Abstract
Background
The most common of the neuropathies associated with diabetes mellitus, diabetic sensorimotor polyneuropathy (DSPN) is a syndrome of diffuse, length-dependent, symmetric nerve dysfunction. The condition is linked with substantial morbidity, frequent healthcare utilization, and compromised quality of life due to related discomfort. Correspondingly, antidepressants, anticonvulsants, and opioids are regularly prescribed with the goal of pain control. However, the agents rarely provide complete pain relief and fail to address progression of the disorder. Whereas strict blood glucose control can slow the onset and worsening of DSPN, near-normoglycemia is not easily attainable. Evidence implicating oxidative processes in the pathogenesis of DSPN offers one potentially important therapeutic avenue. Due to its properties as a potent antioxidant, alpha lipoic acid (ALA) could mitigate the development of DSPN and attenuate resultant symptoms and signs. Approved for treatment of DSPN in Germany, the agent is not more widely used due to uncertainty about its efficacy and reported adverse effects. Here we review the effectiveness and tolerability of ALA in the treatment of symptomatic DSPN.
Methods
The MEDLINE, EMBASE, and Cochrane Library databases were searched for English-language literature on the topic. Randomized, blinded studies comparing parenteral and oral ALA with placebo in the treatment of peripheral neuropathy in diabetic adults were selected. Analysis included studies with a level of evidence of at least 2b.
Results
The current appraisal summarizes data from 1160 participants in the ALADIN, SYDNEY, ORPIL, SYDNEY 2, and ALADIN III trials. In four of the studies, ALA provided significant improvement in manifestations of DSPN.
Conclusion
Treatment with ALA 600 mg iv daily for 3 weeks represents a well-tolerated and effective therapy for DSPN. An oral dose of 600 mg daily administered for up to 5 weeks could offer benefits in symptoms and signs of DSPN without significant side effects.
Introduction
Diabetes mellitus (DM) is estimated to affect 439 million adults throughout the world by 2030.Citation1 Complications of DM include a variety of neuropathies, which can be classified as focal or diffuse.Citation2 Cranial mononeuropathies, diabetic amyotrophy, and focal appendicular neuropathies fall into the ‘focal’ category. ‘Diffuse’ neuropathies include chronic inflammatory demyelinating polyneuropathy and diabetic sensorimotor polyneuropathy (DSPN), the latter being a condition characterized by generalized, length-dependent, symmetric nerve dysfunction.Citation2
Of the neuropathies associated with DM, DSPN is the most common.Citation2,Citation3 The prevalence increases from 10% within the first year of a DM diagnosis to 50% after 25 years.Citation4 Whereas the majority of cases are asymptomatic, symptomatic DSPN represents an important clinical challenge in type 1 and type 2 DM populations.Citation3,Citation5 Beyond substantial morbidity and mortality, painful DSPN translates into emotional distress, sleep disturbance, decreased productivity, and increased demands on healthcare resources.Citation6–Citation11
Given a reduced quality of life, it is not surprising that patients seek treatment for DSPN.Citation7 Patients most commonly report hot, burning, electric, sharp, achy, and tingling sensations in a stocking-glove distribution.Citation8 Many of these symptoms are attributable to small-fiber neuropathy, which often precedes large fiber dysfunction.Citation2 Alternatively, patients may present with negative symptoms, such as numbness and gait unsteadiness, suggestive of large fiber damage.Citation2
In the absence of alternative etiologies, length-dependent deficits in pinprick, temperature, light touch, proprioception, and vibration sense are objective markers of DSPN.Citation2 Abnormalities in strength and reflexes can also occur in advanced stages of disease.Citation2,Citation3 The concomitants of nerve fiber injury can be detected on nerve conduction studies and electromyography. Reductions in distal sensory response amplitudes and conduction velocities are evident prior to the development of motor abnormalities, thereby paralleling the clinical course of DSPN.Citation2
Pathogenesis of DSPN
Chronic hyperglycemia is believed to play a key role in the pathogenesis of DSPN via oxidative stress generated in heterogeneous and overlapping pathways.Citation12–Citation14 Enhanced flux through the polyol pathway, glucose auto-oxidation, and accumulation of advanced glycation end-products are thought to cause oxidative stress; in turn oxidative stress downregulates Na-K-ATPase activity and results in nerve ischemia.Citation12,Citation14 Endoneurial hypoxia and microvascular damage may also occur from the downstream inactivation of nitrous oxide and, thereby, increased vascular tension coupled with decreased blood flow.Citation12 Oxidative stress resulting from hyperglycemia is also reported to cause programmed cell death.Citation12,Citation14 Increased sorbitol, decreased myo-inositol, protein kinase C activation, changes in cellular processing, and immune complex deposition may contribute to the development of DSPN.Citation2,Citation12,Citation14
Treatment approaches: symptomatic and pathogenic
As adjuncts to antidiabetic agents targeting tight glycemic control, many treatments are prescribed with the goal of DSPN symptom relief. Evidence-based guidelines recommend the graded use of tricyclic antidepressants, serotonin–norepinephrine reuptake inhibitors, antiepileptic drugs, opioids, and mexiletine.Citation15,Citation16 Topical agents such as capsaicin and lidocaine are also suggested.Citation15 The effectiveness of the existing approach is suboptimal; research shows that mono- and combination therapies almost never provide complete pain pelief.Citation15
Until recently, glycemic control was the only treatment aimed at etiologic factors in DSPN. Indeed, strict glycemic control over 4–5 years can reduce, postpone, and possibly prevent the development of neurological deficits, nerve conduction abnormalities, and autonomic dysfunction.Citation17,Citation18 While an effective cornerstone of therapy, near-normoglycemia is not always possible to achieve or maintain.Citation19,Citation20 Given the role of oxidative processes in DSPN, antioxidants could offer additional therapeutic benefit. Among the emerging therapies, one of the most promising is alpha lipoic acid (ALA).
