Abstract
Background
Pressure ulcers (PUs) in the sacral region can be a complication of surgical procedures performed in the lithotomy position. Previous reports have noted a difference between men and women in PU development related to the supine position, and body weight and body mass index (BMI) have been also described as known risk factors in supine position-related PU development. The BIG-MAT® system is a noninvasive pressure distribution measurement device used to measure external pressure (EP). We used this system to investigate the relationship between EP to the sacral region in the lithotomy position and selected physical characteristics.
Methods
We recruited 21 young, healthy volunteers (11 men and 10 women, aged 21.4±0.5 years). Using the BIG-MAT system, we measured four types of EP to the sacral region: box pressure, peak box pressure, contact pressure, and peak contact pressure. We analyzed the relationships between these dynamic parameters and physical characteristics of the participants.
Results
There were no differences between men and women in the four types of EP, and no significant differences related to the participants’ height, weight, or BMI.
Conclusion
An individual’s height, weight, and BMI may not contribute to the risk of inducing lithotomy position-related PUs in the sacral region. The noninvasive pressure distribution measurement system BIG-MAT for patients in the lithotomy position during surgery could become a significant device when estimating EP at the sacral region.
Introduction
Pressure ulcers (PUs) are localized injuries to the skin and underlying tissue that generally occur over a bony prominence as a result of external pressure (EP) either alone or in combination with shear forces and friction. PUs are also known as pressure sores, bedsores, and decubitus ulcers. PUs develop when a persisting EP on bony prominences obstructs healthy capillary flow, leading to tissue necrosis.Citation1 Mild EP sores may be experienced by healthy individuals who are restrained over time in a single position. Supine position-related PUs most commonly develop in individuals who are unable to move about, such as those who are bedridden. The most common location for PUs is the sacral region,Citation2 reported to be the site of 22%Citation3 or 38%Citation4 of all PUs.
Patients who undergo prolonged surgical procedures are immobilized for long periods and are therefore at risk of developing PUs. The development of PUs has been explored in only a small proportion of surgical patients.Citation5 The lithotomy position is often used to operate on pelvic viscera and the perineum in urologic, colorectal, and gynecologic surgeries. PUs in the sacral region occasionally occur after prolonged surgical procedures performed in this position.Citation6
It is widely believed that a number of factors can influence the tolerance of skin to EP, thereby increasing the risk of supine position-related PU development, and so, knowing a patient’s physical characteristics is important. A study has reported that a difference exists between men and women in PU development, and low weight is considered to be a significant and distinct risk factor.Citation7 Indeed, there is a higher prevalence of PUs not only in patients with low weight and low body mass index (BMI), but also in overweight patients.Citation8 It has been reported that obese patients are at a higher risk of developing serious PUs than nonobese patients.Citation9 However, it remains unclear why only certain patients develop PUs. Unfortunately, no published studies are available on the impact of sex and physical characteristics on PUs in patients in the lithotomy position. Therefore, further studies in this field are needed to expand the current knowledge base. We hypothesized that lithotomy position-related PUs are induced by patients’ physical characteristics.
Major preventive interventions consist of removing or redistributing the pressure-sensitive areas of the body. Pressure relief is known to be the single most important factor in the prevention of PUs.Citation5 The pressure distribution measurement system BIG-MAT® (Nitta Corp., Osaka, Japan) is a noninvasive method for measuring EP that was designed for industrial applications.Citation10 In our previous studies, we have used the BIG-MAT system to measure the EP in fibular regions to investigate the cause of peroneal nerve paralysisCitation11,Citation12 and in the calf region to investigate the cause of well leg compartment syndromeCitation13 associated with the lithotomy position.
In this study, we used the BIG-MAT system to investigate relationship between the EP applied to the sacral region with participants in the lithotomy position and a series of physical characteristics. The aim of this study was to identify potential risk factors for lithotomy position-related PUs in the sacral region in order to suggest prevention strategies.
Methods
This study was approved by the Ethics Committee of Okayama Prefectural University (approval No 307). We recruited 21 young, healthy university students (11 men and 10 women, aged 21–22 years) as volunteers, and written informed consent was obtained from the participants before starting the study including publication of images and data. We measured the height, weight, and BMI of each participant.
