Abstract
Introduction
Hollow viscus injuries (HVIs) are uncommon but potentially catastrophic conditions with high mortality and morbidity rates. The aim of this study was to analyze our 16-year experience with patients undergoing surgery for blunt or penetrating bowel trauma to identify prognostic factors with particular attention to the influence of diagnostic delay on outcome.
Methods
From our multicenter trauma registry, we selected 169 consecutive patients with an HVI, enrolled from 2000 to 2016. Preoperative, intraoperative, and postoperative data were analyzed to assess determinants of mortality, morbidity, and length of stay by univariate and multivariate analysis models.
Results
Overall mortality and morbidity rates were 15.9% and 36.1%, respectively. The mean length of hospital stay was 23±7 days. Morbidity was independently related to an increase of white blood cells (P=0.01), and to delay of treatment >6 hours (P=0.033), while Injury Severity Score (ISS) (P=0.01), presence of shock (P=0.01), and a low diastolic arterial pressure registered at emergency room admission (P=0.02) significantly affected postoperative mortality.
Conclusion
There is evidence that patients with clinical signs of shock, low diastolic pressure at admission, and high ISS are at increased risk of postoperative mortality. Leukocytosis and delayed treatment (>6 hours) were independent predictors of postoperative morbidity. More effort should be made to increase the preoperative detection rate of HVI and reduce the delay of treatment.
Introduction
Hollow viscus injuries (HVIs) are uncommon and found in ~1% of all blunt abdominal trauma patients.Citation1 Due to their rarity, experience with this injury is limited and no strong consensus exists in the literature regarding diagnosis and management of bowel injuries.Citation2
In penetrating trauma, early abdominal exploration is mandatory in 80% of cases and HVI diagnosis is prompt and easy. In blunt trauma, the non-operative management of solid organ injury has clearly increased the risk of delayed diagnosis and treatment of bowel lesions.Citation3–Citation7 Moreover, clinical and radiological diagnoses of bowel and/or mesenteric injuries are difficult as compared to injuries to other visceral organs, especially in cases of multiple trauma patients with head and spinal cord injuries or with impaired consciousness.Citation8
Accordingly, patients with undetected blunt HVI, who might otherwise have been diagnosed at laparotomy, could potentially progress to sepsis, multiple organ failure, and death. In spite of this, several surgeons do not consider the effect of delay in diagnosis and operative treatment of HVI significant on prognosis, both in adult and pediatric trauma patients.Citation8,Citation9
The purpose of this study was to analyze data on HVIs from a multicenter trauma registry, identify effective prognostic indicators in bowel injuries, and evaluate the effect of diagnostic and operative delay on outcome.
Materials and methods
Study setting
Policlinico Umberto I, S. Andrea Hospital, and S. Giovanni Addolorata Hospital are three large tertiary hospitals (Policlinico Umberto I and S. Andrea Hospital are two Sapienza University Hospitals) located in the central and northern urban areas of Rome, serving almost 2,000,000 people, and treating ~50% of the urban major traumas.
Study design
From a multi-institutional trauma registry including patient data collected from January 2000 to December 2016, 169 consecutive patients operated on for bowel injuries were retrospectively selected. The research was undertaken according to the Italian Privacy Laws concerning collection, storage, and analysis of private data. A formal Institutional Research Ethics Board (Sapienza University and S. Giovanni Addolorata Hospital) approval was not required because of the noninterventional, retrospective, and anonymous study design; however, a signed consent for the treatment and the analysis of data for scientific purpose was obtained from all patients or relatives either at admission or as soon as they could give it.
Both penetrating and blunt bowel injuries were considered, from the cardio-esophageal junction to the rectum at the level of the peritoneal reflection.
All hospital charts as well as the database analysis were reviewed.
Preoperative variables considered for analysis were:
Demographic data, cause and mechanism of injury, comorbid conditions, clinical features at emergency room (ER) admission such as systolic and diastolic blood pressure, heart rate, Glasgow Coma Scale (GCS), white blood cell count (WBC), hemoglobin values, clinical abdominal signs, and associated lesions.
