Abstract
Introduction
Preservation of kidney and renal function is the goal of nonoperative management (NOM) of renal trauma (RT). The advantages of NOM for minor blunt RT have already been clearly described, but its value for major blunt and penetrating RT is still under debate. We present a systematic review and meta-analysis on NOM for RT, which was compared with the operative management (OM) with respect to mortality, morbidity, and length of hospital stay (LOS).
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-analyses statement was followed for this study. A systematic search was performed on Embase, Medline, Cochrane, and PubMed for studies published up to December 2015, without language restrictions, which compared NOM versus OM for renal injuries.
Results
Twenty nonrandomized retrospective cohort studies comprising 13,824 patients with blunt (2,998) or penetrating (10,826) RT were identified. When all RT were considered (American Association for the Surgery of Trauma grades 1–5), NOM was associated with lower mortality and morbidity rates compared to OM (8.3% vs 17.1%, odds ratio [OR] 0.471; 95% confidence interval [CI] 0.404–0.548; P<0.001 and 2% vs 53.3%, OR 0.0484; 95% CI 0.0279–0.0839, P<0.001). Likewise, NOM represented the gold standard treatment resulting in a lower mortality rate compared to OM even when only high-grade RT was considered (9.1% vs 17.9%, OR 0.332; 95% CI 0.155–0.708; P=0.004), be they blunt (4.1% vs 8.1%, OR 0.275; 95% CI 0.0957–0.788; P=0.016) or penetrating (9.1% vs 18.1%, OR 0.468; 95% CI 0.398–0.0552; P<0.001).
Conclusion
Our meta-analysis demonstrated that NOM for RT is the treatment of choice not only for AAST grades 1 and 2, but also for higher grade blunt and penetrating RT.
Introduction
The kidney is the third most frequently injured organ in abdominal trauma after the spleen and liver.Citation1 In the last 30 years, the treatment strategy of renal trauma has changed from operative management (OM) to nonoperative management (NOM).Citation1 Several studies showed improving outcomes when NOM was applied in blunt trauma and, therefore, conservative management gained an increasing popularity among trauma surgeons.Citation2–Citation4
However, specific guidelines regarding renal trauma are still lacking and the few papers providing recommendations are not supported by relevant grades of evidence.
Immediate surgical management of injuries with life-threatening hemorrhage is widely accepted; however, when this clear-cut indication is lacking, several differences in management strategies emerge from the literature.Citation5–Citation8 A successful conservative management for blunt low-grade renal injury (renal contusions and minor lacerations) is well documented with a low complication rate,Citation9,Citation10 but what about the optimal management of penetrating and high-grade blunt injuries?
We first investigated through a systematic review and meta-analysis the efficacy of OM and NOM on any grade, blunt or penetrating, renal trauma and evaluated mortality, morbidity, and length of hospital stay (LOS) for the different types of injuries and management.
Methods
Study selection
The criteria of the “Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement” were followed in the present study.Citation11 Embase, Medline, Cochrane, and PubMed databases were used to identify studies, published up to December 2015, comparing blunt and penetrating renal trauma in adults. The following MESH search headings were used: “operative and non-operative management renal trauma”, “operative and non-operative treatment for blunt and penetrating adult renal injury”, “operative and non-operative treatment for genitourinary trauma”, and “operative and non-operative management kidney injury”. The “related articles” function in PubMed database was used to increase and widen the search to all similar abstracts and studies.
Inclusion criteria
Studies comparing the selected clinical outcomes – that is, mortality, morbidity and length of stay – of adult patients submitted to OM and NOM for renal trauma were selected for the analysis.
Exclusion criteria
We did not consider for meta-analysis: 1) studies in which mortality, morbidity, and LOS were not reported separately for NOM and OM, 2) studies analyzing pediatric patients, or 3) papers reporting series already selected for this meta-analysis.
Data extraction
Data concerning study author, year of publication, patient characteristics, study design, number of patients submitted to NOM or OM, mortality rates, morbidity rates, and length of stay (LOS) were extracted and inserted into a database.
Outcomes of interest and definition
Patients’ demographics (age and sex), trauma characteristics (open or blunt), trauma severity (Injury Severity Score – ISS), American Association for the Surgery of Trauma (AAST) grade, hemodynamic stability, type of management (operative and nonoperative), and clinical outcomes (morbidity, mortality, LOS) were retrieved.
