). Patients were excluded from the study if they lacked exhaustive clinical and radiological follow-up.
Endoscopic Techniques
All the procedures were performed under general anesthesia. The patient was placed in a lithotomy position and an intravenous dose of antibiotic was administered. Cystoscopy was performed with a pediatric operative cystoscope (Storz 9.5 Fr) equipped with an offset lens to allow direct passage of the 3.7 Fr needle in line with the ureter. The bladder was filled with less than half of its capacity to allow the visualization of the ureteral orifices.
The endoscopic technique (ie, “combined STING-HIT”, STING, HIT) was chosen according to the surgeon’s preference and experience. Nevertheless, the “combined STING-HIT” technique was preferred in the case of wide-open ureteral meatus with a short intramural ureteral portion.
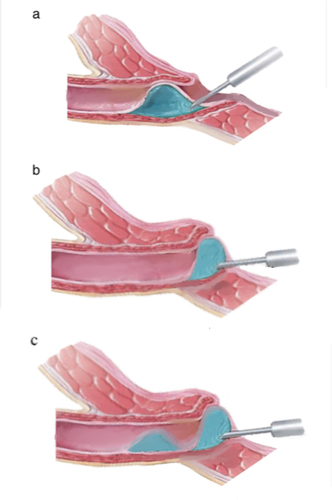
When the “combined STING-HIT” technique was adopted, the lumen of the distal ureter was distended by hydrostatic pressure achieved by placing the irrigation bag 1 meter above the bladder on full flow. The bulking agent was injected, at the 6 o’clock position, 5 mm into the submucosa of the intramural ureteral portion till it reached a coapt in the ureteral tunnel. Then, a subureteral implantation was performed to obtain a “volcano” aspect at the ureteral orifice, as shown in . The STING and the HIT techniques were performed as previously described, as per their original technique.Citation23
Postoperative Evaluation
Patients underwent an ultrasound scan (US) of the urinary tract 4 weeks after injection of the bulking agent to assess the status of the associated hydroureteronephrosis and exclude indirect signs of obstruction. A voiding cystourethrogram (VCGU) was performed at the 3-month follow-up and, in the case of VUR resolution, the continuous antibiotic prophylaxis regimen was discontinued. Treatment was considered successful in the case of symptom remission and VUR resolution on the postoperative VCUG. Renal and bladder ultrasonography were also repeated at the 6, 12, and 24-month follow-ups to confirm the regression of the associated hydroureteronephrosis.
Statistical Analysis
Descriptive statistics were presented as medians with first and third quartiles (1st–3rd) for quantitative variables and as absolute frequencies and percentages for qualitative variables. The Shapiro–Wilk test was used to assess the normality of the distribution of quantitative variables. The Kruskal–Wallis test was employed to compare quantitative variables across the three patient groups. If a statistically significant difference was found, the Mann–Whitney U-test was used to compare quantitative variables between two patient groups when data were skewed or limited. For frequency comparisons, the Chi-square test or Fisher’s Exact test was applied if the expected frequencies were less than 5. The statistical analysis was conducted using Stata 16 (Stata, College Station, Texas, USA).
Results
Patient Characteristics
In the study period, a total of 140 patients and 228 ureters underwent the endoscopic treatment of VUR at a median patient age of 3 (2.0–6.0) years. The female-to-male ratio was 0.8.