Computed tomography (CT) scan findings at admission, Injury Severity Score (ISS), and the Bowel Injury Prediction Score (BIPS). BIPS is a new predictive score for bowel injuries first introduced by McNutt et al, able to predict the risk of a bowel injury when more than two of the following parameters are present at ER admission: 1) high grade mesenteric injury at admission CT scan, 2) increased WBC (>17,000), 3) abdominal tenderness. High grade mesenteric injury was considered as the presence of a mesenteric contusion or hematoma with associated bowel wall thickening and adjacent inter-loop fluid collection, or an active vascular/oral contrast extravasation, bowel transection or pneumoperitoneum.Citation10
Time from ER arrival to operating room and total elapsed time. Intraoperative data included surgical approach, type of treatment and reconstruction, and associated procedures.
Postoperative data included clinical events and follow-up. Mortality, morbidity, and length of hospital stay (LOS) were also retrieved from the database. Mortality was identified as any death occurring within the first 30 days from trauma or during the entire hospital stay. Morbidity was evaluated according to Clavien–Dindo classificationCitation11 and Surgical Site Infection (SSI) classification.Citation12
The primary endpoint of our study was to assess effective predictors of morbidity/mortality and LOS.
Secondary endpoints were the relationship between diagnostic delays and morbidity, mortality, and LOS in HVI and to assess a validated cut-off time for diagnostic delay able to predict the mortality/morbidity rates.
Statistics
Statistical analyses were performed using MedCalc for Windows, version 10.2.0.0 (MedCalc Software, MariaKerke, Belgium).
Patient and trauma features were analyzed using means ± SD for quantitative variables, and using frequencies and percentages for categorical variables. Differences in distribution were calculated using the Student’s t-test and analysis of variance (ANOVA) test for continuous variables, and chi-square test or Fisher’s exact test, depending on the number of cases in each subgroup, for categorical variables.
For multivariate analysis, multiple logistic regression was used, including in the model only the variables found to be significant at univariate analysis.
We used receiver operating characteristic (ROC) curve analysis to determine the best threshold and cut-off values for delay of treatment. Sensitivity, specificity, and positive and negative predictive values were calculated. Statistical significance was conventionally defined as P<0.05.
Results
Patient characteristics are shown in .
Table 1 Patient characteristics
Blunt abdominal trauma was the predominant cause of HVI (81.6%), and a motor vehicle accident was the most frequent mechanism of trauma.
A polytrauma (multiple traumatic injuries, and trauma with an ISS >16) was observed in 68 (40.2%) patients, and the association with shock was noted in 11.2% of cases ().
Table 2 Univariate and multivariate analysis showing predictors of postoperative morbidity and mortality considering both penetrating and blunt trauma
Mean GCS was 10.2 (minimum 3 – maximum 15). Mean abdominal/abbreviated injury scale and ISS were 3 (range 1–6) and 24 (range 3–66), respectively ().
A single bowel or mesenteric injury was observed in 143 (84.6%) patients; jejunum was the most common bowel tract involved (65% of cases), followed by mesenteric and colonic localization. When multiple bowel traumas were noted, the association of bowel and mesenteric injuries was the most frequent condition.
Jejunal suture or resection was the surgical procedure most commonly performed, and ostomy (ileal or colonic) was necessary in 12 (7.1%) cases.
The mean time to surgery after ER arrival was 12±8 hours (5.7±1.2 hours in penetrating trauma and 13.4±4.2 hours in blunt trauma); laparotomy was performed in the first 6, 12, and 24 hours after ER admission in 69.8%, 76.9%, and 87.5% of patients, respectively.
A total of 27 postoperative deaths were observed (mortality rate 15.9%), with 14 (51.8%) deaths in the first 96 hours and directly related to polytrauma.