Morbidity and mortality were defined as in-hospital complication and mortality rates.
Intervention types were defined as: NOM (clinical observation, medical treatment, and proximal or distal renal angio-embolization) and OM (total or partial nephrectomy, nephrorrhaphy, or application of hemostatic agents).
Study endpoints
The primary endpoint was the overall mortality and morbidity defined as any death or complication that occurred after the start of NOM or OM and during the hospital stay for all renal trauma (blunt and penetrating).
The secondary endpoint was the overall mortality and morbidity that occurred after the start of NOM or OM and during the hospital stay for blunt and penetrating renal trauma considered separately.
The tertiary endpoint was the overall mortality and morbidity that occurred after the start of NOM or OM and during the hospital stay for all high-grade renal trauma (AAST 3–5).
The quaternary endpoint was the length of stay after the start of NOM or OM.
Study selection
A total of 465 papers were identified at the end of the literature search. After a first evaluation performed by abstract analysis, 369 studies were excluded because they were irrelevant to the purpose of our study, and 37 studies because of overlapping data. The full-text analysis of the 49 remaining studies resulted in exclusion of 29 because they did not match the inclusion criteria, while 20 were selected for further analysis.Citation5,Citation12–Citation30
Search strategy results
Twenty nonrandomized retrospective cohort studies () accounting for a total of 13,824 patients affected with renal injury form the basis of our analysis; 11,426 patients underwent NOM and 2,398 OM.
Table 1 Study selection
Quality of included studies
The quality of included studies was assessed by two authors (MLT and AM) using the Newcastle–Ottawa Scale (NOS).Citation31 All included studies had good methodological quality (>5 points; mean 6.9 points, range 6–9).
Risk of bias
Distribution of age, sex, and ISS were homogenous between the NOM and OM groups. Conversely, the AAST grade was not homogenous between the two groups: in the NOM group, there were 3,252 (28.5%) high-grade (AAST 3–5) renal trauma whereas in the OM group they were 1,387 (57.8%; P<0.0001).
Statistical analysis
Statistical analysis was conducted using MedCalc for Windows, version 10.2.0.0 (MedCalc Software, MariaKerke, Belgium).
Odds ratio (OR), for dichotomous outcomes, was calculated by the Mantel–Haenszel method, while standardized mean difference (SMD), for continuous outcomes, was calculated by Hedges g statistic. Results from the meta-analysis for OR were considered statistically significant (P<0.05) if the value 1 was not within the 95% CI, whereas for SMD, it was if the value 0 was not within the 95% CI.
Heterogeneity was also studied by calculating the Chi2 and the inconsistency (I2). As I2 detected the absence of homogeneity (>50%), the fixed effect model could not be used; therefore, the random effect model was used for analysis.
If the test of heterogeneity was statistically significant (P<0.05), then more emphasis should be placed on the random effects model.
Results
Twenty retrospective cohort studies comprising 13,824 patients were selected (). Eight studies analyzed 2,998 patients with blunt renal trauma (BRT),Citation5,Citation12,Citation23,Citation26–Citation30 whereas 12 studies analyzed the remaining 10,826 patients with penetrating renal trauma (PRT).Citation14–Citation24,Citation28 Patient characteristics are summarized in .
Table 2 Patient characteristics
NOM was the most frequent and prevalent strategy adopted for renal trauma, with 11,426 (82.4%) patients treated conservatively versus 2,398 (17.3%) patients treated operatively ().
Table 3 Chi-square test analyzing the proportion of patients treated with NOM and OM
NOM was significantly more frequently adopted in BRT, compared to PRT (; P<0.0001). shows the distribution of NOM and OM according to the severity of renal trauma (AAST scale), both for penetrating or blunt trauma. A significantly higher number of patients was treated conservatively for low-grade trauma and a significantly higher number of patients was treated operatively for high-grade trauma (P<0.0001).
Table 4 Chi-square test analyzing the proportion of patients treated with NOM and OM according to AAST scale
Further analysis pursued the following criteria: 1) An analysis concerning all renal trauma (AAST low and high grades) and 2) an analysis concerning only high-grade renal trauma.
NOM versus OM for all renal trauma
Eleven studies compared morbidity,Citation5,Citation12,Citation15,Citation18,Citation22–Citation25,Citation27,Citation29,Citation30 twelve compared mortality,Citation12,Citation13,Citation15,Citation17–Citation19,Citation22,Citation26–Citation30 and four compared LOS,Citation19,Citation26,Citation28,Citation30 according to OM and NOM.
