Abstract
The innovation of penicillin by Dr Alexander Fleming in 1928 and its use in clinical practice saved many lives, especially during the Second World War. Tuberculosis still carries a significant public health threat and has re-emerged over the past two decades, even in modern countries where tuberculosis was thought to be eliminated. The World Health Organization defines antimicrobial resistance as the resistance of a microorganism to an antimicrobial drug that was initially effective for treatment of infections caused by the microbe. Therefore, the findings of the current study will provide data to enable the design of a new educational program to better equip our students in confronting antimicrobial resistance. This study was a cross-sectional, questionnaire-based survey, which was undertaken in the Faculty of Medicine, Universiti Sultan Zainal Abidin, Kuala Terengganu, Malaysia. The study participants were students of the Bachelor of Medicine and Bachelor of Surgery program (MBBS) of Year III, IV, and V. A total of 142 out of 164 (86%) medical students returned the questionnaire. Specifically, the year-wise breakdown of responses was 29% (41), 39% (55), and 32% (45) for Year III, IV, and V, respectively. Among the study respondents, 28% (40) were male, and the remaining 72% (102) were female. In all, 67% of the participants felt more confident in “making an accurate diagnosis of infection/sepsis.” The majority (88%) of the study participants stated that they would like more training on antibiotic selection. This research has found that there is a gap between theoretical input and clinical practice; the students are demanding more educational intervention to face the threat of antimicrobial resistance.
Video abstract
Point your SmartPhone at the code above. If you have a QR code reader the video abstract will appear. Or use:
Introduction
Selman Waksman first used the word antibiotic as a noun in 1941 to describe any small molecule made by a microbe that antagonizes the growth of other microbes.Citation1 Dr Alexander Fleming published his findings of the discovery of penicillin in the British Journal of Experimental Pathology in 1929, and by the 1940s penicillin use was commonplace in clinical practice. This saved many lives, especially during the Second World War.Citation2–Citation4 Penicillin was followed by the invention of a number of antibiotics from 1945 to 1955, namely, streptomycin, chloramphenicol, and tetracycline.Citation1,Citation4 All of these antimicrobials were produced by microbes, actinomycetes and fungi being the unique resources.Citation1,Citation4 The development of antimicrobials not only conquered the management of infectious diseases but also raised the average life expectancy and quality of life for humanity. Therefore, this outstanding achievement led to the belief that “infectious diseases would be conquered shortly.”Citation5 Although the history of clinical uses of antimicrobials is quite recent, the antibiotic tetracycline has been identified as far back as 350–550 CE among the skeletons of the ancient Sudanese Nubia population.Citation6,Citation7 Similar findings were also reported in femoral bones found in the Dakleh Oasis, Egypt.Citation8,Citation9 It has led to the notion that both of these ancient communities’ diets contained tetracycline. The presence of antimicrobials in foods in these prehistoric societies possibly gave protective effects from microbes. Therefore, these communities suffered either low or no infectious diseases.Citation6–Citation9
Tuberculosis (TB) still carries a significant public health threat and has re-emerged over the past two decades, even in modern countries where TB was thought to be eliminated.Citation10–Citation12 TB was declared a global emergency by the World Health Organization (WHO) in 1993, with around 8–10 million new cases annually and over 2–3 million deaths worldwide.Citation13 The WHO defines “AR [antimicrobial resistance] as the resistance of a microorganism to an antimicrobial drug that was initially effective for treatment of infections caused by it.”Citation14 Resistance is also defined “as bacteria that are not inhibited by usually an achievable systemic concentration of an agent with the regular dosing schedule and/or fall in the minimum inhibitory concentration ranges.”Citation15 Similarly, multiple drug resistance is defined as the acquired nonsusceptibility to three or more antimicrobial drugs or drug classes.Citation16,Citation17 The term multiple drug resistance initially was used to identify resistant malignant tumors, and later of Mycobacterium tuberculosis. Now it is used for any microbial infections – bacterium, fungus, or parasite.Citation18 Acquisition of resistance to one antibiotic conferring resistance to another antibiotic, to which the organism has not been exposed, is called cross-resistance.Citation19–Citation22 In all, 80%–90% of the antibiotics are prescribed for ambulatory patients; the rest in hospital admitted cases.Citation23 It is also reported that general practitioners prescribe 90% of antimicrobials.Citation24 It has been estimated in the US by state-sponsored research that 50 of the 150 million prescriptions for antibiotics written for outpatients every year are not evidence-based.Citation25 It has been also identified that as high as 50% of antimicrobials are used without any scientific basis, and antibiotic was prescribed that was either superfluous or debatable.Citation26–Citation28 Multiple studies reported that these very dangerous resistant microbes were created due to misuse of antimicrobials.Citation29–Citation31 The consequences are an increased risk–of additional morbidity and mortality by snowballing the possibility of adverse drug reactions and promotion of AR in community pathogens.Citation32 Researchers have pointed out that globalization ensures quick spreading of antibiotic resistance, for example, the rapid international spread of New Delhi metallo-blactamase.Citation33,Citation34 Therefore, there is an urgent need for an international and nationwide platform to control AR.Citation35–Citation39 European AR Surveillance Network, National AR Monitoring System for Enteric Bacteria (USA), The Surveillance Network (USA), AR Surveillance (Germany), Central Asian and Eastern European Surveillance on AR, and Surveillance of Antibiotic Use and Bacterial Resistance in German Intensive Care Units are the most important investigation programs currently working on AR.Citation35