Alpha lipoic acid (Thioctic acid)
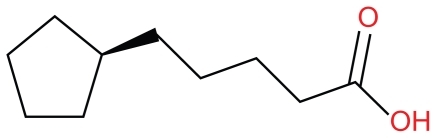
The only fat and water-soluble antioxidant,Citation12 R-lipoic acid (1,2-dithiolane-3-pentanoic acid) was incidentally discovered by Snell et al in 1937 as a potato extract required for bacterial growth;Citation21 the agent was later characterized by Reed and colleagues in 1951 ().Citation12,Citation14,Citation23,Citation24 Ultimately revealed to function as a cofactor for mitochondrial enzymes, ALA is created endogenously by plants and animals.Citation14 After uptake into cells and tissues, it is reduced to dihydrolipoic acid (DHLA).Citation14 Both ALA and DHLA are potent antioxidants, with the latter regenerating other factors such as vitamins C and E in addition to raising glutathione intracellularly.Citation14,Citation25 Further, both ALA and DHLA function as free radical scavengers.Citation14,Citation22
ALA is proposed to mitigate the development of DSPN by addressing reactive oxygen and nitrogen species that are overproduced in the setting of DM.Citation14 In neuroblastoma cell cultures, the agent has been associated with the sprouting of neurites.Citation26 In addition to a regenerative capacity, ALA offers protection against nerve ischemia in rats.Citation12 Experimental models have also shown that the administration of ALA can significantly reduce the expression of glial and neuronal markers, decrease lipid peroxidation, and help correct deficits in nerve blood flow, oxidative stress, and distal sensory and motor nerve conduction.Citation13,Citation27,Citation28
Although synthesized de novo, ALA can also be absorbed from the diet.Citation25,Citation29,Citation30 Dietary supplements ranging in doses from 200–600 mg are likely to provide up to 1000 times the amount of ALA available from a regular diet.Citation30 Preclinical and clinical data indicate ALA is bioavailable and safe in moderate doses.Citation29 Gastrointestinal absorption is variable, and use with food decreases uptake.Citation29,Citation30 Accordingly, it is recommended that the agent be consumed 30 to 60 minutes before, or at least 120 minutes after, a meal.Citation14,Citation30 The antioxidant is very rapidly absorbed and cleared; maximum blood levels are achieved after 30 to 60 minutes, and the half-life of parenteral ALA is 30 minutes.Citation30,Citation31 It is thought to be extensively metabolized in the liver.Citation14 Nevertheless, it is considered safe in hepatic and renal disease.Citation22
Intravenous and oral forms of ALA are approved for the treatment of DSPN in Germany, where it is also covered by insurance.Citation30,Citation32 While not officially sanctioned in many countries, oral formulations are readily available over the counter and online. The agent is relatively inexpensive; in New Zealand currency, each 600 mg tablet costs about 53 cents.Citation33 Despite its qualities as a safe, available, inexpensive antioxidant, ALA is not widely used in part due to incomplete knowledge of its efficacy and adverse effects. The goal of this review is to assess the safety and effectiveness of treatment with parenteral and oral alpha lipoic acid on the symptoms, sensory deficits, and abnormal electrophysiological parameters of adults with symptomatic DSPN.
