Abstract
Purpose
We evaluated the effects of body mass index (BMI) on thermoregulation in obese patients scheduled to undergo laparoscopic abdominal surgery.
Methods
Sixty patients scheduled to undergo laparoscopic abdominal surgery with no pre-medication were included in the study. The patients were classified into 4 groups according to BMI <24.9, 25–39.9, 40–49.9, and >50. Anesthesia was provided with routine techniques. Tympanic and peripheral temperatures were recorded every 5 minutes starting with the induction of anesthesia. The mean skin temperature (MST), mean body temperature (MBT), vasoconstriction time, and vasoconstriction threshold that triggers core warming were calculated with the following formulas: MST = 0.3 (Tchest + Tarm) + 0.2 (Tthigh + Tcalf). MBT was calculated using the equation 0.64Tcore+0.36Tskin, and vasoconstriction was determined by calculating Tforearm−Tfinger.
Results
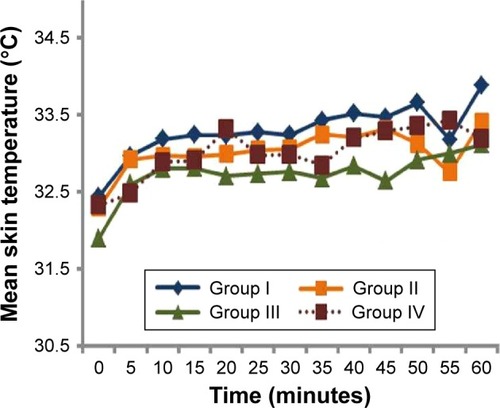
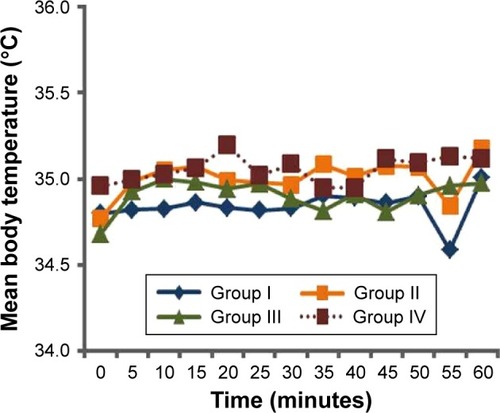
There was no significant difference between the groups in terms of age, gender, duration of operation, and room temperature. Compared to those with BMI <24.9, the tympanic temperature was significantly higher in those with BMI =25–39.9 in the 10th, 15th, 20th, and 50th minutes. In addition, BMI =40–49.9 in the 5th, 10th, 15th, 20th, 25th, 30th, 40th, 45th, 50th, and 55th minutes and BMI >50 in the 5th, 10th, 15th, 20th, 25th, 30th, 50th, and 55th minutes were less than those with BMI <24.9 (P<0.05). There was no significant difference in terms of MST and MBT. Vasoconstriction occurred later, and that vasoconstriction threshold was significantly higher in patients with higher BMIs.
Conclusion
Under anesthesia, the core temperature was protected more easily in obese patients as compared to nonobese patients. Therefore, obesity decreases the negative effects of anesthesia on thermoregulation.
Introduction
As homeothermic beings, humans require a constant core body temperature. Core body temperature is controlled by the temperature regulation system located in the anterior hypothalamus, and daily change is regulated with 0.2°C deviation from normal. While acceptable changes are controlled by the temperature regulation system, significant changes may lead to metabolic dysfunction and even death.Citation1
Besides the fact that anesthetic agents inhibit thermoregulation and cause vasodilation, the coldness of the operation room, cleaning of patients with cold solutions, usage of cold and dry gases for ventilation, irrigation of the surgical field with cold fluids, administration of intravenous cold fluids and blood transfusions, and evaporation from the surgical field have nonnegligible contributions to intraoperative or postoperative hypothermia.Citation2
Recent studies have shown that mild hypothermia (approximately 1°C–2°C) triple the incidence of cardiac events and surgical wound infections, lengthen the duration of hospitalization by 20%, and significantly increase surgical blood loss and related need for blood transfusion.Citation2–Citation4
In obese patients, subcutaneous fat tissue and body surface area increase. Based on its known role in thermogenesis, fat tissue (especially brown fat) may affect the incidence of obesity perioperative hypothermia. For this reason, we evaluated the effects of body mass index (BMI) on thermoregulation in obese patients scheduled to undergo laparoscopic abdominal surgery.
