Abstract
While laparoscopic cholecystectomy is generally accepted as the treatment of choice for simple gallbladder stones, in cases in which common bile duct stones are also present, clinical and diagnostic elements, along with intraoperative findings, define the optimal means of treatment. All available options must be accessible to the surgical team which must necessarily be multidisciplinary and include a surgeon, an endoscopist, and a radiologist in order to identify the best option for a truly personalized surgery. This review describes the different techniques and approaches used based on distinctive recommendations and factors, according to the specific cases treated and the results achieved.
Introduction
The study of the anatomy of the biliary tract has always attracted the interest of numerous scientists, from Leonardo da Vinci to Abraham Vater (1790) although the first cholecystectomy was reported in 1882 by Langenbuc.Citation1 The progress made in recent decades has completely changed surgical approaches, especially with the advent of endoscopic and laparoscopic surgery. Today, the treatment of gallstone disease often requires a multidisciplinary approach involving a surgeon, an endoscopist, and a radiologist.Citation2
While laparoscopic cholecystectomy (LC) is the treatment of choice for gallbladder stones,Citation3 in those cases in which common bile duct (CBD) stones are also present (~10% of the overall cases) treatment options are still open to discussion.Citation4,Citation5 During the last 20 years, CBD stones were treated through endoscopic retrograde cholangiopan-creatography (ERCP) which was proposed pre- or postcholecystectomy.Citation6 However, despite the good results, several issues did arise such as the number of unnecessary procedures (10%),Citation7 the not negligible complications’ rate (between 0.8% and 11.1%),Citation9 and the mortality rate (between 0.1% and 3.3%).Citation8–Citation10
The rapid expansion of laparoscopic surgery also demonstrated that it was possible to resolve cholecysto-choledocolithiasis through a single-stage approach.Citation11 Indeed, there are currently two treatment options for gallbladder and CBD stones: a single- or double-stage procedure. Studies have shown that results are similar in terms of efficacy, morbidity, and mortality.Citation12,Citation13
However, it is now reported that single-stage treatment lowers costs with a shorter hospital stay and improves patient compliance.Citation14,Citation15 Additionally, the issue linked to the unexpected diagnosis of CBD stones remains, as the maximum accuracy of preoperative studies only reaches 80%–90% of the overall cases.Citation16 There is also a possibility that the CBD stones pass through the papilla spontaneously.Citation17 Therefore, the single-stage treatment allows the clearance of unsuspected CBD stones.Citation18
The single-stage approach is particularly interesting because it has not been standardized and presents various technical options with a varying degree of complexity, from both a manual and technological standpoint, which depend on the method used.
In this review, we describe all the technical options currently available for the laparoscopic removal of gallbladder and CBD stones in a single procedure and analyze the results obtained.
We assess the degree of complexity of the methods and the clinical indications and instruments required for the best approach in each individual case.
Methods
A complete clearance of the bile duct via a laparoscopic approach in a single session can be obtained using three techniques:
trans-cystic laparoscopic bile duct clearance (TC-CBDE);
laparoscopic common bile duct exploration (LCBDE); and
rendezvous intraoperative endoscopic retrograde cholangiography (RV-IOERC).
Intraoperative techniques TC-CBDE
LC was performed using four trocars. After preparing the cystic duct and visualizing the bile duct, a fifth trocar cholangiography (intraoperative cholangiography [IOC]) was introduced through a small incision of the cystic duct and the catheter was secured by a clip. Once the diagnosis of lithiasis of the bile duct was confirmed (through IOC), the catheter was removed and drainage was performed via trans-cystic washing, passing through the Dormia basket, the balloon, and using, if necessary, a 3 mm choledoscope. In some cases, because the trans-cystic pathway required pneumatic dilation of the sphincter of Oddi to facilitate the passage of stones, a trans-cystic drain was left in place and removed at a later stage. At the end of the procedure, an IOC was performed to confirm correct clearance. A subhepatic drainage was left in place ().
RV-IOERC
Both procedures (single or double stage) were similar until the cholangiography demonstrated the presence of CBD stones. At that point, we proceeded with the partial freeing of the gallbladder from the liver bed. The surgeon introduced a guide wire into the gallbladder while the endoscopist, without changing the patient’s position, positioned the endoscope. Once the guide wire was confirmed to have reached the papilla, and the papilla was identified, the endoscopist extracted the guide wire and, using it as a guide, introduced the unit for the papillotomy, which was performed safely. The area was washed and the Dormia basket was employed. The surgeon withdrew the guide wire. At the end of the procedure, the endoscopist removed the gas previously introduced. A cholangiography was then performed to examine the drainage of the bile ducts. Finally, the surgeon completed the cholecystectomy ().