Methods
The MEDLINE, EMBASE, and Cochrane Library databases were searched for English-language literature on April 6 and April 11, 2011 using the terms ‘lipoic acid’, ‘alpha lipoic acid’, ‘thioctic acid’, ‘trometamol salt of thioctic acid’, ‘diabetes’, ‘diabetic neuropathy’, and ‘painful peripheral neuropathy’. Randomized studies comparing the use of parenteral or oral ALA with placebo in the treatment of painful peripheral neuropathy in adults with type 1 and type 2 DM were selected. Meta-analyses and systematic reviews were also considered. Information on adverse events was culled from the trials. The reference lists of articles were also reviewed. Studies evaluating the effect of ALA on autonomic neuropathy and diabetic mononeuropathy were excluded. Studies for which primary data could not be obtained were excluded. As the one meta-analysis reviewed did not adhere to the standards of the Cochrane Collaboration, it was not included in the primary review.Citation32
There was no disagreement among authors regarding the studies selected for inclusion.
Results
Five randomized double-blind placebo-controlled trials, the ALADIN, SYDNEY, ORPIL, SYDEY 2, and ALADIN III studies, comprising a total of 1160 people were selected (see and for summaries of the studies). The study populations included individuals ranging in age from 18 to 74 years with type 1 and 2 DM. Mean body mass indices ranged from 27.7 to 30.9. On average, initial glycosylated hemoglobin was <12%. The average duration of DM ranged from 10.4 to 15.1 years, while that of DSPN ranged from 2.8 to 5 years. The studies took place in inpatient and outpatient treatment centers throughout Germany, Russia, and Israel. The trials relied on mono- and multicenter participation.Citation20,Citation34–Citation37
Table 1 Placebo-controlled trials studying the efficacy of parenteral and oral alpha lipoic acid in the treatment of symptoms, clinical signs, and electrophysiology of diabetic sensorimotor polyneuropathy
Table 2 Placebo-controlled trials studying the safety of parenteral and oral alpha lipoic acid in the treatment of symptomatic diabetic sensorimotor polyneuropathy
The five studies evaluated the effectiveness of ALA on DSPN using three different types of drug administration. Two studies evaluated the role of parental ALA compared with placebo.Citation20,Citation37 The parenteral treatment was given to separate intervention groups in doses of 100 mg daily, 600 mg daily, and 1200 mg daily. A total of 14 treatments were given over 3 weeks in both studies.Citation20,Citation37 Two of the studies examined the effects of oral ALA relative to control patients with DSPN.Citation34,Citation35 Oral treatment was given to individual groups at total daily doses of 600 mg, 1200 mg, and 1800 mg. Duration of treatment ranged from 3 to 5 weeks.Citation34,Citation35 One trial included a combination of parenteral and oral alpha lipoic acid given sequentially.Citation36 Combination therapy included schedules of ALA 600 mg iv daily for 3 weeks prior to 1800 mg orally daily for 6 months and 600 mg iv daily prior to oral placebo for 6 months versus iv placebo treatment followed by oral placebo treatment. The total study duration was 7 months.Citation36
The trials included a variety of outcome measures including symptom scores, clinical signs, and electrophysiology. All 5 included trials used the subjective measure of Total Symptom Score (TSS) as the primary endpoint (). The TSS is the summation of the presence, severity, and duration of lancinating pain, burning pain, prickling, and numbness. Total scores can range from 0 to 14.64; a peak score suggests the continuous presence of severe discomfort in all four symptom domains. Beyond statistically significant changes in the measure, a clinically meaningful improvement in TSS was defined as a mean difference of at least 1.83 points.Citation34,Citation38 Several secondary measures of patient experience were also reported, including the four individual components of the TSS, the Number-Severity-Change (NSC) metric, the Global Assessment of Efficacy (GAE), and the Hamburg Pain Adjective List (HPAL).
Table 3 Total Symptom Score measure for sticking or lancinating pain, burning, prickling, and numbness
In addition to measures of subjective improvement, studies also gauged the effect of ALA on measurable clinical signs. Two secondary measures comprised the Neuropathy Impairment Score (NIS) and the NIS in the lower limbs (NIS-LL). Endpoints also included the Neuropathy Disability Scale (NDS), a quantified neurological examination derived from cranial nerve, sensory, motor, and reflex integrity.Citation39 Electrophysiological measures variably included amplitude, velocity, and latency of the tibial and peroneal nerves in addition to the amplitude and latency of the sural nerve.
