Abstract
Aim
Patients with type 2 diabetes mellitus (T2DM) have an increased risk of bone fractures. A variable increase in fracture risk has been reported depending on skeletal site, diabetes duration, study design, insulin use, and so on. The present meta-analysis aimed to investigate the association between T2DM with fracture risk and possible risk factors.
Methods
Different databases including PubMed, Institute for Scientific Information, and Scopus were searched up to May 2016. All epidemiologic studies on the association between T2DM and fracture risk were included. The relevant data obtained from these papers were analyzed by a random effects model and publication bias was assessed by funnel plot. All analyses were done by R software (version 3.2.1) and STATA (version 11.1).
Results
Thirty eligible studies were selected for the meta-analysis. We found a statistically significant positive association between T2DM and hip, vertebral, or foot fractures and no association between T2DM and wrist, proximal humerus, or ankle fractures. Overall, T2DM was associated with an increased risk of any fracture (summary relative risk =1.05, 95% confidence interval: 1.04, 1.06) and increased with age, duration of diabetes, and insulin therapy.
Conclusion
Our findings strongly support an association between T2DM and increased risk of overall fracture. These findings emphasize the need for fracture prevention strategies in patients with diabetes.
Introduction
Diabetes is an increasingly prevalent disease, with significant associated morbidity and mortality.Citation1 Type 2 diabetes mellitus (T2DM) is a group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both.Citation1,Citation2 Long-term hyperglycemia and inadequate glycemic control both contribute to the development of diabetic complications, including nephropathy, retinopathy, neuropathy, and macrovascular diseases such as acute coronary syndrome, claudicatio intermittens, and stroke.Citation1–Citation3
Besides micro- or macrovascular long-term complications, T2DM patients also have various skeletal disorders, including osteoporosis and fractures.Citation4 Diabetes could impact the bone through several mechanisms, some of which may have contradictory effects.Citation5 The bone turnover and, thus, the skeletal integrity may also be affected by diabetes, and diabetic bone disease can represent an overlooked complication of diabetes.Citation6 Diabetic osteopathy is characterized by microarchitectural changes that decrease the bone quality and strength, leading to an increased risk of bone fracture in both types of diabetes.Citation2 Patients with T2DM display a unique skeletal phenotype and impaired structural and geometric properties.Citation7
The prevalence of osteoporosis increases dramatically with age.Citation8 T2DM also increases with increasing age, and therefore, diabetes and osteoporosis often coexist in older adults.Citation8–Citation10 Authors present the overview of factors involved in the risk of osteoporosis and fractures in both types of diabetes.Citation1
In T2DM patients, bone mineral density (BMD) seems to be normal to elevated.Citation11 For many years, diabetic patients were not considered to be at risk of osteoporosis, based on reports of their higher BMD compared with healthy individuals. However, later studies revealed that persons with T2DM might be at increased risk for bone fractures, despite having higher BMD.Citation12,Citation13 The risk of bone fractures in patients with diabetes may be unrelated to BMD, and T2DM reduces bone quality rather than BMD.Citation11 These findings suggest that factors other than BMD may be underlying the higher fracture risk observed in diabetes patients. For example, the association of diabetes with fracture risk has differed depending on the location of fracture, sex, age, duration of diabetes, and the effect of diabetes medications.Citation11,Citation14–Citation16 Longer disease duration, the presence of diabetic complications, inadequate glycemic control, insulin use, and increased risk for falls are all reported to increase fracture risk.Citation7 A variable increase in fracture risk has been reported, ranging from onefold to threefold, depending on the risk factors.Citation7,Citation11,Citation14–Citation16
The relationship between T2DM and fracture risk has been the subject of considerable interest over the past years, and several studies have examined the risk of fracture in persons with T2DM.Citation4–Citation17 These studies have demonstrated inconsistent conclusions: reported associations have been positive,Citation18–Citation21 null,Citation15,Citation16,Citation22 or even inverse.Citation23,Citation24 Since a meta-analysis is warranted to clarify the association between T2DM and fracture risk, this study provides a systematic review and meta-analysis of association between T2DM and risk of fracture. We also evaluated possible sources of heterogeneity between studies and the risk factors for fracture among diabetic patients, including age, body mass index (BMI), sex, fracture site, duration of diabetes, the effect of diabetes medications, and so on.
Methods
Search strategy
We performed a literature search in reputable databases including PubMed/Medline, Scopus, and Institute for Scientific Information Web of Knowledge from 1980 to May 2016 using special keywords such as “diabetes mellitus”, “type 2 diabetes mellitus”, “glucose”, “insulin”, “fracture”, “bone”, “osteoporosis”, “bone mineral density”, and “risk factors”. In the initial search, all articles that had these keywords in their titles or abstracts were chosen, and other unrelated articles were eliminated. The obtained articles were rechecked by the other expert authors. We also searched bibliographies of retrieved articles for additional references. The human researches only were highlighted. To decrease bias, two authors performed the search, selection of papers, and extracting data of articles independently.