LCBDE
The bile duct was prepared after confirming the presence of CBD stones. A vertical choledochotomy with a length of about 1–1.5 cm was performed. We proceeded with the clearance of the bile duct through washing and direct extraction of the stones. In the presence of impacted stones, a lithotripter was used. We evaluated the effectiveness of the clearance using a choledoscope. The choledochotomy was closed with a running suture after positioning a T-tube that was left in place for about 3 weeks and then removed after cholangiography. In certain cases, direct closure of the choledochotomy was proposed. The subhepatic drainage was left in place ().
The confirmation of concomitant stones of the CBD was obtained intraoperatively by performing a cholangiography (IOC). There is a consensus on the execution of IOC only in suspected casesCitation19 and, although other methods can be used, they do not have the same sensitivity and specificity. Magnetic resonance cholangiopancreatography is the most sensitive, but has a significantly higher cost as well as a resolving power which cannot detect stones smaller than 0.5 cm.Citation20 The use of laparoscopic probes for intraoperative ultrasound studies was reported to produce very good results.Citation21 However, the use of this method is not very widespread because of its high costs.
Trans-cystic clearance is the most natural method to clear the bile duct. In the vast majority of cases, the stones migrate from the gallbladder and can therefore be removed via the same physiological course. This technique also respects the integrity of the sphincter of Oddi, particularly important in young patients.Citation22
The success rate of the trans-cystic approach for the removal of CBD stones is around 75% of the cases treated.Citation23 One study reported a higher effectiveness of the method (85%–90%) with a rate conversion of 10%.Citation24 The mean operative time was 115±40 minutes.Citation25
Long-term results are also positive with a minimum percentage (3.1%) of recurrence.Citation26 Obviously, trans-cystic clearance cannot be performed in the presence of stones with a diameter >1 cm, although it was shown by Vracko and Wiechel that, in 90% of the cases, the diameter of the CBD stones did not exceed by >1 mm the diameter of the cystic duct.Citation27 Trans-cystic clearance requires experience and the use of suitable laparoscopic instruments such as the Dormia basket, the balloon catheter, and washings. Another instrument which is very useful is the choledoscope (3 mm) that is effective for the removal of the stones and in the assessment of complete clearance, although it remains difficult to examine the bile duct above the insertion of the cystic duct.
For this reason, IOC is advisable upon completion of surgery. The rate of major complications (bile leak) was 2.8%, while the minor complications were around 5%. The mortality rate was about 0%–1%. The average hospital stay was 48 hours.Citation28,Citation29
Failure of the trans-cystic approach was due to local inflammation and anatomical constraints, as well as due to the number and size of the stones.Citation30 Other risk factors were jaundice and comorbidity.Citation31
There are other technical aids which are useful in trans-cystic clearance: in the presence of small stones (<0.6 cm), some authors undertook trans-cystic pneumatic dilation of the papilla to facilitate the expulsion of the stones.Citation32
The RV-IOERC method was reported to be particularly indicated in bile duct clearance. It is important to adequately define this technique because the guide wire used in the “rendezvous” distinguishes this method from simple papillotomy. As reported by La Greca et al, not everyone uses this technique, but many perform a simple intraoperative papillotomy after LC.Citation33 For this reason, it is difficult to compare the various reported results. Many reports, however, showed the superiority of this method compared to the double-stage approach.Citation34
This technique also reduced the incidence of post-ERCP pancreatitis.Citation35 In RV-IOERC, the sphincter of Oddi is destroyed; this can have important consequences in young patients.Citation36
The duration of the endoscopic portion of RV-IOERC varied between 9 and 82 minutes (mean 35 minutes) and, of course, the presence of an endoscopist in the operating room was necessary. The success rate was very high (92.3%) with reduction of the hospital stay.Citation37 Certainly, in the presence of concomitant stenosis of the sphincter of Oddi, RV-IOERC becomes an absolute indication.