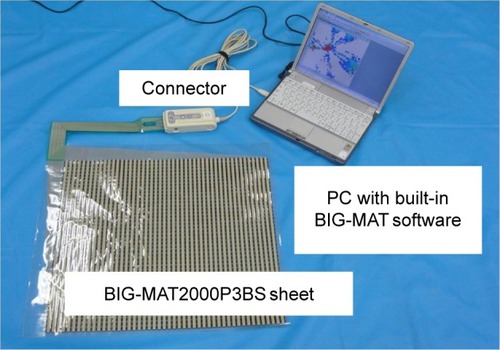
The BIG-MAT system comprises a pressure distribution measurement sheet with 2,112 (44×48) sensors (BIG-MAT2000P3BS®; dimensions L 440, W 480, D 0.4 mm), a sensor connector, and a personal computer (PC) with built-in BIG-MAT software (). The system was calibrated by careful placement of a 25 kg concrete block.
Figure 1 BIG-MAT® pressure distribution measurement system.
Abbreviation: PC, personal computer.
The BIG-MAT2000P3BS sheet was placed on the mattress of an electric operating table class IB® (Takara Belmont Corp., Osaka, Japan). The 3 cm thick mattress was made from flexible polyurethane foam in a single-layer structure. During measurements, the participant was asked to lie on the table in the lithotomy position (). Both knees and lower legs were placed on a knee-crutch-type leg holder (KCLH) system Knee Crutch® (Takara Belmont Corp.). By using the angle gauge, both hip joints were flexed at 90° from the trunk, externally rotated at 40° from the midline, and abducted at 20°; both knee joints were flexed at 90° until both lower legs were parallel to the table surface.Citation14 After having been in the lithotomy position for 5 minutes, the participants remained in the same position for an additional minute while the measurements were being performed. The participants were kept awake throughout.
Figure 2 Lithotomy position.

We measured and recorded the EP distribution at the sacral region using the BIG-MAT system in the neutral state. Digital measurement values were converted to pressure information by the software, which displayed two-dimensional, visually understandable squares for each of the 2,112 sensor cells. Outputs from all sensor cells were also displayed as a number in the range 0–255. Changes in pressure values were consecutively recorded, and chronological changes were saved as movie files on the PC. We recorded 100 pressure distribution views for each participant, followed by measurement of the pressure distribution for the BIG-MAT2000P3BS sheet.
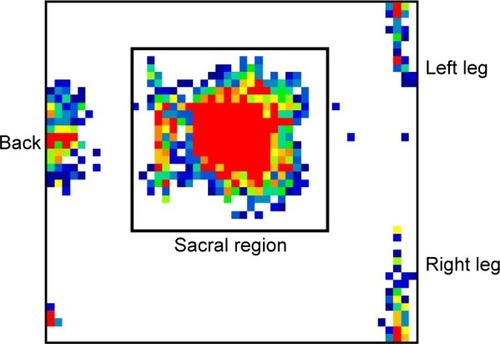
shows a representative view of the pressure distribution. We selected a square area of the display (the box) corresponding to the sacral region for analysis, and evaluated the total force on the sensor cells within the box, and four measures of EP: the box pressure (BP), peak box pressure (PBP), contact pressure (CP), and peak contact pressure (PCP). BP represented the mean pressure on the sensor cells inside the box, which was equal to the total force applied in the box divided by the total area of the box. PBP represented the mean pressure on 2×2 loaded sensor cells that corresponded with the highest pressure within the box (peak area), which was equal to the total force in these four squares divided by the peak area. CP represented the mean pressure on the loaded sensor cells inside the box, which was equal to the total force divided by the area covered by the loaded sensor cell. PCP represented the mean pressure on the loaded sensor cells within the peak area, which was equal to the total force in the four squares divided by the loaded sensor cell area within the peak area.
Figure 3 Representative view of the pressure distribution at the surface of the sacral region with the participant in the lithotomy position.
Analyses were performed using Excel 2013® (Microsoft Corp., Redmond, WA, USA) and Deltagraph 5.4.5v J® (Deltapoint Inc., Monterey, CA, USA). BMI was calculated as the participant’s weight (kg) divided by the square of their height (m). Values were expressed as mean ± standard deviation. Unpaired Student’s t-tests were used for statistical comparisons between the men and women. Simple linear regression analyses were performed to determine correlations between the total force, BP, PBP, CP, and PCP, and participant-specific physical characteristics, such as sex, height, weight, and BMI. A P-value of <0.05 was considered to be significant.