Inclusion and exclusion criteria
All epidemiologic studies presenting cohort and case–control studies on the association between T2DM and fracture risk (low-trauma hip, distal forearm, proximal humerus, ankle, foot, nonvertebral, or vertebral fracture) were considered. Studies were excluded: if they were performed on individuals with type 1 diabetes mellitus or impaired glucose tolerance, if they did not provide data that allowed calculation of standard errors for effect estimates, if they were meta-analyses and systematic reviews. We also excluded studies with duplicate citation. When there were multiple publications from the same population or cohort, only data from the most recent report were included. When necessary, authors were contacted for additional information.
Data extraction
For all studies, the following data were extracted: first author’s name, year of publication, country, study design, sample size, age, sex, BMI, follow-up period (for cohort studies), duration of diabetes, diabetes medications, fracture site and number of cases, risk estimates and corresponding confidence intervals (CIs), factors controlled for by matching or multivariable analysis and adjustment for potential confounders. Two of the authors independently reviewed the abstracts and full articles and collected data according to a standard protocol. Discrepancies were resolved in a joint meeting through discussion. The data were entered into data collection forms and then entered in Microsoft Excel.
Data synthesis and analysis
We used the logarithm of the relative risk (RR) with its standard error for the meta-analysis. The method of DerSimonian and Laird was used for extracting summary RR estimates and the corresponding 95% CIs. The Cochran’s Q, meta-regression, and I2 were used as measures of heterogeneity of the studies. Considering the significant heterogeneity of the studies, the random effects model was applied. We conducted a meta-regression analysis with age, BMI, region, sex, fracture site, duration of follow-up (in cohort studies), and duration of diabetes as independent variables and log RR as the dependent variable to assess sources of heterogeneity. Funnel plots and Egger’s test were used to examine the publication bias. Sensitivity analyses were prespecified. Statistical analyses were carried out with using R software (version 3.2.1) and STATA (version 11.1). P-values <0.05 were considered as significant in heterogeneity tests. All statistical tests were two sided.
Results
In the primary search, about 1,200 titles were retrieved and about 203 were considered relevant and screened. In a secondary screening, 91 papers were excluded based on abstract evaluation. Therefore, 112 articles were retained for detailed full-text evaluation. After full-text evaluation, we excluded another 81 articles of these: six were excluded because of overlapping publication, 17 were duplicated articles, 15 were retrospective and review studies, five were meta-analyses, 12 studies were performed on persons with type 1 diabetes mellitus or impaired glucose tolerance, 21 did not provide data that allowed calculation of standard errors for effect estimates, and five reported only crude data that were not adjusted for age. Finally, 30 epidemiologic studies including two case–control and 28 cohort studies on the association between T2DM and fracture risk and possible risk factors, which were published between 1980 and 2016, were selected for the meta-analysis ().Citation15,Citation16,Citation24–Citation51 The characteristics and extracted data from these studies are shown in .
Figure 1 Flowchart of the literature search.
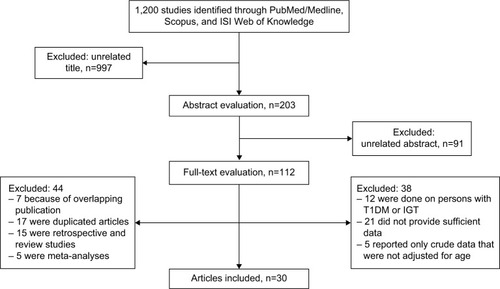
Table 1 The characteristics of the studies entered into the meta-analysis
We included both the case–control studies and the 28 cohort studies in the primary meta-analysis. Due to severe heterogeneity of the reported prevalence (P<0.001), meta-analysis was performed by using a random effects method.
Considering all the included studies, the total number of participants and incident cases of fracture were 5,815,277 and 113,203, respectively.
shows a summary of the RR estimates from the included studies of the association between T2DM and fracture incidence. Fifteen of 30 studies had reported the association between T2DM and hip fracture incidence. We found a statistically significant positive association between T2DM and hip fracture incidence (summary RR =1.20, 95% CI: 1.17–1.23; ). Also, the association between T2DM and fracture of the vertebral (summary RR =1.16, 95% CI: 1.05–1.28) or foot (summary RR =1.37, 95% CI: 1.21–1.54) was statistically significant ().
Figure 2 The results of meta-analysis of the association between type 2 diabetes mellitus and risk of hip fracture.
Abbreviations: CI, confidence interval; ES, effect size.