Although the Ministry of Health, Malaysia, has been issuing antibiotic use guidelines for more than two decades, compliance with these guidelines was found to be lacking.Citation40 The same study also reported that antibiotic resistance is common in Malaysian general hospitals.Citation40 In 1994, another study reported that ampicillin, cloxacillin, cephalosporins, gentamicin, co-trimoxazole, and tetracyclines were highly resistant in six Malaysian general hospitals. Researchers concluded that AR is a “constant threat and challenge for clinicians” in Malaysia especially in treating nosocomial infections.Citation41 The Medical Journal of Malaysia in 2003 published three articles on the issue of AR in Malaysian communities. All three of these articles were highly concerned about AR and its impact on public health.Citation42–Citation44 Dr VKE Lim, a very renowned physician in Malaysia, in his recent editorial review of the subject, mentioned that a multifaceted strategy is required to improve antibiotic prescribing and control the emergence of antibiotic resistance. Education of both doctors and patients would form the cornerstone of the strategy.Citation45 Another three studies of research published in 2004, 2011, and 2013 reported that a significant proportion of antimicrobials were prescribed inappropriately especially in upper respiratory tract infection. These studies concluded that this irrational prescribing would promote more AR.Citation46–Citation48 These studies accept that more educational intervention will promote rational prescribing and professional responsibility, which will ultimately enlighten health professionals with more expertise against AR.Citation46–Citation48 A number studies conducted in the general public of Malaysia reported that Malaysians have inadequate knowledge about antimicrobials. These findings reinforce the notion that there is an urgent need for an educational program to raise awareness and advocate a movement among patients.Citation49–Citation51 Another study reported that a poor knowledge level exists among the general public of Malaysia, and this promotes more frequent and incorrect use of antimicrobials. The same survey also encouraged educational intervention among ordinary citizens.Citation52 Professor Lim again mentioned in his recent review that the global public threat of AR can only be addressed through good antibiotic stewardship programs. To overcome the global public health threat of AR, all relevant stakeholders of the health service should work in unison.Citation53
Rational prescribing is the paramount issue in the struggle against AR. It is tough to convey new ideas to doctors and other health professionals because they are already entrenched in their own notions and thoughts. Therefore, it is suggested that intervention should be conducted during the early days of medical training. The WHO, in 2012, has emphasized the importance of rational prescribing in the undergraduate medical curriculum.Citation54 There were different levels of awareness regarding prescribing, but almost every study recommended more educational interventions in the undergraduate curriculum.Citation55–Citation65 Different studies emphasized that teaching and learning about antimicrobials, both at the undergraduate and postgraduate medical curricula, remain the most noteworthy approach in the fight against AR.Citation55,Citation66–Citation68 Antimicrobials are “considered among the essential drugs of a core curriculum in clinical pharmacology for undergraduate medical students.”Citation69
Although there are some related studies conducted throughout the world, there were not many studies specific to Malaysia. One pilot study published in 2014 suggested extensive improvement of the curriculum and education for health care professionals to ensure the rational use of antimicrobials.Citation70 The first batch of medical students admitted at Universiti Sultan Zainal Abidin (UniSZA) was in 2009, graduated in 2014, to work as house officers in different hospitals for the Ministry of Health, Malaysia.Citation71 As other universities in Malaysia, UniSZA is subscribed to the integrated curriculum for undergraduate medical education and pharmacology is taught in preclinical years of Year I and II as a lecture-based subject.Citation72 The Faculty of Medicine, UniSZA, is scheduled to conduct a major revision in the next few years of the undergraduate medical curriculum.Citation73,Citation74 Therefore, this exercise is to ensure highly professional and committed medical doctors are produced in society.Citation75–Citation78 Medical students are future doctors for any society, and they are the primary stakeholders in any health care system.Citation60 Therefore, their beliefs and practices regarding antibiotic prescribing and resistance will have an impact on AR. The current study will provide suitable data to design a new educational program to equip our students in their fight against AR. UniSZA is a new medical school in Malaysia and the first two batches have already graduated and are working as house officers in different government tertiary hospitals of Malaysia. It is mandatory for the faculty of medicine to reorganize and review the curriculum according to the Malaysian Government regulation.Citation73,Citation74
Materials and methods
This study was a cross-sectional, questionnaire-based survey, which was undertaken in the Faculty of Medicine, UniSZA, Malaysia. The study participants were students of the MBBS program in Year III, IV, and V. As the total population size was 179, a universal sampling method was applied to select the respondents. Data were collected from May to June 2015 using a validated instrument. The principal author was much impressed with a multicenter study conducted in Europe.Citation65 He contacted the corresponding author Professor (Dr) Céline Pulcini in France and obtained formal permission to use the validated instrument. The questionnaire was again pretested and validated in the local context. The questionnaire was administered to 15 medical students who did not participate in the primary study. Their responses were collected and analyzed for validity and reliability. The Cronbach alpha was calculated as 0.69. A total of 164 (179-15 non-participants) questionnaires were given to the study respondents after a prearranged lecture class. They were asked to complete anonymously the questionnaires. Study respondents were given 15 minutes to complete the questionnaire which was handed over immediately to the principal investigator.
The questionnaire consisted of 21 questions. Initially, demographic features were recorded. The first question was a 5-point Likert scale, where responses ranged from “very unconfident” to “uncertain”. It was used to assess the respondent’s confidence in prescribing. Six questions were set to give an idea of the student’s training in antibiotic prescribing. Out of six, five questions were arranged in the Likert scale-based questions with options of “yes”, “no”, and “unsure”. One question was to assess the total hours of training the respondents had received during their undergraduate study. Then, the next five questions were set to evaluate the respondent’s knowledge of AR. Two of these were set out so as to put a tick mark for “yes”, “no”, or “unsure”. The other three questions were arranged in six rows, which indicated the percentage range in the following manner: row 1 was up to 1%, row 2 was >1%–20%, row 3 for 21%–40%, row 4 for 41%–60%, row 5 included 61%–80%, and the last row showed a percentage range from 81% to 100%. The self-reported practices regarding the antibiotic usage of the study population were also assessed by using two questions that consisted of five rows. Each row showed the percentage range in the answer. Ranges of percentage were 1%–20% in the first row, 21%–40% in the second, 41%–60% in the third, 61%–80% in the fourth, and finally 81%–100% in the fifth. The respondent’s perception of the factors contributing to antibiotic resistance was assessed by another question that consisted of a 4-point Likert scale, whose responses ranged from “very important” to “not important at all”. The next two knowledge-based questions were about the number of new classes of antibiotics that became clinically available in the last 30 years as well as those that will become available in the next 30 years. The last three questions were used to assess the respondent’s perceptions of AR.