The overall morbidity rate was 36.1% (16 patients); the abdominal surgical related complication rate was 19%, and superficial and medium SSI were the most frequent cause of postoperative morbidity. Pulmonary complications were the most prevalent systemic postoperative complication and occurred in 12% of cases.
The mean LOS was 23±7 days (range 1–350).
Prognostic indicators for postoperative mortality after bowel injuries were: ISS (P=0.010, OR =1.489, 95% CI =0.998 to 2.247), the presence of shock (P=0.026, OR =1.178, 95% CI =1.258 to 5.687), and low diastolic pressure registered at ER admission (P=0.029, OR =1.247, 95% CI =0.119 to 0.844) ().
Delay of treatment was not a prognostic indicator for post-operative mortality, even after patients who died during the first 24 hours were excluded from the analysis (P=0.780).
The statistical analysis revealed that morbidity was strongly and independently related to an increase of WBC during the initial ER evaluation (P=0.016, OR =2.254, 95% CI =0.514 to 1.126), and delay of treatment >6 hours (P=0.031, OR =1.941, 95% CI =0.818 to 1.414) ().
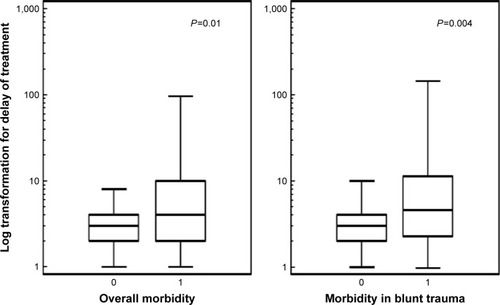
When the whole series was considered, the mean delay of diagnosis and treatment for the patients who developed a postoperative complication was 19.1±3.2 hours, compared to 6.2±1.9 hours for patients who did not present postoperative morbidity (ANOVA test, P=0.01) (, ). The same results were observed when the analysis was limited to blunt trauma patients: the mean delay of diagnosis and treatment for patients who developed a postoperative com-plication was 22.5±3.6 hours, compared to 6.1±1.4 hours for patients who did not present postoperative morbidity (ANOVA test, P=0.007) () (). In this subgroup, BIPSCitation10 value was an independent predictor of outcome (P=0.001, OR =0.029, 95% CI =1.359 to 6.158), indicating a significant predictive role in blunt trauma patients ().
Table 3 Univariate and multivariate analysis showing predictors of postoperative morbidity and mortality for blunt trauma
Table 4 Univariate and multivariate analysis showing predictors of delay of treatment
An ROC curve analysis was performed in order to identify predictive cut-off and threshold values in delay of diagnosis and treatment for morbidity. The analysis showed positive predictive values for postoperative morbidity of 73.5% and 100% for a delay of treatment of 12 and 24 hours, demonstrating that patients with a bowel injury treated 1 day after ER admission have a 100% possibility to develop a postoperative complication ( and ).
Figure 2 ROC curve for delay of treatment and morbidity.
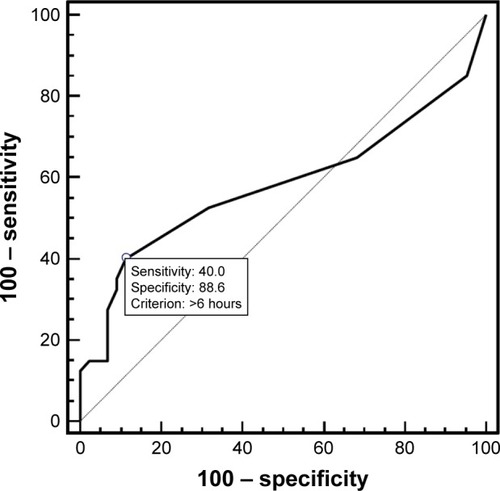
Table 5 Specificity/sensitivity and positive/negative predictive values of different cut-off time values of delay of treatment for morbidity
When predictors of treatment delay was analytically studied, a significant correlation was identified with heart rate (P=0.036, OR =2.756, 95% CI =0.741 to 1.159), presence of shock (P=0.037, OR =2.547, 95% CI =1.176 to 7.258), type of trauma (P=0.045, OR =2.951, 95% CI =1.258 to 6.223), and BIPS (P=0.001, OR =0.029, 95% CI =1.359 to 6.158) (), indicating that the presence of these parameters strongly suggests a prompt surgical treatment.