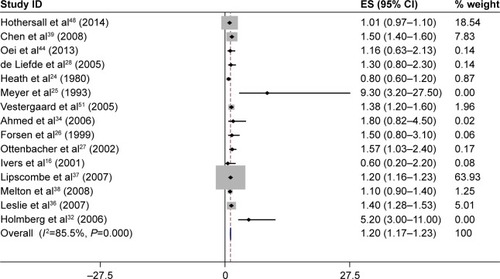
Table 2 Summary relative risk estimates from case–control and cohort studies of the association between type 2 diabetes mellitus and fractures incidence using meta-analysis methods
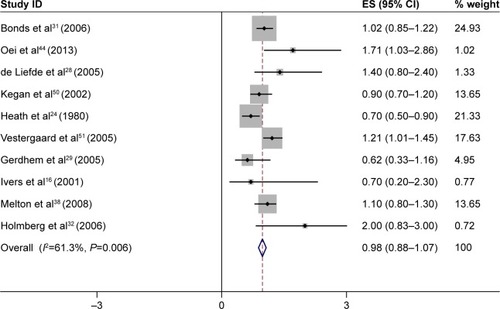
As seen in , there was no significant association between T2DM and wrist fracture incidence. Ten of 30 studies had reported the association between T2DM and wrist fracture incidence, and the summary RR for all 10 studies combined was 0.98 (95% CI: 0.88–1.07; ). Also, we found no association between T2DM and fracture of the proximal humerus (summary RR =1.09, 95% CI: 0.86–1.31) or ankle (summary RR =1.13, 95% CI: 0.95–1.32; ).
Figure 3 The results of meta-analysis of the association between type 2 diabetes mellitus and risk of wrist fracture.
Abbreviations: CI, confidence interval; ES, effect size.
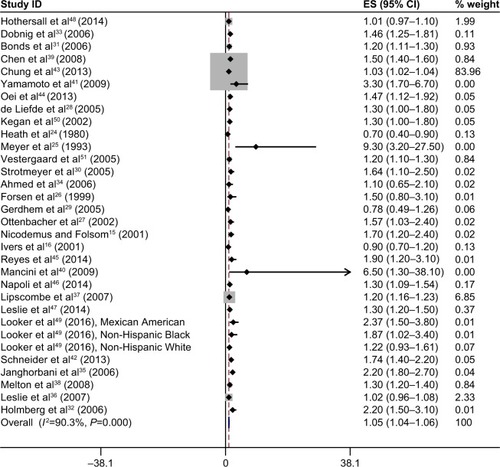
shows the individual study results and the overall summary results for the included studies of T2DM and overall fracture incidence. As observed in the figure, there was a statistically significant positive association between T2DM and overall fracture (summary RR =1.05, 95% CI: 1.04–1.06).
Figure 4 The results of meta-analysis of association between type 2 diabetes mellitus and risk of overall fractures.
Abbreviations: CI, confidence interval; ES, effect size.
We also conducted subgroup meta-analyses for the most important known confounders and for risk factors that have an influence on the association between T2DM and fracture risk. gives the summary RR and P-value estimates from the included studies for incident fracture according to the risk factors.
Table 3 Risk factors for the association between type 2 diabetes and fracture risk
The association of T2DM with fracture risk differed by age, although diabetes was associated with a significantly higher risk of fractures for all age subgroups; the risk of fracture was increased with age (continuous; summary RR =1.10, 95% CI: 1.07–1.13). Also, effect modification was much greater in the oldest subgroup, with progressively less effect modification in younger age subgroups (summary RR age 50–59 years 1.17 [95% CI: 1.15–1.21], age 60–69 years 1.20 [95% CI: 1.10–1.30], age ≥70 years 1.30 [95% CI: 1.21–1.40]); there was heterogeneity among studies by age (P for heterogeneity [Phet] <0.001; ).
The result of our meta-analysis showed increased risk of overall fractures in diabetic men compared with diabetic women (Phet =0.043; ).
For BMI, the estimation of summary was stronger for BMI <30 kg/m2 (summary RR =1.44, 95% CI: 1.24–1.64) than for BMI ≥30 kg/m2 (summary RR =1.30, 95% CI: 1.22–1.37; Phet<0.001; ).
We conducted subgroup meta-analyses by region. Twelve studies were conducted in the USA,Citation15,Citation24,Citation27,Citation28,Citation31,Citation32,Citation36,Citation39,Citation43,Citation47,Citation50,Citation51 three in Canada,Citation37,Citation38,Citation48 11 in Europe,Citation25,Citation26,Citation29,Citation30,Citation33,Citation35,Citation41,Citation45,Citation46,Citation49,Citation52 three in Asia,Citation40,Citation42,Citation44 and two in Australia.Citation16,Citation34 Results were consistent by geographic area (Phet =0.29; ).