There are four routes available to students to pursue a degree program in Malaysia. The Ministry of Education conducts two qualifying programs to the first degree programs: the first program allows students to matriculate at secondary school. This program is usually a 1-year program, but may extend up to 2 years if necessary. The majority of UniSZA students have completed the 1-year matriculation program. The second route is the Malaysia Certificate of Higher Education, which is a 1.5-year program. Also, a 1-year foundation training is conducted by top Malaysian universities. Finally, students can opt to complete a diploma after secondary school, and later apply for entry into a degree program.Citation71
This research obtained UniSZA Research Ethics Committee (UHREC) ethical approval; the certificate was obtained (UniSZA. C/1/UHREC/628-1 [4], March 5, 2015) before the study was conducted. Research ethics were strictly maintained, especially regarding confidentiality. Explanation concerning the purpose of the study was given, and informed consent was obtained verbally from the participants to utilize their data for research purposes. UHREC had examined the questionnaire before the study was started. UHREC was satisfied that there were no sensitive questions. The current research was a questionnaire-based knowledge, attitude, and practice study, which was totally anonymous and voluntary. Thus, researchers thought verbal consent was sufficient. The principal investigator informed UHREC and took permission for the verbal consent procedures before data collection began. This study recovered 86% of the questionnaires as respondents were given total liberty to refuse the study. Simple descriptive statistics were used to generate frequencies and percentages using SPSS Version 20 (IBM Corporation, Armonk, NY, USA).
Results
Demographic profile
A total of 142 out of 164 (86%) medical students returned the questionnaire. Specifically, the year-wise response was 29% (41), 39% (55), and 32% (45) for Year III, IV, and V, respectively. Among the study respondents, 28% (40) were male, and the remaining 72% (102) were female. The majority (92%, 131) of the respondents were single, but the rest were either engaged (5%, 7) or married (2%, 3). Similarly, the majority of the current study population were Malay (82%, 116) and the rest were either Indian (10%, 14) or Chinese (7%, 10) in ethnic origin. The study population had different religious backgrounds; 84% (119) identified as Muslim, Hindu (8%, 11), Buddhist (6%, 8), and Christian (1%, 2). In all, 78% (111) of the present study population have undergone a 1-year matriculation and the rest either a 2-year matriculation (1%, 2) or other (17%, 24) ().
Table 1 Demography of study population (n=142)
Levels of confidence in prescribing
The participants felt more confident in “making an accurate diagnosis of infection/sepsis” (67%, 95), “interpreting microbiological results” (55%, 78), “choosing the correct antibiotic” (55%, 78), “choosing the correct dose and interval of administration” (42%, 52), “using a combination therapy if appropriate” (44%, 63), “choosing between intravenous and oral administration” (56%, 79), “deciding not to prescribe an antibiotic if the patient has fever, but no severity criteria, and if you are not sure about your diagnosis” (56%, 79), “planning to streamline/stop the antibiotic treatment according to the clinical evaluation and investigations” (51%, 72), and “planning the duration of the antibiotic treatment” (49%, 69). The respondents felt unconfident in “interpreting microbiological results” (25%, 36), “choosing the correct antibiotic” (30%, 42), “choosing the correct dose and interval of administration” (42%, 60), “using a combination therapy if appropriate” (40%, 57), “deciding not to prescribe an antibiotic if the patient has fever, but no severity criteria, and if you are not sure about your diagnosis” (26%, 37), “planning to streamline/stop the antibiotic treatment according to the clinical evaluation and investigations” (31%, 44), and “planning the duration of the antibiotic treatment” (35%, 49). The detailed results are shown in . There were no significant differences (P>0.05) observed in any of parameters of confidence of antibiotic prescribing between year and the sex of the respondents ( and ).
Table 2 Levels of confidence in different areas of antibiotic prescribing (n=142)
Table 3 Comparison among Year III, IV, and V in levels of confidence of antibiotic prescribing
Table 4 Comparison between sexes in levels of confidence of antibiotic prescribing
Training in antibiotic prescribing
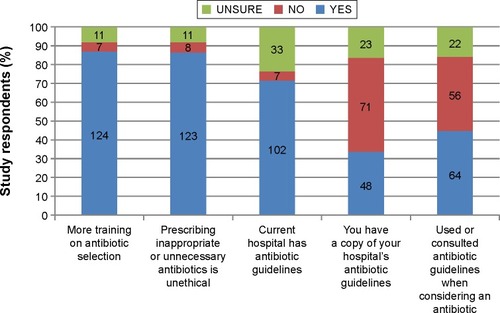
The majority (88%, 124) of the study participants stated that they would like more training in the antibiotic selection, seven students (5%) did not want further education, and another eleven students (8%) were unsure. Most of the respondents (87%, 123) felt prescribing inappropriate or unnecessary antibiotics to be professionally unethical. In all, 72% (102) of the respondents were confident that their current teaching Hospital Sultanah Nur Zahirah (HSNZ) has antibiotic guidelines, but 23% (33) students were unaware, and 5% (7) students indicated that there are no antibiotic guidelines for HSNZ. In all, 50% (71) of the respondents do not possess a copy of HSNZ antibiotic guidelines or found it on the internet while 34% (48) of students said they received a copy and 16% (23) students were unsure about it. Personally consulting antibiotic guidelines when considering an antibiotic for a patient was only practiced by 45% (64) students, and the rest, 39% (56) and 16% (22) students, were either not practiced or unsure (). There were statistically (P=0.018) significant differences observed among Year of Study of the respondents regarding the question “How many hours of training in the principles of prudent antibiotic use do you think you have received during your undergraduate study?”
