Abstract
Precis
During the management of cesarean scar pregnancy, gestational mass size >6 cm, uterine scar thickness <0.2 cm, peak systolic velocity >70 cm/s, and resistance index <0.35 are independent risk factors for excessive hemorrhage.
Objective
The objective of this study was to investigate risk factors associated with excessive hemorrhage during the management of cesarean scar pregnancy (CSP).
Patients and methods
A retrospective case–control study was conducted, including 40 patients who experienced excessive bleeding and 80 controls without severe hemorrhage.
Results
Six parameters (two clinical and four ultrasound parameters) potentially related to excessive hemorrhage were analyzed. Single-variable statistical analyses showed that the case group had higher gestational age (74.1±23.6 days), higher pretreatment serum β-human chorionic gonadotropin (HCG) level (46,201±32,294 mIU/mL), larger gestational mass size (6.5±2.2 cm), thinner uterine scar thickness (0.17±0.12 cm), and richer peritrophoblastic perfusion (peak systolic velocity [PSV] 72.8±33.7 cm/s, resistance index [RI] 0.35±0.12), showing statistical significance compared with the control group. Further multivariable logistic regression analysis of the association between each of the risk factors and hemorrhage confirmed that increased gestational mass size and PSV were risk factors for hemorrhage (odds ratio [OR] 3.624, 95% confidence interval [CI] [1.179–11.138] and OR 1.062, 95% CI [1.007–1.121]) and increased uterine scar thickness and RI were protective factors against hemorrhage (OR 0.181, 95% CI [0.034–0.957] and OR 0.851, 95% CI [0.729–0.994]); however, there was no statistical significance between the two clinical parameters.
Conclusion
Gestational mass size >6 cm, uterine scar thickness <0.2 cm, PSV >70 cm/s, and RI <0.35 are independent risk factors for excessive hemorrhage during the management of CSP.
Introduction
A particular complication of a pregnancy after cesarean delivery is the implantation of gestational sac in the scar, known as cesarean scar pregnancy (CSP).Citation1,Citation2 The incidence of CSP has been estimated to range from 1/1,800 to 1/2,500 of all cesarean deliveries.Citation3 To date, there is still no standard treatment. Proposed treatment includes medical interventions (injection of methotrexate [MTX]) and surgical interventions (uterine artery embolization [UAE], suction curettage, local CSP resection, and hysterectomy).Citation4–Citation6 Termination of pregnancy is recommended soon after confirmation of diagnosis, so as to avoid severe complications, such as uterine rupture and massive bleeding.
The results of management are encouraging, but not every patient’s uterus and future fertility could be preserved. Uncontrollable hemorrhage still occurs during the treatment. Therefore, it is of great necessity to identify the potential risk factors for massive hemorrhage. Several studies have reported that gestational age, serum β-human chorionic gonadotropin (HCG), size of gestational mass, thickness of myometrial layer, and peritrophoblastic perfusion are related to excessive hemorrhage.Citation7,Citation8 Ultrasound examination plays an important role in CSP. However, the previous grading system of blood flow was semi-quantitative (absent or mild, moderate, and significant), subjective to physicians according to ultrasonographic findings.
Our research is a case–control study, trying to evaluate both clinical and ultrasound parameters in predicting severe hemorrhage in CSP, especially the quantitative parameters for peritrophoblastic perfusion, in the hope of helping identifying patients at a high risk of bleeding and assisting decision making in the treatment of CSP.
Patients and methods
A case–control study was designed and conducted in Peking Union Medical College Hospital (PUMCH). Our research was approved by the ethics committee of PUMCH, who deemed written informed consent not necessary due to the retrospective nature of the study and all data being de-identified.
Patient selection
The study was based on information of patients admitted and diagnosed with CSP and treated by suction curettage between January 2007 and December 2014. During the 8 years, there were a total of 325 women diagnosed with CSP who were admitted to PUMCH. Excessive hemorrhage was defined as a blood loss >400 mL during the suction curettage according to the previous literatureCitation9 and the necessity for patients to receive at least one of the following additional interventions, including UAE plus secondary suction curettage, local CSP resection, and hysterectomy. In all, 40 patients with CSP having excessive hemorrhage during suction curettage were assigned to the case group (n=40). The control subjects were chosen with the use of computerized randomization through a 2:1 (control:case) random sample of all the other patients with CSP who received the same treatment during the same period, but who did not have a blood loss >400 mL during suction curettage that required additional interventions (n=80).
The patient information, including patient age at diagnosis, gravidity, parity, interval between current CSP and last cesarean, gestational age at diagnosis, pretreatment serum β-HCG level, gestational mass size, uterine scar thickness, peak systolic velocity (PSV), and resistance index (RI), was collected from the medical records and the clinical database.