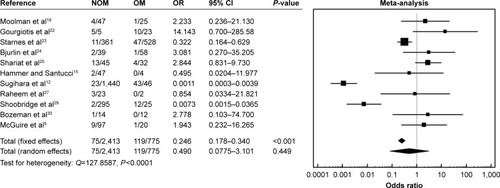
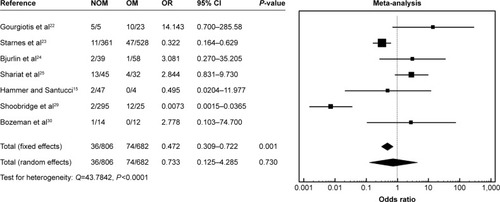
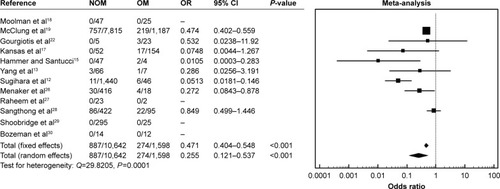
A higher mortality rate for OM (17.1%, 274/1,598) compared to NOM (8.3% 887/10,642; OR 0.471; 95% CI 0.404–0.548; P<0.001) was observed when all renal trauma were considered ().
Figure 1 Overall mortality.
Abbreviations: CI, confidence interval; NOM, nonoperative management; OM, operative management; OR, odds ratio.
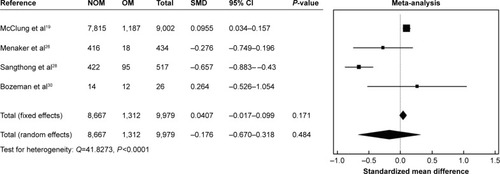
No statistical differences were encountered in terms of morbidity and LOS (OR 0.490; 95% CI 0.0775–3.101; P=0.449 and SMD =0.0407; 95% CI −0.017 to 0.099; P=0.171; and ).
NOM versus OM for all-grade BRT
Five studies compared morbidity,Citation5,Citation12,Citation27,Citation29,Citation30 seven compared mortality,Citation12,Citation13,Citation26–Citation30 and three compared LOS.Citation26,Citation28,Citation30
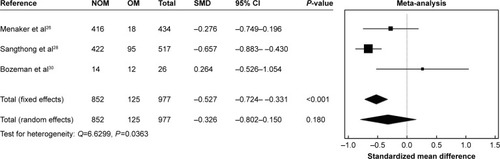
We observed significantly higher morbidity and mortality rates with OM versus NOM when only blunt trauma were studied (the analysis included all grades of renal trauma according to the AAST scale; and ).
Figure 4 Morbidity for blunt renal trauma.
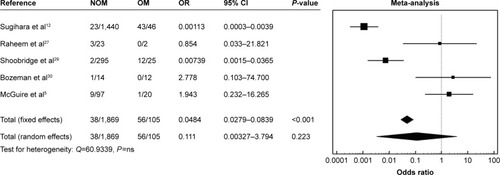
Figure 5 Mortality for blunt renal trauma.
Abbreviations: CI, confidence interval; NOM, nonoperative management; OM, operative management; OR, odds ratio.
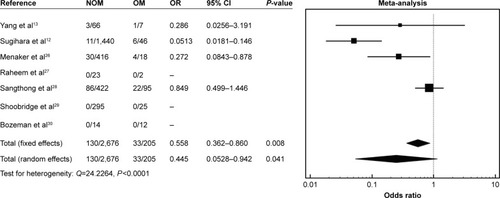
After NOM, we observed a lower morbidity rate (38/1,869, 2%) when compared to OM (56/105, 53.3%) (OR 0.0484; 95% CI 0.0279–0.0839; P<0.001) as well as a lower mortality rate (130/2,676, 4.8%, vs 33/205, 16.1%; OR 0.445; 95% CI 0.0528–0.942; P=0.041).
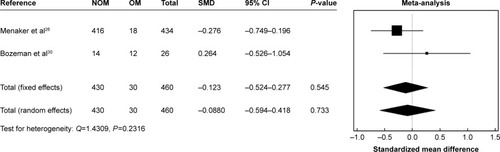
LOS was similar between OM and NOM (SMD −0.326; 95% CI −0.802 to 0.150; P=0.180; ).