Results
The age, sex, height, weight, and BMI of the 21 volunteers are shown in . There were no sex differences in the total force, BP, PBP, CP, and PCP on the sacral region (). No significant linear correlations were observed between the total force, BP, PBP, CP, or PCP and the participants’ height (P=0.76, 0.47, 0.67, 0.28, and 0.67, respectively), weight (P=0.58, 0.39, 0.93, 0.23, and 0.93, respectively), or BMI (P=0.21, 0.51, 0.63, 0.40, and 0.63, respectively).
Table 1 Participant characteristics
Table 2 Total force and the four types of external pressure on the sacral region with participants lying in the lithotomy position
Discussion
The primary novel finding of this study was that there were no sex differences in the four types of EP measured using the BIG-MAT system in the lithotomy position. Furthermore, there were no significant correlations between the measured EPs and the participants’ height, weight, or BMI.
Capillary blood pressure
EP applied over an area of the body, especially over bony prominences, can lead to obstruction of the capillary vessels. This deprives tissues of oxygen and nutrients, causing ischemia (deficiency of blood in a particular area), hypoxia (inadequate amount of oxygen available to the cells), edema, inflammation, and, ultimately, necrosis and ulcer formation. Thus, PUs are caused by EP applied to soft tissue that results in completely or partially obstructed blood flow to the tissue.
Excessive pressure for a period of time may result in the development of PUs. Previous studies have reported that capillary blood pressure was 32 mmHg with microinjection in human skinCitation15 and 25 mmHg in canine muscle.Citation16 Therefore, it is generally accepted that healthy capillary pressure ranges from 20 to 40 mmHg, with 32 mmHg being considered the average.Citation1 If the EP exceeds 32 mmHg, it will induce occlusion of the capillary vessel, resulting in ischemic injury. It has been recommended that EP loading to the skin surface be kept below 32 mmHg and as low as possible.Citation17 In addition, when a person is lying down, EPs may approach the diastolic blood pressure under bony prominences.Citation18 Tissue interface pressure, that is, the force per unit area that acts perpendicularly between the body and the patient’s support surface at bony prominences, is extremely high near the sacral area in patients who undergo prolonged surgical procedures. In our present results, the mean value of PCP on the sacral region with the participants in the lithotomy position was 93.3 mmHg. This value was significantly >32 mmHg (P<0.001) and probably the diastolic blood pressure and was similar to the value of EP measured physiologically in our previous studies.Citation11–Citation13 From this result, it would be expected that operation in the lithotomy position can cause position-related PUs.
Sex
We found no sex difference in the total force and the four types of EP. In a previous study, logistic regression analysis demonstrated that sex did not predict PUs on admission to university-operated tertiary care hospitals, medical centers, and skilled nursing homes.Citation19 Studies reported that sex was not significantly associated with the presence of PUs in university teaching hospitalsCitation20 and intensive care unit (ICU).Citation21 According to logistic regression analysis, sex was not a significant predictor of PUs in hospital settings.Citation22 Thus, sex difference may not affect EP on the sacral region in the lithotomy position.