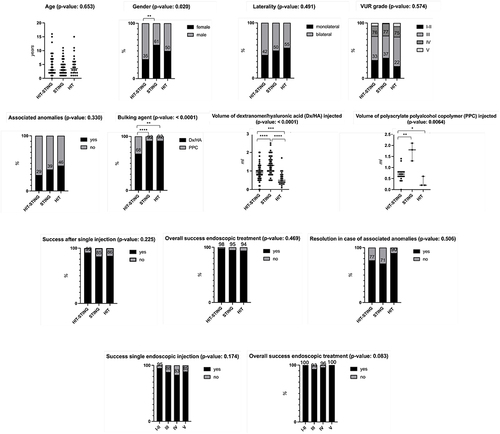
As shown in , 74 patients (F:M = 26:48) and 119 (52%) refluent ureterovesical junctions were approached using the “combined STING-HIT” technique: 6 (5%) grade V, 23 (19%) grade IV, 51 (43%) grade III, 39 (33%) grade I–II. The VUR was unilateral in 31 (42%) and bilateral in 43 (58%) patients. In 52 (71%) patients, the VUR was primary while in the remaining 22 (29%) it was secondary or associated with congenital or acquired abnormalities of the urinary tract (posterior urethral valves: n = 3; duplex kidney: n = 8; isolated bladder diverticula n = 2; solitary kidney: n = 4; neurogenic bladder: n = 4; ectopic kidney: n = 1). The bulking agent adopted was the dextranomer/hyaluronic acid (Dx/HA) in 81 (68%) ureters, while in the remaining 38 (32%) ureters the polyacrylate-polyalcohol copolymer (PPC) was preferred. The median volume of the Dx/HA injected was 0.9 (0.6–1.1) mL while the median volume of the PPC injected was 0.7 (0.6–0.8) mL.
Table 1 Baseline Characteristics of the Cohort of Patients Included in the Study
Forty-four patients (F:M = 27:17) and 73 (32%) refluent ureterovesical junctions were approached using the STING technique: 1 (1%) grade V, 16 (21%) grade IV, 29 (40%) grade III, 27 (37%) grade I–II. The VUR was unilateral in 22 (50%) and bilateral in the remaining 22 (50%) patients. In 27 (61%) patients the VUR was primary while in the remaining 17 (39%) it was secondary or associated with congenital or acquired abnormalities of the urinary tract (posterior urethral valves: n = 3; duplex kidney: n = 7; isolated bladder diverticula n = 3; neurogenic bladder: n = 2; ectopic kidney: n = 2). The bulking agent adopted was the Dx/HA in 67 (92%) ureters, while in the remaining 6 (8%) ureters the PPC was preferred. The median volume of the Dx/HA injected was 1.3 (1.0–1.6) mL while the median volume of the PPC injected was 1.8 (1.6–2.0) mL.
Twenty-two patients (F:M =11:11) and 36 (16%) refluent ureterovesical junctions were approached using HIT technique: 2 (6%) grade V, 7 (19%) grade IV, 19 (53%) grade III, 8 (22%) grade I–II. The VUR was unilateral in 12 (55%) and bilateral in the remaining 10 (45%) patients. In 12 (55%) patients the VUR was primary while in the remaining 10 (45%) it was secondary or associated with congenital or acquired abnormalities of the urinary tract (posterior urethral valves: n = 2; duplex kidney: n = 3; neurogenic bladder: n = 2; ectopic kidney: n = 2; epispadias: n = 1). The bulking agent adopted was the Dx/HA in 33 (92%) ureters, while in the remaining 3 (8%) ureters the PPC was preferred. The median volume of the Dx/HA injected was 0.5 (0.4–0.8) mL while the median volume of the PPC injected was 0.2 (0.2–0.4) mL.
No significant differences were found between the 3 groups of patients in terms of gender, age at treatment, and VUR grade or VUR secondary or associated with other anomalies of the urinary tract.
Outcomes
After a single injection of the bulking agent, VUR resolved clinically and radiologically in 203 (88%) ureters. The VUR resolution rate after a single endoscopic treatment was 95% (n=70/74) in case of grade I–II VUR, 88% (n=87/99) in case of grade III VUR; 83% (n=38/46) in case of grade IV VUR; 89% (n=8/9) in case of grade V VUR (p-value: 0.174).
Overall, one or two endoscopic treatments succeeded in 219 (96%) ureters. The overall VUR resolution rate following one or two endoscopic treatments was 100% (74/74) in case of grade I–II VUR, 93% (n=92/99) in case of grade III VUR; 96% (n=44/46) in case of grade IV VUR; 100% (n=9/9) in case of grade V VUR (p-value: 0.083).