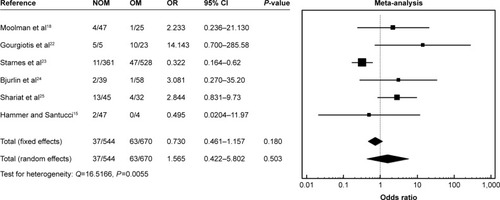
NOM versus OM for all-grade PRT
Six studies compared morbidity,Citation15,Citation18,Citation22–Citation25 and five compared mortality.Citation15,Citation17–Citation19,Citation23 No studies specifically analyzed LOS.
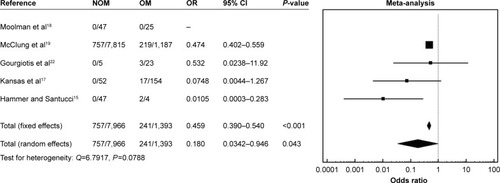
A significantly lower mortality rate of NOM (757/7,966, 9.5%) when compared to OM (241/1,393, 13.3%; OR 0.459; 95% CI 0.390–0.540; P<0.001) was recorded for all penetrating trauma ().
Figure 7 Mortality for penetrating renal trauma.
Abbreviations: CI, confidence interval; NOM, nonoperative management; OM, operative management; OR, odds ratio.
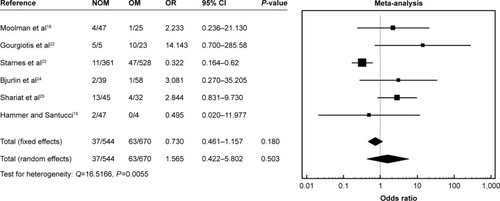
Morbidity was similar for OM and NOM (OR 1.565; 95% CI 0.422–5.802; P=0.503; ).
NOM versus OM for high-grade (3–5) renal trauma
Seven studies compared morbidity,Citation15,Citation22–Citation25,Citation29,Citation30 seven compared mortality,Citation13,Citation15,Citation19,Citation22,Citation26,Citation29,Citation30 and three compared LOS.Citation19,Citation26,Citation30
When all high-grade BRT or PRT were considered, a higher mortality rate for OM (17.9%, 790/8,658), when compared to NOM (9.1%, 229/1,276; OR 0.332; 95% CI 0.155–0.708; P=0.004; ), and a reduced LOS (SMD 0.0905, 95% CI 0.030–0.151, P=0.003) were recorded ().
Figure 9 Overall mortality, high-grade renal trauma.
Abbreviations: CI, confidence interval; NOM, nonoperative management; OM, operative management; OR, odds ratio.
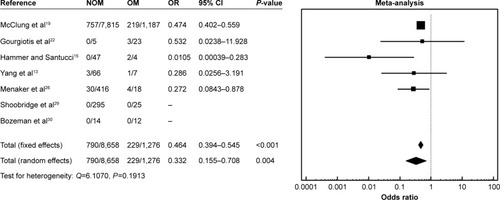
Figure 10 Overall length of stay, high-grade renal trauma.
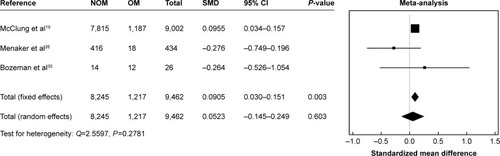
No statistical differences were observed in terms of morbidity (OR 0.733, 95% CI 0.125–4.285, P=0.730; ).
NOM versus OM for high-grade BRT
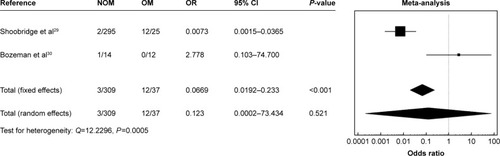
Two studies compared morbidity,Citation29,Citation30 four compared mortality,Citation13,Citation26,Citation29,Citation30 and two compared LOS.Citation26,Citation30
A significantly higher mortality rate for OM versus NOM (4.1%, 33/791 vs 8.1%, 5/62; OR 0.275; 95% CI 0.0957–0.788; P=0.016) was recorded ().
Figure 12 Mortality in high-grade blunt trauma.
Abbreviations: CI, confidence interval; NOM, nonoperative management; OM, operative management; OR, odds ratio.