Discussion
Less than 1% of all patients who present with blunt trauma will have an HVI, and only 0.3% of all blunt trauma patients will have a perforated small bowel injury.Citation1,Citation13 It has been demonstrated that, due to the low incidence of these traumas, most trauma centers in the US reported seeing an average of 14 patients with HVI per year, resulting in limited exposure and experience of trauma surgeons who manage fewer than five HVI patients annually, even in large I level trauma centers.Citation1,Citation13
This reduced expertise of trauma surgeons is associated with the lack of clear international recommendations or established consensus in terms of optimal diagnostic approach.Citation14 Diagnostic peritoneal lavage progressively lost clinical application in the emergent setting, and abdominal CT scan often still fails to recognize indirect signs of traumatic bowel perforation.Citation15 Nowadays the advent and diffusion of dual-phase multidetector computer tomography with multiplanar reconstruction has improved the diagnostic accuracy of bowel and mesenteric injuries, but the limited experience of radiologists with these uncommon lesions and the concomitant presence of other abdominal organ injuries, still make this radiologic diagnosis challenging.Citation16–Citation19
In addition, the increased prevalence of non-operative management for blunt trauma patients has reduced the rate of urgent laparotomies, thus decreasing the opportunity to treat an unrecognized bowel injury or perforation.Citation3–Citation7
In penetrating trauma, abdominal exploration is still commonly performed in 80% of cases, thus resulting in a significant difference in treatment delay as compared to blunt trauma.Citation20,Citation21 In our series, patients with penetrating trauma were surgically treated in a mean time of 5.7±1.2 hours compared to patients with blunt trauma who underwent surgery in a mean time of 13.4±4.2 hours (P=0.01, ANOVA test). Several authors have shown the important diagnostic role of laparoscopy in hemodynamically stable patients with penetrating abdominal trauma: in experienced hands it can determine the integrity of peritoneum and diaphragm, and the presence of bowel and parenchymatous organ injuries. Overall, it can avoid non-therapeutic exploratory laparotomy in up to 70% of patients and, in selected cases, it can also have a therapeutic role in repairing minor lesions.Citation22,Citation23 Also in blunt abdominal trauma, laparoscopy could represent a similar diagnostic option, especially in patients with equivocal clinical and radiologic findings, before doing a laparotomy. However, its role remains undefined because the number of treated patients is small and only few series with promising results have been reported.Citation24,Citation25
According to the literature, the ileum is the most common site of bowel injury, followed by mesentery and colon.Citation1,Citation13 Perforation can be a common consequence of HVI and massive fecal peritonitis is the most worrisome complication.Citation26 Thus, the delay of diagnosis has become a “keyword” in management and treatment of HVI.
Even though past as well as more recent pediatric studies suggest that “short” diagnostic delays have no or little role in determining morbidity and mortality rates, our study highlights the importance of a prompt diagnosis and treatment of bowel injuries in order to reduce morbidity and hospital stay.Citation9
Letton and Worrell, in a multicenter study analyzing 358 pediatric patients, demonstrated that any significant statistical difference in terms of morbidity and mortality was found when patients were divided into four groups depending on treatment delay (0–6 hours, 6–12 hours, 12–24 hours, and >24 hours). Citation9
Despite these findings, and according to other reports,Citation1,Citation2,Citation8,Citation13 we demonstrated that treating an HVI within 6 hours from ER admission significantly reduces, at multivariate analysis, the complication rate (P=0.045, OR =1.614, 95% CI =0.752 to 1.973), and the delay of treatment became, with the increase of WBC, an independent prognostic factor for postoperative morbidity.
