Abstract
Novel antiplatelet drugs, including ticagrelor, are being successively introduced into the therapy of atherothrombotic conditions due to their superiority over a standard combination of clopidogrel with acetylsalicylic acid in patients with acute coronary syndromes (ACS). A P2Y12 receptor antagonist, ticagrelor, is unique among antiplatelet drugs, because ticagrelor inhibits the platelet P2Y12 receptor in a reversible manner, and because it demonstrates a wide palette of advantageous pleiotropic effects associated with the increased concentration of adenosine. The pleiotropic effects of ticagrelor comprise cardioprotection, restoration of the myocardium after an ischemic event, promotion of the release of anticoagulative factors and, eventually, anti-inflammatory effects. Beyond the advantageous effects, the increased concentration of adenosine is responsible for some of ticagrelor’s adverse effects, including dyspnea and bradycardia. Large-scale clinical trials demonstrated that both standard 12-month therapy and long-term use of ticagrelor reduce the risk of cardiovascular events in patients with ACS, but at the expense of a higher risk of major bleeding. Further trials focused on the use of ticagrelor in conditions other than ACS, including ischemic stroke, peripheral artery disease and status after coronary artery bypass grafting. The results of these trials suggest comparable efficacy and safety of ticagrelor and clopidogrel in extra-coronary indications, but firm conclusions are anticipated from currently ongoing studies. Here, we summarize current evidence on the superiority of ticagrelor over other P2Y12 antagonists in ACS, discuss the mechanism underlying the drug–drug interactions and pleiotropic effects of ticagrelor, and present future perspectives of non-coronary indications for ticagrelor.
Introduction
Activation of platelets on a ruptured or eroded atherosclerotic plaque is a key event in atherothrombosis, including acute coronary syndromes (ACS) and acute ischemic stroke (AIS).Citation1 Beyond thrombus formation, activated platelets trigger and disseminate vascular inflammation by exposure and release of pro-inflammatory molecules, thereby contributing to the progression of atherosclerosis. Platelet P2Y12 receptors for adenosine diphosphate (ADP) are essential for platelet activation.Citation2 For this reason, dual antiplatelet therapy (DAPT) comprising acetylsalicylic acid (ASA) and antagonists of the P2Y12 receptor is widely used to prevent recurrent ischemic events in patients with ACS.Citation3,Citation4 Among the P2Y12 antagonists, clopidogrel has been the standard treatment since its approval by the US Food and Drug Administration in 1997. Findings from recent large-scale clinical trials demonstrated that platelet inhibition with a novel and more potent P2Y12 receptor antagonist, ticagrelor, and prasugrel reduced the rate of ischemic events compared to clopidogrel.Citation5,Citation6 Subsequently, ticagrelor and prasugrel have been recommended as the first line treatment in both patients with ST segment elevation myocardial infarction (STEMI) and non-ST segment elevation ACS at moderate-to-high risk of ischemic events, regardless of the initial treatment strategy.Citation3,Citation4 Clopidogrel in turn should be used only if ticagrelor and prasugrel are not available, or are contraindicated.Citation3,Citation4 In contrast to clopidogrel and prasugrel, ticagrelor 1) blocks the P2Y12 receptor reversibly, 2) increases the concentration of adenosine, and in contrast to clopidogrel 3) is metabolized independently of the interindividual genetic variability.Citation5 Therefore, ticagrelor is being increasingly investigated in patients with ACS, as well as in non-coronary indications.
In this review, we briefly present the pharmacokinetics and pharmacodynamics of P2Y12 antagonists, summarize the current evidence on the superiority of ticagrelor over clopidogrel in ACS, discuss the mechanism underlying the drug–drug interactions and pleiotropic effects of ticagrelor, and present future perspectives of non-coronary indications for ticagrelor.
P2Y12 receptor characteristics, P2Y12 antagonists pharmacokinetics and pharmacodynamics
P2Y12 receptor is a G-coupled receptor expressed mainly on platelet cells and merely present on microglial cells.Citation7,Citation8 Binding of ADP results in receptor activation, inhibition of adenyl cyclase, decrease in cyclic adenosine monophosphate level, and finally platelet aggregation.Citation7 Expression of P2Y12 receptor may vary due to 1) substitution in the P2Y12R coding gene, 2) qualitative abnormalities of the platelet P2Y12R which result in extensive bleeding disorders, and 3) chronic conditions like diabetes mellitus (DM) and chronic kidney disease (CKD) which are associated with high activity of P2Y12R.Citation7,Citation9 Although the scope of P2Y12R functions exceeds beyond platelet activity, the primary function of the P2Y12 receptor includes platelet activation and therefore its inhibition evokes interest in the prevention of thrombotic events.Citation8
A summary of pharmacodynamic and pharmacokinetic properties of oral P2Y12 antagonists is presented in .Citation10 Clopidogrel is a prodrug. Following oral administration and intestinal absorption of clopidogrel, it is inactivated by esterases and only 15% of the dose is further metabolized in a two-step process by different hepatic cytochrome P450 (CYP450) isoenzymes. The response to clopidogrel is highly variable. The most important aspects that influence the response to clopidogrel include genetic factors, comorbidities, with an emphasis on DM and chronic renal failure, as well as adjunctive pharmacotherapy, including proton pump inhibitors, calcium-channel blockers, coumarin derivatives and statins.Citation7 Thus, about one-third of the clopidogrel recipients remain resistant to its anti-aggregatory effect – a phenomenon called high on-treatment platelet reactivity.Citation11
Table 1 Pharmacodynamics and pharmacokinetics of oral P2Y12 inhibitors
A third-generation thienopyridine, prasugrel, is also administered as a prodrug, which needs intestinal and hepatic conversion.Citation10 However, only one CYP450 step is involved in this process, and prasugrel pharmacokinetics and pharmacodynamics are less dependent on genetic variability.Citation10 Prasugrel active metabolite achieves inhibition of platelet aggregation (IPA) within 1 hour after administration.Citation10 Consequently, DAPT using this newer P2Y12 inhibitor results in faster, more consistent, and stronger platelet inhibition.Citation10
In contrast to both clopidogrel and prasugrel, ticagrelor is a unique non-thienopyridine P2Y12 antagonist, which does not require metabolic activation, binds to the P2Y12 receptor in a reversible manner, reaches IPA within 30 minutes after administration, and demonstrates pleiotropic effects probably by increasing adenosine concentration and by yet unknown mechanisms. These features likely set ticagrelor in a higher position among the P2Y12 antagonists, and contribute to the wide spectrum of clinical benefits.