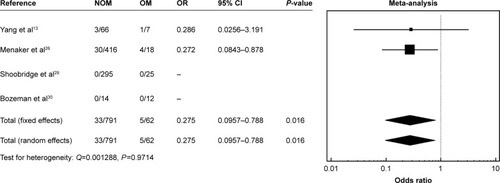
Morbidity and LOS were similar between OM and NOM (OR 0.123; 95% CI 0.0002–73.434; P=0.521 and SMD −0.0880; 95% CI −0.594 to 0.418; P=0.733, respectively; and ).
NOM versus OM for high-grade PRT
Six studies compared morbidity,Citation15,Citation18,Citation22–Citation25 and four compared mortality.Citation15,Citation18,Citation19,Citation22 No studies specifically analyzed LOS.
A significantly higher mortality rate of OM versus NOM (9.1%, 757/7,914 vs 18.1%, 224/1,239; OR 0.468; 95% CI 0.398–0.552; P<0.001) was observed ().
Figure 15 Mortality in high-grade penetrating trauma.
Abbreviations: CI, confidence interval; NOM, nonoperative management; OM, operative management; OR, odds ratio.
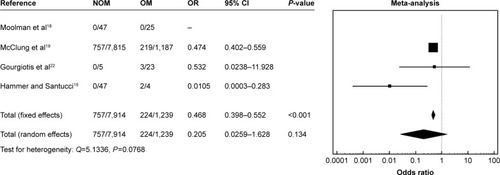
No statistical differences were observed in terms of morbidity (OR 1.565; 95% CI 0.422–5.802; P=0.503) between the two groups ().
Discussion
The kidney is the third most commonly injured solid organ after blunt trauma, and the second most commonly affected after penetrating trauma.Citation1 Every year, 245,000 renal trauma cases occur worldwide, with blunt trauma representing approximately 80% of cases.Citation1
The treatment strategy of BRT has not changed in the last 30 years. The standard of care is, in most cases, nonoperative and up to 95% of the pediatric patients do not undergo surgery.Citation1–Citation4,Citation9 Conversely, the management of penetrating injuries has significantly changed.Citation29,Citation30 Traditionally, penetrating renal injuries were managed with exploration, nephrorrhaphy, partial nephrectomy, or nephrectomy.Citation17,Citation18 The approach to renal gunshot wounds was still more prudent and careful, with surgical exploration and repair considered mandatory treatment. In 1997, Wessells et al suggested that many grade 2 penetrating renal injuries can be managed nonoperatively.Citation32 In 1998, Velmahos et al reported that a kidney exploration was not necessary in approximately 40% of renal gunshot trauma.Citation33 In 2006, the same authors showed that a nonoperative management was successful in 50% of isolated penetrating kidney injuries.Citation34
In our meta-analysis, we demonstrated that NOM was the most frequent and prevalent strategy of cure used for renal trauma in adults, with 11,426 (82.4%) patients conservatively treated (17.3%) versus 2,398 patients who underwent surgery. However, when we analyzed the distribution of NOM and OM on the basis of the severity of renal trauma (AAST scale), we observed a significantly higher number of patients with low-grade trauma treated conservatively and a significantly higher number of patients with high-grade trauma treated operatively (P<0.0001). Furthermore, NOM was more frequently used in BRT, compared to PRT (P<0.0001).
Major debate concerns the indications for surgical exploration – both for BRT and PRT in high-grade trauma. The experience translated from NOM in pediatric hepatic and splenic trauma, the availability of multi-slice computerized tomography, and the acquisition of angiographic embolization techniques demonstrated that, NOM in selected hepatic and splenic high-grade trauma, also in adults, has better outcomes in terms of morbidity, mortality, and LOS when compared to surgical exploration.Citation34–Citation37 In the present study, we clearly demonstrated that NOM can be safely performed even for high-grade RT, allowing a significant reduction of the mortality rate (9.1% vs 17.9%; OR 0.332; 95% CI 0.155–0.708; P=0.004; ).
When blunt and penetrating high-grade RT data were analyzed separately, we found similar outcomes: mortality in blunt trauma decreased from 8.1% after OM to 4.1% after NOM (OR 0.275; 95% CI 0.0957–0.788; P=0.016), and in penetrating trauma from 18.1% after OM to 9.1% after NOM (OR 0.468; 95% CI 0.398–0.552; P<0.001).