Knowledge that may shape perceptions of AR
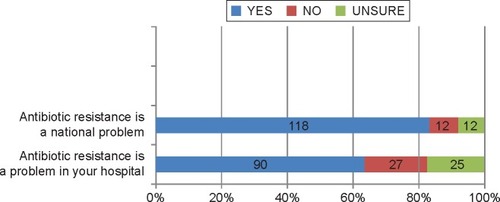
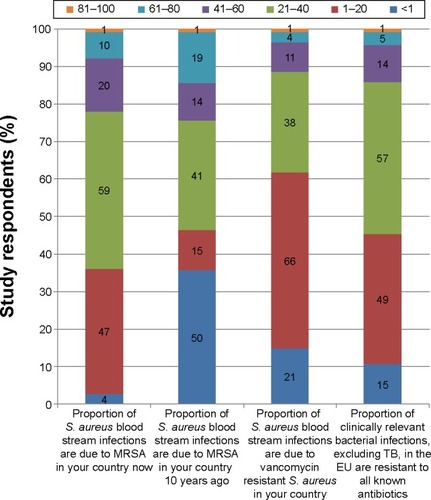
Most students (83%, 118) felt that antibiotic resistance was a national problem, and 63% (90) felt that the situation also exists in the teaching hospital (). In all, 42% (59) of respondents stated that methicillin-resistant Staphylococcus aureus was responsible for a greater proportion (21%–40%) of S. aureus bacteremia in Malaysia, while 35% (50) respondents stated that it was <1% 10 years ago. In all, 49% (65) respondents thought that over 1%–20% of S. aureus bacteremias were caused by vancomycin-resistant bacteria in Malaysia, and 40% (57) respondents believed that over 21%–40% of all bacterial infections in Malaysia (excluding TB) were resistant to all known antibiotics (). There were no significant differences (P>0.05) observed in any of parameters regarding knowledge that may shape the perception of AR between year and sex of the respondents.
Antibiotic usage
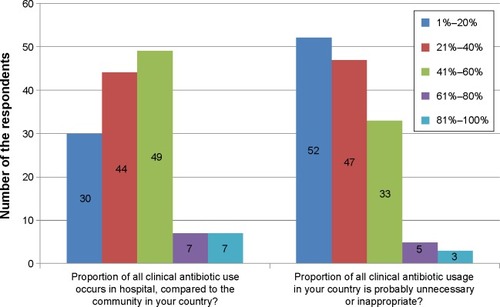
About 35% (49) of the respondents felt that the proportion of all clinical antibiotic use in a hospital in Malaysia comprised of 41%–60% of cases when compared to the community. In all, 37% (52) of the respondents agreed that the clinical antibiotic usage in this country is probably unnecessary or inappropriate by 1%–20% ().
Contributors to resistance
The majority of the respondents agreed that “too many antibiotic prescriptions” (55%, 78), “too many broad spectrum antibiotics used” (50%, 71), and “excessive use of antibiotics in livestock” (43%, 61) were leading contributors to AR (). Another group felt that “too long durations of antibiotic treatment” (42%, 59), “dosing of antibiotics are too low” (36%, 51), “poor hand hygiene” (27%, 38), “not removing the focus of infection” (41%, 58), and “paying too much attention to pharmaceutical representatives/advertising” (37%, 53) were moderately important factors contributing to AR (). The rest of the study participants gave the opinion for slightly important and not important contributors to generate AR (). There were no significant differences (P>0.05) observed in any of parameters of confidence of antibiotic prescribing between years and the sex of the respondents ( and ).
Table 5 Perceptions of the importance of potential contributors to antibiotic resistance (n=142)
Table 6 Comparison among Year III, IV, and V in levels of contributors to resistance
Table 7 Comparison between sexes on their view regarding contributors to resistance
Development of antibiotics
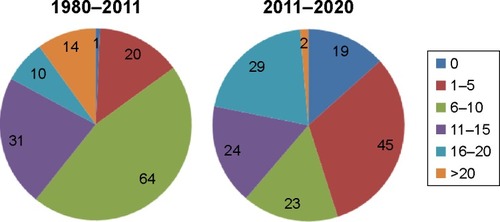
In all, 44% (63) of the respondents believed that six to ten antibiotic classes were available during the period 1980–2011, and 23% (45) of students thought that there would be six to ten new antibiotic classes in 2011–2020 ().
Perceptions of AR
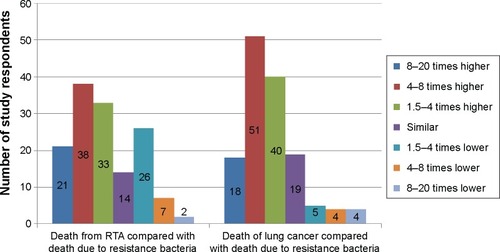
Resistant bacteria are believed to cause 25,000 deaths per year in Europe.Citation79 Road traffic accidents (RTAs) and lung cancer are responsible for around two to three and ten times as many deaths, respectively.Citation80 Overall, 27% (38) and 36% (51) of research participants think that deaths due to AR were four to eight times higher than RTA and lung cancer, respectively (). In all, 23% (33) medical students in the study were able to answer correctly for estimation of RTAs while 36% (51) answered correctly the reasonable estimate for comparison between deaths due to lung cancer and AR. Most of the respondents (45%, 65) felt that the antibiotics they would prescribe as doctors would likely contribute to the problem of AR later, and 42% (60) students believed that antibiotic resistance would become a possible clinical problem during their career.