Diagnosis of CSP
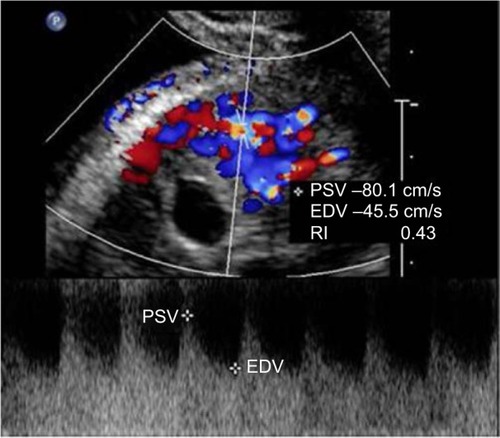
All patients included in our study were confirmed the diagnosis of CSP, based on the criteria postulated by Godin et al,Citation10 including: 1) a history of cesarean delivery; 2) positive serum β-HCG level; 3) visualization of an empty uterine cavity and cervical canal; 4) detection of the placenta or a well-formed gestational mass embedded in the scar; 5) lack of continuity of myometrial image between the bladder and the gestational mass; and 6) color Doppler ultrasound demonstrating blood flow surrounding the gestational mass. An ultrasound image of CSP is shown in .
Ultrasound examination
Ultrasound examinations were performed by color Doppler ultrasound diagnosis apparatus using a 5–9 MHz transvaginal probe (Phillips iU22, GE Logiq 9). Concerning the peritrophoblastic perfusion, both qualitative analysis of spectrograms identifying characteristic blood flow patterns and quantitative variables, including arterial PSV and RI, were detected and calculated (). All the data concerning ultrasound parameters included in our research were collected at diagnosis before the treatment of CSP.
Figure 2 Doppler waveforms of peritrophoblastic blood flow.
Abbreviations: PSV, peak systolic velocity; EDV, end diastolic velocity; RI, resistance index.
Statistical analyses
Statistical analyses were performed with SPSS software version 19, with statistical significance being accepted at P<0.05. Data on demographic characteristics were expressed as mean ± standard deviation. Quantitative variables were analyzed by using Student’s t-test or analysis of variance test (ANOVA) test. Qualitative variables were evaluated by using two-tailed χ2 test. Odds ratios (ORs) with 95% confidence intervals (CIs) were calculated by using logistic regression analysis.
Results
Demographic information
Statistical analyses showed no significant differences between the case group and the control group in the demographic information of patients, including the patients’ age at diagnosis (33.3±5.7 years vs 33.7±5.1 years), the gravidity (4.3±1.5 vs 4.1±1.2), the parity (1.4±0.5 vs 1.2±0.7), and the interval between the current CSP and last cesarean (63.4±52.4 months vs 55.6±44.3 months; ).
Table 1 Demographic comparison of patients with CSP
Management of CSP
In the control group, 80 patients only underwent suction curettage under the surveillance of ultrasound without additional interventions.
In the case group, 40 patients first received suction curettage under the surveillance of ultrasound and then needed additional interventions due to excessive hemorrhage. These patients were classified into three subgroups in accordance with their additional therapy, including the UAE plus secondary suction curettage subgroup (n=15, 37.5%), the local CSP resection subgroup (n=18, 45%), and the hysterectomy subgroup (n=7, 17.5%).
Blood loss during treatment of CSP
Overall, the mean bleeding volume was 1,440±955 mL vs 215±84 mL for the case group vs the control group, showing significant statistical difference with P=0.001. Specifically, in the case group, the mean bleeding volume was 621±165 mL, 966±328 mL, and 2,314±784 mL for the UAE plus secondary suction curettage subgroup, the local CSP resection subgroup, and the suction curettage subgroup, respectively, in an ascending order. Compared with the UAE plus secondary suction curettage subgroup, the latter two subgroups showed significantly much more blood loss, with P-values 0.048 and 0.001 ().
Table 2 Comparison of blood loss during management of CSP
Analyses of high-risk factors for excessive hemorrhage during treatment of CSP
For the case group and the control group, the mean gestational age at diagnosis was 74.1±23.6 days and 57.3±22.3 days, the mean pretreatment serum β-HCG level was 46,201±32,294 IU/mL and 24,189±10,584 IU/mL, the mean gestational mass size was 6.5±2.2 cm and 3.1±1.1 cm, the mean uterine scar thickness was 0.17±0.12 cm and 0.31±0.15 cm, the mean PSV was 72.8±33.7 cm/s and 47.5±23.8 cm/s, and the mean RI was 0.35±0.12 and 0.45±0.11, respectively. All the abovementioned clinical and ultrasound parameters between the case group and the control group showed significant differences ().