Our data demonstrated that hemodynamically stable patients do not always need surgical exploration, because major renal trauma may heal either spontaneously or after minimally invasive procedures. Matthews et al reported spontaneous healing in 87% of 31 patients affected with a renal injury and urinary extravasation.Citation38 Haas et al described a high renal salvage rate using ureteral stents in patients with renal trauma and urinary extravasation.Citation39 In a series of 20 patients with either grade 4 or 5 renal trauma who were conservatively treated, Moudouni et al reported six open delayed procedures, whereas the remaining patients healed spontaneously or after ureteral stent positioning.Citation40 Altman et al compared two groups of patients affected with grade 5 injuries.Citation7 Six were managed conservatively and seven were operated on. The authors affirmed that patients treated conservatively had a lower morbidity rate, with functioning renal parenchyma at follow-up CT scan.Citation7
Moreover, our analysis showed a lower LOS of NOM versus OM and similar morbidity rates of both NOM and OM in patients with BRT or penetrating high-grade renal trauma, suggesting that NOM can be safely undertaken, avoiding laparotomies, kidney resections, and nephrectomies, and allowing hospital cost reduction.
Conclusion
The results of this meta-analysis showed that not only is NOM the treatment of choice for low-grade RT, but also that it should be considered as the first-line treatment even for high-grade blunt or penetrating RT, because it is associated to lower mortality rates and LOS, and similar morbidity rates.
Disclosure
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest in the subject matter discussed in this manuscript and report no conflicts of interest in this work.
References
- KuanJKWrightJLNathensABRivaraFPWessellsHAmerican Association for the Surgery of TraumaAmerican Association for the Surgery of Trauma Organ Injury Scale for kidney injuries predicts nephrectomy, dialysis, and death in patients with blunt injury and nephrectomy for penetrating injuriesJ Trauma200660235135616508495
- ShariatSFTrinhQDMoreyAFDevelopment of a highly accurate nomogram for prediction of the need for exploration in patients with renal traumaJ Trauma20086461451145818545108
- SantucciRAWessellsHBartschGEvaluation and management of renal injuries: consensus statement of the renal trauma subcommitteeBJU Int200493793795415142141
- HommesMNavsariaPHSchipperIBKrigeJEKahnDNicolAJManagement of blunt liver trauma in 134 severely injured patientsInjury201546583784225496854
- McGuireJBultitudeMFDavisPKoukounarasJRoycePLCorcoranNMPredictors of outcome for blunt high grade renal injury treated with conservative intentJ Urol2011185118719121074795
- McAninchJWFederleMPEvaluation of renal injuries with computerized tomographyJ Urol198212834564607120545
- AltmanALHaasCDinchmanKHSpirnakJPSelective nonoperative management of blunt grade 5 renal injuryJ Urol200016412730 discussion 30–3110840417
- MoudouniSMHadj SlimenMManuntaAManagement of major blunt renal lacerations: is a nonoperative approach indicated?Eur Urol200140440941411713395
- HagiwaraASakakiSGotoHThe role of interventional radiology in the management of blunt renal injury: a practical protocolJ Trauma200151352653111535904
- HusmannDAGillingPJPerryMOMorrisJSBooneTBMajor renal lacerations with a devitalized fragment following blunt abdominal trauma: a comparison between nonoperative (expectant) versus surgical managementJ Urol19931506177417778230501
- MoherDLiberatiATetzlaffJAltmanDGPRISMA GroupPreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementPLoS Med200967e100009719621072
- SugiharaTYasunagaHHoriguchiHManagement trends, angioembolization performance and multiorgan injury indicators of renal trauma from Japanese administrative claims databaseInt J Urol2012196559563 author reply 56422404502
- YangCSChenICWangCYLiuCCShihHCHuangMSPredictive indications of operation and mortality following renal traumaJ Chin Med Assoc2012751212422240532
- SahinHAkayAFYilmazGTaçyildizIHBircanMKRetrospective analysis of 135 renal trauma casesInt J Urol200411533233615147552