Discussion
Demographic profile
The response rate of the students for the current study was 86%, which is very similar to that of a Danish recommendation.Citation81 Universal sampling was adopted because of small population size (179) and 15 of them participated in the pilot study. Consequently, 164 was the total population to whom the questionnaire was distributed; among them, 142 (86%) returned and 22 did not participate in the study. The study respondents are able to enjoy complete freedom to participate or not. Hence, it is hard to answer why they did not return the questionnaire. Furthermore, a total of 157 (15+142) joined the current work. So, actually among 179 clinical students of UniSZA, 88% participated in this cross-sectional research. In this study, there were more female medical students than male colleagues; this finding is analogous to that in many other studies.Citation75–Citation78,Citation82–Citation84
Levels of confidence in prescribing
The participants felt more confident in “making an accurate diagnosis of infection/sepsis” (67%), “interpreting microbiological results” (55%), “choosing the correct antibiotic” (55%), “choosing the correct dose and interval of administration” (42%), “using a combination therapy if appropriate” (44%), “choosing between intravenous and oral administration” (56%), “deciding not to prescribe an antibiotic if the patient has fever, but no severity criteria, and if you are not sure about your diagnosis” (56%), “planning to streamline/stop the antibiotic treatment according to the clinical evaluation and investigations” (51%), and “planning the duration of the antibiotic treatment” (49%). Overall, 50% or more of current study participants were confident of six of nine issues of the level of confidence in prescribing. Current study findings regarding knowledge level of antibiotic prescribing and resistance were not satisfactory, but research participants were medical students of Years III–V. Again, at UniSZA, from year III, students are first exposed to the hospital and patients. As in first 2 years, they go to preclinical subjects with only little early clinical exposure. Therefore, study participants have at least 3 months to 2 years and 3 months extra time to learn more regarding antibiotic prescribing in their clinical years. Moreover, after graduation, according to Malaysian regulations, they will be working as a house officer for another 2 years under strict supervision. Consequently, there is time for improvement. Our study findings were lower than some European studies and Bangladeshi studies conducted on interns or house officers.Citation65,Citation85–Citation87 But regarding “using a combination therapy if appropriate,” our respondents obtain an almost similar score to the studies, although our participants were medical students and those were trainee doctors.Citation85,Citation87
Training in antibiotic prescribing
The majority (88%) of the respondents stated that they would like more training on antibiotic selection. Most of the respondents (87%) felt prescribing antibiotics irrationally was unethical. About 72% of study respondents were sure that HSNZ had antibiotic guidelines, but 50% of them did not possess a copy of the guide, and only 45% had consulted the antibiotic guidelines (). Study findings showed that the respondents have realized there is a gap between their theoretical lecture-based input,Citation72 regarding antimicrobials, and clinical practice. Similar studies from different countries also indicated demand for more educational intervention.Citation55–Citation65,Citation70,Citation87 The total antimicrobials class hours at the faculty of medicine is 7 hours during the first 2 years of the preclinical stage. All are lecture-based teaching hours. UniSZA’s medical curriculum does not currently possess any class for teaching antimicrobial selection. Therefore, students when started clinical clerking they comprehend that there is an urgent need for training of drug, including antimicrobial selection procedure.
Knowledge that may shape perceptions of AR
Most students (83%) felt that antibiotic resistance is a national problem, and 63% felt that the situation also exists in HSNZ (). In all, 42% of our medical students stated that 21%–40% S. aureus infections were due to methicillin-resistant Staphylococcus aureus while 35% thought it was <1% 10 years ago. In all, 49% research participants thought that over 1%–20% of S. aureus bacteremias were caused by vancomycin-resistant bacteria in Malaysia, and 40% students believed that over 21%–40% of all bacterial infections in Malaysia (excluding TB) were resistant to all known antibiotics (). These findings were more or less similar to Bangladeshi and European studies.Citation85,Citation87
Antibiotic usage
About 35% and 23% of the research participants thought that 41%–60% antimicrobials used in hospitals in Malaysia and the antibiotic chosen were inappropriate (). Current study findings regarding antimicrobial usage in the hospital are lower than the US studyCitation23 but the irrational use of antibiotics was quite similar to a number of studies.Citation25–Citation28
Contributors to resistance
The majority of this study respondents agreed that “too many antibiotic prescriptions” (55%), “too many broad spectrum antibiotics used” (50%), and “excessive use of antibiotics in livestock” (43%) were primary contributors to AR (). These findings were similar to some studies conducted in different parts of the world.Citation85,Citation88–Citation90 Another group felt that “too long durations of antibiotic treatment” (42%), “dosing of antibiotics are too low” (36%), “poor hand hygiene” (27%), “not removing the focus of infection” (41%, 58), and “paying too much attention to pharmaceutical representatives/advertising” (37%) were moderately important factors contributing to AR (). A good number of research participants were quite aware of poor hand hygiene as a contributor to AR. A lot of studies have reported that poor hand hygiene contributes to AR.Citation90–Citation92 Since our respondents were still students and remain within the university, they have yet to be exposed to the persuasions of the pharmaceutical industries.Citation76,Citation87,Citation93
Development of antibiotics
In all, 45% and 32% of the research participants believed that six to ten and eleven to 15 antibiotic classes became available during the period 1980–2011 and 2011–2020, respectively (). The present study findings were different from a European study. In this study, respondents believed that more antimicrobials were available during 2011–2020.Citation65
Perceptions of AR
About 23% and 10% of research participants think that death due to RTA and lung cancer is four to five and eight to 20 times higher than AR, respectively (). These findings were only 9% in a multicenter European study.Citation65 Research respondents (10–13%) thought that death due to RTA and lung cancer were similar with AR but a European study reported that 51% of study respondents believed there are similar mortality numbers in AR, RTA and lung cancer ().Citation65
Limitation of the study
This is a cross-sectional study. Therefore, the findings are only the snapshot of the current clinical batches of medical students in UniSZA, Malaysia. Again, the sample size was small because the UniSZA MBBS program has only 179 clinical medical students. Therefore, it will be difficult to generalize the findings for the whole country.