The estimation of summary for incident fracture according to duration of diabetes was stronger with 10 or more years of diabetes (summary RR =1.0, 95% CI: 0.93–1.6) than diabetes duration of <10 years (RR =1.19, 95% CI: 1.13–1.26); there was heterogeneity by duration of diabetes (<10 years vs ≥10 years; Phet <0.001; ).
Finally, the estimation of summary was stronger with follow-up durations of <10 years (RR =1.19, 95% CI: 1.16–1.22) than 10 or more years of follow-up (summary RR =1.13, 95% CI: 1.08–1.18; Phet =0.004; ).
The results of meta-analysis of association of T2DM with fracture risk by physical activity showed a significant inverse association between T2DM and fracture (summary RR =0.75, 95% CI: 0.65–0.86) and that physical activity was associated with a decrease risk for fracture incidence in diabetic patients and might be more protective in this regard. We found no significant association between T2DM and fracture incidence by smoking status (summary RR =1.29, 95% CI: 0.92–1.88). Insulin therapy and use of systemic corticosteroids were associated with an increased fracture risk; the summary of estimation was 1.52 (95% CI: 1.42–1.61) for insulin therapy and 1.51 (95% CI: 1.29–1.72) for use of systemic corticosteroids. Also, treatment with thiazolidinediones (TZDs) was not associated with an increase fracture risk (summary RR =0.75, 95% CI: 0.60–0.91; ).
According to the publication bias tests, the effect of bias in these studies was not significant. P-values for Egger’s regression asymmetry test were 0.32. presents the Begg’s funnel plot of the included trials related to the risk of factors in diabetic patients. Regression analysis of this plot indicated no significant asymmetry (P≥0.05) and thus no evidence of bias ().
Figure 5 Begg’s funnel plot for publication bias in the risk difference analysis.
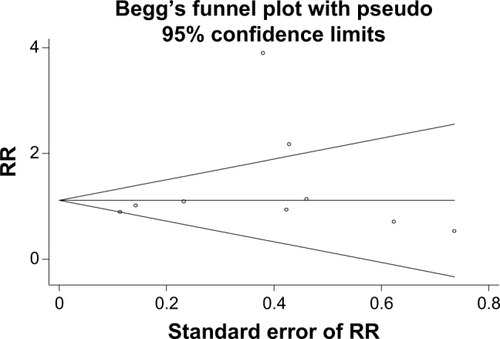
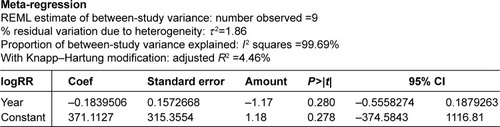
Interpretation of meta-regression showed that there was no significant relationship between the risk factors in diabetic patients and the year of study (P≥0.05; ).
Discussion
Osteoporotic fractures and diabetes mellitus (DM) continue to be important medical, social, and economic concerns to the society. Our study gives an overall picture of the risk of any fracture in people with T2DM. The risks reported from previous studies of people with T2DM vary substantially. In some studies, diabetes was significantly associated with an increased risk for hip fractures,Citation25,Citation27,Citation32,Citation36,Citation37,Citation39,Citation51 wrist fractures,Citation44,Citation51 proximal humerus fractures,Citation38,Citation50 vertebral fractures,Citation31,Citation38,Citation40,Citation41,Citation43 and overall fractures.Citation30–Citation32,Citation38,Citation42,Citation44,Citation47,Citation51 In contrast, other studies have found no association between diabetes with hip fractures,Citation16,Citation24,Citation26,Citation28,Citation34,Citation38,Citation44,Citation48 wrist fractures,Citation16,Citation24,Citation28,Citation29,Citation31,Citation32,Citation38,Citation50 proximal humerus fractures,Citation16,Citation24,Citation32 vertebral fractures,Citation24,Citation29,Citation32,Citation51 or overall fractures.Citation16,Citation29 We found an association between T2DM and overall fracture (summary RR =1.05, 95% CI: 1.04–1.06). These results strongly agreed with previous meta-analysis studies that showed an increase risk of fractures in T2DM patients.Citation11,Citation14 Janghorbani et al, in a meta-analysis of case–control and cohort studies, confirmed a 1.2 (95% CI: 1.01–1.5) RR for any fracture and 1.7 (95% CI: 1.3–2.2) RR for hip fracture in both men and women suffering from T2DM.Citation14 VestergaardCitation11 combined studies up to 2007 in a meta-analysis and concluded that the risk ratio for hip fracture in T2DM was 1.38 (95% CI: 1.25–1.53). The observed differences in RR between the oldest and most recent meta-analyses discussed were small. Thus, the estimation from meta-analyses of fracture RR in T2DM showed a statistically significant positive association between T2DM and fracture incidence.