ALA efficacy: parenteral administration
In the Alpha-Lipoic Acid in Diabetic Neuropathy (ALADIN) Trial, (level of evidence 1b),Citation32 328 patients with DM 2 were recruited. Three hundred and twenty-six participants were randomized to one of four groups in a multicenter, double-blind, placebo controlled study. Eighty-two patients were given a placebo. Members of treatment groups received ALA at doses of 100 mg per day (n = 81), 600 mg per day (n = 77), or 1200 mg per day (n = 86) by iv. The drug was administered on 14 days over the course of 3 weeks. A significant decrease in TSS was noted in the intervention group relative to placebo by day 5; the effect was maintained until treatment end. There was no significant difference between the mean changes in TSS scores for the 100 mg per day treatment group and the placebo group. In addition to significant improvements from baseline TSS (5 points, P < 0.001 in the 600 mg group, 4.5 points, P = 0.003 in the 1200 mg group), there were significant improvements in the components of burning, paresthesias, and numbness in the 600 mg and 1200 mg groups (P < 0.05). The percentage of patients who experienced a clinically meaningful response reached significance in the 600 mg per day group relative to placebo (P = 0.002). The HPAL showed commensurate reductions in pain with both treatment groups compared with placebo (P < 0.001). Physicians rated global efficacy of ALA as very good or good in a significantly greater proportion of patients in the 600 mg per day treatment group relative to placebo (P = 0.001). A dose of 1200 mg per day resulted in significant change in the NDS (P = 0.03). Of the 326 initially enrolled, 260 participants completed the trial. Adverse events were reported in all groups but only reached significance in the 1200 mg per day arm (P < 0.05), with side effects including headache, nausea, and vomiting.Citation37
The Symptomatic Diabetic Neuropathy (SYDNEY) Trial (level of evidence 1b)Citation32 was an inpatient, single-center, randomized, double-masked placebo-controlled trial including a total of 120 patients with type 1 and 2 DM. Sixty participants were randomized to receive 600 mg of ALA and 60 were randomized to receive a placebo. There was a 1-week placebo run-in phase for both groups. The trial was conducted over the next 3 weeks, during which time 14 doses of ALA or placebo were given parenterally. Similar to the results of the ALADIN trial, a significant treatment effect was first appreciated in the experimental group relative to the placebo group by day 4; there was subsequent steady improvement thereafter. On the last day, the TSS of patients in the treatment group had improved by a mean of 5.72 points (P < 0.001). Further, there was significant improvement in all components (pain, burning, paresthesias, and numbness) measured by the TSS. Confirming the beneficial relationship between ALA and subjective relief, the SYDNEY Trial showed significant amelioration in the mean change of positive and negative sensory symptoms by the NSC metric (P < 0.05), although there was no significant improvement in perceptions of weakness. Patients rated the global efficacy of ALA as very good or good in a significantly greater proportion of participants in the 600 mg per day treatment group relative to placebo (P < 0.01). Significant improvement in NIS scores (2.7 points, P < 0.001) was also observed. The distal latency of the sural nerve was significantly shorter in the ALA group than in the placebo group (P = 0.017); however, no other significant effects on nerve conduction were identified. Of 120 participants, seven given placebo and one taking ALA reported unspecified adverse effects. None of the side effects were considered causally related to the experimental agent. One hundred eighteen participants completed the trial.Citation20
ALA efficacy: oral administration
Twenty-four patients with DM 2 participated in the Oral Pilot (ORPIL) trial (level of evidence 1b),Citation32 a single-center randomized, double-blind placebo-controlled study. Twelve patients were assigned to the placebo group. Twelve patients were assigned to a treatment group, in which ALA 600 mg was administered orally three times daily. The trial demonstrated that a 3-week course of oral ALA at a dose of 1800 mg a day translates into a significant reduction in the mean TSS for the feet (3.75 points, P = 0.021). After 3 weeks, those in the treatment group also reported a significant improvement in the burning component of the TSS (P = 0.012). HPAL scores decreased but not to a level of significance. Relative to placebo, there was significant improvement in the NDS for the treatment group (P = 0.025). A total of 22 participants completed the trial. There were no differences in the adverse events between groups, and no specific side effects were reported.Citation35