Conclusion
Taking into account the limitation of a cross-sectional study, this study was able to find the prevailing perception of respondents regarding antimicrobial prescribing and resistance. This research has evidently concluded that there is a gap between theoretical input and clinical practice. Students have demanded more educational intervention to face this potential threat of AR. Clinical competency regarding antibiotic prescribing during their housemanship was mainly acquired by emulating senior colleagues, and this should be replaced by P-drug selection program in the MBBS curriculum and also during housemanship. Both national and local guidelines for antibiotic prescribing should be made available more easily, preferably as a free download from the university or hospital website. Moreover, care must be taken to update the guidelines regularly. In summary, AR is a multifactorial problem. Therefore, much integration and cooperation among all health professionals, including patients, is needed to eliminate and reduce the risk of bacterial resistance developing to antimicrobials.
Acknowledgments
The authors are much grateful to all participating medical students of Faculty of Medicine, UniSZA, Malaysia. The authors would like to extend their sincere thanks to Seraj Zohurul Haque, Year IV medical student, Faculty of Medicine, University of Dundee, Dundee DD1 4HN, Scotland, UK. As a final point, we express our gratitude to Dr Mohd Afandi bin Muhamad, Malaysia, for his comment and notes. This study has obtained no funding.
Disclosure
The authors report no conflicts of interest in this work.
References
- ClardyJFischbachMACurrieCRThe natural history of antibioticsCurr Biol20091911R437R44119515346
- American Chemical SocietyThe Discovery and Development of Penicillin 1928–1948International Historic Chemical LandmarkWashington, DCACS1999 Available from: http://www.acs.org/content/dam/acsorg/education/whatischemistry/landmarks/flemingpenicillin/the-discovery-and-development-of-penicillin-commemorative-booklet.pdfAccessed November 10, 2015
- DigginsFThe true history of the discovery of penicillin by Alexander FlemingBiomed Sci2003246249
- PeláezFThe historical delivery of antibiotics from microbial natural products – can history repeat?Biochem Pharmacol200671798199016290171
- SagaTYamaguchiKHistory of antimicrobial agents and resistant bacteriaJMAJ2009522103108
- BassettEJKeithMSArmelagosGJMartinDLVillanuevaARTetracycline-labeled human bone from ancient Sudanese Nubia (A.D. 350)Science1980209153215347001623
- NelsonMLDinardoAHochbergJArmelagosGJBrief communication: mass spectroscopic characterization of tetracycline in the skeletal remains of an ancient population from Sudanese Nubia 350–550 CEAm J Phys Anthropol201014315115420564518
- CookMMoltoEAndersonCFluorochrome labelling in Roman period skeletons from Dakhleh Oasis, EgyptAm J Phys Anthropol1989801371432679120
- ArmelagosGJDisease in ancient NubiaScience1969163225258
- BorgdorffMWvan SoolingenDThe re-emergence of tuberculosis: what have we learnt from molecular epidemiology?Clin Microbiol Infect2013191088990123731470
- DeloguGSaliMFaddaGThe biology of mycobacterium tuberculosis infectionMediterr J Hematol Infect Dis201351e201307024363885
- SohailMTuberculosis: A re-emerging enemyJ Mol Genet Med200621878819565002
- World Health Organization ReportGlobal Tuberculosis Control, Surveillance, Planning, Financing, W.H.O./HTM/TB/2005GenevaWorld Health Organization2005 Available from: http://library.cphs.chula.ac.th/Ebooks/AnnualReport/TB/TB2005.pdfAccessed March 04, 2016
- World Health OrganizationAntimicrobial resistance Fact Sheet No. 194. Updated 2015. Available from: http://www.who.int/mediacentre/factsheets/fs194/en/Accessed November 10, 2015
- BishtRKatiyarASinghRMittalPAntibiotic resistance – a global issue of concernAsian J Pharm Clin Res20092210431049
- RogerFGGreenwoodDNorbbySRWhitleyRJAntibiotic and Chemotherapy, The Problem of Resistance8th edEdinburghChurchill Livingstone20032547
- MagiorakosAPSrinivasanACareyRBMultidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistanceClin Microbiol Infect201218326828121793988
- LevySBFactors impacting on the problem of antibiotic resistanceJ Antimicrob Chemother2002491253011751763
- TripathiKDEssentials of Medical Pharmacology, Antimicrobial Drugs: General Consideration5th edNew DelhiJaypee Brother’s Medical Publishers (P) Ltd2003627640
- ColeECAddisonRMRubinoJRInvestigation of antibiotic and antibacterial agent cross-resistance in target bacteria from homes of antibacterial product users and nonusersJ Appl Microbiol200395466467612969278
- BarkerKFAntibiotic resistance: a current perspectiveBr J Clin Pharmacol199948210912410417485
- HouangETGreenwoodDAminoglycoside cross-resistance patterns of gentamicin-resistant bacteriaJ Clin Pathol1977308738744413843
- CarsOMölstadSMelanderAVariation in antibiotic use in the European UnionLancet200135792711851185311410197
- LlorCBjerrumLAntimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problemTher Adv Drug Saf20145622924125436105
- LevySBThe challenge of antibiotic resistanceSci Am1998278346539487702
- WiseRHartTCarsOAntimicrobial resistance. Is a major threat to public healthBMJ199831771596096109727981
- RichardsJEmergence & spread of multiresistant organisms: can infection control measures help?Int J Infect Control2009v5i2
- HarrisonPFLederbergJAntimicrobial Resistance: Issues and OptionsWashington, DCNational Academy Press1998
- LevySBThe Antibiotic Paradox. How Miracle Drugs Are Destroying the MiracleNew YorkPlenum Publishing2002
- LevySBAntibiotic resistance: an ecological imbalanceChadwickDGoodeJAntibiotic Resistance: Origins, Evolution, Selection and SpreadChichesterWileyCiba Foundation Symposium 2071997114