T2DM and fracture share similar and opposing risk factors. In our effort to identify the variables contributing to the higher risk of fracture among diabetic patients, we found a range of risk factors for fracture that are also associated with diabetes. In accordance with previous studies, some of the risk factors identified were increasing age, sex, BMI, physical activity, smoking status, duration of diabetes, and glycemic control.
The results of our meta-analysis showed that the incidence of fractures increased with age and duration of diabetes. Studies showed that patients’ age and duration of diabetes were negatively correlated with insulin-like growth factor-1 (IGF-1), and serum IGF-1 levels were negatively associated with increased risk of fractures in diabetic patients.Citation52 Thus, the incidence of fractures may increase with age and duration of diabetes in diabetic patients.
We found that diabetic men had an increased risk of overall fractures compared with diabetic women (Phet =0.043). Meta-analysis conducted by Janghorbani et alCitation14 indicated that fracture risk was relatively higher in T2DM men than in T2DM women. The results of these meta-analysis studies could have easily been due to chance, because in these studies, the number of cases in men was relatively small.
Some studies have found that 21%–64% of T2DM men have hypogonadism, with higher prevalence rates in the elderly.Citation53,Citation54 Thus, we can say that the presence of DM may cause hypogonadism and may be one of the risk factors of secondary osteoporosis, especially in elderly men. Furthermore, several studies have shown that the RR of fractures in men is significantly increased with smoking, alcohol consumption, anticonvulsant treatment, physical inactivity, and low free androgen index.Citation55,Citation56
Evidence regarding a direct relation of better glycemic control with reduced risk of fracture is very weak.Citation16 We were not able to evaluate the possible impact of all blood glucose-lowering drugs because of the limitations of the available data. Our findings showed an increased risk of fracture in those using insulin or systemic corticosteroids. There was also no increased risk with TZD use. The use of TZDs has been associated with an increased fracture risk in both T2DM men and women. TZDs could have a negative effect on bone quality, since they suppress the differentiation of mesenchymal stem cells into osteoblasts in favor of differentiation to adipocytes.Citation57–Citation59 Some previous studies have reported an increased risk of fracture in those using insulin.Citation34,Citation38,Citation60,Citation61 This increased fracture risk was most probably due to an increased risk of falls because of hypoglycemic events which may impair the bone quality in the diabetic skeleton and also because insulin is often used in patients with diabetes of longer duration, thus diabetic patients are likely to have long-term negative hyperglycemic effects on bone quality that lead to increased fracture risk.Citation62–Citation64
The mechanisms whereby diabetes increases the fracture risk are not entirely clear. A possible cause of the increased risk of fracture in T2DM is diabetes-related comorbidity, such as diabetic retinopathy, peripheral neuropathy, and cerebral stroke or hypoglycemia, which may increase the risk of falling.Citation14,Citation43,Citation65,Citation66 It has been hypothesized that physiologic changes resulting from chronic hyperglycemia could degrade the bone quality through inhibition of osteocalcin, increased reactive oxygen species, accumulation of advanced glycation end products in bone, or inhibition of IGF-1.Citation67 In addition, other factors related to T2DM, such as the micro-vascular and macrovascular complications, oxidative stress, renal dysfunction, elevated renal calcium loss, and persistent inflammation present in T2DM, may further impair bone health and increase fracture risk.Citation46 It is documented that poor nerve function is a cause of fallsCitation68 and that an increased risk of fractures is associated with DM retinopathy, longer DM duration, and insulin treatment.Citation16 Thus, these DM-related complications increase fracture risk.
The combination of poor bone quality and frequent falls would be expected to increase the risk of fracture independently of BMD.Citation16 In some studies with T2DM women, lower total hip BMD was significantly associated with higher risk of fractures, even after adjustment for multiple covariates.Citation43 In contrast, some studies reported lack of statistical association between BMD and fractures in subjects with T2DM.Citation41 From these observations, the authors concluded that BMD was not sensitive enough to assess the risk of fracture in subjects with T2DM.Citation43 A meta-analysis also showed that T2DM patients had higher hip BMD than non-DM controls, despite an increased risk of hip fracture, suggesting that BMD values may not reflect bone fragility in T2DM.Citation11
It has been hypothesized that the complications of diabetes (peripheral neuropathy, peripheral vascular disease), diabetes treatment (insulin), or both could increase the risk of falls and fractures.Citation69,Citation70
Limitations
Our results have important clinical and public health implications; it will further contribute to the public health burden of any fractures. Also, our meta-analysis had several limitations. In this meta-analysis, we were unable to conduct separate analyses by ethnicity; insufficient available data about association between T2DM and fracture by ethnicity prevented us from the evaluation of such cases. Other limitation is the lack of information on BMD, which could explain part of the observed associations. Thus, it was not possible for us to evaluate the impact of controlling for BMD on the relation between diabetes and fracture risk. Furthermore, some included studies did not enjoy acceptable quality or presented defective quantitative data that could not be included in the meta-analysis. Finally, some studies associated with diabetes and fracture risk were not accessible.