As shown in and , the overall resolution rate after a single endoscopic injection of bulking agent was higher for the “combined STING-HIT” technique as compared to the STING or HIT technique alone (92% vs 85% vs 86%; p-value: 0.225). Similar results were reported after one or two endoscopic treatments. In this case, the “combined STING-HIT” technique showed a successful rate of 98% compared to the 95% of the STING technique and the 94% of the HIT technique (p-value: 0.469).
Table 2 Surgical Outcomes Comparing the 3 Different Endoscopic Techniques
Figure 2 Baseline characteristics of the cohort of patients included in the study (upper rows) and surgical outcomes comparing the 3 different endoscopic techniques (lower rows).
No complications were reported intra- or post-operatively. In the group of children undergoing the STING procedure, a single patient complained of flank pain, and a worsening hydroureteronephrosis was shown a few days after the procedure. A double-J stent was placed in situ and the associated hydroureteronephrosis resolved at the urinary ultrasound scan performed at the 4-weeks of follow-up.
Discussion
Since its first introduction in 1981,Citation12 the endoscopic treatment for VUR in children has increasingly widespread. To date, many reports have been published reporting highly divergent success rates, varying from 68 to 82%.Citation24–26 These results mainly depend on the bulking agent adopted,Citation27 the injection technique employed,Citation13,Citation15 and several other predictive factors, including VUR grade at presentation, surgeon’s experience,Citation28 patient gender, and endoscopic appearance of the mound.Citation13 In terms of surgical expertise, research has demonstrated that prior training significantly impacts the procedural outcomes of endoscopic treatment for VUR within pediatric urology fellowship programs. It has been noted that less experienced pediatric urology fellows may encounter higher failure rates when initially performing VUR dilation procedures.Citation28 Regarding the surgical technique employed, two main endoscopic approaches have been popularized so far, including the STING and HIT techniques. Since 2010, in our pediatric tertiary referral center, a new technique has been developed and increasingly adopted: the “combined STING-HIT technique”. Further modifications now include the use of proximal and distal intraluminal injections (ie, the double HIT technique) that result in coaptation of both the ureteral tunnel and orifice.Citation19–21 In this study, we retrospectively reviewed our data and compared the safety and efficacy of the “combined STING-HIT technique” with the standard endoscopic treatments of VUR in children, including the STING and the HIT techniques.
Our results showed that the “combined STING-HIT” technique was associated with a resolution rate of 98% of cases (ie, 100 in case of grade V VUR, 96% in case of grade IV VUR, 96% in case of grade III VUR; 100% in case of grade I–II VUR), replicating and improving the success rate described with the HIT technique by Kirsch et al.Citation14 Worth noting that 24% of patients in our study suffered from high-grade (IV–V) VUR compared to 9% in the study performed by Kirsch et al.Citation14
On the other hand, our experience with the STING technique was similar to what was described in the existing studies,Citation13 with a success rate of 85% of cases after a single endoscopic injection and 95% of cases after one or two endoscopic treatments. Similarly to what was described by Routh et al,Citation29 we also noted a high-resolution rate by adopting the HIT technique. This is particularly interesting if we consider that the best results in literature were described when almost an intra-ureteral injection was performed.
Based on the above, the higher success of the “combined STING-HIT” procedure after a single (92% of cases) or two (98% of cases) administrations could be explained by considering that the intra-ureteric injection guaranteed a strong and stable anti-reflux mechanism and the sub-ureteral injection permitted to coapt of the orifice at low vesical pressure.