- CarsOHedinAHeddiniAThe global need for effective antibiotics – moving towards concerted actionDrug Resist Updat201114686921444235
- LenskiREBacterial evolution and the cost of antibiotic resistanceInt Microbiol19981426527010943373
- van der BijAKPitoutJDThe role of international travel in the worldwide spread of multiresistant EnterobacteriaceaeJ Antimicrob Chemother20126792090210022678728
- JohnsonAPWoodfordNGlobal spread of antibiotic resistance: the example of New Delhi metallo-β-lactamase (NDM)-mediated carbapenem resistanceJ Med Microbiol20136249951323329317
- BrandtCMakarewiczOFischerTThe bigger picture: the history of antibiotics and antimicrobial resistance displayed by scientometric dataInt J Antimicrob Agents201444542443025216545
- United States Centers for Disease Control and PreventionAntibiotic Resistance Threats in the United States2013 Available from: http://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdfAccessed November 10, 2015
- World Health OrganizationAntimicrobial Resistance Global Report on Surveillance2014GenevaWorld Health Organization Available from: http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdfAccessed November 10, 2015
- HasanRJabeenKMehrajVTrends in Mycobacterium tuberculosis resistance, Pakistan, 1990–2007Int J Infect Dis2009136e377e38219369103
- CarletJJarlierVHarbarthSVossAGoossensHPittetDParticipants of the 3rd World Healthcare-Associated Infections ForumReady for a world without antibiotics? The Pensières Antibiotic Resistance Call to ActionAntimicrob Resist Infect Control2012111122958833
- LimVKCheongYMSuleimanABPattern of antibiotic usage in hospitals in MalaysiaSingapore Med J19933465255288153716
- CheongYMLimVKJegathesanMSuleimanABAntimicrobial resistance in 6 Malaysian general hospitalsMed J Malaysia19944943173267674966
- NorazahALimVKEMunirahSNKamelAGMStaphylococcus aureus carriage in selected communities and their antibiotic susceptibility patternsMed J Malaysia20035825526114569746
- LeeWSPuthuchearySDSpecies distribution and antibiotic resistance of Shigella isolates in an urban community in MalaysiaMed J Malaysia20035826226714569747
- TengCLNurjahanMIHashimNAPunithambigaiPLeongKCMihatObUpper respiratory tract infections: To what extent is the management evidence based?Med J Malaysia20035815916614569735
- LimVKEAntibiotic resistance in the communityMed J Malaysia200358215615814569734
- TengCLLeongKCAljunidSMCheahMAntibiotic prescription in upper respiratory tract infectionsAsia Pac Fam Med200431–23845
- TengCLTongSFKhooEMAntibiotics for URTI and UTI – prescribing in Malaysian primary care settingsAust Fam Physician201140532532921597554
- KhoBPOngCMTanFTWeeCYAntibiotic prescribing for upper respiratory tract infections in Sarawak district hospitalsMed J Malaysia201368213614023629559
- ChanGCTangSFParental knowledge, attitudes and antibiotic use for acute upper respiratory tract infection in children attending a primary healthcare clinic in MalaysiaSingapore Med J200647426627016572235
- Ling OhAHassaliMAAl-HaddadMSSyed SulaimanSAShafieAAAwaisuAPublic knowledge and attitudes towards antibiotic usage: a cross-sectional study among the general public in the state of Penang, MalaysiaJ Infect Dev Ctries20115533834721628809
- LimKKTehCCA cross-sectional study of public knowledge and attitude towards antibiotics in Putrajaya, MalaysiaSouth Med Rev201252263323532680
- IslahudinFTameziAMAShahNMKnowledge, attitudes, and practices about antibiotic use among the general public in MalaysiaSoutheast Asian J Trop Med Public Health20144561474148226466434
- LimVAntibiotic StewardshipIeJSME20126Suppl 1S75S79
- World Health OrganizationThe Evolving Threat of Antimicrobial Resistance: Options for ActionGenevaWorld Health Organization2012 Available from: http://apps.who.int/iris/bitstream/10665/44812/1/9789241503181_eng.pdfAccessed November 10, 2015
- WrightEPJainPSurvey of antibiotic knowledge amongst final year medical studentsJ Antimicrob Chemother20045355055114762052
- HumphreysHDillaneTO’ConnellBLukeLCSurvey of recent medical graduates’ knowledge and understanding of the treatment and prevention of infectionIr Med J200699585916548226
- AbboLMCosgroveSEPottingerPSMedical students’ perceptions and knowledge about antimicrobial stewardship: how are we educating our future prescribers?Clin Infect Dis20135763163823728148
- KamulegeyaAKizitoANBalidawaHUgandan medical and health sciences interns’ infection control knowledge and practicesJ Infect Dev Ctries201371072673324129625
- JorakAKeihanianFSaeidiniaAHeidarzadehASaeidiniaFA cross-sectional study on knowledge, attitude, and practice of medical students toward antibiotic resistance and its prescription, IranAdv Environ Biol2014817675681
- HarakehSAlmatrafiMUngapenHPerceptions of medical students towards antibiotic prescribing for upper respiratory tract infections in Saudi ArabiaBMJ Open Respir Res20152e000078
- SuaifanGARYShehadehMDarwishDAAl-IjelHYousef Al-MMDarwishRMA cross-sectional study on knowledge, attitude and behavior related to antibiotic use and resistance among medical and non-medical university students in JordanAfr J Phar Pharmacol2012610763770
- ThriemerKKatualaYBatokoBAntibiotic prescribing in DR Congo: A knowledge, attitude, and practice survey among medical doctors and studentsPLoS One201382e5549523441152
- HuangYGuJZhangMKnowledge, attitude and practice of antibiotics: a questionnaire study among 2500 Chinese studentsBMC Med Educ20131316324321449
- KållbergCMedical Students’ Views on the Current and Future Antibiotic Resistance SituationSahlgrenska Academy, University of Gothenburg Available: http://www.reactgroup.org/uploads/react/resources/260/Medical%20students%E2%80%99%20views%20on%20the%20current%20and%20future%20antibiotic%20resistance%20situation.en.319.pdfAccessed November 10, 2015