Table 3 High-risk factors for excessive hemorrhage during the management of CSP
The results of further multivariable logistic regression analyses are shown in . Statistically significant higher ORs were found for the gestational mass size (OR 3.624, 95% CI [1.179–11.138]) and the PSV (OR 1.062, 95% CI [1.007–1.121]) in the case group. Statistically significant lower ORs were found for the uterine scar thickness (OR 0.181, 95% CI [0.034–0.957]) and the RI value (OR 0.851, 95% CI [0.729–0.994]). However, the gestational age at diagnosis and the pretreatment serum β-HCG level did not show significant differences statistically.
Table 4 Results from multivariable logistic regression analysis of ORs, together with 95% CIs, for the risk of excessive hemorrhage
Discussion
Although many treatments have been suggested for CSP, severe hemorrhage still occurs in some patients. Various hemo-static measures have been used for prevention and control of profuse bleeding, such as local injection of vasopressin, intrauterine balloon tamponade, bilateral uterine artery ligation, and UAE.Citation11,Citation12 Even though, a small part of patients still experience excessive bleeding, even resulting in hysterectomy and loss of future fertility. Therefore, exploring and understanding the risk factors for severe hemorrhage in the treatment of CSP has a great significance in helping us counsel such patients and choose appropriate therapeutic interventions.
Color Doppler ultrasonography has widespread application in the diagnosis and treatment of CSP. It is a noninvasive, radiation-free, cost-effective technique that can be easily performed and frequently repeated. Ultrasound images could provide information on the size of gestational mass and the thickness of cesarean scar, as well as excellent visualization of the blood supply.Citation13 Previous grading system of blood flow (absent or mild, moderate, significant) is semiquantitative, made subjectively by physicians. Recently, ultrasound quantification of blood flow has been developed. In addition to qualitative analysis of spectrograms identifying characteristic blood flow patterns, quantitative variables such as arterial PSV and RI are also detected and calculated.Citation14 RI reflects the resistance to blood flow in the vessel influenced by vasoconstriction, dilation, or external vascular compression. PSV is influenced by respiratory variability, but RI, unlike measure of maximal and minimal velocities, is a ratio that is not altered by the angle of the Doppler and takes into account the direction and volume of blood flow. Therefore, the monitoring of both PSV and RI could reduce the inter-observer bias between patients.Citation14
In our study, we compared six parameters potentially related to hemorrhage, including two clinical parameters and four ultrasound parameters. Single-variable statistical analyses showed that the case group had larger gestational age, higher pretreatment serum β-HCG level, larger gestational mass size, thinner uterine scar thickness, and richer peritrophoblastic perfusion. Further multivariable logistic regression analysis of the association between each of the risk factors and hemorrhage confirmed that increased gestational mass size and PSV were risk factors for hemorrhage and increased uterine scar thickness and RI were protective factors against hemorrhage.
The results of the four ultrasonographic parameters in our research are consistent with several previous studies.Citation15,Citation16 Large gestational mass size could involve abundant blood supply, resulting in much more blood loss during the procedure.Citation15 Thin myometrial layer between the gestational mass and the bladder presented with an elevated risk of rupture and bleeding.Citation16,Citation17
Peritrophoblastic perfusion has a strong association with hemorrhage, and its importance has been paid more and more attention on. The cesarean scar is due to lack of decidual tissue, and it is easy for the chorionic tissue to implant into the myometrium layer of the uterus, resulting in rich blood perfusion around the gestational mass.Citation4,Citation18 Grading of blood flow could reflect the density of newly formed blood vessels and decide the possibility of vascular rupture, predicting the risk of hemorrhage.Citation4,Citation18 To our best knowledge, there has been little information about quantitative parameters for peritrophoblastic perfusion. In our study, we detected and collected two quantitative parameters, PSV and RI, to evaluate the risk of massive hemorrhage. It is observed that higher PSV and lower RI are independent risk factors for uncontrollable hemorrhage, with OR 1.062 (1.007–1.121) and 0.851 (0.729–0.994), respectively.
However, the two clinical parameters, gestational age at diagnosis and pre-treatment serum β-HCG level, were not independent risk factors for severe hemorrhage after multi-variable regression analyses. Whether these two parameters are associated with massive hemorrhage during the procedure is still controversial.Citation7,Citation8 It is possible that, since the gestational mass implants in the cesarean scar, maldevelopment of chorionic villi may cause disproportion to the gestational age and blood flow. Serum β-HCG level is a biochemical index reflecting the activity of trophoblastic cells, but lower activity of trophoblastic cells could be accompanied by abundant neovascularization. In addition, our sample size was small, and further studies with larger sample sizes should be performed.