However, it has been reported that people older than 65 years have the risk for PUs, with a prevalence of 37 and 52 per 100,000 population for men and women, respectively.Citation2 Unadjusted analyses from a population-based retrospective cohort study revealed statistically significant associations with sex of the incidence of hospital-acquired PUs.Citation23 In univariate and multivariate analyses, the female sex was associated with hospital-acquired PUs.Citation24 Postoperatively, more women than men developed PUs, and female sex was one risk factor identified in multiple stepwise regression analyses.Citation25 One reason for the sex difference may be attributed to soft tissue quality; that is, body composition, such as tissue mass and area, frequently differs between men and women. Generally, men are taller and heavier than women. Body muscle percentage, leg bone-free lean mass, calf muscle cross-sectional area, and calf muscle density are greater in men than in women, whereas the opposite is true for body fat percentage, leg fat mass, calf fat cross-sectional area, and calf fat density.Citation26
Body mass index
In the present study, there were no significant differences associated with the participants’ weight or BMI for the total force or the four types of EP. A study reported that BMI was not significant in ICU patients with PUs.Citation27
However, weight and BMI are widely considered to be predictive factors of supine position-related PU development. Unadjusted analyses have revealed statistically significant associations between BMI and the incidence of hospital-acquired PUs.Citation23 In multivariate analyses, BMI was associated with the presence of hospital-acquired PUs.Citation24 In logistic regression, morbid obesity (BMI ≥40 kg/m2) was associated with PUs in critically injured blunt trauma patients.Citation28
Conversely, being underweight was a significant and distinct factor in PU development in a neurologic ICU.Citation7 The postoperative patients who developed PUs weighed significantly less and had a lower BMI.Citation25 Thin patients were at higher risk of PUs in the sacral region than those with normal weight and obese patients.Citation29 Individuals who were underweight had a higher risk of developing PUs in nursing home.Citation30 According to logistic regression analysis, low BMI was a significant predictor of PUs in hospital settings.Citation22
An international PU prevalence survey showed that there was a higher prevalence of PUs in patients with low BMI and in those with low or high body weight; furthermore, one in ten patients with PUs was extremely obese.Citation8 It has been reported that the incidence of PUs in intensive care patients who were underweight, normal weight, obese, and extremely obese was 8.6%, 5.5%, 2.8%, and 9.9%, respectively.Citation31
In the present study, the mean BMI was 21.4±3.0 kg/m2 with limited variation. It may be clear that the more an individual weighs, the greater the force that would be exerted; however, whether the peak area would increase enough to compensate for an increase in pressure seems unlikely. Future studies should investigate the relationship between PUs and a large range of BMI, including underweight and overweight participants, using curve-fitting with various functions. This relationship remains to be proven by future research; such research would help quantify the potential risk associated with metabolic disorders in slim and obese individuals.
Position
Different positions, such as the supine and lithotomy positions, may result in different contact areas and external loading at various body locations. Muscle and fat tissue loading at the sacral region under bony prominences in the lithotomy position will be substantially greater than that when the patient is lying down. For some immobile patients, the onset of PUs is likely to occur sooner when maintaining a sitting posture than when lying down.
In the operating room, the patient’s body is generally placed on a specific soft mattress spread over the flat electric operating table. The probability of developing PUs is dependent on the pad and operating table mattress.Citation32 The mattress is useful for patients who are at moderate to high risk of developing PUs. Some pressure-redistribution overlays significantly decrease the postoperative incidence of PUs in surgical patients.Citation6 EP to the sacral region in the lithotomy position is reduced by the decrease in loading from using the KCLH system. Therefore, sex and weight differences in the EP at a body location may depend on the contact area and external loading.
Study limitations
This study has some limitations. First, we selected BP, PBP, CP, and PCP as representative EPs when using the BIG-MAT system, but we were unable to gather clear evidence on the correlations between these EPs and the actual perfusion pressure within the capillary vessels. Therefore, in future, we will need to obtain additional data on the correlations between perfusion pressure and the EPs measured using the BIG-MAT system.
Second, some cases of PUs occur with operations under general anesthesia. General anesthetics lower blood pressure, that is, cause hypotension, which may compromise perfusion in loaded tissues; patients undergoing prolonged surgeries are considered at a high risk of developing PUs. When a patient is conscious, prolonged time spent in a specific position that causes skin and muscle compression gradually results in discomfort. Under anesthesia, patients are unconscious, do not experience discomfort, and are unable to control their position. Therefore, we should measure EPs in participants with the use of sedation, analgesia, and muscle relaxant.