We also demonstrated, through the ROC curve, that a delay in treatment >24 hours has a positive predictive value of 100% for postoperative complications.
Some studies, however, demonstrated that delay of treatment significantly affects postoperative mortality as well; Fakhry et al, enrolling 198 patients from the registries of eight US trauma centers, demonstrated that mortality rates increased from 2% for patients treated within the first 8 hours from ER admission, to 9.1%, 16.7%, and 30.8% for patients treated after 8–16, 16–24, and >24 hours, respectively.Citation2
Accordingly, Faria et al observed, in their series of 102 patients with both blunt and penetrating bowel injuries, that all postoperative deaths occurred in patients operated on after the first 24 hours.Citation26
Our series failed to demonstrate the influence of the delay of treatment on postoperative mortality; in fact, the statistical analysis outlined the presence of shock, as well as a reduced diastolic artery pressure and ISS as independent prognostic indicators of postoperative mortality.
In order to facilitate the diagnosis of HVI, McNutt et al recently introduced a new effective predictive score for blunt bowel and mesenteric injury.Citation10 The authors retrospectively combined three different physical, hematological, and radiological parameters (admission CT scan grade of mesenteric injury, WBC, and abdominal tenderness) in order to evaluate their predictive value for the presence of an HVI. They demonstrated that patients with a BIPS of ≥2, were 19 times more likely to have an HVI than patients with a BIPS of less than 2 (P<0.001, OR =19.2; 95% CI =6.78 to 54.36), showing that the system can be used in combination to create a bowel injury score, with a score of ≥2 strongly associated with HVI.Citation10
We specifically analyzed this parameter in our series and demonstrated that patients with a BIPS score >2 had a significant probability to develop a postoperative complication (P=0.029, OR =2.143, 95% CI =1.359 to 6.158) compared to patients with a BIPS <2.
Conclusion
HVIs are an uncommon finding in abdominal trauma patients. Several prognostic factors have been identified for morbidity and mortality, and among them delay of treatment has been identified as an independent predictor of morbidity, strongly affecting the postoperative course.
More efforts should be directed at increasing the preoperative detection rate of HVIs; new and effective predictive radiological tools in association with physical and hematological parameters (BIPS) seem to increase the diagnostic sensitivity and reduce the delay of treatment to less than 6–12 hours after ER admission.
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- FakhrySMWattsDDLuchetteFAEAST Multi-Institutional Hollow Viscus Injury Research GroupCurrent diagnostic approaches lack sensitivity in the diagnosis of perforated blunt small bowel injury: analysis from 275,557 trauma admissions from the EAST multi-institutional HVI trialJ Trauma200354229530612579055
- FakhrySMBrownsteinMWattsDDBakerCCOllerDRelatively short diagnostic delays (<8 hours) produce morbidity and mortality in blunt small bowel injury: an analysis of time to operative intervention in 198 patients from a multicenter experienceJ Trauma200048340841410744277
- StassenNABhullarIChengJDEastern Association for the Surgery of TraumaNonoperative management of blunt hepatic injury: an Eastern Association for the Surgery of Trauma practice management guidelineJ Trauma Acute Care Surg2012735 Suppl 4S288S29323114483
- StassenNABhullarIChengJDEastern Association for the Surgery of TraumaSelective nonoperative management of blunt splenic injury: an Eastern Association for the Surgery of Trauma practice management guidelineJ Trauma Acute Care Surg2012735 Suppl 4S294S30023114484