The complication rate was on average 5.1% with a conversion rate of 4.7% and recurrence rate of 1%.Citation38
In cases in which a combined laparoscopic–endoscopic approach is used, when papillotomy is performed before or after the LC, it is necessary to change the position of the patient with a further loss of time.Citation39
The direct approach to the bile duct through choledochotomy must be reserved in cases of a CBD caliber >1 cm, thickened walls, and in the presence of numerous stones having a diameter >1 cm.Citation40 This method is technically more difficult, with a longer operative time,Citation41 but it maintains the integrity of the sphincter of Oddi. The choledoscope proved useful also in this approach as it allowed the inspection of the intrahepatic bile ducts. With this method, the percentage of success was high (96.7%) with a rate of postoperative bile leak of 3.3% and reduced complications (8%).Citation42
The closure of a choledochotomy requires the positioning of a T-tube sec Kehr which is removed after about 3 weeks. This technique has recently been replaced by the proposal of direct closure of the CBD. Many reports showed that this approach was safe and reduced both operative time and hospital stay.Citation43,Citation44 Factors that negatively affected the results were jaundice and comorbidities with a conversion rate of 8.3%. Postoperative hospital stay varied between 3 and 12 days and depended on the use of a T-tube and on complications.Citation45
Discussion
A consensus in the optimal treatment of gallbladder and bile duct stones has not been reached. Normally, symptoms (which include pain, jaundice, and cholangitis, along with the presurgical workup) lead to a diagnosis. In some cases, however, the discovery of CBD stones can be a fortuitous finding during LC. The first issue is whether or not to treat the CBD stones even if they are asymptomatic.
Although it was reported that approximately one third of the stones with a diameter <6 mm pass spontaneously,Citation17 there are no highly indicative prognostic factors to quantify this possibility. Therefore, as stated in the European Association of Endoscopic Surgery consensus, all cases of bile duct stones discovered during LC should be treated.Citation46
Another preliminary aspect that must be clarified is how to diagnose CBD stones. Performing a routine IOC in all patients who undergo LC is not recommended since it will not reduce the lesions of the bile ducts and asymptomatic gallbladder stones are rare.Citation47 There is no unanimous consensus and some authors report a minor incidence of biliary lesion with the routine use of IOC.Citation48 Therefore, we propose IOC only in suspected cases, also because it is more sensitive than preoperative magnetic resonance cholangiography.Citation49 Intraoperative ultrasound is another reliable and sensitive method although it is not widespread due to its high cost and a long learning curve.Citation50
When a diagnosis of cholecysto-choledocolithiasis has been confirmed, treatment must be chosen. There are many possibilities to obtain complete clearance. In the past, the treatment of choice was a sequential two-step procedure in which clearance was achieved by performing an ERCP first and an LC later. This is currently still the most widespread methodCitation51 and can produce good results. However, we must remember the high number of unnecessary tests and the non-negligible increase in major complications and mortality.Citation52 The consequences linked to the loss of function of the sphincter of Oddi are also relevant.Citation53
The expanding skills in laparoscopic surgery have made it possible to treat gallbladder and bile duct stones in a single step. In recent years, this method has attracted considerable attention. The advantages are a reduction in cost and better patient compliance.Citation54
In this review, single-stage management methods of CBD stones are described, evaluating indications, results, and technical and organizational complexity. Trans-cystic clearance is the simplest approach and is recommended in the majority of cases.Citation55 It has clear indications regarding the size and number of stones and requires a good laparoscopic technique and a minimum organizational commitment.Citation56 It yields good results also in the case of acute cholecystitis.Citation57 When trans-cystic clearance cannot be performed, two techniques can be used: direct access to the CBD and RV-IOERC.
Both are methods that require a greater amount of time.Citation58 Laparoscopic choledochotomy is technically more difficult,Citation59 while RV-IOERC requires the presence of an endoscopist and therefore considerably more organization.Citation60
Even with these methods there are absolute indications: in the case of concomitant papillary stenosis, RV-IOERC is more indicated, while in the presence of stones that are larger than 1 cm and a dilated CBD, choledochotomy is preferable.
There are very few studies that compare these techniques. Another difficulty stems from the nonuniform terminology used in the literature: often in intraoperative papillotomy, the guide wire is not used.Citation39 Additionally, with the term “CBD exploration,” it is not clear if access is trans-cystic or through a choledochotomy.Citation61
Undoubtedly, the methods used require specific technical skills that cannot be extended to all centers without proper training. In particular, the method of rendezvous involves the presence of an endoscopist in the operating room and this is difficult to arrange in many centers.