Third, risk factors of PU development are protein–calorie malnutrition, skin wetness caused by sweating or incontinence, diseases such as arteriosclerosis that reduce blood flow to the skin, or diseases that reduce sensation in the skin, such as paralysis or neuropathy. A report showed that the following risk factors may play a role in PU development in the ICU: fecal incontinence and diarrhea, low preoperative protein and albumin concentrations, disturbed sensory perception, moisture of the skin, impaired circulation, use of inotropic drugs, diabetes mellitus, the patient being too unstable to turn, decreased mobility, and high acute physiology and chronic health evaluation (APACHE) II score.Citation33 Furthermore, reduced mobility, urinary incontinence, cognitive impairment, low serum albumin, and length of stay,Citation20 and infection, age, length of stay, and total Braden score were significantly associated with the presence of PUs,Citation21 and older age, Caucasian race, and lower Braden Scale scores were predictors of PUs.Citation19 Patients aged 65 years and older were at the highest risk.Citation2 Scores on the Braden Scale at the time of admission, number of vasopressors, occurrence of multiple surgeries during admission, and risk of mortality were significant predictors of PUs in hospital settings.Citation22 The Braden Scale is composed of six broad clinical categories: sensory perception, moisture, activity, mobility, nutrition, and friction and shear, with a score of 18 or less indicating an increased risk of developing PUs.Citation1 These physiologic and pathologic risk factors place the patients at risk because of impairment of the microcirculatory system. In the present study, the participants were young, healthy adult volunteers with limited BMI. Future studies should include participants who have not only wide ranges of age and BMI, but also pathologic conditions associated with increased risks of reduced blood flow and PU development in the sacral region during surgeries.
Fourth, the duration of surgery is a risk factor for the development of PUs.Citation22,Citation33 PUs in subdermal tissues under bony prominences are very likely to occur between the first hour and 4–6 hours after sustained loading.Citation34 PUs can also occur within 2–6 hours. The median operative time for patients developing PUs was 4.48Citation35 and 4.6 hours.Citation6 Combined with a prolonged surgical time, the lithotomy position may cause PUs. The duration of surgery should, therefore, be as short as possible. In future, we should measure EPs in participants over a long period.
Finally, because the BIG-MAT system is not currently approved for clinical use as a medical instrument, it can only be used in clinical studies with the approval of the relevant ethics committees.
Conclusion
Using the BIG-MAT system, we measured four types of EP on the sacral region for participants lying in the lithotomy position. There were no sex-related differences in the EPs, or any significant correlations between the EPs and the participants’ height, weight, or BMI. Thus, patients’ height, weight, and BMI may not contribute to their risk of developing lithotomy position-related PUs in the sacral region. The noninvasive pressure distribution measurement system BIG-MAT for patients in the lithotomy position during operation could become a significant device to estimate EP at the sacral region.
Acknowledgments
The authors thank the students of Okayama Prefectural University who participated as volunteers in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- LyderCHPressure ulcer prevention and managementJAMA2003289222322612517234
- KrögerKNiebelWMaierIStausbergJGerberVSchwarzkopfAPrevalence of pressure ulcers in hospitalized patients in Germany in 2005: data from the Federal Statistical OfficeGerontology200955328128719018126
- GroeneveldAAndersonMAllenSThe prevalence of pressure ulcers in a tertiary care pediatric and adult hospitalJ Wound Ostomy Continence Nurs200431310812015867739
- MeehanMNational pressure ulcer prevalence surveyAdv Wound Care19947327303436387827737
- StottsNARisk of pressure ulcer development in surgical patients: a review of the literatureAdv Wound Care199912312713610655792
- PhamBTeagueLMahoneyJSupport surfaces for intraoperative prevention of pressure ulcers in patients undergoing surgery: a cost-effectiveness analysisSurgery2011150112213221683861
- FifeCOttoGCapsutoEGIncidence of pressure ulcers in a neurologic intensive care unitCrit Care Med200129228329011246307