- DyarOJPulciniCHowardPNathwaniDESGAP (ESCMID Study Group for Antibiotic Policies)European medical students: a first multicentre study of knowledge, attitudes, and perceptions of antibiotic prescribing and antibiotic resistanceJ Antimicrob Chemother201469384284624191307
- LaxminarayanRDuseAWattalCAntibiotic resistance – the need for global solutionsLancet Infect Dis201313121057109824252483
- World Health OrganizationManaging for rational medicine useEssential Medicines and Health Products Information PortalGenevaWorld Health Organization2012 Chapter 27. Available from: http://apps.who.int/medicinedocs/documents/s19604en/s19604en.pdfAccessed November 10, 2015
- World Health OrganizationPromoting Rational Use of Medicines: Core ComponentsGenevaWorld Health Organization2002 Available from: http://www.who.int/medicines/publications/policyperspectives/ppm05en.pdfAccessed November 10, 2015
- OrmeMFrolichJVrhovacBEducation Sub-Committee of the European Association for Clinical Pharmacology and TherapeuticsTowards a core curriculum in clinical pharmacology for undergraduate medical students in EuropeEur J Clin Pharmacol20025863564012483457
- JamshedSQElkalmiRRajiahKUnderstanding of antibiotic use and resistance among final-year pharmacy and medical students: a pilot studyJ Infect Dev Ctries20148678078524916878
- RahmanNIAzizAAZulkifliZPerceptions of students in different phases of medical education of the educational environment: Universiti Sultan Zainal AbidinAdv Med Educ Pract2015621122225848333
- IsmailSSalamAAlattraqchiAGEvaluation of doctors’ performance as facilitators in basic medical science lecture classes in a new Malaysian medical schoolAdv Med Educ Pract2015623123725878516
- Malaysian Qualifications AgencyCode of Practice for Program Accreditation2nd edSelangor Darul EhsanMalaysia2008
- Malaysian Qualifications AgencyCode of Practice for Institutional Audit1st edSelangor Darul EhsanMalaysia2008
- SalamAYousufRIslamMZProfessionalism of future medical professionals in Universiti Sultan Zainal Abidin, MalaysiaBangladesh J Pharmacol20138124130
- SalamAHaqueMIslamMZComparative study of professionalism of future medical professionals among three private medical colleges of BangladeshAsian J Pharm Clin Res201363170179
- SalamAHaqueMHelaliAMComparative study on professionalism of forthcoming medical doctors between two private medical colleges in Savar, BangladeshInt J Pharm Pharm Sci201359Suppl 3659665
- IslamMZSalamAHelaliAMComparative study of professionalism of future medical doctors between Malaysia and BangladeshJ App Pharm Sci2014446671
- ECDC/EMEA Joint Technical ReportThe Bacterial Challenge: Time to React2009 Available from: http://ecdc.europa.eu/en/publications/Publications/0909_TER_The_Bacterial_Challenge_Time_to_React.pdfAccessed November 10, 2015
- World Health OrganizationWHO methods and data sources for global burden of disease estimates 2000–2011Global Health Estimates Technical Paper WHO/HIS/HSI/GHE/2013.4WHOGeneva2013Accessed November 10, 2015
- KongsvedSMBasnovMHolm-ChristensenKHjollundNHResponse rate and completeness of questionnaires: a randomized study of Internet versus paper-and-pencil versionsJ Med Internet Res200793e2517942387
- ChenMKChevalierJAAre women overinvesting in education? Evidence from the medical professionJ Hum Cap201262124149
- BBCWomen docs “weakening” medicine2004 Available from: http://news.bbc.co.uk/1/hi/health/3527184.stmAccessed November 10, 2015
- ElstonMAWomen and medicine: the futureRoyal College of Physicians2009 Available from: https://www.rcplondon.ac.uk/sites/default/files/documents/women-and-medicine-future-full-report.pdfAccessed November 10, 2015
- PulciniCWilliamsFMolinariNDaveyPNathwaniDJunior doctors’ knowledge and perceptions of antibiotic resistance and prescribing: a survey in France and ScotlandClin Microbiol Infect2011171808720132254
- AggarwalSMathewJSinghHSharmaVAttitude, and perception of junior resident doctors’ regarding antibiotic resistance – a pilot studyJ Acute Dis20143169
- HoqueRMostafaAHaqueMIntern doctors’ views on the current and future antibiotic resistance situation of Chattagram Maa O Shishu Hospital Medical College, BangladeshTher Clin Risk Manag2015111177118526316762
- AberaBKibretMMuluWKnowledge and beliefs on antimicrobial resistance among physicians and nurses in hospitals in Amhara Region, EthiopiaBMC Pharmacol Toxicol20141512624887310
- SutradharKBSahaAHudaNHUddinRIrrational use of antibiotics and antibiotic resistance in Southern Rural Bangladesh: perspectives from both the physicians and patientsAnnu Res Rev Biol20144914211430
- Navarro-San FranciscoCDel ToroMDCoboJKnowledge and perceptions of junior and senior Spanish resident doctors about antibiotic use and resistance: results of a multicenter surveyEnferm Infecc Microbiol Clin201331419920422819389
- SARI Infection Control SubcommitteeGuidelines for Hand Hygiene in Irish Health Care SettingsPublished on behalf of SARI by HSE, Health Protection Surveillance Centre. SARI Infection Control Subcommittee2004151 Available from: https://www.hpsc.ie/A-Z/Gastroenteric/Handwashing/Publications/File,1047,en.pdfAccessed November 10, 2015
- Centers for Disease Control and PreventionGuideline for hand hygiene in health-care settings: recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task ForceMMWR Recomm Rep200251145 quiz CE1–E4. Available: http://www.cdc.gov/mmwr/PDF/rr/rr5116.pdf. Accessed March 04, 2016
- SierlesFSBrodkeyACClearyLMMedical students’ exposure to and attitudes about drug company interactions: a national surveyJAMA200529491034104216145023