- HammerCCSantucciRAEffect of an institutional policy of nonoperative treatment of grades I to IV renal injuriesJ Urol200316951751175312686825
- BuckleyJCMcAninchJWSelective management of isolated and nonisolated grade IV renal injuriesJ Urol20061766 Pt 124982502 discussion 250217085141
- KansasBTEddyMJMydloJHUzzoRGIncidence and management of penetrating renal trauma in patients with multiorgan injury: extended experience at an inner city trauma centerJ Urol20041724 Pt 11355136015371841
- MoolmanCNavsariaPHLazarusJPontinANicolAJNonoperative management of penetrating kidney injuries: a prospective auditJ Urol2012188116917322591960
- McClungCDHotalingJMWangJWessellsHVoelzkeBBContemporary trends in the immediate surgical management of renal trauma using a national databaseJ Trauma Acute Care Surg201375460260624064872
- AragonaFPepePPatanèDMalfaPD’ArrigoLPennisiMManagement of severe blunt renal trauma in adult patients: a 10-year retrospective review from an emergency hospitalBJU Int2012110574474822313622
- van der VliesCHOlthofDCvan DeldenOMManagement of blunt renal injury in a level 1 trauma centre in view of the European guidelinesInjury201243111816182021742328
- GourgiotisSGermanosSDimopoulosNVougasVAnastasiouTBaratsisSRenal injury: 5-year experience and literature reviewUrol Int20067729710316888410
- StarnesMDemetriadesDHadjizachariaPInabaKBestCChanLComplications following renal traumaArch Surg20101454377381 discussion 381–38220404289
- BjurlinMAJengEIGobleSMDohertyJCMerlottiGJComparison of nonoperative management with renorrhaphy and nephrectomy in penetrating renal injuriesJ Trauma201171355455821610541
- ShariatSFJenkinsARoehrbornCGKaramJAStageKHKarakiewiczPIFeatures and outcomes of patients with grade IV renal injuryBJU Int20081026728733 discussion 73318435808
- MenakerJJosephBSteinDMScaleaTMAngiointervention: high rates of failure following blunt renal injuriesWorld J Surg201135352052721190111
- RaheemOFloydMSJrCaseyRGRenal trauma in the west of Ireland – a regional reviewScientificWorldJournal2009913714319252753
- SangthongBDemetriadesDMartinMManagement and hospital outcomes of blunt renal artery injuries: analysis of 517 patients from the National Trauma Data BankJ Am Coll Surg2006203561261717084321
- ShoobridgeJJBultitudeMFKoukounarasJMartinKERoycePLCorcoranNMA 9-year experience of renal injury at an Australian level 1 trauma centreBJU Int2013112Suppl 2536023418742
- BozemanCCarverBZabariGCalditoGVenableDSelective operative management of major blunt renal traumaJ Trauma200457230530915345977
- WellsGASheaBO’ConnellDThe Newcastle-Ottawa Scale (NOS) for assessing the quality of non randomized studies in meta-analysesOttawa, ONOttawa Hospital Research Institute Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htmAccessed December 15, 2016
- WessellsHMcAninchJWMeyerABruceJCriteria for nonoperative treatment of significant penetrating renal lacerationsJ Urol1997157124278976207
- VelmahosGCDemetriadesDCornwellEE3rdSelective management of renal gunshot woundsBr J Surg1998858112111249718011
- DemetriadesDHadjizachariaPConstantinouCSelective nonoperative management of penetrating abdominal solid organ injuriesAnn Surg2006244462062816998371
- ChristmasABWilsonAKManningBSelective management of blunt hepatic injuries including nonoperative management is a safe and effective strategySurgery20051384606610 discussion 610–61116269288
- GourgiotisSVougasVGermanosSOperative and nonoperative management of blunt hepatic trauma in adults: a single-center reportJ Hepatobiliary Pancreat Surg200714438739117653638
- ScarboroughJEIngrahamAMLiepertAEJungHSO’RourkeAPAgarwalSKNonoperative management is as effective as immediate splenectomy for adult patients with high-grade blunt splenic injuryJ Am Coll Surg2016223224925827112125
- MatthewsLASmithEMSpirnakJPNonoperative treatment of major blunt renal lacerations with urinary extravasationJ Urol19971576205620589146579
- HaasCAReigleMDSelzmanAAElderJSSpirnakJPUse of ureteral stents in the management of major renal trauma with urinary extravasation: is there a role?J Endourol19981265455499895260
- MoudouniSMPatardJJManuntaAGuiraudPGuilleFLobelBA conservative approach to major blunt renal lacerations with urinary extravasation and devitalized renal segmentsBJU Int200187429029411251518