- KerwinAJHautERBurnsJBEastern Association for the Surgery of Trauma Practice Management Guidelines Ad Hoc CommitteeThe Eastern Association of the Surgery of Trauma approach to practice management guideline development using Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) methodologyJ Trauma Acute Care Surg2012735 Suppl 4S283S28723114482
- DiazJJJrCullinaneDCDuttonWDThe management of the open abdomen in trauma and emergency general surgery: part 1-damage controlJ Trauma20106861425143820539186
- ComoJJBokhariFChiuWCPractice management guidelines for selective nonoperative management of penetrating abdominal traumaJ Trauma201068372173320220426
- BrownsteinMRBuntingTMeyerAAFakhrySMDiagnosis and management of blunt small bowel injury: a survey of the membership of the American Association for the Surgery of TraumaJ Trauma200048340240710744276
- LettonRWWorrellVAPSA Committee on Trauma Blunt Intestinal Injury Study GroupDelay in diagnosis and treatment of blunt intestinal injury does not adversely affect prognosis in the pediatric trauma patientJ Pediatr Surg201045116116520105598
- McNuttMKChinapuvvulaNRBeckmannNMEarly surgical intervention for blunt bowel injury: the Bowel Injury Prediction Score (BIPS)J Trauma Acute Care Surg201578110511125539210
- DindoDDemartinesNClavienPAClassification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a surveyAnn Surg2004240220521315273542
- HoranTCGaynesRPMartoneWJJarvisWREmoriTGCDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infectionsInfect Control Hosp Epidemiol199213106066081334988
- WattsDDFakhrySMEAST Multi-Institutional Hollow Viscus Injury Research GroupIncidence of hollow viscus injury in blunt trauma: an analysis from 275,557 trauma admissions from the East multi-institutional trialJ Trauma200354228929412579054
- MahmoodITawfekZAbdelrahmanYSignificance of computed tomography finding of intra-abdominal free fluid without solid organ injury after blunt abdominal trauma: time for laparotomy on demandWorld J Surg20143861411141524368575
- IaselliFMazzeiMAFirettoCBowel and mesenteric injuries from blunt abdominal trauma: a reviewRadiol Med20151201213225572542
- YuJFulcherASTurnerMACockrellCHalvorsenRABlunt bowel and mesenteric injury: MDCT diagnosisAbdom Imaging2011361506120063092
- KhanIBewDEliasDALewisDMeacockLMMechanisms of injury and CT findings in bowel and mesenteric traumaClin Radiol201469663964724606835
- LandryBAPatlasMNFaidiSCoatesANicolaouSAre we missing traumatic bowel and mesenteric injuries?Can Assoc Radiol J201667442042527266653
- AtriMHansonJMGrinblatLBrofmanNChughtaiTTomlinsonGSurgically important bowel and/or mesenteric injury in blunt trauma: accuracy of multidetector CT for evaluationRadiology2008249252453318796660
- NelsonRSingerMPrimary repair for penetrating colon injuriesCochrane Database Syst Rev20033CD00224712917927
- KirkpatrickAWBaxterKASimonsRKGermannELucasCELedgerwoodAMIntra-abdominal complications after surgical repair of small bowel injuries: an international reviewJ Trauma200355339940614501878
- AhmedNWhelanJBrownleeJChariVChungRThe contribution of laparoscopy in evaluation of penetrating abdominal woundsJ Am Coll Surg2005201221321616038818
- UranuesSPopaDEDiaconescuBSchrittwieserRLaparoscopy in penetrating abdominal traumaWorld J Surg20153961381138825446491
- JohnsonJJGarweTRainesARThe use of laparoscopy in the diagnosis and treatment of blunt and penetrating abdominal injuries: 10-year experience at a level1 trauma centerAm J Surg2013205331732123375706
- LinHFChenYDLinKLWuMCWuCYChenSCLaparoscopy decreases the laparotomy rate for hemodynamically stable patients with blunt hollow viscus and mesenteric injuriesAm J Surg2015210232633325963637
- FariaGRAlmeidaABMoreiraHBarbosaECorreia-da-SilvaPCosta-MaiaJPrognostic factors for traumatic bowel injuries: killing timeWorld J Surg201236480781222350477