Superiority of ticagrelor over clopidogrel in ACS
presents a comparison of the efficacy and safety outcomes between ticagrelor and other P2Y12 antagonists in patients with ACS.
Table 2 Comparison of the efficacy and safety outcomes between ticagrelor and other P2Y12 antagonists in patients with ACS, with or without ST segment elevation
The superiority of ticagrelor over clopidogrel has been initially established based on the results of the multicenter, double-blind, randomized PLATO (Platelet Inhibition and Patient Outcomes) study, which compared ticagrelor and clopidogrel for the prevention of cardiovascular (CV) events in 18,624 patients with ACS, with or without ST segment elevation.Citation5 PLATO showed a reduction in the primary efficacy endpoint (a composite of death from vascular causes, acute myocardial infarction [AMI], or stroke) in patients treated with ticagrelor, as compared to those treated with clopidogrel (9.8% vs 11.7%, respectively, p<0.001) at 12 months. Importantly, no significant difference in the rates of major bleeding was found between the ticagrelor and clopidogrel groups (11.6% vs 11.2%, p=0.43), although ticagrelor was associated with a higher rate of fatal intracranial bleeding, and lower rate of fatal bleeding of other types. The conclusions from PLATO were confirmed in a real-life setting in the Swedish web-system for enhancement and development of evidence-based care in heart disease evaluated according to recommended therapies as well as in several other studies listed in .Citation12 Additionally, a recent meta-analysis of nine randomized clinical trials that included 106,288 patients showed reduced all-cause mortality, CV mortality, rate of AMI and stent thrombosis with ticagrelor, compared to clopidogrel, while the rate of major bleeding between the two groups was comparable.Citation13
The benefits of long-term administration of DAPT with ticagrelor were demonstrated in the PEGASUS TIMI 54 trial (Prevention of Cardiovascular Events in Patients with Prior Heart Attack Using Ticagrelor Compared to Placebo on a Background of Aspirin-Thrombolysis in Myocardial Infarction 54),Citation14 which randomized 21,162 patients who had had AMI 1–3 years earlier to ticagrelor at a dose of 90 mg twice daily, ticagrelor at a dose of 60 mg twice daily, or placebo. Both doses were shown to decrease the composite endpoint of CV death, AMI, or stroke (7.85% vs 9.04%, p=0.008 for 90 mg vs placebo, 7.77% vs 9.04%, p=0.004 for 60 mg vs placebo) after 33 months of treatment. However, the rate of major bleeding was higher with both doses of ticagrelor (2.60% with 90 mg and 2.30% with 60 mg) than with placebo (1.06%, p<0.001 for each dose vs placebo), without significant differences in fatal bleeding. Based on the PEGASUS TIMI 54 trial, it seems that patients with generally low bleeding risk might benefit from prolonged treatment with ticagrelor over 12 months. However, additional research is required to define the target population for this treatment strategy.
The promising results of the PLATO and PEGASUS TIMI 54 trials were not confirmed in the PHILO study (Phase the International Study of Ticagrelor and Clinical Outcomes in Asian ACS Patients) and a substudy in the Asian cohort of the PLATO-US, undermining the benefits of ticagrelor in Asian patients.Citation15,Citation16 Both in PHILO and in the Asian cohort of PLATO-US there was a tendency toward more death, AMI, and AIS in patients treated with ticagrelor compared with clopidogrel (hazard ratio, 1.47; 95% confidence interval [CI]: 0.88–2.44 in PHILO and 0.68–2.01 in the PLATO-US cohort). Additionally, there were more major bleedings on ticagrelor in the PHILO study, whereas the bleeding rate in the PLATO-US cohort study was not increased, and comparable with the rest of the PLATO study.Citation15,Citation17 Nevertheless, the higher rate of ischemic events in Asian patients calls for further investigation regarding the benefits of ticagrelor administration in Asian populations.
Ticagrelor was not superior to clopidogrel when combined with anticoagulant therapy. A study that compared a double therapy comprising ticagrelor and warfarin with a triple therapy comprising ASA, clopidogrel, and warfarin demonstrated a comparable rate of thrombotic and bleeding events in both groups.Citation18 Additionally, in the GEMINI ACS-1 (A Study to Compare the Safety of Rivaroxaban Versus Acetylsalicylic Acid in Addition to Either Clopidogrel or Ticagrelor Therapy in Participants with Acute Coronary Syndrome) trial, the rate of thrombotic and bleeding events for rivaroxaban versus aspirin was similar in the ticagrelor group compared with the clopidogrel group. However, the choice of clopidogrel or ticagrelor during the trial was not randomized, but was rather based on the investigator’s preference. These analyses are exploratory and leave space for various hypotheses. In the absence of sufficient efficacy and safety data, the use of ticagrelor or prasugrel as a part of triple therapy is not recommended.Citation19
Indirect comparison of the two cornerstone studies comparing the efficacy of ticagrelor and prasugrel (PLATO and TRITON TIMI 38) revealed that prasugrel results in greater reduction of PLATO-defined primary endpoints (overall CV death, AMI, ischemic stroke) and mortality in STEMI groups, with no difference in primary endpoint in patients with non-ST segment elevation myocardial infarction (NSTEMI; ). Moreover, prasugrel increased the risk of non-coronary artery bypass graft (CABG)-associated major bleeding. However, two studies and one meta-analysis which compared ticagrelor and prasugrel directly in terms of the reduction of PLATO-defined efficacy and safety endpoints showed no differences in CV mortality, the rate of AMI and AIS at 1 and 3 months.Citation16–Citation18 Importantly, the latter study and the meta-analysis showed reduced rate of stent thrombosis in patients receiving prasugrel, which, however, did not translate into reduced mortality.Citation20,Citation21 The reduced rate of stent thrombosis on prasugrel may be due to stronger and more rapid platelet inhibition by prasugrel, compared to ticagrelor.Citation22 Interestingly, in patients with AMI and type 2 DM, ticagrelor seems to demonstrate greater inhibition of ADP-induced platelet reactivity in comparison to prasugrel, in both the acute and chronic phases of treatment.Citation23
Figure 1 Ticagrelor versus prasugrel – efficiency and safety comparison.
Abbreviations: RRR, relative risk reduction; NNT, number needed to treat; RRI, relative risk increase; NNH, number needed to harm; CABG, coronary artery bypass graft; NSTE-ACS, non-ST-elevation acute coronary state; STEMI, ST segment elevation myocardial infarction.