The findings were supported by the SYDNEY 2 trial (level of evidence 1b),Citation32 a multicenter double-blind placebo-controlled study conducted over 5 weeks. In the study, 181 participants with DM 1 and 2 were randomized to receive a placebo (n = 43), ALA 600 mg per day (n = 45), ALA 1200 mg per day (n = 47) or ALA 1800 mg per day (n = 46). Treatment was started after a 1-week placebo run-in phase. Significant improvements in TSS were noted by week 1 in the 1800 mg group and by week 2 in the 600 and 1200 mg groups. The significant improvements in total TSS were maintained at treatment end with all active doses (P < 0.05). Consistent with the ORPIL trial, the agent most effectively alleviated symptoms of pain and burning. Significant improvements were seen in NSC scores for all ALA doses relative to placebo (P < 0.05 except NSC number in ALA 1800, P = 0.08). Members of all ALA groups rated treatment significantly more favorably than those in the placebo group (P < 0.05). Interestingly, significant improvement in the overall NIS was noted only at a dose of 1200 mg (P < 0.05), while sensory function in the lower limbs (NIS-LL) improved significantly with ALA 600 mg per day over 5 weeks (P < 0.05). The results of nerve conduction studies were not reported. Of the initial 181 participants, 166 completed the trial. Fifteen left the study, mostly due to adverse effects including nausea, vomiting, and vertigo. Overall, side effects were reported by 27% of the 600 mg group (P = 0.53), 43% of the 1200 mg group (P = 0.03), and 54% of those in the 1800 mg group (P < 0.001 relative to placebo).Citation34
ALA efficacy: sequential parenteral and oral administration
Of the 509 participants initially enrolled, 383 completed the multicenter ALADIN III trial (level of evidence 2b).Citation32 Conducted over a total of 7 months, DM 2 patients were randomized to one of three groups; the first group received placebo in a 3-week iv phase and the subsequent 6-month oral phase (n = 168). The second group received ALA 600 mg iv daily for 3 weeks prior to oral placebo for 6 months (n = 174). The third group received ALA 600 mg iv daily for 3 weeks followed by ALA 600 mg three times daily for 6 months (n = 167). In contrast to the ALADIN and SYDNEY results, treatment with ALA 600 mg iv daily in the ALADIN III trial was not associated with significant changes in mean TSS-feet when compared with placebo at 3 weeks. After an additional 6 months of 1800 mg per day oral therapy, the area under the curve was smaller in the active groups. However, there was no significant difference in symptoms as rated by the TSS after 7 months between any of the active or control groups. The ALADIN III trial demonstrated improvement in NIS after the iv phase of treatment with ALA 600 mg per day over 3 weeks. However, there was no significant difference in NIS after an additional 6 months of oral treatment at a dose of 600 mg three times daily relative to placebo. The rates of side effects were not significantly different between groups.Citation36
Summary of data and discussion
The current appraisal includes data derived from a total of 1160 participants enrolled in the ALADIN, SYDNEY, ORPIL, SYDNEY 2, and ALADIN III studies. Two trials comprising 446 patients in total explored the efficacy and safety of short-term parenteral ALA treatment versus placebo. Compared with placebo, iv ALA was associated with significant, clinically meaningful improvements in sensory symptoms and neuropathic deficits. Doses of 600 mg daily and 1200 mg daily offered equivalent benefits, but the higher dose was associated with significantly more side effects than placebo. The results were confirmed in a meta-analysis pooling data from a total of 1258 participants in the ALADIN, ALADIN III, SYDNEY, and NATHAN II trials.Citation40 While the validity of the research has been challenged,Citation32,Citation38 the work indicated that ALA 600 mg iv daily for 3 weeks translates into a clear therapeutic benefit without significant side effects.Citation40
Two trials consisting of 205 patients total evaluated the effectiveness and tolerability of short-term oral ALA treatment with placebo. Relative to placebo, oral ALA alleviated symptoms and impairments to a significant and clinically meaningful degree at total daily doses of 600 mg, 1200 mg, and 1800 mg. However, there was evidence of dose-related toxicity, with adverse event rates reaching significance at a dose of 1200 mg and climbing at a dose of 1800 mg daily after 5 weeks. The combination of parenteral (600 mg daily for 3 weeks) and oral therapy (600 mg three times daily for 6 months) administered over a total of 7 months failed to translate into significant improvements.
Studies exploring the efficacy of parenteral and oral ALA on the symptoms, signs, and electrophysiological parameters of DSPN date back to at least 1959.Citation41 Validity of data from initial trials is constrained by small sample size, lack of blinding, absence of placebo control, and potentially inadequate treatment doses.Citation38 While the quality of investigations has improved over time, even the most recent randomized double-blind placebo-controlled trials have some methodological limitations.Citation38,Citation42 Further, none provides true Class I evidence.