Hong et al compared the laparoscopic exploration of the bile duct with intraoperative papillotomy and did not find differences in terms of surgical time, postoperative complications, retained CBD stones, and hospital stay.Citation61 In a review by La Greca et al, RV-IOERC appeared to decrease the risk of residual stones compared to choledochotomy.Citation38 In a study by ElGeidie et al, two groups of patients underwent either intraoperative papillotomy or direct clearance of the biliary tract yielding equivalent results in terms of success rate, surgical time, and hospital stay.Citation62 In our work, we compared the trans-cystic clearance with RV-IOERC and did not find differences in terms of success rate and postoperative complications. However, the surgical time was significantly longer and the cost was higher in the group who underwent RV-IOERC.Citation63
In general, trans-cystic access to the bile duct is the method most widely used especially in Western countries, while in Eastern countries this approach is restricted to a few cases, probably due to a difference in the natural progression of the disease.Citation65
Direct approach to the bile duct is technically more difficult, resulting in increased intraoperative time and hospital stay, especially when a T-tube is used.Citation66 Several studies have, however, reported that it was possible to use a direct closure of the CBD to save time.Citation67 There are conditions in which the use of a T-tube is essential, for example, when the diameter of the CBD is <1 cm, the walls are thin, and the biliary outflow is uncertain. In the various reported cases, the percentage of choledochotomy that is closed earlier than expected is about 30%–40% of the total.Citation55 However, as indicated by Cochrane in 2013, multiple randomized trials with long-term results are required in order to exclude complications such as biliary stricture or recurrence.Citation67
A multicenter study should be used to evaluate preoperative conditions indicating which technique is the most appropriate for that specific clinical case, also because the centers do not always have at their disposal all available methods.
RV-IOERC is the treatment that requires the most organization and is therefore not very widespread.Citation39 The success rate is greater and the number of complications is reduced compared to sequential treatment.Citation69,Citation70 Jaundice and the presence of comorbidities are negative factors in this technique.Citation71,Citation72 Close cooperation between the surgeon and the endoscopist is absolutely necessary. This approach reduces the risk of the destruction of the sphincter of Oddi in young patients.
The treatment in a single step of the gallbladder and bile duct stones includes several techniques that together allow the treatment of almost all cases.Citation72 The degree of technical difficulty and organizational requirements undoubtedly vary among the various techniques and the most suitable approach to treat each individual case should be chosen. It is very difficult to compare the different techniques because the reported cases are not homogeneous and often report different methods.
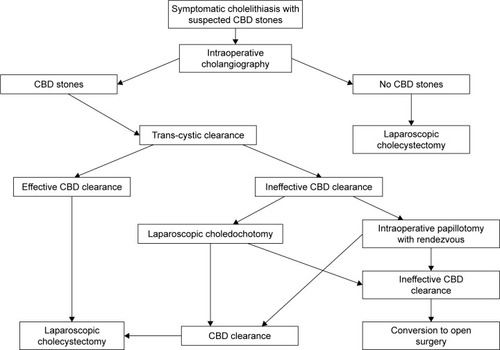
The clinical and diagnostic characteristics, along with intraoperative findings, define the ideal technique to be used, as shown in a flowchart ().
Figure 4 Flowchart for the treatment of cholecysto-choledocolithiasis.
A team that intends to treat cholecysto-choledocolithiasis should ideally work and cooperate closely with interdisciplinary collaborations. In other words, the surgeon should collaborate closely with an endoscopist and a radiologist.
The approach in a single step is therefore the method of choice in the treatment of gallbladder and CBD stones and all available options must be accessible to the surgical team. Subsequent studies should indicate the predictive parameters in order to choose the best option for a truly personalized surgery.
Disclosure
The authors report no conflict of interests in this work.