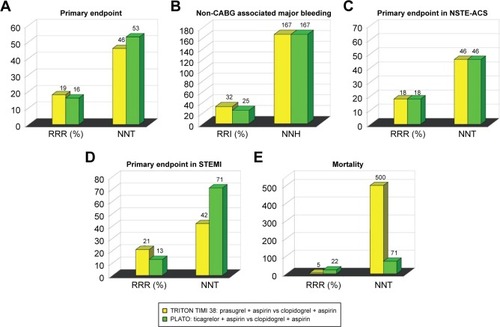
The difference in bleeding risk between ticagrelor and prasugrel remains unclear (). The previously mentioned meta-analysis demonstrated that ticagrelor is associated with a numerically, albeit nonsignificant, lower risk of major bleeding than prasugrel during 1 year follow-up.Citation13 However, a real-world comparison of ticagrelor and prasugrel in 16,098 patients with ACS demonstrated a significantly lower rate of major bleeding events on prasugrel during 1-month follow-up.Citation24 More studies are required to identify the P2Y12 antagonist associated with the lowest bleeding rate. Interestingly, a trial in which recombinant activated factor VII, fibrinogen concentrate, and factor XIII concentrate were used to overcome antiplatelet effect by acting on fibrin formation or fibrinolysis may point to the cessation of ticagrelor-related unrestrained bleeding.Citation25
Ticagrelor drug–drug interactions in ACS
Among interactions with other drugs, concomitant use of ticagrelor with morphine, statins, and digoxin seems relevant.Citation4 Morphine has been reported to reduce the absorption of ticagrelor by its inhibitory effect on gastric motility.Citation26 Studies performed on patients with AMI receiving ticagrelor and either morphine or placebo demonstrated diminished and delayed antiplatelet effect in the morphine group. Additionally, a clinically relevant decrease of maximal serum concentrations of both ticagrelor and its active metabolite and prolonged clearance of ticagrelor were observed.Citation27,Citation28 Interestingly, in healthy volunteers a similar decrease of concentration of ticagrelor achieved by a comparable dose of morphine was observed, although platelet inhibition remained adequate.Citation29 It is likely that the publication of the results of IMPRESSION (Influence of Morphine on Pharmacokinetics and Pharmacodynamics of Ticagrelor in Patients with Acute Myocardial Infarction) trial will elucidate this interaction.Citation30
In addition, morphine causes, via a similar mechanism, significant decrease in the action of clopidogrel.Citation31 Current European Society of Cardiology guidelines for the management of AMI recommend intravenous morphine titration in severe pain, however indicating the possibility of failure of antiplatlet effect due to interaction with morphine.Citation32
Revision of results of the PLATO trial which focused on the interaction between ticagrelor and statins concluded that co-administration of ticagrelor and statins decreased both vascular and all-cause mortality, compared to clopidogrel and statins.Citation29 Increased concentration of simvastatin in the presence of ticagrelor was confirmed also in healthy volunteers.Citation33 These results have been attributed to the fact that ticagrelor, in contrast to clopidogrel, weakly inhibits CYP450 3A4 and delays metabolism of certain statins, especially simvastatin. Both ticagrelor and rosuvastatin were shown to increase the concentration of adenosine in animal models, which may further contribute to the beneficial effect of their co-administration.Citation34,Citation35 Nevertheless, a series of case studies have reported an increased risk of rhabdomyolysis when ticagrelor was co-administrated with high-dose statins in patients with CKD, suggesting that the ticagrelor–statins interaction may be clinically relevant in particular patient populations.Citation36,Citation37
The co-administation of ticagrelor with digoxin warrants caution as well. Because ticagrelor is a weak inhibitor of P-glycoprotein, which is involved in the metabolism of digoxin, the concentration of digoxin may increase once ticagrelor is initiated. Hence, in patients treated with ticagrelor the concentration of digoxin should be monitored.Citation38
Genetic polymorphism
The genetic background of ticagrelor response has been investigated previously in several pharmacogenetics studies, but the genetic determination of ticagrelor response in humans still remains unknown. The PLATO trial demonstrated that ticagrelor reduces the rate of a combined endpoint of CV death, AMI, or stroke with no increase in the incidence of major bleeding as compared to clopidogrel, irrespective of cytochrome P450 2C19 (CYP2C19) and adenosine triphosphate (ATP) binding cassette subfamily B (ABCB1) genetic polymorphisms.Citation39 In the genetic substudy of the PLATO trial, a two-phase design was used for a genome-wide association study (GWAS): a discovery phase, which consisted of 3,998 individuals genotyped, and a replication phase of an additional 6,015 individuals. The GWAS results on ticagrelor pharmacokinetics in a large cohort of ticagrelor-treated ACS patients showed an association of three different genetic loci (SLCO1B1-rs4149056, CYP3A4-rs62471956, rs56324128, and UGT2B7-rs61361928) with ticagrelor levels. Importantly, the modest genetic impact on plasma levels of ticagrelor and the active metabolite of ticagrelor (AR-C124910XX [ARC]) did not translate into effect on any efficacy (ie, CV death, MI, and stroke) or safety endpoints (ie, non-CABG-related bleeds or investigator-reported dyspnea).Citation40 In a recent study, the impact of genetic variations within both ITGA2B and ITGB3 encoding genes on ex vivo antiplatelet effects of ticagrelor in Chinese healthy subjects was studied. In 28 carriers of ITGA2B rs5911 GG genotype was associated with lower level of platelet ADP-induced platelet activation after incubation with ticagrelor. The study showed that the SNP can decrease the ex vivo antiplatelet activity of ticagrelor, especially at low concentration, though the baseline platelet activity was not affected by the polymorphism. However, the ITGB3 rs4642 or rs4634 polymorphisms had no effect on either the baseline platelet activity or the ex vivo antiplatelet effect of ticagrelor.Citation41 In another study, the same group of researchers further evaluated a population of 196 healthy Chinese volunteers in order to analyze the association between platelet reactivity with or without ticagrelor and nine P2Y12 SNPs (rs1907637 C.T, rs79320243 A.G/htSNP, rs10935842 A.T/htSNP, rs6787801 T.C/htSNP, rs6801273 A.G, rs16863323 G.A, rs2046934 T.C, rs6785930 C.T, and rs6809699 G.T/htSNP) and the GNB3 rs5443 C.T polymorphism.Citation42 However, genetic variations in P2Y12 and GNB3 were not associated with interindividual variability in platelet inhibition after partial ex vivo blockade with ticagrelor. The abovementioned observations stand in line with the first study, which observed that SNPs in P2Y12, P2Y1, and ITGB3 do not affect ticagrelor-induced inhibition of ADP-induced platelet aggregation.Citation43 In another study conducted in healthy Chinese male subjects, eight different SNPs within PEAR1 gene were evaluated in order to analyze their association with in vitro platelet reactivity and ticagrelor pharmacokinetics. It was found that PEAR1 rs12041331 polymorphism is associated with in vitro antiplatelet activity of ticagrelor but no significant difference in ticagrelor pharmacokinetics with the rs12041331 genotype was observed. Minor homozygotes of two SNPs (rs12041331, rs12566888) exhibited statistically significant lower maximal platelet activation and minor allele carriers of rs4661012 polymorphism exhibited statistically significant higher maximal platelet activation. PEAR1 intronic variant rs12041331 AA genotype and 3′-UTR variant rs4661012 GG genotype were associated with an increased IPA after in vitro ticagrelor incubation at low and high concentrations, respectively. However, the mechanisms by which rs12041331 polymorphism influences ticagrelor response remain unknown. No significant difference in the pharmacokinetic parameters of ticagrelor and ARC were observed among PEAR1 genotypes of candidate SNPs.Citation44 At present, there are no data supporting any impact of genetic polymorphisms in the pharmacokinetics of ticagrelor on clinical outcomes of patients.