Conclusion
This study gives an overall picture of the risk of all fractures in people with T2DM. Our findings showed a positive association between T2DM and hip fractures, vertebral fractures, and foot fractures. We also found no association between T2DM and wrist fractures, proximal humerus fractures, or ankle fractures. Overall, the results of this meta-analysis strongly support an association between T2DM and increased risk of any fracture. With a worldwide increasing prevalence of diabetes, the contribution of diabetes to the incidence of low-trauma fracture may increase.
In our effort to identify the variables contributing to the higher risk of fracture among diabetic patients, we found a range of risk factors for fracture that are also associated with diabetes. The incidence of fractures increased with age and was higher in T2DM men than in T2DM women. According to the results, the expected rate of BMD loss in bones in diabetics seems to be higher than in nondiabetics. But in some studies, this trend was reversed. Due to limited data on BMI studies, our analysis showed that patients with T2DM have higher BMI and have lesser risk of fracture. Also, elevated RRs are seen in those with longer diabetes duration and in those using insulin and systemic corticosteroids. These findings emphasize the need for developing risk prediction models in order to avoid systematically underestimating the risk of osteoporosis-related fracture in patients with diabetes. Also, our findings emphasize the need for fracture prevention strategies in patients with T2DM.
Acknowledgments
The authors are grateful to the Deputy of Research and Technology, Ilam University of Medical Sciences for their support.
Disclosure
The authors report no conflicts of interest in this work.
References
- JackuliakPPayerJOsteoporosis, fractures, and diabetesInt J Endocrinol2014201482061525050121
- de WaardEAvan GeelTASavelbergHHKosterAGeusensPPvan den BerghJPIncreased fracture risk in patients with type 2 diabetes mellitus: an overview of the underlying mechanisms and the usefulness of imaging modalities and fracture risk assessment toolsMaturitas201479326527425192916
- American Diabetes AssociationDiagnosis and classification of diabetes mellitusDiabetes Care201235Suppl 16471
- SchwartzAVDiabetes mellitus: does it affect bone?Calcif Tissue Int200373651551914517715
- MilczarczykAFranekEOsteoporosis and bone fractures in patients with diabetes mellitusDiabet Dosw i Klin2008826367
- HamannCKirschnerSGuntherKPHofbauerLCBone, sweet bone-osteoporotic fractures in diabetes mellitusNat Rev Endocrinol20128529730522249517
- DedeADTournisSDontasITrovasGType 2 diabetes mellitus and fracture riskMetabolism201463121480149025284729
- van StaaTPDennisonEMLeufkensHGCooperCEpidemiology of fractures in England and WalesBone200129651752211728921
- BlanchardJFLudwigSWajdaAIncidence and prevalence of diabetes in Manitoba, 1986–1991Diabetes Care19961988078118842595
- WildSRoglicGGreenASicreeRKingHGlobal prevalence of diabetes: estimates for the year 2000 and projections for 2030Diabetes Care20042751047105315111519
- VestergaardPDiscrepancies in bone mineral density and fracture risk inpatients with type 1 and type 2 diabetes–a meta-analysisOsteoporos Int200718442744417068657
- SchwartzAVVittinghoffEBauerDCAssociation of BMD and FRAX score with risk of fracture in older adults with type 2 diabetesJAMA2011305212184219221632482
- MaLOeiLJiangLAssociation between bone mineral density and type 2 diabetes mellitus: a meta-analysis of observational studiesEur J Epidemiol201227531933222451239
- JanghorbaniMVan DamRMWillettWCHuFBSystematic review of type 1 and type 2 diabetes mellitus and risk of fractureAm J Epidemiol2007166549550517575306
- NicodemusKKFolsomARIowa Women’s Health StudyType 1 and type 2 diabetes and incident hip fractures in postmenopausal womenDiabetes Care20012471192119711423501
- IversRQCummingRGMitchellPPedutoAJBlue Mountains Eye StudyDiabetes and risk of fracture: the Blue Mountains Eye StudyDiabetes Care20012471198120311423502
- HofbauerLCBrueckCCSinghSKDobnigHOsteoporosis in patients with diabetes mellitusJ Bone Miner Res20072291317132817501667