- VanGilderCMacFarlaneGMeyerSLachenbruchCBody mass index, weight, and pressure ulcer prevalence: an analysis of the 2006–2007 International Pressure Ulcer Prevalence SurveysJ Nurs Care Qual200924212713519287251
- BaughNZuelzerHMeadorJBlankenshipJWound wise: wounds in surgical patients who are obeseAm J Nurs200710764050
- SatoSMizumaMKawateNKasaiFWatanabeHEvaluation of sit-to-stand motion using a pressure distribution measurement system – effect of differences in seat hardness on sit-to-stand motionDisabil Rehabil Assist Technol20116429029820923319
- MizunoJNambaCTakahashiTMeasurement of external pressure of peroneal nerve tract coming in contact with lithotomy leg holders using pressure distribution measurement system BIG-MAT®Masui201463101167117125693355
- MizunoJTakahashiTFactors that increase external pressure to the fibular head region, but not medial region, during use of a knee-crutch/leg-holder system in the lithotomy positionTher Clin Risk Manag20151125526125733841
- MizunoJTakahashiTMale sex, height, weight, and body mass index can increase external pressure to calf region using knee-crutch-type leg holder system in lithotomy positionTher Clin Risk Manag20161230531226955278
- LeeJWCassorlaLLithotomy, specific positions, patient positioning and associated risksMillerRDPardoMCJrBasics of Anesthesia6th edPhiladelphiaElsevier Saunders2011304305
- LandisEMMicro-injection studies of capillary blood pressure in human skinHeart193015209228
- HargensARAkesonWHMubarakSJFluid balance within the canine anterolateral compartment and its relationship to compartment syndromesJ Bone Joint Surg Am1978604499505670272
- KrouskopTAGarberSLInterface pressure measurementsJ Enterostomal Ther19901741822380428
- AllenVRyanDWMurrayAMeasurements of interface pressure between body sites and the surfaces of four specialised air mattressesBr J Clin Pract19944831251298031686
- BergstromNBradenBKempMChampagneMRubyEMulti-site study of incidence of pressure ulcers and the relationship between risk level, demographic characteristics, diagnoses, and prescription of preventive interventionsJ Am Geriatr Soc199644122308537586
- GallagherPBarryPHartiganIMcCluskeyPO’ConnorKO’ConnorMPrevalence of pressure ulcers in three university teaching hospitals in IrelandJ Tissue Viability200817410310918378140
- BoursGJDe LaatEHalfensRJLubbersMPrevalence, risk factors and prevention of pressure ulcers in Dutch intensive care units. Results of a cross-sectional surveyIntensive Care Med200127101599160511685300
- TschannenDBatesOTalsmaAGuoYPatient-specific and surgical characteristics in the development of pressure ulcersAm J Crit Care201221211612522381988
- GardinerJCReedPLBonnerJDHaggertyDKHaleDGIncidence of hospital-acquired pressure ulcers – a population-based cohort studyInt Wound J201613580982025469585
- CornielloALMoyseTBatesJKarafaMHollisCAlbertNMPredictors of pressure ulcer development in patients with vascular diseaseJ Vasc Nurs2014322556224944172
- LindgrenMUnossonMKrantzAMEkACPressure ulcer risk factors in patients undergoing surgeryJ Adv Nurs200550660561215926965
- SherkVDThiebaudRSChenZKarabulutMKimSJBembenDAAssociations between pQCT-based fat and muscle area and density and DXA-based total and leg soft tissue mass in healthy women and menJ Musculoskelet Neuronal Interact201414441141725524966
- TerekeciHKucukardaliYTopCOnemYCelikSOktenliCRisk assessment study of the pressure ulcers in intensive care unit patientsEur J Intern Med200920439439719524181
- NewellMABardMRGoettlerCEBody mass index and outcomes in critically injured blunt trauma patients: weighing the impactJ Am Coll Surg200720451056106117481540
- KottnerJGefenALahmannNWeight and pressure ulcer occurrence: a secondary data analysisInt J Nurs Stud201148111339134821601854
- AkcaNKAydinGGümüsKPressure ulcers and their associated factors in nursing home inmatesJ Coll Physicians Surg Pak2015251273025604365
- HyunSLiXVermillionBBody mass index and pressure ulcers: improved predictability of pressure ulcers in intensive care patientsAm J Crit Care201423649450025362673
- NixonJMcElvennyDMasonSBrownJBondSA sequential randomised controlled trial comparing a dry visco-elastic polymer pad and standard operating table mattress in the prevention of post-operative pressure soresInt J Nurs Stud19983541932039801935
- KellerBPWilleJvan RamshorstBvan der WerkenCPressure ulcers in intensive care patients: a review of risks and preventionIntensive Care Med200228101379138812373461
- GefenAHow much time does it take to get a pressure ulcer? Integrated evidence from human, animal, and in vitro studiesOstomy Wound Manage200854102628303518927481
- AronovitchSAIntraoperatively acquired pressure ulcers: are there common risk factors?Ostomy Wound Manage2007532576917293630