Mechanism underlying the pleiotropic effects of ticagrelor
The results of the PLATO trial were embraced with growing interest in the extra-platelet effects of ticagrelor. Ticagrelor administration was shown to be associated with the increased concentration of adenosine caused by 1) inhibition of adenosine reuptake by blocking human equilibrative nucleoside transporter 1,Citation45 and 2) increased release of ATP, subsequently transformed into adenosine.Citation46
Although ticagrelor was proved to elevate serum adenosine levels only in higher doses than standard, a similarity between part of pleiotropic effects exerted by ticagrelor and those mediated by adenosine was proved and described.Citation47,Citation48 This may suggest that some pleiotropic effects of ticagrelor are achieved via adenosine-dependent mechanism. Effects induced by an increased concentration of adenosine and stimulation of adenosine receptors (A1–A3) are summarized in .Citation49,Citation50 Comparably, probable adenosine-dependent pleiotropic effects of ticagrelor together with pleiotropic mechanisms of unknown origin and mechanisms underlying the adenosine inhibition reuptake are presented in .
Figure 2 Mechanisms underlying the probable adenosine-dependent and non-adenosine-dependent pleiotropic effects of ticagrelor.
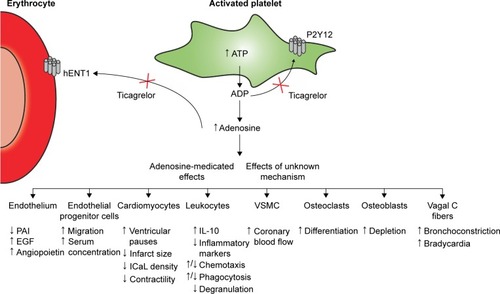
Table 3 Effects induced by stimulation of membrane-bound adenosine receptors (A1–A3)
The first described pleiotropic effect was decreased death rate in patients with ACS receiving ticagrelor (PLATO subgroup) who presented with sepsis or pulmonary infection.Citation51 This phenomenon was proposed to be based on adenosine- related depletion of pro-inflammatory factors by acting on A2A and A2B adenosine receptors, as well as on decreased platelet reactivity, and thus prevention of disseminated intravascular coagulation.Citation52,Citation53 In another study, vasodilation of coronary arteries and increased coronary blood flow velocity (CBFV) were described in patients with NSTEMI undergoing percutaneous coronary intervention. Ticagrelor exhibited higher maximal CBFV/baseline CBFV ratio than prasugrel at increasing concentrations of adenosine infusion rate, confirming that the increased CBFV on ticagrelor is associated with the inhibition of adenosine reuptake.Citation54 In a study performed on diabetic rats, ticagrelor in combination with rosuvastatin decreased the infarct size due to more potent adenosine-dependent myocardial reperfusion.Citation34 Ticagrelor was shown to increase the concentration of (cluster of differentiation) CD34+/CD133+ endothelial progenitor cells (EPC) in peripheral blood, which are responsible for endothelial regeneration in patients after ACS.Citation55 The mechanism underlying the increased concentration of EPC is adenosine-modulated migration of EPC instigated by activation of A2A and A3 receptors as well as increased production of endothelial growth factor, interleukin-8 and angiopoietin-1 in endothelial cells, monocytes, and macrophages.Citation56–Citation59 Ticagrelor was also shown to inhibit differentiation of osteoclasts and promote differentiation of osteoblasts via adenosine A2A receptors in vitro.Citation60 Another pleiotropic effect of ticagrelor includes reduced expression and activity of tissue factor and plasminogen activator inhibitor-1 in left atrium appendage endocardial cells isolated from patients with atrial fibrillation, which might translate into reduced risk of stroke and other ischemic events due to thrombus formation in the left atrium.Citation61 On the contrary, ticagrelor has been proved to reduce L-type Ca(2+) current density in rat ventricular myocytes as well as to decrease sarcomere shortening of electrically stimulated cardiomyocytes.Citation62
The increased serum concentration of adenosine seems to be responsible also for ticagrelor-related adverse effects, including dyspnea, ventricular pauses, bradycardia, and bradyarrhythmias. summarizes the most frequent adverse effects of ticagrelor in patients with ACS, coronary artery disease, and pulmonary disease (asthma, chronic obstructive pulmonary disease [COPD]). Dyspnea during ticagrelor administration and during simultaneous adenosine infusion was confirmed in numerous studies.Citation63–Citation65 Dyspnea is caused by adenosine acting on A1 and A2A receptors present on C fibers of vagal nerve causing bronchoconstriction.Citation66 Ticagrelor-related dyspnea is described as sudden and unexpected air hunger or unsatisfied inspiration, and in most cases is recognized as mildly intense.Citation67 The diagnosis of ticagrelor-related dyspnea is based on exclusion of other causes of dyspnea. Occurrence of dyspnea varies among trials and depends mainly on the length of administration and dosage of ticagrelor. For example, dyspnea was the reason for ticagrelor discontinuation in 2%–9% ACS patients,Citation68 whereas dyspnea was not observed in healthy elderly volunteers and mild asthma or mild-to-moderate COPD patients.Citation65 The lack of dyspnea in the latter study was probably due to short duration of the trial.