Our study also had some limitations. First, there might be other risk factors that we did not consider but could influence the final results of multivariable logistic regression analyses. Second, although four independent risk factors for excessive hemorrhage were identified, our study did not put forward a practicable and easy-to-use evaluation protocol that could help clinicians to assess and identify patients at a high risk of massive bleeding and to assist decision-making for the treatment of CSP. Third, further prospective studies in multiple medical institutions will be needed to validate our research findings.
Conclusion
During the management of CSP, gestational mass size >6 cm, uterine scar thickness <0.2 cm, PSV >70 cm/s, and RI <0.35 are independent risk factors for excessive hemorrhage.
Acknowledgments
This study was supported by the Capital Medical Development Foundation of China (No 2016-2-4015) and National Natural Science Foundation of China (No 81402140). The authors thank Dr Zhenzhen Liu and Dr Xining Wu for their assistance in relation to ultrasound examination of cesarean scars in pregnancy.
Disclosure
The authors report no conflicts of interest in this work.
References
- JurkovicDHillabyKWoelferBLawrenceASalimRElsonCJFirst trimester diagnosis and management of pregnancies implanted into the lower uterine segment cesarean section scarUltrasound Obstet Gynecol200321322022712666214
- JurkovicDHillabyKWoelferBLawrenceASalimRElsonCJCesarean scar pregnancyUltrasound Obstet Gynecol200321331012666232
- Timor-TritschIEMonteagudoAUnforeseen consequences of the increasing rate of cesarean deliveries: early placenta accreta and cesarean scar pregnancy. A reviewAm J Obstet Gynecol20122071142922516620
- Timor-TritschIEMonteagudoASantosRTsymbalTPinedaGArslanAAThe diagnosis, treatment, and follow-up of cesarean scar pregnancyAm J Obstet Gynecol2012207144.e144.e1322607667
- RotasMAHabermanSLevgurMCesarean scar ectopic pregnancies: etiology, diagnosis, and managementObstet Gynecol200610761373138116738166
- LitwickaKGrecoECesarean scar pregnancy: a review of management optionsCurr Opin Obstet Gynecol20112341542122011956
- DuYJZhangXHWangLQRisk factors for hemorrhage during suction curettage after uterine artery embolization for treating cesarean scar pregnancy: a case-control studyGynecol Obstet Invest201580425926425926054
- WangQMaHPengHHeLBianCZhaoXRisk factors for intra-operative hemorrhage and bleeding risk scoring system for cesarean scar pregnancy: a case-control studyEur J Obstet Gynecol Reprod Biol201519514114526544025
- LiKNDaiQLiuZZSuNWangMJiangYXClinical value of ultrasonography in predicting massive hemorrhage during cesarean scar pregnancyZhongguo Yi Xue Ke Xue Yuan Xue Bao20153758559026564512
- GodinPABassilSDonnezJAn ectopic pregnancy developing in a previous cesarean section scarFertil Steril1997673984009022622
- JiangTLiuGHuangLMaHZhangSMethotrexate therapy followed by suction curettage followed by Foley tamponade for caesarean scar pregnancyEur J Obstet Gynecol Reprod Biol2011156220921121392878
- LeAShanLXiaoTZhuoRXiongHWangZTransvaginal surgical treatment of cesarean scar ectopic pregnancyArch Gynecol Obstet2013287479179623143407
- Bij de VaateAJBrolmannHAvan der VoetLFvan der SlikkeJWVeersemaSHuimeJAUltrasound evaluation of the cesarean scar: relation between a niche and postmenstrual spottingUltrasound Obstet Gynecol2011371939921031351
- RiggsBJCohenJSShivakumarBDoppler ultrasonography of the central retinal vessels in children with brain deathPediatr Crit Care Med201718325826428114163
- WangJHQianZDZhuangLYDuYJZhuLHHuangLLRisk factors for intraoperative hemorrhage at evacuation of a cesarean scar pregnancy following uterine artery embolizationInt J Gynecol Obstet20131233240243
- ShaoMJHuMXXuXJZhangLHuMManagement of cesarean scar pregnancies using an intrauterine or abdominal approach based on the myometrial thickness between the gestational mass and the bladder wallGynecol Obstet Invest20137615115723949246
- ChenWLJinLSuccessful treatment of endogenous cesarean scar pregnancies with transabdominal ultrasound-guided suction curettage aloneEur J Obstet Gynecol Reprod Biol2014183202225461346
- ZhaiJFXuMZhangBGaoJWChenNTreatments of cesarean scar pregnancy and the corresponding results in ten yearsEur Rev Med Pharmacol Sci201519142523252726221877