The population of patients in our study included children with primary VUR and children with secondary VUR or VUR associated with other anatomical or functional anomalies of the urinary tract. VUR is the most common anomaly associated with duplex kidneys and, in 90% of cases, it involves the lower pelvicalyceal pole.Citation30 Previous studies on VUR in complex duplex systems showed a resolution rate success of 63%, significantly lower than the resolution rates reported after endoscopic correction in the overall population of children with VUR.Citation31 Ureteral reimplantation was for years the gold standard for the approach to complex VUR after incision or puncture of ureterocele and in the case of para-ureteral diverticula. However, in 2007 Chertin et alCitation32 reported the results of endoscopic treatment of VUR cases, including 33 patients with ureterocele. Cherwinka et alCitation33 presented Atlanta’s experience with the endoscopic treatment of VUR associated with para-ureteral bladder diverticula. Bladder dysfunction is associated with VURCitation34 and has been reported to be more frequently bilateral.Citation35 We included patients with neurogenic bladder despite this diagnosis correlated with treatment failure in the prior series.Citation36 The reason for treatment failure seemed to be the implant displacement due to uninhibited detrusor contraction in voiding dysfunction.Citation37
Proving the high success rate of the endoscopic treatment also in the case of secondary VUR or VUR associated with other anatomical or functional anomalies of the urinary tract, our data, even if limited, showed that these approaches can be proposed as a first-line treatment also in this high-risk group of patients to avoid open surgery. The association of a high volume of bulking agent injection, adequate pharmacotherapy, and micturition rehabilitation seemed to be the key to reducing the failure rate and guaranteeing this high success rate.
The main limits of our study include its retrospective and non-randomization nature, particularly the possibility of confounding bias due to unidentified factors. A prospective and randomized trial of endoscopic injection techniques would have strengthened the significance of our findings and the predictive power of our outcome variables.
Conclusion
The endoscopic approaches proved highly effective in treating symptomatic VUR in children, significantly reducing the necessity for open surgery in most cases. However, lower success rates were observed in cases of higher VUR grades or when VUR was secondary or associated with other urinary anomalies. The “combined STING-HIT” technique emerged as a safe and efficient procedure, consistently achieving higher resolution rates whether administered in a single or dual bulking agent injection.
Ethical Approval
All procedures performed in the study involving human participants were under the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. According to our Institution’s regulations (ie, Department of Pediatric Surgery, Buzzi Children’s Hospital, 20154 Milan, Italy), the need for ethics approval for this non-interventional study’s retrospectively obtained and anonymized data were waived. The reservedness of the collected information was ensured according to Regulation (EU)/2016/679 GDPR (Regulation (EU) 2016/679), Legislative Decree n.101/18. Full informed consent was obtained from the study participants’ guardians.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
We want to thank the Foundation Romeo and Enrica Invernizzi for supporting this project. Moreover, we would like to acknowledge the support of the APC central fund of the University of Milano.
References