Table 4 Incidence of the most frequent adverse effects of ticagrelor in patients with acute coronary syndrome, coronary artery disease, and pulmonary disease (asthma, COPD)
Bradycardia as well as ventricular pauses are side effects of adenosine-related stimulation of adenosine A1 receptor present in heart tissue.Citation69 Bradycardia is recognized as a side effect of all oral P2Y12 antagonists; however, it seems to occur more often on ticagrelor. Differences in the incidence of bradycardia in various studies depend on the definition of “bradycardia” (any decrease in the heart rate versus heart rate below 60 beats per minute). Due to chronotropic effect, ticagrelor decreases the heart rate in all patients, but only in a few cases does ticagrelor cause clinically relevant bradycardia. For example, in 300 patients with AMI, ticagrelor was associated with double the risk of bradycardia (80 patients) than with clopidogrel (32 patients).Citation70 It is not known, however, which clinical event described as bradycardia met the clinical definition of bradycardia, as its incidence varies significantly amidst the trials (PHILO, PLATO, PEGASUS), where bradycardia incidence varied from 1.5% to 7%. Nevertheless, several cases were reported where ticagrelor induced development of secondary degree type 2 block and complete atrioventricular block.Citation71,Citation72
In a substudy of PLATO 5.8% of patients developed asymptomatic, sinusoid ventricular pauses (>3s) during the first week of treatment, which ceased with time.Citation73 In the PHILO and PEGASUS trials the occurrence of ventricular pauses was 0% and 1.6%, respectively, making ventricular pauses a clinically irrelevant complication. Noteworthy, in one case report both bradycardia and dyspnea were reversed using aminophylline, suggesting that administration of aminophylline might counteract the adenosine-related adverse effects of ticagrelor.Citation74
Ticagrelor in non-coronary indications
Major clinical trials involving ticagrelor in non-coronary indications are included in .
Table 5 Ticagrelor in non-coronary indications
Ischemic stroke and transient ischemic attacks
Major evidence of benefits of ticagrelor in AIS or transient ischemic attacks (TIA) arises from the SOCRATES trial (Acute Stroke or Transient Ischemic Attack Treated with Aspirin or Ticagrelor and Patient Outcomes). In SOCRATES, ticagrelor was not superior over ASA in terms of efficacy outcomes in any group of patients. Moreover, both drugs were associated with comparable risk of bleeding and other adverse effects, except for more common dyspnea among patients treated with ticagrelor.Citation75 Noteworthy, a subanalysis of the SOCRATES results in Asian patients compared with non-Asian patients demonstrated equal efficacy of ticagrelor in both groups, but a lower risk of major hemorrhage in Asian patients receiving ticagrelor.Citation76 The beneficial effects of ticagrelor were hypothesized to be associated with the prior long-term use of ASA, which would result in transient DAPT.Citation77,Citation78 In the absence of no clear explanation, as of today, ticagrelor has not been included in the recent guidelines of secondary prevention of stroke.Citation79,Citation80
Peripheral arterial disease (PAD)
The use of ticagrelor seems to be associated with a reduced risk of PAD progression among patients with prior AMI. A summary of the previous reports could not firmly demonstrate the superiority of either ticagrelor or clopidogrel in the treatment and prevention of the complications of PAD.Citation81–Citation83 Ultimately, results of the EUCLID (Examining Use of Ticagrelor in Peripheral Artery) trial conclude that both drugs have a comparable efficacy and safety profile, and that there are no differences in adverse effects.Citation84 Nevertheless, novel antiplatelet agents have not yet been introduced in routine pharmacotherapy of PAD.Citation85
Coronary artery bypass grafting
Antithrombotic therapy following the procedure of coronary artery bypass grafting is generally based on ASA. Nevertheless, graft failure due to thrombosis occurs in up to 10% of cases and therefore P2Y12 inhibitors are incrementally introduced in patients after CABG. A retrospective observation of 705 patients suggests that exposure to ticagrelor shortly before CABG is associated with a higher risk of hemorrhagic complications. This effect was not observed when ticagrelor was discontinued 3 days prior to surgery.Citation86 A study focusing on the turnover of platelets after CABG suggests that ticagrelor is more efficient than clopidogrel in patients, in whom rapid supply of young platelets occurs.Citation87 A comprehensive insight into the use of ticagrelor after CABG is anticipated from results of the current TiCAB (Ticagrelor in CABG) trial, which aims to compare the efficacy and safety of ticagrelor and ASA after CABG.Citation88
Conclusion
Ticagrelor has the potential to revolutionize the treatment of coronary artery disease and ACS due to reduction of CV death as proved in the PEGASUS TIMI 54 trial, when implemented as a component of DAPT. Ticagrelor seems to demonstrate more potent platelet inhibition in ACS patients with DM and/or COPD, as compared with prasugrel, at equal bleeding risk.Citation22,Citation89 Nevertheless, the underperformance of ticagrelor in Asian population shown in the PHILO study needs further investigation. At present, no genetic polymorphisms influencing the metabolism of ticagrelor have been identified to clarify the differences in the efficacy/safety profile of ticagrelor depending on race and comorbidities. The role of ticagrelor in patients with stroke/TIA, PAD, and post-CABG remains limited, as no superiority of ticagrelor over clopidogrel has been shown. Nevertheless, the decreased reuptake of adenosine, which is likely responsible for ticagrelor pleiotropic effects, strengthens the role of ticagrelor in long-term antiplatelet therapy in patients with ACS, as well as in non-ACS indications. For example, ticagrelor might be beneficial in sepsis, as it decreases the concentration of inflammatory biomarkers and modulates the formation of fibrin clots. Regarding the unique pharmacokinetic and pharmacodynamics properties of ticagrelor, as well as the not yet entirely clear pleiotropic effects, ticagrelor remains an active research topic. Once the mechanisms underlying ticagrelor’s mode of action are clarified in vivo, the indications of ticagrelor administration are likely to expand.
Disclosure
Research subject was implemented with CEPT infrastructure financed by the European Union – the European Regional Development Fund within the Operational Program “Innovative economy” for 2007–2013. The study was supported financially as part of the research grant from the National Science Center OPUS research grant (grant number 2013/11/B/NZ7/01541). The authors report no other conflicts of interest in this work.