- KorpelainenRKorpelainenJHeikkinenJVaananenKKeinanen- KiukaanniemiSLifestyle factors are associated with osteoporosis in lean women but not in normal and overweight women: a population-based cohort study of 1,222 womenOsteoporos Int2003141344312577183
- KelseyJLBrownerWSSeeleyDGNevittMCCummingsSRRisk factors for fractures of the distal forearm and proximal humerus. The Study of Osteoporotic Fractures Research GroupAm J Epidemiol199213554774891570814
- MeltonLJ3rdAchenbachSJO’FallonWMKhoslaSSecondary osteoporosis and the risk of distal forearm fractures in men and womenBone200231111912512110424
- VogtMTCauleyJATomainoMMStoneKWilliamsJRHerndonJHDistal radius fractures in older women: a 10-year follow-up study of descriptive characteristics and risk factors. The Study of Osteoporotic FracturesJ Am Geriatr Soc20025019710312028253
- TuominenJTImpivaaraOPuukkaPRonnemaaTBone mineral density in patients with type 1 and type 2 diabetesDiabetes Care19992271196120010388989
- Van DaelePLAStolkRPBurgerHBone density in non-insulin-dependent diabetes mellitusAnn Intern Med199512264094147856988
- HeathH3rdMeltonLJ3rdChuCPDiabetes mellitus and risk of skeletal fractureN Engl J Med1980303105675707402221
- MeyerHETverdalAFalchJARisk factors for hip fracture in middle-aged Norwegian women and menAm J Epidemiol199313711120312118322761
- ForsenLMeyerHEMidthjellKEdnaTHDiabetes mellitus and the incidence of hip fracture: results from the Nord-Trøndelag Health SurveyDiabetologia199942892092510491750
- OttenbacherKJOstirGVPeekMKGoodwinJSMarkidesKSDiabetes mellitus as a risk factor for hip fracture in Mexican-American older adultsJ Gerontol A Biol Sci Med Sci20025710M648M65312242318
- de LiefdeIIvan der KliftMde LaetCEvan DaelePLHofmanAPolsHABone mineral density and fracture risk in type-2 diabetes mellitus: the Rotterdam StudyOsteoporos Int200516121713172015940395
- GerdhemPIsakssonAAkessonKObrantKJIncreased bone density and decreased bone turnover, but no evident alteration of fracture susceptibility in elderly women with diabetes mellitusOsteoporos Int200516121506151215824889
- StrotmeyerESCauleyJASchwartzAVNevittMCResnickHEBauerDCNontraumatic fracture risk with diabetes mellitus and impaired fasting glucose in older white and black adults: the health, aging, and body composition studyArch Intern Med2005165141612161716043679
- BondsDELarsonJCSchwartzAVRisk of fracture in women with type 2 diabetes: the Women’s Health Initiative Observational StudyJ Clin Endocrinol Metab20069193404341016804043
- HolmbergAHJohnellONilssonPMNilssonJBerglundGAkessonKRisk factors for fragility fracture in middle age. A prospective population-based study of 33,000 men and womenOsteoporos Int20061771065107716758143
- DobnigHPiswanger-SolknerJCRothMType 2 diabetes mellitus in nursing home patients: effects on bone turnover, bone mass, and fracture riskJ Clin Endocrinol Metab20069193355336316735485
- AhmedLAJoakimsenRMBerntsenGKFonneboVSchirmerHDiabetes mellitus and the risk of non-vertebral fractures: the Tromsø StudyOsteoporos Int200617449550016283065
- JanghorbaniMFeskanichDWillettWCHuFProspective study of diabetes mellitus and risk of hip fracture: the Nurses’ Health StudyDiabetes Care20062971573157816801581
- LeslieWLixLPriorHDerksenShMetgeCO’NeilJBiphasic fracture risk in diabetes: a population-based studyBone20074061595160117392047
- LipscombeLJamalSBoothGKawkerGThe risk of hip fractures in older individuals with diabetesDiabetes Care200730483584117392544
- MeltonLJLeibsonCLAchenbachSJTherneauTMKhoslaSFracture risk in type 2 diabetes: update of a population-based studyJ Bone Miner Res20082381334134218348689
- ChenHFHoCALiCYIncreased risks of hip fracture in diabetic patients of TaiwanDiabetes Care2008311758017947342
- ManciniTMazziottiGDogaMVertebral fractures in males with type 2 diabetes treated with rosiglitazoneBone200945478478819527806
- YamamotoMYamaguchiTYamauchiMKajiHSugimotoTDiabetic patients have an increased risk of vertebral fractures independent of BMD or diabetic complicationsJ Bone Miner Res200924470270919049338
- SchneiderAWilliamsEBrancatiFBleckerSCoreshJSelvinEDiabetes and risk of fracture-related hospitalization: the atherosclerosis risk in communities studyDiabetes Care20133651153115823248194
- ChungDJChoiHJChungYSLimSKYangSOShinCSThe prevalence and risk factors of vertebral fractures in Korean patients with type 2 diabetesJ Bone Miner Metab201331216116823076296