Although investigators of the reviewed trials may have calculated the number participants necessary to detect meaningful change in study endpoints, ultimate sample size was sometimes inadequate due to participant attrition; drop-out rate reached 25% in one of the studies included in the present analysis.Citation36 Further, the incorporation of as many as 71 treatment sites in multicenter designs likely introduced variability in scoring that affected outcomes.Citation36 Patients with DM 1 and DM 2 were included in the studies reviewed here. While DSPN represents an important clinical problem in both populations, the pathophysiology and response to treatment could differ. Similarly, the magnitude of therapeutic effect could be contingent on baseline status, and initial TSS varied widely across studies. While patients with a baseline TSS of at least 2 were included in one study,Citation37 other trials required TSS be at least 7.5.Citation20,Citation34 Concurrent administration of certain diabetic therapies and antioxidants with ALA could also have influenced results. In three of the studies reviewed, use of diet, oral antidiabetics, and/or insulin constituted a criterion for inclusion.Citation35–Citation37 Although details of the therapies were not outlined, the authors noted the continuation of usual diabetic treatment throughout the study period in one instance.Citation20 Importantly, not all of the trials specifically excluded patients who were using, or had recently used, other antioxidants.Citation20
Whereas the randomized controlled trials reviewed demonstrate significant improvement in symptoms and signs of neuropathy, there is little evidence that ALA has a meaningful effect on nerve conduction. One potential explanation is that ALA preferentially treats small fiber neuropathy, which is not measurable by electrodiagnostic studies. Alternatively, objective improvements in some clinical signs and nerve conduction could take years to manifest. Preliminary support for this notion is provided by two long-term studies. Despite methodological flaws, the ALADIN II trial demonstrated that treatment with ALA at doses of 600 mg and 1200 mg given parenterally for 5 days and then orally for 2 years led to significant improvements in nerve conduction.Citation30 The international NATHAN I trial showed that neuropathy progressed in placebo conditions but improved with oral ALA 600 mg daily over 4 years.Citation43 Future trials evaluating long-term administration of ALA could better define the patterns of effectiveness and tolerability of the agent over years.
All of the reviewed studies suggest ALA is safe at a once daily dose of 600 mg in both iv and oral forms. The investigations also demonstrate significant toxicity emerges at a dose of 1200 mg once daily with both routes of administration after 3–5 weeks of treatment.Citation34,Citation37 Interestingly, ALA at a total daily dose of 1800 mg was well tolerated when administered in three divided doses for as long as 6 monthsCitation35,Citation36 but not as a single daily dose over just 5 weeks.Citation34 The trend raises the possibility that higher amounts of ALA could be well-tolerated if given in smaller divided doses. Of note, the drug formulations varied across the studies and could have influenced side effect rates and symptom relief in meaningful ways.
The current body of evidence suggests that both parenteral and oral forms of ALA can translate into statistically significant symptom relief within 1 week, with steady and continuous improvement thereafter.Citation20,Citation34,Citation37 However, it is uncertain if the trajectory of improvement continues, plateaus, or declines with prolonged treatment and following discontinuation of the agent. Some data indicate the benefits of ALA are not sustained following therapy completion. One study showed that after the discontinuation of ALA 600 mg daily for a mean of 5 years, about 73% of patients developed neuropathic symptoms within 2 weeks in the absence of gabapentin therapy.Citation44 Authors maintain that transitioning from ALA to gabapentin and other conventional medications resulted in increased side effects, more outpatient visits, and heightened daily cost of therapy.Citation44 While the return of symptoms could represent the natural course of disease, it is unclear if transient use of ALA could ultimately worsen symptoms.
In the absence of symptoms, patients with DSPN do not necessarily seek evaluation. As experimental models suggest it has protective properties, starting ALA treatment at the time of DM diagnosis might improve its long-term benefits. Early initiation might be especially important because the ability to endogenously synthesize ALA declines with age in DM.Citation30 In addition to optimal timing and duration of ALA therapy, future studies should explore the use of ALA in combination with other antioxidants given the multifaceted nature of oxidative stress in DSPN.
While there is some evidence that other antioxidants, such as vitamin E, can significantly ameliorate neuropathic symptoms and nerve conduction in patients with DM 2,Citation45,Citation46 larger scale trials generally fail to show significant improvements in hyperglycemia and diabetic complications.Citation47,Citation48 ALA could represent a superior treatment because it has unique properties as an antioxidant and insulin mimetic.Citation14,Citation22,Citation30 Unlike other antioxidants, ALA is amphiphilic, allowing action in aqueous and lipid media.Citation30 Thus, the positive effects of ALA on DSPN could reflect enhancement of its known role as a cofactor in mitochondrial reactions, but also in other systemic processes. Through downstream scavenging by DHLA and antioxidant recycling, ALA could initiate a cascade of events that continues to provide benefits long after its metabolism.Citation14,Citation22,Citation30 Beyond its role as an antioxidant, ALA could also help mitigate complications of DM by improving insulin sensitivity and glucose disposal.Citation14,Citation22,Citation30 Future studies should investigate optimal combinations of antidiabetic therapies and ALA.