References
- LindenMDJacksonDEPlatelets: pleiotropic roles in atherogenesis and atherothrombosisInt J Biochem Cell Biol2010421762176620673808
- HechlerBGachetCPurinergic receptors in thrombosis and inflammationArterioscler Thromb Vasc Biol2015352307231526359511
- WindeckerSKolhPAlfonsoF2014 ESC/EACTS guidelines on myocardial revascularization: the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI)Eur Heart J2014352541261925173339
- RoffiMPatronoCColletJP2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC)Eur Heart J20163726731526320110
- WallentinLBeckerRCBudajATicagrelor versus clopidogrel in patients with acute coronary syndromesN Engl J Med20093611045105719717846
- WiviottSDBraunwaldEMcCabeCHPrasugrel versus clopidogrel in patients with acute coronary syndromesN Engl J Med20073572001201517982182
- ZhangYZhangSDingZRole of P2Y12 receptor in thrombosisAdv Exp Med Biol201790630732427628007
- BurnstockGPurinergic signalling: therapeutic developmentsFront Pharmacol2017866128993732
- LecchiAFemiaEAPaolettaSInherited dysfunctional platelet P2Y12 receptor mutations associated with bleeding disordersHamostaseologie20163627928327487748
- TengRTicagrelor: pharmacokinetic, pharmacodynamic and pharmacogenetic profile: an updateClin Pharmacokinet2015541125113826063049
- MevesSHSchroderKDEndresHGKrogiasCKrugerJCNeubauerHClopidogrel high-on-treatment platelet reactivity in acute ischemic stroke patientsThromb Res201413339640124406048
- SahlenAVarenhorstCLagerqvistBOutcomes in patients treated with ticagrelor or clopidogrel after acute myocardial infarction: experiences from SWEDEHEART registryEur Heart J2016373335334227436867
- ShahRRashidAHwangIFanTMKhouzamRNReedGLMeta- analysis of the relative efficacy and safety of oral P2Y12 inhibitors in patients with acute coronary syndromeAm J Cardiol20171191723172828385176
- BonacaMPBhattDLCohenMLong-term use of ticagrelor in patients with prior myocardial infarctionN Engl J Med20153721791180025773268
- GotoSHuangCHParkSJEmanuelssonHKimuraTTicagrelor vs clopidogrel in Japanese, Korean and Taiwanese patients with acute coronary syndrome – randomized, double-blind, phase III PHILO studyCirc J2015792452246026376600
- SerebruanyVLTomekAPyaYBekbossynovaMKimMHInferiority of ticagrelor in the PHILO trial: play of chance in East Asians or nightmare confirmation of PLATO-USA?Int J Cardiol201621537237627128564
- KangHJClareRMGaoRTicagrelor versus clopidogrel in Asian patients with acute coronary syndrome: a retrospective analysis from the Platelet Inhibition and Patient Outcomes (PLATO) trialAm Heart J201516989990526027629
- BraunOOBicoBChaudhryUConcomitant use of warfarin and ticagrelor as an alternative to triple antithrombotic therapy after an acute coronary syndromeThromb Res2015135263025467434
- LevineGNBatesERBittlJA2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelinesJ Thorac Cardiovasc Surg20161521243127527751237
- RolliniFFranchiFChoJRA head-to-head pharmacodynamic comparison of prasugrel vs. ticagrelor after switching from clopidogrel in patients with coronary artery disease: results of a prospective randomized studyEur Heart J2016372722273026848148
- SucatoVCorradoECastellanaCReal-world use of ticagrelor and prasugrel in patients with NSTEMI undergoing percutaneous coronary interventionJ Cardiovasc Med (Hagerstown)201718645045128306694
- FranchiFRolliniFChoJRImpact of escalating loading dose regimens of ticagrelor in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: results of a prospective randomized pharmacokinetic and pharmacodynamic investigationJACC Cardiovasc Interv201581457146726404199
- FranchiFRolliniFAggarwalNPharmacodynamic comparison of prasugrel versus ticagrelor in patients with type 2 diabetes mellitus and coronary artery disease: the OPTIMUS (Optimizing Antiplatelet Therapy in Diabetes Mellitus)-4 studyCirculation201613478079227559041
- LarmoreCEffronMBMolifeC“Real-world” comparison of prasugrel with ticagrelor in patients with acute coronary syndrome treated with percutaneous coronary intervention in the United StatesCatheter Cardiovasc Interv20168853554426577386
- CalmetteLMartinACLe BonniecBTicagrelor reversal: in vitro assessment of four haemostatic agentsJ Clin Pathol201770973373928159767
- KubicaJKubicaAJilmaBImpact of morphine on antiplatelet effects of oral P2Y12 receptor inhibitorsInt J Cardiol201621520120827128531
- KubicaJAdamskiPOstrowskaMMorphine delays and attenuates ticagrelor exposure and action in patients with myocardial infarction: the randomized, double-blind, placebo-controlled IMPRESSION trialEur Heart J20163724525226491112
- ParodiGBellandiBXanthopoulouIMorphine is associated with a delayed activity of oral antiplatelet agents in patients with ST-elevation acute myocardial infarction undergoing primary percutaneous coronary interventionCirc Cardiovasc Interv20158e00159325552565
- HoblELReiterBSchoergenhoferCMorphine decreases ticagrelor concentrations but not its antiplatelet effects: a randomized trial in healthy volunteersEur J Clin Invest20164671426449338
- KubicaJAdamskiPOstrowskaMInfluence of morphine on pharmacokinetics and pharmacodynamics of ticagrelor in patients with acute myocardial infarction (IMPRESSION): study protocol for a randomized controlled trialTrials20151619825925591
- WangZYChenMZhuLLPharmacokinetic drug interactions with clopidogrel: updated review and risk management in combination therapyTher Clin Risk Manag20151144946725848291
- IbanezBJamesSAgewallS2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC)Eur Heart J Epub2017826
- TengRMitchellPDButlerKAPharmacokinetic interaction studies of co-administration of ticagrelor and atorvastatin or simvastatin in healthy volunteersEur J Clin Pharmacol20136947748722922682
- BirnbaumYBirnbaumGDBirnbaumINylanderSYeYTicagrelor and rosuvastatin have additive cardioprotective effects via adenosineCardiovasc Drugs Ther20163053955027830382