Methods
After approval of the ethics committee (Firat University Ethics Committee on Non-Invasive Research, 13.01.2015/01/04), trial number (ACTRN12615000375550), and written informed consents from patients were obtained, this study was performed at the Firat University Hospital. Sixty patients scheduled to undergo laparoscopic abdominal surgery with no premedication were included in the study. Patients were chosen from cases that took place between 09:00 and 13:00 hours. Patients with high fever, diabetes mellitus, muscle diseases, hypo/hyperthyroidism, Parkinson’s disease, Raynaud’s phenomenon, and history of drug use that would affect body temperature (β-blockers, calcium channel blockers, clonidine, steroids, antiepileptics, and nonsteroidal anti-inflammatory drugs [NSAIDs], benzodiazepines) were not included. Also, patients who underwent a surgery that took <60 minutes or >180 minutes were not included in the study. Patients whose hemodynamic parameters changed >30% during the surgery, or patients who require vasopressors, vasodilators, or blood transfusions were excluded from the study.
The patients were categorized into 4 groups based on their BMI: group I (n=15): BMI <24.9, group II (n=15): BMI =25–39.9, group III (n=15): BMI =40–49.9 (n=15), and group IV: BMI >50 (n=15).
The induction (2 mg/kg propofol and 0.6 mg/kg rocuronium) and maintenance (2% sevoflurane in 50% O2 and remifentanil infusion) of anesthesia were achieved with routine methods. Endotracheal intubation was performed for mechanical ventilation at a target end-tidal carbon dioxide value between 35 and 40 mmHg. At the termination of surgery, sevoflurane was stopped, and 100% O2 inhalation was started. Reversal of neuromuscular blockade was achieved with 0.05 mg/kg neostigmine and 0.01 mg/kg of atropine sulfate. Perioperative heartbeat (bpm), mean arterial pressure and tympanic, chest, arm, ½ medial inner face of forearm, ventral face of the distal phalanx of middle finger, thigh, and calf temperatures were recorded every 5 minutes. Waking up from anesthesia was achieved with routine methods, and patients were taken into the recovery room.
The mean skin temperature (MST), mean body temperature (MBT), vasoconstriction time, and vasoconstriction threshold that triggers core warming were calculated with the following formulas: the MST = 0.3(Tchest + Tarm) + 0.2(Tthigh + Tcalf).Citation5 The MBT was calculated using the equation 0.64Tcore+0.36Tskin, and vasoconstriction was determined by calculating Tforearm−Tfinger =0–4. The core temperature at the moment of vasoconstriction was used to determine the vasoconstriction threshold.Citation6–Citation9
IBM SPSS (Statistical Package for the Social Sciences) version 20 program was used for statistical analyses. The parametric data were taken as mean ± standard deviation and evaluated with variance analysis, after which independent t-test was used for intergroup comparisons. For intragroup comparison, paired sample t-test was used. The American Society of Anesthesiology (ASA) risk classes of the groups were evaluated with chi-square test. A P-value of <0.05 was deemed statistically significant.
Results
There was no significant difference between the groups in terms of age, gender, duration of operation, and room temperature (). When compared with group I, tympanic temperature was significantly higher in the 10th, 15th, 20th, and 50th minutes in group II; in the 5th, 10th, 15th, 20th, 25th, 30th, 40th, 45th, 50th, and 55th minutes in group III; and in the 5th, 10th, 15th, 20th, 25th, 30th, 50th, and 55th minutes in group IV (P<0.05; ). There was no significant difference in terms of MST and MBT ( and ). Vasoconstriction occurred later in groups with higher BMIs (in the 10th, 25th, 15th, and 55th minutes, respectively, according to BMI). Vasoconstriction threshold was significantly higher in patients with higher BMIs (35.75°C, 36.06°C, 36.20°C, and 36.20°C, respectively, from groups I to IV). There was no significant difference between the groups in terms of trembling scores, and there was no significant correlation between BMI and trembling.
Figure 1 Tympanic temperatures of the groups (°C).
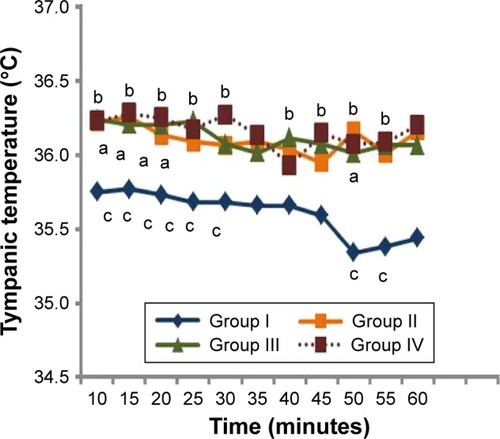
Table 1 Demographic data of patients
Discussion
Anesthesia is one of the practices that tend to create hypothermia by changing the temperature regulation system of the body. Hypothermia development follows a special course during general anesthesia. Core temperature decreases by 1°C–1.5°C during the first hour, and this hypothermia displays a slower and linear decrease during the rest of the time. Consequentially, temperature enters a plateau phase and the core temperature stays the same.Citation2 In this study, we evaluated the effects of anesthesia on thermoregulation in obese patients, and found that tympanic temperature was higher in patients with higher BMIs, while MST and MBT did not change. Interestingly, vasoconstriction occurred later, and that vasoconstriction threshold was higher.