- Elder JS, Peters CA, Arant BS, et al. Pediatric vesicoureteral reflux guidelines panel summary report on the management of primary vesicoureteral reflux in children. J Urol. 1997;157(5):1846–1851. doi:10.1016/S0022-5347(01)64882-1
- Zhang T, Wiygul J. Correlation not causation - looking back at the history of VUR. Urology. 2024;S009042952400445X. doi:10.1016/j.urology.2024.06.002
- Boswell TC, Maric T, Khoury AE, Farrugia MK. Urinary tract dilatation and vesicoureteral reflux - Adult outcomes, who should be followed, and how to follow them. J Pediatric Urology. 2023;19(4):450–455. doi:10.1016/j.jpurol.2023.04.038
- Nordenström J, Sjöström S, Dellenmark-Blom M. Parents’ experiences of treatment and outcomes in high-grade vesicoureteral reflux in infants – one piece in the puzzle of VUR management? J Pediatric Urology. 2024;S1477513124002845. doi:10.1016/j.jpurol.2024.05.020
- Kutasy B, Coyle D. History of endoscopic treatment of vesicoureteral reflux. Pediatr Surg Int. 2023;39(1):187. doi:10.1007/s00383-023-05468-0
- Escolino M, Kalfa N, Castagnetti M, et al. Endoscopic injection of bulking agents in pediatric vesicoureteral reflux: a narrative review of the literature. Pediatr Surg Int. 2023;39(1):133. doi:10.1007/s00383-023-05426-w
- Chang CL, Yang SSD, Hsu CK, Chen CH, Chang SJ. Effectiveness of various treatment modalities in children with vesicoureteral reflux grades II–IV: a systematic review and network meta-analysis. BMJPO. 2023;7(1):e002096. doi:10.1136/bmjpo-2023-002096
- Fanos V, Cataldi L. Antibiotics or surgery for vesicoureteric reflux in children. Lancet. 2004;364(9446):1720–1722. doi:10.1016/S0140-6736(04)17359-5
- Kim SW, Lee YS, Han SW. Endoscopic injection therapy. Investig Clin Urol. 2017;58(Suppl 1):S38. doi:10.4111/icu.2017.58.S1.S38
- Hajiyev P, Burgu B. Contemporary management of vesicoureteral reflux. European Urology Focus. 2017;3(2–3):181–188. doi:10.1016/j.euf.2017.08.012
- Zvizdic Z, Catic A, Zivojevic S, Jonuzi A, Glamoclija U, Vranic S. The correlation between ureteric orifice morphology and primary vesicoureteral reflux grade and the impact on the effectiveness of endoscopic reflux correction. J Pediatric Urology. 2024;20(2):295–301. doi:10.1016/j.jpurol.2023.10.027
- Matouschek E. Treatment of vesicorenal reflux by transurethral teflon-injection (author’s transl). Urologe A. 1981;20(5):263–264.
- O’Donnell B, Puri P. Treatment of vesicoureteric reflux by endoscopic injection of Teflon. BMJ. 1984;289(6436):7–9. doi:10.1136/bmj.289.6436.7
- Kirsch AJ, Perez-Brayfield M, Smith EA, Scherz HC. The modified sting procedure to correct vesicoureteral reflux: improved results with submucosal implantation within the intramural ureter. J Urol. 2004;171(6 Part 1):2413–2416. doi:10.1097/01.ju.0000127754.79866.7f
- Capozza N, Caione P. Modification of the sting procedure for vesicoureteral reflux: ureteral repositioning and injection. Arch Esp Urol. 2008;61(2). doi:10.4321/S0004-06142008000200021
- Garcia-Aparicio L, Martin-Sole O, Capdevila-Vilaro B, Perez-Bertolez S. Long-term outcome of randomized clinical trial between polyacrylate-polyalcohol copolymer (PPC) and dextranomer-hyaluronic acid copolymer (Dx/HA) as bulking agents for endoscopic treatment of primary vesicoureteral reflux (VUR). World J Urol. 2023;41(10):2855–2859. doi:10.1007/s00345-023-04548-z
- Pensabene M, Cimador M, Spataro B, et al. Intraoperative ultrasound-assisted endoscopic treatment of primary intermediate and high-grade vesicoureteral reflux in children in a long-term follow-up. J Pediatric Urology. 2024;20(1):132.e1–132.e11. doi:10.1016/j.jpurol.2023.10.008
- Renaux-Petel M, Grynberg L, Lubet A, Comte D, Liard-Zmuda A. Vantris vs. deflux for treatment of paediatric vesicoureteral reflux: efficacy and obstruction risk. French J Urology. 2024;34(2):102585. doi:10.1016/j.fjurol.2024.102585
- Arceo-Olaiz RA, Scherz HC, Kirsch AJ. Endoscopic treatment of VUR. Urology Video J. 2022;15:100163. doi:10.1016/j.urolvj.2022.100163