Conclusion
Treatment with ALA 600 mg iv daily for 3 weeks represents a well-tolerated and effective therapy for DSPN. Similarly, an oral dose of 600 mg daily administered for up to 5 weeks could offer benefits in symptoms and signs of DSPN without significant side effects. Whereas a single study using sequential parenteral and oral therapy failed to show a significant effect, the preponderance of evidence supports the use of ALA in treating the symptoms and signs of DSPN. Further randomized, double-blind, placebo-controlled trials of larger scale and longer duration are necessary to strengthen existing data and provide greater insight into the long-term efficacy of ALA.
Disclosure
The authors report no conflicts of interest in this work.
References
- ShawJESicreeRAZimmetPZGlobal estimates of the prevalence of diabetes for 2010 and 2030Diabetes Res Clin Pract20108741419896746
- RutkoveSBA 52-year-old woman with disabling peripheral neuropathy: review of diabetic polyneuropathyJAMA20093021451145819738078
- TraceyJADyckJBThe spectrum of diabetic neuropathiesPhys Med Rehabil Clin N Am200819
- SugimotoKMurakawaYSimaAFDiabetic neuropathy – a continuing enigmaDiabetes Metab Res Rev20001640843311114101
- DyckPJKratzKMKarnesJLThe prevalence by staged severity of various types of diabetic neuropathy, retinopathy, and nephropathy in a population-based cohort: the Rochester Diabetic Neuropathy StudyNeurology1993438178248469345
- GoreMBrandenburgNDukesEPain severity in diabetic peripheral neuropathy is associated with patient functioning, symptom levels of anxiety and depression, and sleepJ Pain Symp Manage200530374385
- GoreMBrandenburgNAHoffmanDLBurden of illness in painful diabetic peripheral neuropathy: the patients’ perspectivesJ Pain2006789290017157775
- GalerBSGianasAJensenMPPainful diabetic polyneuropathy: epidemiology, pain description, and quality of lifeDiabetes Res Clin Pract20004712312810670912
- McDermottAMToelleTRRowbothamDJThe burden of neuropathic pain: results from a cross-sectional surveyEur J Pain20061012713516310716
- AbbottCAVileikyteLWilliamsonSMulticenter study of the incidence of and predictive risk factors for diabetic neuropathic foot ulcerationDiabetes Care199821107110759653597
- CoppiniDVBotwellPAWengCShowing neuropathy is related to increased mortality in diabetic patients – a survival analysis using an accelerated failure time modelJ Clin Epidemiol20005351952310812325
- VallianouNEvangelopoulosAKoutalasPAlpha-lipoic acid and diabetic neuropathyRev Diabet Stud2009623023620043035
- BaydasGDonderEKilibozMNeuroprotection by alpha-lipoic acid in streptozotocin-induced diabetesBiochemistry (Mosc)2004691001100515521814
- PackerLKraemerKRimbachGMolecular aspects of lipoic acid in the prevention of diabetes complicationsNutrition20011788889511684397
- ArgoffCEBackonjaM-MBelgradeMConsensus Guidelines: treatment planning and optionsMayo Clin Proc2006814 SupplS122516608049
- KuritzkyLManaging diabetic peripheral neuropathic pain in primary careJ Fam Pract2010595 SupplS152220544053
- The Diabetes Control and Complications Trial Research GroupThe effect of intensive diabetes therapy on the development and progression of neuropathyAnn Intern Med19951225615687887548
- AmthorK-FDahl-JorgensenKBergTJThe effect of 8 years of strict glycaemic control on peripheral nerve function in IDDM patients: the Oslo StudyDiabetologica199437579584
- ZieglerDPainful diabetic neuropathy: treatment and future aspectsDiabetes Metab Res Rev200824Suppl 1S525718395890
- AmetovASBarinovADyckPJThe sensory symptoms of diabetic polyneuropathy are improved with alpha-lipoic acid: the SYDNEY trialDiabetes Care20032677077612610036
- SnellEEStrongFMPetersonWHGrowth factors for bacteria: Fractionation and properties of an accessory factor for lactic acid bacteriaBiochem J1937311789179916746518
- PohZXGohKPA current update on the use of alpha lipoic acid in the management of type 2 diabetes mellitusEndocr Metab Immune Disord Drug Targets2009939239819601918
- ReedLJDeBuskBGGunsalusICHornbergerCSJrCrystalline alpha lipoic acid; acetalytic agent associated with pyruvate dehydrogenaseScience1951114939414854913