- BirnbaumGDBirnbaumIYeYBirnbaumYStatin-induced cardioprotection against ischemia-reperfusion injury: potential drug–drug interactions. Lesson to be learnt by translating results from animal models to the clinical settingsCardiovasc Drugs Ther20152946146726303765
- van VurenAJde JongBBootsmaHPVan der VeenMJFeithGWTicagrelor-induced renal failure leading to statin-induced rhabdomyolysisNeth J Med20157313613825852115
- KidoKWheelerMBSeratnahaeiABaileyABainJARhabdomyolysis precipitated by possible interaction of ticagrelor with high-dose atorvastatinJ Am Pharm Assoc201555320323
- Siller-MatulaJMTrenkDKrahenbuhlSMichelsonADDelle-KarthGClinical implications of drug–drug interactions with P2Y12 receptor inhibitorsJ Thromb Haemost20141221324406062
- WallentinLJamesSStoreyRFEffect of CYP2C19 and ABCB1 single nucleotide polymorphisms on outcomes of treatment with ticagrelor versus clopidogrel for acute coronary syndromes: a genetic substudy of the PLATO trialLancet20103761320132820801498
- VarenhorstCErikssonNJohanssonAEffect of genetic variations on ticagrelor plasma levels and clinical outcomesEur Heart J2015361901191225935875
- LiMPXiongYXuAAssociation of platelet ITGA2B and ITGB3 polymorphisms with ex vivo antiplatelet effect of ticagrelor in healthy Chinese male subjectsInt J Hematol20149926327124474638
- LiMPTangJWenZPInfluence of P2Y12 polymorphisms on platelet activity but not ex-vivo antiplatelet effect of ticagrelor in healthy Chinese male subjectsBlood Coagul Fibrinolysis20152687488126083990
- StoreyRFMelissa ThorntonSLawranceRTicagrelor yields consistent dose-dependent inhibition of ADP-induced platelet aggregation in patients with atherosclerotic disease regardless of genotypic variations in P2RY12, P2RY1, and ITGB3Platelets20092034134819637098
- LiMHuYWenZAssociation of PEAR1 rs12041331 polymorphism and pharmacodynamics of ticagrelor in healthy Chinese volunteersXenobiotica201747121130113827937053
- van GiezenJJSidawayJGlavesPKirkIBjorkmanJATicagrelor inhibits adenosine uptake in vitro and enhances adenosine-mediated hyperemia responses in a canine modelJ Cardiovasc Pharmacol Ther20121716417221697355
- OhmanJKudiraRAlbinssonSOldeBErlingeDTicagrelor induces adenosine triphosphate release from human red blood cellsBiochem Biophys Res Commun201241875475822306816
- CattaneoMSchulzRNylanderSAdenosine-mediated effects of ticagrelor: evidence and potential clinical relevanceJ Am Coll Cardiol2014632503250924768873
- van den BergTNEl MessaoudiSRongenGATicagrelor does not inhibit adenosine transport at relevant concentrations: a randomized crossover study in healthy subjects in vivoPLoS One201510e013756026509673
- LaubachVEFrenchBAOkusaMDTargeting of adenosine receptors in ischemia-reperfusion injuryExpert Opin Ther Targets20111510311821110787
- CattaneoMSchulzRNylanderSAdenosine-mediated effects of ticagrelorJ Am Coll Cardiol2014632503250924768873
- StoreyRFJamesSKSiegbahnALower mortality following pulmonary adverse events and sepsis with ticagrelor compared to clopidogrel in the PLATO studyPlatelets20142551752524127651
- MullerKAChatterjeeMRathDGeislerTPlatelets, inflammation and anti-inflammatory effects of antiplatelet drugs in ACS and CADThromb Haemost201511449851826224127
- HaskoGCronsteinBNAdenosine: an endogenous regulator of innate immunityTrends Immunol200425333914698282
- AlexopoulosDMouliasAKoutsogiannisNDifferential effect of ticagrelor versus prasugrel on coronary blood flow velocity in patients with non-ST-elevation acute coronary syndrome undergoing percutaneous coronary intervention: an exploratory studyCirc Cardiovasc Interv2013627728323735473
- BonelloLFrereCCointeSTicagrelor increases endothelial progenitor cell level compared to clopidogrel in acute coronary syndromes: a prospective randomized studyInt J Cardiol201518750250725846661
- FernandezPJaraCAguileraVAdenosine A(2)A and A(3) receptors are involved in the human endothelial progenitor cells migrationJ Cardiovasc Pharmacol20125939740422217884
- DubeyRKGillespieDGJacksonEKA(2B) adenosine receptors stimulate growth of porcine and rat arterial endothelial cellsHypertension20023953053511882603
- ShenJHalendaSPSturekMWildenPACell-signaling evidence for adenosine stimulation of coronary smooth muscle proliferation via the A1 adenosine receptorCirc Res20059757458216100051
- ClarkANYoukeyRLiuXA1 adenosine receptor activation promotes angiogenesis and release of VEGF from monocytesCirc Res20071011130113817901362
- MedieroAWilderTReddyVSTicagrelor regulates osteoblast and osteoclast function and promotes bone formation in vivo via an adenosine-dependent mechanismFASEB J2016303887390027511945
- ReinerMFBreitensteinAHolyEWTicagrelor, but not clopidogrel active metabolite, displays antithrombotic properties in the left atrial endocardiumEur Heart J2017381291691928065908
- KucukMCelenMCYamasanBEOlgarYOzdemirSEffects of ticagrelor on ionic currents and contractility in rat ventricular myocytesCardiovasc Drugs Ther20152941942426410045
- WittfeldtAEmanuelssonHBrandrup-WognsenGTicagrelor enhances adenosine-induced coronary vasodilatory responses in humansJ Am Coll Cardiol20136172372723312702
- StoreyRFBlidenKPPatilSBIncidence of dyspnea and assessment of cardiac and pulmonary function in patients with stable coronary artery disease receiving ticagrelor, clopidogrel, or placebo in the ONSET/OFFSET studyJ Am Coll Cardiol20105618519320620737
- ButlerKMayaJTengREffect of ticagrelor on pulmonary function in healthy elderly volunteers and asthma or chronic obstructive pulmonary disease patientsCurr Med Res Opin20132956957723448616
- UnverdorbenMParodiGPistolesiMStoreyRFDyspnea related to reversibly-binding P2Y12 inhibitors: a review of the pathophysiology, clinical presentation and diagnosticsInt J Cardiol201620216717326386945
- StoreyRFBeckerRCHarringtonRACharacterization of dyspnoea in PLATO study patients treated with ticagrelor or clopidogrel and its association with clinical outcomesEur Heart J2011322945295321804104