References
- GlennFGrafeWRJrHistorical events in biliary tract surgeryArch Surg19669358488525331876
- FletcherDRChanges in the practice of biliary surgery and ERCP during the introduction of laparoscopic cholecystectomy to Australia: their possible significanceAust N Z J Surg199464275808291982
- CervantesJRojasGAntonJChanges in gallbladder surgery: comparative study 4 years before and 4 years after laparoscopic cholecystectomyWorld J Surg19972122012048995079
- AttiliAFCarulliNRodaEEpidemiology of gallstone disease in Italy: prevalence data of the Multicenter Italian Study on Cholelithiasis (M.I.COL.)Am J Epidemiol199514121581657817971
- MartinDJVernonDRToouliJSurgical versus endoscopic treatment of bile duct stonesCochrane Database Syst Rev20062CD003327
- CisekPLGreaneyGCThe role of endoscopic retrograde cholangiopancreatography with laparoscopic cholecystectomy in the management of choledocholithiasisAm Surg199460107727767524385
- LoperfidoSAngeliniGBenedettiGMajor early complications from diagnostic and therapeutic ERCP: a prospective multicenter studyGastrointest Endosc19984811109684657
- CottonPBLehmanGVennesJEndoscopic sphincterotomy complications and their management: an attempt at consensusGastrointest Endosc19913733833932070995
- SalminenPLaineSGullichsenRSevere and fatal complications after ERCP: analysis of 2555 procedures in a single experienced centerSurg Endosc20082291965197018095023
- SiikiATamminenATomminenTKuusanmäkiPERCP procedures in a Finnish community hospital: a retrospective analysis of 1207 casesScand J Surg20121011455022414468
- PetelinJBLaparoscopic common bile duct explorationSurg Endosc200317111705171512958681
- AlexakisNConnorSMeta-analysis of one- vs. two-stage laparoscopic/endoscopic management of common bile duct stonesHPB (Oxford)201214425425922404264
- LuJChengYXiongXZLinYXWuSJChengNSTwo-stage vs single-stage management for concomitant gallstones and common bile duct stonesWorld J Gastroenterol201218243156316622791952
- TopalBVrommanKAertsRVerslypeCVan SteenbergenWPenninckxFHospital cost categories of one-stage versus two-stage management of common bile duct stonesSurg Endosc201024241341619554369
- RogersSJCelloJPHornJKProspective randomized trial of LC+LCBDE vs ERCP/S+LC for common bile duct stone diseaseArch Surg20101451283320083751
- ShiozawaSTsuchiyaAKimDHUseful predictive factors of common bile duct stones prior to laparoscopic cholecystectomy for gallstonesHepatogastroenterology200552661662166516334752
- CollinsCMaguireDIrelandAFitzgeraldEO’SullivanGCA prospective study of common bile duct calculi in patients undergoing laparoscopic cholecystectomy: natural history of choledocholithiasis revisitedAnn Surg20042391283314685097
- PhillipsEHToouliJPittHASoperNJTreatment of common bile duct stones discovered during cholecystectomyJ Gastrointest Surg200812462462818176853
- HorwoodJAkbarFDavisKMorganRProspective evaluation of a selective approach to cholangiography for suspected common bile duct stonesAnn R Coll Surg Engl201092320621020223077
- RichardFBoustanyMBrittLDAccuracy of magnetic resonance cholangiopancreatography for diagnosing stones in the common bile duct in patients with abnormal intraoperative cholangiogramsAm J Surg2013205437137323518180
- MachiJOishiAJTajiriTMurayamaKMFurumotoNLOishiRHRoutine laparoscopic ultrasound can significantly reduce the need for selective intraoperative cholangiography during cholecystectomySurg Endosc200721227027417122981
- TanakaMTakahataSKonomiHLong-term consequence of endoscopic sphincterotomy for bile duct stonesGastrointest Endosc19984854654699831833
- NathansonLKO’RourkeNAMartinIJPostoperative ERCP versus laparoscopic choledochotomy for clearance of selected bile duct calculi: a randomized trialAnn Surg2005242218819216041208
- KarvounisEGriniatsosJArnoldJAtkinGIslaAMWhy does laparoscopic common bile duct exploration fail?Int Surg2006912909316774179
- LyassSPhillipsEHLaparoscopic transcystic duct common bile duct explorationSurg Endosc200620Suppl 2S441S44516544067
- PaganiniAMGuerrieriMSarnariJThirteen years’ experience with laparoscopic transcystic common bile duct exploration for stones. Effectiveness and long-term resultsSurg Endosc2007211344017111284