- Cerwinka WH, Scherz HC, Kirsch AJ. Dynamic hydrodistention classification of the ureter and the double HIT method to correct vesicoureteral reflux. Arch Esp Urol. 2008;61(8). doi:10.4321/S0004-06142008000800005
- Kirsch AJ, Arlen AM. Evaluation of new Deflux administration techniques: intraureteric HIT and Double HIT for the endoscopic correction of vesicoureteral reflux. Expert Rev Med Dev. 2014;11(5):439–446. doi:10.1586/17434440.2014.929491
- Report of the International Reflux Study Committee. Medical versus surgical treatment of primary vesicoureteral reflux: Report of the international reflux study committee. Pediatrics. 1981;67(3):392–400. doi:10.1542/peds.67.3.392
- Yap TL, Chen Y, Nah SA, Ong CCP, Jacobsen A, Low Y. STING versus HIT technique of endoscopic treatment for vesicoureteral reflux: a systematic review and meta-analysis. J Pediatric Surg. 2016;51(12):2015–2020. doi:10.1016/j.jpedsurg.2016.09.028
- Läckgren G, Wåhlin N, Sköldenberg E, Stenberg A. Long-term followup of children treated with dextranomer/hyaluronic acid copolymer for vesicoureteral reflux. J Urol. 2001;166(5):1887–1892. doi:10.1016/s0022-5347(05)65713-8
- Chertin B, Caluwé D D, Puri P. Endoscopic treatment of primary grades iv and v vesicoureteral reflux in children with subureteral injection of Polytetrafluoroethylene. J Urol. 2003;169(5):1847–1849. doi:10.1097/01.ju.0000062300.71507.3a
- Puri P, Ninan GK, Surana R. Subureteric Teflon Injection(STING). Eur Urol. 1995;27(1):71–75. doi:10.1159/000475128
- Stenberg A, Lackgren G. A new bioimplant for the endoscopic treatment of vesicoureteral reflux: experimental and short-term clinical results. J Urol. 1995;154:800–803. doi:10.1097/00005392-199508000-00127
- Selvi I, Canbaz FA, Dönmez Mİ, et al. Does pre-fellowship experience alter success rates of endoscopic treatment of vesicoureteral reflux during pediatric urology fellowship? J Pediatric Urology. 2022;18(4):527.e1–527.e8. doi:10.1016/j.jpurol.2022.06.001
- Routh JC, Reinberg Y, Ashley RA, et al. Multivariate comparison of the efficacy of intraureteral versus subtrigonal techniques of dextranomer/hyaluronic acid injection. J Urol. 2007;178(4S):1702–1706. doi:10.1016/j.juro.2007.03.174
- Thomas JC. Vesicoureteral Reflux and Duplex Systems. Adv Urology. 2008;2008:1–3. doi:10.1155/2008/651891
- Läckgren G, Wåhlin N, Sköldenberg E, Nevéus T, Stenberg A. Endoscopic treatment of vesicoureteral reflux with dextranomer/hyaluronic acid copolymer is effective in either double ureters or a small kidney. J Urol. 2003;170(4 Part 2):1551–1555. doi:10.1097/01.ju.0000084672.98131.f7
- Chertin B, Mohanan N, Farkas A, Puri P. Endoscopic treatment of vesicoureteral reflux associated with ureterocele. J Urol. 2007;178(4S):1594–1597. doi:10.1016/j.juro.2007.03.170
- Cerwinka WH, Scherz HC, Kirsch AJ. Endoscopic treatment of vesicoureteral reflux associated with paraureteral diverticula in children. J Urol. 2007;178(4):1469–1473. doi:10.1016/j.juro.2007.05.168
- Sillén U. Bladder dysfunction in children with vesico-ureteric reflux. Acta Paediatr Suppl. 1999;88(431):40–47. doi:10.1111/j.1651-2227.1999.tb01317.x
- Soygür T, Arikan N, Yesillii Ç, Göğüş O. Relationship among pediatric voiding dysfunction and vesicoureteral reflux and renal scars. Urology. 1999;54(5):905–908. doi:10.1016/S0090-4295(99)00291-5
- Lavelle MT, Conlin MJ, Skoog SJ. Subureteral injection of Deflux for correction of reflux: analysis of factors predicting success. Urology. 2005;65(3):564–567. doi:10.1016/j.urology.2004.09.068
- Capozza N, Lais A, Matarazzo E, Nappo S, Patricolo M, Caione P. Influence of voiding dysfunction on the outcome of endoscopic treatment for vesicoureteral reflux. J Urol. 2002;168(4 Pt 2):1695–1698. doi:10.1016/S0022-5347(05)64391-1