- HardingSAVan GaalWJSchraleRPractical experience with ticagrelor: an Australian and New Zealand perspectiveCurr Med Res Opin2015311469147726086451
- MustafaSJMorrisonRRTengBPellegAAdenosine receptors and the heart: role in regulation of coronary blood flow and cardiac electrophysiologyHandb Exp Pharmacol2009193161188
- RenQRenCLiuXDongCZhangXTicagrelor vs. clopidogrel in non-ST-elevation acute coronary syndromesHerz20164124624926525521
- SharmaMMascarenhasDATicagrelor associated heart block: the need for close and continued monitoringCase Rep Cardiol20172017507489128246559
- GoldbergARosenfeldINordkinIHalabiMLife-threatening complete atrioventricular block associated with ticagrelor therapyInt J Cardiol201518237938025594929
- SciricaBMCannonCPEmanuelssonHThe incidence of bradyarrhythmias and clinical bradyarrhythmic events in patients with acute coronary syndromes treated with ticagrelor or clopidogrel in the PLATO (Platelet Inhibition and Patient Outcomes) trial: results of the continuous electrocardiographic assessment substudyJ Am Coll Cardiol2011571908191621545948
- MinnerSASimonePChungBBShahAPSuccessful reversal of bradycardia and dyspnea with aminophylline after ticagrelor loadJ Pharm Pract Epub2016125
- JohnstonSCAmarencoPAlbersGWTicagrelor versus aspirin in acute stroke or transient ischemic attackN Engl J Med2016375354327160892
- WangYMinematsuKWongKSTicagrelor in acute stroke or transient ischemic attack in Asian patients: from the SOCRATES trial (Acute Stroke or Transient Ischemic Attack Treated with Aspirin or Ticagrelor and Patient Outcomes)Stroke20174816717327899747
- MorisDBakoyiannisCAvgerinosELetter by Moris et al regarding article, “Ticagrelor in acute stroke or transient ischemic attack in Asian patients: from the SOCRATES trial (Acute Stroke or Transient Ischemic Attack Treated with Aspirin or Ticagrelor and Patient Outcomes)”Stroke201748e11028209714
- AmarencoPAlbersGWDenisonHEfficacy and safety of ticagrelor versus aspirin in acute stroke or transient ischaemic attack of atherosclerotic origin: a subgroup analysis of SOCRATES, a randomised, double-blind, controlled trialLancet Neurol20171630131028238711
- BayonaHOwolabiMFengWA systematic comparison of key features of ischemic stroke prevention guidelines in low- and middle-income vs. high-income countriesJ Neurol Sci201737536036628320168
- CouttsSBWeinTHLindsayMPCanadian Stroke Best Practice Recommendations: secondary prevention of stroke guidelines, update 2014Int J Stroke20151028229125535808
- SpiliopoulosSKatsanosKPastromasGInitial experience with ticagrelor in patients with critical limb ischemia and high on-clopidogrel platelet reactivity undergoing complex peripheral endovascular proceduresCardiovasc Intervent Radiol2014371450145724510279
- KatsanosKSpiliopoulosSSahaPComparative efficacy and safety of different antiplatelet agents for prevention of major cardiovascular events and leg amputations in patients with peripheral arterial disease: a systematic review and network meta-analysisPLoS One201510e013569226274912
- SpiliopoulosSPastromasGCurrent status of high on-treatment platelet reactivity in patients with coronary or peripheral arterial disease: mechanisms, evaluation and clinical implicationsWorld J Cardiol2015791292126730297
- HiattWRFowkesFGHeizerGTicagrelor versus clopidogrel in symptomatic peripheral artery diseaseN Engl J Med2017376324027959717
- Gerhard-HermanMDGornikHLBarrettC2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelinesJ Am Coll Cardiol201769e71e12627851992
- TomsicASchotborghMAManshandenJSLiWWde MolBACoronary artery bypass grafting-related bleeding complications in patients treated with dual antiplatelet treatmentEur J Cardiothorac Surg20165084985627174551
- SchneiderDJChavaSFactors influencing platelet reactivity in patients undergoing coronary artery bypass surgeryCoron Artery Dis20162718519026751426
- de WahaASandnerSvon ScheidtMA randomized, parallel group, double-blind study of ticagrelor compared with aspirin for prevention of vascular events in patients undergoing coronary artery bypass graft operation: rationale and design of the Ticagrelor in CABG (TiCAB) trial: an investigator-initiated trialAm Heart J2016179697627595681
- CampoGVieceli Dalla SegaFPavasiniRBiological effects of ticagrelor over clopidogrel in patients with stable coronary artery disease and chronic obstructive pulmonary diseaseThromb Haemost201711761208121628331925
- Siller-MatulaJMTrenkDSchrörKResponse variability to P2Y12 receptor inhibitorsJACC Cardiovasc Interv201361111112824262612
- VercellinoMSanchezFABoasiVTicagrelor versus clopidogrel in real-world patients with ST elevation myocardial infarction: 1-year results by propensity score analysisBMC Cardiovasc Disord2017179728381298
- Jimenez-BritezGFreixaXFlores-UmanzorEOut-of-hospital cardiac arrest and stent thrombosis: ticagrelor versus clopidogrel in patients with primary percutaneous coronary intervention under mild therapeutic hypothermiaResuscitation201711414114528242212
- BeigelRIakobishviliZShlomoNReal-world use of novel P2Y12 inhibitors in patients with acute myocardial infarction: a treatment paradoxCardiology2017136212827548273
- MotovskaZHlinomazOMiklikRPrasugrel versus ticagrelor in patients with acute myocardial infarction treated with primary per-cutaneous coronary intervention: multicenter randomized PRAGUE-18 studyCirculation20161341603161227576777
- BirkelandKParraDRosensteinRAntiplatelet therapy in acute coronary syndromes: focus on ticagrelorJ Blood Med2010119721922282698
- TurgeonRDFernandesKAJuurlinkDTuJVMamdaniMTicagrelor and bradycardia: a nested case-control studyPharmacoepidemiol Drug Saf2015241281128526448559
- GurbelPABlidenKPButlerKRandomized double-blind assessment of the ONSET and OFFSET of the antiplatelet effects of ticagrelor versus clopidogrel in patients with stable coronary artery disease: the ONSET/OFFSET studyCirculation20091202577258519923168