- VrackoJWiechelKLHow often might a trans-cystic-duct stone extraction be feasible?Surg Endosc199812112159419296
- HanifFAhmedZSamieMANassarAHLaparoscopic transcystic bile duct exploration: the treatment of first choice for common bile duct stonesSurg Endosc20102471552155620044767
- Rojas-OrtegaSArizpe-BravoDMarín LópezERCesin-SánchezRRomanGRGómezCTranscystic common bile duct exploration in the management of patients with choledocholithiasisJ Gastrointest Surg20037449249612763406
- CuschieriADuctal stones: pathology, clinical manifestations, laparoscopic extraction techniques, and complicationsSemin Laparosc Surg20007424626111323762
- StrömbergCNilssonMLeijonmarckCEStone clearance and risk factors for failure in laparoscopic transcystic exploration of the common bile ductSurg Endosc20082251194119918363068
- MasoniLMariFSPietropaoloVOnoratoMMeucciMBresciaALaparoscopic treatment for unsuspected common bile duct stones by transcystic sphincter of Oddi pneumatic balloon dilation and pressure-washing techniqueWorld J Surg20133761258126223474857
- La GrecaGBarbagalloFDi BlasiMLaparo-endoscopic “Rendezvous” to treat cholecysto-choledocolithiasis: effective, safe and simplifies the endoscopist’s workWorld J Gastroenterol200814182844285018473408
- JonesMJohnsonMSamourjianESchlauchKOzobiaNERCP and laparoscopic cholecystectomy in a combined (one-step) procedure: a random comparison to the standard (two-step) procedureSurg Endosc20132761907191223239300
- ArezzoAVettorettoNFamigliettiFMojaLMorinoMLaparoen-doscopic rendezvous reduces perioperative morbidity and risk of pancreatitisSurg Endosc20132741055106023052536
- WuSDZhangZHLiDYNitroester drug’s effects and their antagonistic effects against morphine on human sphincter of Oddi motilityWorld J Gastroenterol200511152319232315818745
- TzovarasGBaloyiannisIZachariELaparoendoscopic rendezvous versus preoperative ERCP and laparoscopic cholecystectomy for the management of cholecysto-choledocholithiasis: interim analysis of a controlled randomized trialAnn Surg2012255343543922261836
- La GrecaGBarbagalloFSofiaMLatteriSRusselloDSimultaneous laparoendoscopic rendezvous for the treatment of cholecystocholedocholithiasisSurg Endosc2010244769780
- RábagoLRVicenteCSolerFTwo-stage treatment with preoperative endoscopic retrograde cholangiopancreatography (ERCP) compared with single-stage treatment with intraoperative ERCP for patients with symptomatic cholelithiasis with possible choledocholithiasisEndoscopy200638877978617001567
- BerthouJCDrouardFCharbonneauPMoussalierKEvaluation of laparoscopic management of common bile duct stones in 220 patientsSurg Endosc199812116229419297
- LillyMCArreguiMEA balanced approach to choledocholithiasisSurg Endosc200115546747211353963
- KhaledYSMaldeDJde SouzaCKaliaAAmmoriBJLaparoscopic bile duct exploration via choledochotomy followed by primary duct closure is feasible and safe for the treatment of choledocholithiasisSurg Endosc201327114164417023719974
- ChenCCWuSDTianYSiwoEAZengXTZhangGHSphincter of Oddi-preserving and T-tube-free laparoscopic management of extrahepatic bile duct calculiWorld J Surg201135102283228921779932
- YinZXuKSunJIs the end of the T-tube drainage era in laparoscopic choledochotomy for common bile duct stones is coming? A systematic review and meta-analysisAnn Surg20132571546623059495
- YeXHongXNiKTengXXieKPreoperative factors predicting poor outcomes following laparoscopic choledochotomy: a multivariate analysis studyCan J Surg201356422723223883491
- Scientific Committee of the European Association for Endoscopic Surgery (EAES)Diagnosis and treatment of common bile duct stones (CBDS). Results of a consensus development conferenceSurg Endosc19981268568649602006
- FordJASoopMDuJLovedayBPRodgersMSystematic review of intraoperative cholangiography in cholecystectomyBr J Surg201299216016722183717
- SlimKMartinGDoes routine intra-operative cholangiography reduce the risk of biliary injury during laparoscopic cholecystectomy? An evidence-based approachJ Visc Surg2013150532132423911201