In a study that compared 10 obese patients with BMIs between 30.0 and 34.9 with 10 nonobese women with BMIs between 18.5 and 24.9 who have had abdominal surgeries, and received active heating methods, obesity was found to increase intraoperative core body temperature, decrease intraoperative hypothermia incidence, and cause higher core body temperature during awakening.Citation10
In Kurz et al’s study on 40 patients who had elective colon surgeries, they classified patients according to body fat percentages (10%–24%, 25%–35%, and 36%–50%) and body surface areas (<35, 36–44, and >45 kg/m2). They showed that the decrease in body temperature and amount of redistribution hypothermia was inversely related to body fat percentage and body surface area.Citation11
In a study conducted on 10 obese (fat percentage >25%) and 10 nonobese (<25%) male patients who underwent open abdominal surgery, core temperature, and vasoconstriction thresholds were shown to be higher in the obese patients.Citation12
Savastano et al studied the relationship between adiposity and regional body temperatures in resting and thermoneutral conditions.Citation13 They compared 13 patients with BMIs between 18–25 and 23 patients with BMIs >30. Using an infrared thermography method, they did not find any difference in the core temperature; however, they showed that abdominal skin temperature was lower and finger bed temperature was higher in obese patients. They declared that the huge abdominal subcutaneous fat tissue in the obese constituted a barrier that prevented heat transfer and protected from normothermia. In this study, we found that core temperature decreased in non-obese patients, and normothermia was better protected during anesthesia, which is known to disrupt thermoneutrality.
Boutet and Kassir have emphasized that BMI did not reflect the real metabolic profile of an obese patient.Citation14 Another study showed that skin blood flow effectively shunts thermal insulation caused by the fat tissue, while others stated that BMI was significantly inversely correlated with skin vasodilation dependent on the endothelium.Citation15,Citation16
This study’s major limitation is small sample size as in other studies in the literature.Citation10–Citation13
Conclusion
Obese patients who underwent laparoscopic bariatric surgery under general anesthesia were shown to have better core temperature protection, which was dependent on the degree of obesity. Contrary to all other unwanted effects of obesity in anesthesia practices, it was observed to relieve the negative effects of anesthesia on thermoregulation.
Acknowledgments
This article’s abstract was presented in national congress (48. Turkish Anesthesiology and Reanimation Congress, December 2–6 2015, Antalya, Turkey).
Disclosure
The authors report no conflicts of interest in this work.
References
- SesslerDITemperature monitoringMillerRDMiller AnesthesiaPhiladelphiaChurchill Livingstone201013671389
- SesslerDIPerioperative heat balanceAnesthesiology200092257859610691247
- StevenMFKhaMTLeeAFClinical importance of body temperature in the surgical patientJ Ther Biol2000251–2151155
- ŞahinAAyparÜEffect of amino acid solutions on intraoperative hypothermia and postoperative shiveringActa Anaesthesiol Scand2002461646711903074
- ShanksCAMean skin temperature during anaesthesia: an assessment of formulae in the supine surgical patientBr J Anaesth19754788718761201164
- RamanathanNLA new weighting system for mean surface temperature of the human bodyJ Appl Physiol19641953153314173555
- BurtonACHuman calorimetry: the average temperature of the tissues of the bodyJ Nutr19359261280
- RubinsteinEHSesslerDISkin-surface temperature gradients correlate with fingertip blood flow in humansAnesthesiology19907335415452393139
- SesslerDISkin-temperature gradients are a validated measure of fingertip perfusionEur J Appl Physiol2003893–440140212736848
- FernandesLABrazLGKogaFAComparison of peri-operative core temperature in obese and non-obese patientsAnaesthesia201267121364136923088746
- KurzASesslerDINarztELenhardtRLacknerFMorphometric influences on intraoperative core temperature changesAnesth Analg19958035625677864426
- KasaiTHiroseMMatsukawaTTakamataATanakaYThe vasoconstriction threshold is increased in obese patients during general anaesthesiaActa Anaesthesiol Scand200347558859212699518
- SavastanoDMGorbachAMEdenHSBradySMReynoldsJCYanovskiJAAdiposity and human regional body temperatureAm J Clin Nutr20099051124113119740972
- BoutetCKassirRSleeve gastrectomy and roux-en-Y gastric bypass lead to comparable changes in body composition after adjustment for initial body mass indexObes Surg20162681932193327129803
- de GraafAAFreidigAvan OmmenBHuman thermoregulation and obesityFASEB J200923Suppl 1596602
- CaballeroAAroraSSaouafRMicrovascular and macrovascular reactivity is reduced in subjects at risk for type 2 diabetesDiabetes19994891856186210480619