- OeiLZillikensMDehghanAHigh bone mineral density and fracture risk in type 2 diabetes as skeletal complications of inadequate glucose control: the Rotterdam StudyDiabetes Care20133661619162823315602
- ReyesCEstradaPNoguésXThe impact of common co-morbidities (as measured using the Charlson index) on hip fracture risk in elderly men: a population-based cohort studyOsteoporos Int20142561751175824676845
- NapoliNStrotmeyerESEnsrudKEFracture risk in diabetic elderly men: the MrOS studyDiabetologia201457102057206524908567
- LeslieWDMorinSNLixLMMajumdarSRDoes diabetes modify the effect of FRAX risk factors for predicting major osteoporotic and hip fracture?Osteoporos Int201425122817282425092059
- HothersallEJLivingstoneSJLookerHCContemporary risk of hip fracture in type 1 and type 2 diabetes: a national registry study from ScotlandJ Bone Miner Res20142951054106024155126
- LookerACEberhardtMSSaydahSHDiabetes and fracture risk in older U.S. adultsBone20168291525576672
- KeganTHKelseyJLSidneySQuesenberryCPFoot problems as risk factors of fracturesAm J Epidemiol20021551092693111994232
- VestergaardPRejnmarkLMosekildeLRelative fracture risk in patients with diabetes mellitus, and the impact of insulin and oral antidiabetic medication on relative fracture riskDiabetologia20054871292129915909154
- KanazawaIYamaguchiTSugimotoTSerum insulin-like growth factor-I is negatively associated with serum adiponectin in type 2 diabetes mellitusGrowth Horm IGF Res201121526827121839662
- TanRSPuSJImpact of obesity on hypogonadism in the andropauseInt J Androl200225419520112121568
- Barrett-ConnorEKhawKTYenSSEndogenous sex hormone levels in older adult men with diabetes mellitusAm J Epidemiol199013258959012239904
- SeemanEMeltonLJ3rdO’FallonWMRiggsBLRisk factors for spinal osteoporosis in menAm J Med19837569779836650552
- ScaneACFrancisRMSutcliffeAMFrancisMJRawlingsDJChappleCLCase-control study of the pathogenesis and sequelae of symptomatic vertebral fractures in menOsteoporos Int199991919710367034
- YaturuSBryantBJainSKThiazolidinedione treatment decreases bone mineral density in type 2 diabetic menDiabetes Care20073061574157617363747
- AungKHtayTThiazide diuretics and the risk of hip fractureCochrane Database Syst Rev201110CD005185
- BazelierMTGallagherAMvan StaaTPUse of thiazolidinediones and risk of osteoporotic fracture: disease or drugs?Pharmacoepidemiol Drug Saf201221550751422392882
- MonamiMCresciBColombiniABone fractures and hypoglycemic treatment in type 2 diabetic patients: a case-control studyDiabetes Care200831219920318024851
- KimJHJungMHLeeJMSonHSChaBYChangSADiabetic peripheral neuropathy is highly associated with nontraumatic fractures in Korean patients with type 2 diabetes mellitusClin Endocrinol (Oxf)2012771515521906118
- Roman de MettelingeTCambierDCaldersPVan Den NoortgateNDelbaereKUnderstanding the relationship between type 2 diabetes mellitus andfalls in older adults: a prospective cohort studyPLoS One201386e6705523825617
- HuangESKarterAJDanielsonKKWartonEMAhmedATThe association between the number of prescription medications and incident falls in a multi-ethnic population of adult type-2 diabetes patients: the diabetes and aging studyJ Gen Intern Med201025214114619967465
- PijpersEFerreiraIde JonghRTOlder individuals with diabetes have an increased risk of recurrent falls: analysis of potential mediating factors: the Longitudinal Ageing Study AmsterdamAge Ageing201241335836522156559
- Leidig-BrucknerGZieglerRDiabetes mellitus a risk for osteoporosis?Exp Clin Endocrinol Diabetes2001109Suppl 2493514
- InzerilloAMEpsteinSOsteoporosis and diabetes mellitusRev Endocr Metab Disord20045326126815211098
- MoseleyKFType 2 diabetes and bone fracturesCurr Opin Endocrinol Diabetes Obes201219212813522262002
- PatelSHyerSTweedKRisk factors for fractures and falls in older women with type 2 diabetes mellitusCalcif Tissue Int2008822879118175036
- MontagnaniAGonnelliSAlessandriMNutiROsteoporosis and risk of fracture in patients with diabetes: an updateAging Clin Exp Res2011232849021743287
- GillespieLDRobertsonMCGillespieWJInterventions for preventing falls in older people living in the communityCochrane Database Syst Rev20092CD007146