- BuddinghKTNieuwenhuijsVBvan BuurenLHulscherJBde JongJSvan DamGMIntraoperative assessment of biliary anatomy for prevention of bile duct injury: a review of current and future patient safety interventionsSurg Endosc20112582449246121487883
- BrownLMRogersSJCelloJPBraselKJInadomiJMCost-effective treatment of patients with symptomatic cholelithiasis and possible common bile duct stonesJ Am Coll Surg2011212610491060e1e721444220
- PhillipsEHLibermanMCarrollBJFallasMJRosenthalRJHiattJRBile duct stones in the laparoscopic era. Is preoperative sphincterotomy necessary?Arch Surg19951308880885 discussion 885–8867632150
- BergmanJJvan der MeySRauwsEALong-term follow-up after endoscopic sphincterotomy for bile duct stones in patients younger than 60 years of ageGastrointest Endosc19964466436498979051
- BansalVKMisraMCGargPPrabhuMA prospective randomized trial comparing two-stage versus single-stage management of patients with gallstone disease and common bile duct stonesSurg Endosc20102481986198920135172
- BerthouJCHDronBCharbonneauPMoussalierKPellissierLEvaluation of laparoscopic treatment of common bile duct stones in a prospective series of 505 patients: indications and resultsSurg Endosc200721111970197417522929
- BoveABongarzoniGPaloneGWhy is there recurrence after transcystic laparoscopic bile duct clearance? Risk factor analysisSurg Endosc20092371470147519263129
- ChiarugiMGalatiotoCDecaniniLLaparoscopic transcystic exploration for single-stage management of common duct stones and acute cholecystitisSurg Endosc201226112412921792715
- SaccomaniGDuranteVMagnoliaMRCombined endoscopic treatment for cholelithiasis associated with choledocholithiasisSurg Endosc200519791091415868278
- SalmRWaningerJMaternUFarthmannEHLaparoscopic techniques in therapy of choledocholithiasisChirurg1994655418423 German8050294
- MeyerCLeJVRohrSDuclosBReimundJMBaumannRManagement of common bile duct stones in a single operation combining laparoscopic cholecystectomy and peroperative endoscopic sphincterotomyJ Hepatobiliary Pancreat Surg20029219620012140606
- TinocoRTinocoAEl-KadreLPeresLSuethDLaparoscopic common bile duct explorationAnn Surg2008247467467918362631
- HongDFXinYChenDWComparison of laparoscopic cholecystectomy combined with intraoperative endoscopic sphincterotomy and laparoscopic exploration of the common bile duct for cholecystocho-ledocholithiasisSurg Endosc200620342442716395539
- ElGeidieAAElShobaryMMNaeemYMLaparoscopic exploration versus intraoperative endoscopic sphincterotomy for common bile duct stones: a prospective randomized trialDig Surg2011285–642443122236538
- BoveADi RenzoRMPaloneGA comparative study of minimally invasive treatment of cholecystocholedocholithiasisAm Surg2013793E108E11023461932
- ChanderJVindalALalPGuptaNRamtekeVKLaparoscopic management of CBD stones: an Indian experienceSurg Endosc201125117218120535498
- LezocheEPaganiniAMTechnical considerations and laparoscopic bile duct exploration: transcystic and choledochotomySemin Laparosc Surg20007426227811323763
- WuXYangYDongPPrimary closure versus T-tube drainage in laparoscopic common bile duct exploration: a meta-analysis of randomized clinical trialsLangenbecks Arch Surg2012397690991622644601
- GurusamyKSKotiRDavidsonBRT-tube drainage versus primary closure after laparoscopic common bile duct explorationCochrane Database Syst Rev20136CD005641
- SwahnFRegnérSEnochssonLEndoscopic retrograde cholangiopancreatography with rendezvous cannulation reduces pancreatic injuryWorld J Gastroenterol201319366026603424106403
- GurusamyKSSahaySJBurroughsAKDavidsonBRSystematic review and meta-analysis of intraoperative versus preoperative endoscopic sphincterotomy in patients with gallbladder and suspected common bile duct stonesBr J Surg201198790891621472700
- TricaricoACioneGSozioMEndolaparoscopic rendezvous treatment: a satisfying therapeutic choice for cholecystocholedocolithiasisSurg Endosc200216458558811972193
- NobleHWhitleyENortonSThompsonMA study of preoperative factors associated with a poor outcome following laparoscopic bile duct explorationSurg Endosc201125113013920567852
- LiMKTangCNLaiECManaging concomitant gallbladder stones and common bile duct stones in the laparoscopic era: a systematic reviewAsian J Endosc Surg201142535822776221