- ReedLJThe chemistry and function of lipoic acidAdv Enzymol Relat Subj Biochem19571831934713444113
- PackerLTritschlerHJWesselKNeuroprotection by the metabolic antioxidant alpha-lipoic acidFree Radic Biol Med1997223593788958163
- DimpfelWSpulerMPierauFKThioctic acid induces dose-dependent sprouting of neurites in cultured rat neuroblastoma cellsDev Pharmacol Ther1990141931992114274
- NickanderKKMcPheeBRLowPAAlpha-lipoic acid: antioxidant potency against lipid peroxidation of neural tissues in vitro and implications for diabetic neuropathyFree Radic Biol Med1996216316398891666
- NagamatsuMNickanderKKSchmelzerJDLipoic acid improves nerve blood flow, reduces oxidative stress, and improves distal nerve conduction in experimental diabetic neuropathyDiabetes Care199518116011677587852
- ShayKPMoreauRFSmithEJAlpha-lipoic acid as a dietary supplement: molecular mechanisms and therapeutic potentialBiochim Biophys Acta200917901149116019664690
- SinghUJialalIAlpha-lipoic acid supplementation and diabetesNutr Rev20086664665719019027
- Breithaupt-GroglerKNiebchGSchneiderEDose-proportionality of oral thioctic acid-coincidence of assessments via pooled plasma and individual dataEur J Pharm Sci19998576510072479
- MijnhoutGSAlkhalafAKleefstraNAlpha lipoic acid: a new treatment for neuropathic pain in patients with diabetesNeth J Med20106815816220421656
- Ltd. PMPriceMe – Online Shopping and Price Comparison New Zealand2011 http://www.priceme.co.nz/search.aspx?q=alpha+lipoic+acidAccessed April 24, 2011
- ZieglerDAmetovABarinovAOral treatment with alpha-lipoic acid improves symptomatic diabetic polyneuropathy: the SYDNEY 2 trialDiabetes Care2006292365237017065669
- RuhnauKJMeissnerHPFinnJREffects of 3-week oral treatment with the antioxidant thioctic acid (alpha-lipoic acid) in symptomatic diabetic polyneuropathyDiabet Med1999161040104310656234
- ZieglerDHanefeldMRuhnauKJTreatment of symptomatic diabetic polyneuropathy with the antioxidant alpha-lipoic acid: a 7-month multicenter randomized controlled trial (ALADIN III Study). ALADIN III Study Group. Alpha-Lipoic Acid in Diabetic NeuropathyDiabetes Care1999221296130110480774
- ZieglerDHanefeldMRuhnauKJTreatment of symptomatic diabetic peripheral neuropathy with the anti-oxidant alpha-lipoic acid. A 3-week multicentre randomized controlled trial (ALADIN Study)Diabetologia199538142514338786016
- TangJWingerchukDMCrumBAAlpha-lipoic acid may improve symptomatic diabetic polyneuropathyNeurologist20071316416717495764
- DyckPJDetection, characterization, and staging of polyneuropathy: assessed in diabeticsMuscle Nerve19881121323277049
- ZieglerDNowakHKemlplerPTreatment of symptomatic diabetic polyneuropathy with the antioxidant alpha-lipoic acid: a metaanalysisDiabetes200421114121
- BiewengaGHaenenGRBastAThe role of lipoic acid in the treatment of diabetic polyneuropathyDrug Metab Rev199729102510549421684
- ReljanovicMReichelGRettKTreatment of diabetic polyneuropathy with the antioxidant thioctic acid (alpha-lipoic acid): a two year multicenter randomized double-blind placebo-controlled trial (ALADIN II). Alpha Lipoic Acid in Diabetic NeuropathyFree Radic Res19993117117910499773
- ZieglerDPainful diabetic neuropathy: advantage of novel drugs over old drugs?Diabetes Care200932Suppl 2S41441919875591
- RuessmannHJSwitching from pathogenetic treatment with alpha-lipoic acid to gabapentin and other analgesics in painful diabetic neuropathy: a real-world study in outpatientsJ Diabetes Complications20092317417718403218
- FarvidMSHomayouniFAmiriZImproving neuropathy scores in type 2 diabetic patients using micronutrients supplementationDiabetes Res Clin Pract.2011 [Epub ahead of print]
- TutuncuNBBayraktarMVarliKReversal of defective nerve conduction with vitamin E supplementation in type 2 diabetes: a preliminary studyDiabetes Care199821191519189802743
- SuksomboonNPoolsupNSinprasertSEffects of vitamin E supplementation on glycaemic control in type 2 diabetes: systematic review of randomized controlled trialsJ Clin Pharm Ther201136536321198720
- ScottJKingGOxidative stress and antioxidant treatment in diabetesAnn N York Acad Sci20041031204213